Abstract
The clinical applications of botulinum (BoNT) have expanded from the initial use and approval in ophthalmology to include many other conditions dependent upon neurotransmitter release and the SNARE protein complex. As the clinical use and regulatory agency approvals of BoNTs have expanded, extensive experience and published studies support that BoNTs are effective and safe when administered by experienced practitioners. However, there is little data and continued debate on the safest, most accurate, and most effective method to deliver BoNTs to the intended target. This chapter will review the most common guidance techniques for BoNT therapy including anatomic or manual guidance and the instrumented guidance techniques of electromyography (EMG), electrical stimulation (E-Stim), ultrasound (US), and fluoroscopy (Flouro), including discussion of the current level of evidence for the advantages and limitations of each technique.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Botulinum toxin
- Guidance techniques
- Ultrasound
- Electrical stimulation
- E-Stim
- Electromyography
- EMG
- Targeting
- Accuracy
Introduction
Over the past two decades, the clinical applications of botulinum (BoNT) have expanded from the initial use and approval in ophthalmology to include many other conditions which depend upon neurotransmitter release and the SNARE protein complex. Current approvals and proposed applications of BoNTs include conditions ranging from its widely accepted use for muscle overactivity (spasticity, dystonia, tremor, and rigidity) to include neurosecretory, urological, gastrointestinal, and other disorders including pain for which the mechanism of action of BoNTs is incompletely understood.
As the clinical use and regulatory agency approvals of BoNTs have expanded, extensive experience and published studies support that these agents are effective and safe when administered by experienced practitioners. However, there is little data and continued debate on the safest, most accurate, or most effective method to deliver BoNTs to the intended target. This chapter will review the most common guidance techniques for BoNT therapy including anatomic or manual guidance and instrumented guidance techniques including electromyography (EMG) , electrical stimulation (E-Stim), ultrasound (US), and fluoroscopy (Flouro), including discussion of the current level of evidence for the advantages and limitations of each of these techniques .
Guidance Techniques
Anatomic or Manual Guidance
Anatomic (manual) guidance relies on visual identification of surface anatomy, palpation of anatomic landmarks, and/or passive or active range of motion (PROM, AROM) to estimate a muscle position and depth. Once the clinician identifies the muscle, a skin site for needle entry is selected that provides the most direct approach to the intended target and avoids blood vessels and other critical structures. The skin at the site for needle insertion is disinfected and the needle is inserted through the skin and advanced blindly to the estimated muscle position and depth. With manual guidance, standard hypodermic needles are used for injection, typically 25–30 gauge and 0.5–2 1/2 in. in length depending on the estimated depth of the target. The anatomic/manual technique was especially common in the early days of BoNT therapy when many clinicians relied solely on their knowledge of gross and surface anatomy, cross-sectional, or functional anatomy to identify the site for needle insertion and BoNT injection. While a detailed knowledge of anatomy is critical for all injections including chemodenervation procedures, most physicians no longer recommend relying solely on this technique for the majority of BoNT procedures [1] as it has been shown to be inaccurate (see below) [2,3,4]. However, regardless of what supplementary guidance technique is used, all physicians must rely first and foremost on their knowledge of surface, cross-sectional, and functional anatomy when performing chemodenervation procedures .
Advantages
-
1.
All physicians receive education and training in gross and functional anatomy during medical school and perhaps again during residency training.
-
2.
Anatomic guidance requires no specialized equipment and minimal resources, usually only anatomic reference guides. There are many useful print and online resources which can serve as a starting point for estimating the site of needle insertion and target injection [5,6,7,8].
-
3.
Some muscles are easily palpated and/or localized by their anatomic landmarks and position on the limb, trunk, or neck. Examples of easily identified and palpated muscles include the biceps brachii and tibialis anterior.
Limitations: While knowledge of surface and functional anatomy is required for all chemodenervation procedures, relying solely on this technique without supplemental guidance has many limitations [9, 42].
-
1.
Inadequate familiarity with anatomy: Many clinicians who perform chemodenervation procedures had their last exposure to gross anatomy in medical school, often in the distant past, leaving them with only remote memories of the course material. It is difficult for practicing physicians to arrange time and get access to gross anatomy training courses.
-
2.
Individual anatomic variations in location and size: There is substantial individual variation in muscle anatomy, including shape or form, relative size, location or depth, as well as the absence or presence of certain muscles. It is difficult or impossible to determine by inspection or palpation alone whether such an anatomic variation exists in a patient. For example, the palmaris longus (PL), reportedly the most variable muscle in humans, is absent in 4–26% of individuals. Even when present, the PL varies in size; can have one or more bellies and can be either tendinous or muscular at either the proximal or distal end [10, 11]. In some individuals, the PL is unusually large, thereby potentially having a greater contribution to wrist flexion force than expected (Fig. 1a, b). When treating a patient with wrist flexor spasticity, this anatomic variation alone may impact the outcome of BoNT injections. The PL is often left untreated as it is thought to contribute little to wrist flexion. If, however, a large PL is present, failure to target this muscle may contribute to treatment failure and a false conclusion of insufficient dosing in other wrist flexor muscles rather than recognizing the need to inject the PL.
-
3.
Disease processes can also distort anatomy: Spastic muscles may be shortened and shifted in position. Dystonic muscles may hypertrophy from repeated over-contraction.
-
4.
Complex overlapping anatomy and muscle depth: There are approximately 20 muscles in the forearm alone, with so many deep and overlapping that it may be difficult or impossible to estimate the position of these muscles by palpation or inspection. The same is true for estimating the position and depth of muscles in other areas, such as the neck or lower limb where the muscles are deep to overlying adipose tissue.
-
5.
Interposed critical structures: As well as hitting the intended target, proper injection must avoid hitting nerves, blood vessels, and other critical structures. By visual inspection, it is impossible to project the site of vessels, nerves, or other structures that are in the path to the target muscle and that should be avoided.
-
6.
Patient positioning: When estimating a muscle’s location, most physicians rely on one or more of the available anatomic reference guides [5,6,7]. The majority of these guides were developed for use in diagnostic electromyography, not for botulinum toxin or other chemodenervation procedures. These guides require that the patient’s limb be placed in a specific position, often the standard anatomic position. When treating patients with movement disorders or spasticity, it is often difficult or impossible to position patients as described in the book, limiting the accuracy of the guides’ recommended position for needle insertion.
Caveats: A thorough knowledge of anatomy is mandatory for all physicians who perform BoNT injections or other chemodenervation regardless of what supplemental technique may be used, as anatomy serves as the basis for utilizing other targeting techniques . Most physicians and all of the toxin manufacturers recommend supplemental guidance along with anatomic assessment when guiding most BoNT procedures. Neurolytic chemodenervation procedures with phenol or denatured ethyl alcohol should not be performed without guidance with E-Stim or E-Stim + US.
Electromyography /EMG Guidance
EMG is the most commonly reported or recommended localization techniques for BoNT injections involving muscle targets [2, 12,13,14,15,16]. EMG guidance requires equipment either a standard electrodiagnostic machine, EMG amplifier, or combined EMG amplifier-E-Stim unit as well as insulated (usually Teflon-coated) injecting needle electrodes of the appropriate length to reach the intended target muscle or muscles and ground and reference electrodes (Fig. 2a–c).
When using EMG to guide BoNT injections , the patient should be situated comfortably both to provide easy access to the muscles and facilitate a relaxation in the target muscle groups. The steps in identifying the optimal site for the needle electrode insertion using anatomic localization include inspection, measurement, and palpation with or without performing PROM or AROM of the muscle. The area of the body to be injected is exposed to reveal the region of interest and the patient positioned to allow access to this region. Proper positioning typically requires the assistance of other staff especially for patients who have significant spasticity, involuntary movements, or ROM limitations, as well as for those who have difficulty cooperating or following directions. If many muscles are to be injected, the patient should be carefully repositioned to optimize each injection site. Once the patient is positioned, the reference and ground electrodes are placed; the insulated injection needle serves as the active electrode.
The skin over the selected site is then disinfected and the needle electrode is inserted through the skin and advanced to the target while listening for audible EMG activity. Insertional activity will be heard when the needle enters the muscle. Insertional activity is then followed by a tonal change from a low, dull pitch to the crisp high frequency of motor unit action potentials (MUAPs) , which confirms that the electrode is in an actively contracting muscle. If the tone remains dull (i.e., low frequency), the needle position should be adjusted, advanced, or redirected until a high frequency “crisp” tone is obtained.
If possible, the patient should be instructed to relax completely, then to voluntarily contract the target muscle. This facilitates muscle localization as the injector can hear the muscle interference pattern with voluntary activation of the target muscle, but there should be no sound (or only the sound of distant motor units) with activation of surrounding muscles.
EMG alone can be effective in localizing muscles for BoNT procedures if the patient is able to simultaneously contract the target muscle and relax adjacent muscles, even those with a similar action and/or antagonist muscles. This approach, however, may be difficult or impossible for many patients with spasticity or secondary dystonia due to impaired selective motor control and/or co-contraction or mass synergies [17]. For example, when targeting the flexor carpi radialis (FCR) for BoNT in a patient with post-stroke spasticity (PSS) , co-contraction may be present in other forearm muscles making it impossible to determine in which of the simultaneously firing muscles (flexor digitorum superficialis (FDS), pronator teres (PT) , or flexor digitorum profundus (FDP) ) the needle electrode is located. In this situation, it may be possible to ascertain the position of the needle by PROM of the target muscle, as stretching the muscle may elicit increased firing. Similarly, careful inspection of the patient’s abnormal posture may also help determine which muscle the needle is in. However, many physicians faced with this situation would choose E-Stim (E-Stim) to guide the BoNT procedure rather than EMG [15, 18].
Advantages and Limitations of EMG for BoNT Procedures
-
1.
Identification of over-contracting muscles: The primary advantage of EMG is that it provides feedback (auditory or visual, depending on the equipment used) indicating the level of activity or overactivity in a muscle. It is particularly useful in patients with complex patterns of cervical dystonia (CD) or limb dystonia where EMG can demonstrate whether a muscle is actively firing when it should be at rest and thereby contributing to the abnormal head, neck, or limb posture [19, 20].
-
2.
Fine or discrete localization: In focal hand dystonia, there is often dystonic contraction of just part of a larger muscle. Such patients may have, for example, flexion in a single finger, indicating dystonic involvement of just one fascicle of the FDS or FDP. Thus, in limb dystonia, EMG is useful when it is important to isolate individual muscle fascicles for injection.
Limitations
-
1.
Inadequate familiarity with EMG procedures and EMG equipment: The use of EMG requires training for safety and proper use of the equipment. The need for training can be minimized by using commercially available audio EMG units without stimulation capability. Inexpensive units are widely available, so that cost is not a major limiting factor.
-
2.
Factors limiting accuracy: The accuracy of muscle localization by EMG is limited by;
-
(a)
Co-contraction and muscle synergies
-
(b)
Loss of reciprocal inhibition, leading to diffuse activation of multiple muscles including co-contraction of agonists and antagonists.
-
(c)
Loss of EMG signal when patients are sedated for BoNT injections, particularly if general anesthesia is used.
-
(a)
-
3.
Not always needed: EMG is not generally used for chemodenervation of orbicularis oculi in patients with blepharospasm or many of the thin, superficial muscles of facial expression.
-
4.
Non-muscle targets: EMG is not helpful for localizing non-muscle targets such as glands for sialorrhea or hyper-secretory disorders.
-
5.
Blind insertion: EMG uses blind insertion of the needle that may penetrate vessels, nerves, organs, or other structures in the path to the target muscle.
-
6.
Pain/discomfort: Patients often report more pain with the insertion of insulated needle electrodes than with standard hypodermic needles.
-
7.
Cost: Insulated needle electrodes are more costly than hypodermic needles.
Caveats: When considering BoNT treatment for muscle overactivity, EMG can provide useful information related to the level of activity in a muscle. EMG is likely more useful in patients with focal dystonia than in those with spasticity. Some of the limitations of EMG guidance can be resolved by carefully selecting the patient in whom EMG will be used and combining EMG with other guidance, such as E-stim or US. US has the advantage of reducing the risks of blind needle insertion and can be combined with EMG-guided procedures.
Electrical Stimulation (E-Stim)
E-Stim is an EMG technique whereby the muscle with the needle in place is stimulated through the injection EMG needle. It is used or recommended by many clinicians who perform chemodenervation procedures including BoNT injections and neurolytic procedures (such as phenol or ethyl alcohol nerve/motor point blocks). We consider E-Stim to be required for all neurolytic procedures or diagnostic nerve blocks. E-Stim is only useful for BoNT injections of muscle targets and is not informative when injecting glands or non-muscle targets. Similar to EMG, E-Stim may not be required or useful when treating the orbicularis oculi in blepharospasm or other superficial muscles of face. When performing neurolytic chemodenervation procedures (with phenol or denatured ethyl alcohol), the physician has several options including performing a motor nerve or nerve trunk block, motor nerve branch block, or motor points/motor endplate blocks (MoEPs) [15, 21]. When the motor nerve trunk or motor nerve is targeted for neurolysis, all of the muscles innervated by that nerve trunk or nerve will be affected by the block. Motor branch blocks are more selective than nerve trunk blocks and can allow targeting of specific muscles and/or fascicles with MoEP targeting being the most selective E-Stim localization technique. E-Stim localization can help guide the injector to the selected level of neurolysis, from broad nerve trunk blocks of multiple muscles to MoEP blocks resulting in focal treatment of a muscle or muscle fascicle. E-Stim is similarly helpful when performing BoNT chemoneurolysis in muscle targets.
E-Stim guidance for neurolysis or BoNT chemodenervation procedures requires either a small hand-held stimulator (Fig. 2c, d) or an electrodiagnostic instrument (Fig. 2a), ground and reference electrodes, and insulated injecting needle electrodes of a length appropriate for the estimated muscle or nerve depth and the trajectory of the needle insertion.
When using E-Stim) guidance to determine the best site for needle insertion, physicians typically use published information for muscle anatomy from reference guides, nerves from anatomy texts or atlases, and MoEPs from published studies/information (see section in this chapter on MoEP targeting) [5, 6, 8]. The area of the body to be injected is then exposed to reveal the region of interest and the patient positioned to allow access to this region.
Proper positioning typically requires the assistance of other staff, especially in patients who have significant spasticity, involuntary movements, or ROM limitations as well as in those who have difficulty cooperating or following directions. If many muscles are to be injected, the patient should be carefully repositioned to optimize each injection site. Once the patient is positioned, the reference and ground electrodes are placed; the injection needle serves as the active electrode. With the site for needle insertion identified, the skin is cleaned or disinfected using the physician or institution’s standard protocol and the needle is inserted through the skin and advanced toward the target. US guidance can be used in combination with E-stim to allow continuous visualization and to avoid blind insertion. When the physician estimates (or visualizes with US) that the needle is near the nerve or within the muscle target, the stimulator is turned on starting at a low intensity. The intensity of stimulation for intramuscular injection is gradually increased until there is a visible muscle twitch or joint movement, typically at an intensity of 1–3 mA. The needle can be maneuvered so that successive reductions in stimulation intensity continue to produce a maximum twitch in the desired muscle. Once the needle is in the proper position, the injection then proceeds. If the needle is not at the desired target, it is then advanced, redirected, or repositioned and stimulation repeated until positioning is correct. When performing motor point blocks, the stimulation intensity required has been reported to be at 0.25–0.5 mA [15]. If upon stimulation, contraction occurs in several muscles or a muscle other than the target, the clinician should reposition the needle to isolate the target muscle. Care must be taken to avoid overstimulation which may lead to volume conduction and false localization.
Advantages
-
1.
E-Stim produces a direct visual feedback via muscle twitch and/or joint movement confirming that the needle is likely to be within the target muscle.
-
E-Stim provides more reliable information about the location of the needle than voluntary contraction, especially in patients where co-contraction, mass synergy, or impaired motor control) limit their ability to isolate a muscle for contraction, thereby limiting the utility of EMG.
-
E-Stim can be used when patients are sedated, whereas the EMG is attenuated or absent with sedation.
-
-
2.
E-Stim can be used to isolate thin muscles (e.g., rectal sphincter) which may be difficult to isolate with EMG.
-
3.
E-Stim may be helpful in isolating deep or overlapping muscles where it is difficult to palpate the muscle or estimate its precise location or depth.
-
4.
Studies have shown that E-Stim is more accurate than manual needle placement [22, 23].
Disadvantages
-
1.
Inadequate familiarity with E-Stim procedures and E-Stim/EMG equipment: The use of E-stim requires training for safety and proper use of the equipment. Inexpensive units are widely available, so that cost is not a major limiting factor. Performing E-Stim correctly also requires a certain amount of skill to avoid localization errors. Localization errors with E-stim may occur through;
-
(a)
Volume conduction: When excessive current is used by turning the stimulator intensity up too high, the area or zone of depolarization is enlarged. This may lead to stimulation of and twitch in a muscle distant from the stimulating needle electrode. In this situation, the physician may falsely conclude that the needle electrode is in the target muscle when it is located outside of the muscle or in another muscle. Such false localization may lead to an unwarranted conclusion of treatment failure or the need to increase toxin dose, weakness in an untargeted muscle, and/or other adverse events.
-
(b)
Placement by a nerve: When the stimulating needle electrode is outside the target muscle but adjacent to the motor nerve branch innervating the muscle, stimulation will lead to a visible twitch even though the needle tip is outside of the intended muscle target for injection.
-
(a)
-
2.
Pain and prolonged procedure: The current from electrical stimulation can be quite painful. Pain is minimized by using the lowest stimulation intensity required to produce a twitch in the muscle, typically not exceeding 3mAmp [15, 24]. The use of E-stim can prolong procedure time compared to manual placement or EMG ([18, 19, 23, 25]; Alter et al. 2010).
-
3.
Possible need for sedation: Most, if not all children, will require sedation which increases the;
-
(a)
Risk of the procedure especially in medically fragile patients.
-
(b)
Time and cost of the chemodenervation or neurolysis procedure.
-
(c)
Time away from school or work for the patient and/or family members/caregivers
-
(a)
Caveats: The current level of evidence suggests that E-Stim is more accurate than EMG, particularly when treating patients with spasticity or generalized dystonia. E-Stim is required for all nerve blocks and neurolytic procedures and can be combined with US to further increase the accuracy of muscle or nerve targeting .
Motor End Plate Targeting or Localization Technique
BoNTs exert their action in muscle at the neuromuscular junction, found at the motor end plate (MoEP) . Therefore, physicians and researchers have questioned, suggested, and investigated whether MoEP targeting can increase toxin uptake into the target muscle and hence the clinical efficacy or, by being provided at the site of action, reduce the required effective dose of BoNT [26,27,28,29]. The location of MoEP or end plate zones in animal models and in humans has been studied both by histochemical staining and electrophysiological methods [28, 30,31,32]. Coers described three arrangements of MoEP in human muscles: (1) a single innervation band, (2) multiple innervation bands, and (3) innervation bands scattered throughout the muscle [31]. Christensson reported that the MoEP in stillborn infants were arranged as a single transverse band at the midpoint of unipennate muscles and in a concave band in bipennate muscles such as the gastrocnemius [30].
More recent anatomical studies detail the location of MoEP in various lower and upper limb muscles [21, 29, 33,34,35]. In particular:
-
Posterior calf muscles: In the medial and lateral gastrocnemius and soleus muscles, Kim et al. reported that the MoEPs are arranged along the length of the muscle with the most;
-
Proximal MoEPs in the medial gastrocnemius, lateral gastrocnemius, and soleus at 9.6% (+/− 3.5%), 12.0% (+/− 3.4%), and 20.5% (+/− 3.9%) of calf/leg length, respectively [34].
-
Distal MoEP were reportedly located at 37.5% (+/− 5.5%), 37.9% (+/−2.3%), and 46.7% (+/− 3.6%) of lower limb length, respectively [34].
-
-
Biceps brachii: MoEP are arranged in the muscle in an inverted V [33] with the MoEP zone location in cm and as a ratio of olecranon-acromion length as follows;
-
1 cm in width
-
7 cm proximal to the olecranon, laterally with a MoEP zone ratio of 0.25
-
11 cm proximal to the olecranon, midline with a MoEP zone ratio of 0.39
-
8 cm proximal to the olecranon, medially with a MoEP zone ration of 0.28
-
-
Psoas Muscle: In a 2010 cadaver study, Van Campenhaut et al. published information on the number, location, and distribution of MoEP in the psoas muscle of adult cadavers.
-
The psoas muscle was made up of converging muscle fibers of variable lengths
-
An average of 3.7 (range 2–7) nerve branches from the lumbar plexus innervated the psoas muscle along its length.
-
That the majority of MoEPs were located proximal to the sacral promontory and were distributed between 30.83%–70.25% of the distance from T12 to the inguinal ligament [35].
-
MoEP targeting procedure for BoNT injections: MoEP targeting techniques generally require EMG, E-Stim, or US guidance methods and include;
-
The use of published reference data on motor point location and/or distribution combined with anatomic, EMG, E-Stim, or US guidance for BoNT injections.
-
With EMG, the location of the needle at the MoEP is identified by hearing the distinctive sound referred to as endplate noise and injecting toxin in this zone/location [26].
-
If using a diagnostic EMG unit with a visual display, MoEPs can be targeted by adjusting the needle position within the muscle until the initial deflection of all the motor unit action potentials recorded by the needle electrode is negative [36].
-
If using E-Stim, MoEP are targeted by repositioning the needle and reducing the stimulation intensity until the maximal visible muscle twitch is present with minimal intensity [21].
-
While the resolution of current US transducers does not allow direct visualization of MoEPs, US can be used to place the needle accurately in the zone of the published location of MoEPs in the target muscle [37].
Advantages of MoEP Targeting
-
1.
Ease of use: MoEP targeting is easily incorporated into BoNT procedures regardless of what other guidance technique used in addition to anatomic localization.
-
2.
Ease of localization: The published information on the location and distribution of MoEPs in many commonly targeted muscles are easily accessed.
-
3.
Potential increased benefit: Studies suggest that utilizing MoEP targeting may reduce the required effective dose and/or improve outcome following BoNT injections [21, 29].
Limitations of MoEP Targeting
-
1.
Lack of data on MoEPs: Maps of the location and distribution of MoEP are not available for all muscles
-
2.
Longer procedure: Utilizing electrophysiological means of MoEP targeting (EMG, E-Stim) may increase the time required to perform the BoNT injection procedure.
-
3.
Lack of applicability for all BoNT uses: MoEP targeting cannot be used for non-muscle targets.
Caveats: MoEP targeting may be a useful addition to traditional guidance techniques, resulting in improved outcomes and reducing the required effective dose. Many clinicians advocate for or recommend using MoEP targeting for BoNT injections [21, 26, 27, 38], but the data comparing other targeting techniques with and without the use of MoEP is limited.
Imaging-Based Guidance
Fluoroscopy and Computerized axial tomography (CT): While fluoroscopy and CT have occasionally been reported as an option to guide chemodenervation procedures [39,40,41,42,43,44,45], the use of these techniques is limited by;
-
Inconvenience: Inconvenient access to and cost of the radiographic imaging equipment may take these procedures out of the office, making them unfeasible for most BoNT injections.
-
Cost and time: These procedures add substantial cost and time to chemodenervation procedure
-
Repeated exposure to ionizing radiation: Given that chemodenervation sessions are frequently repeated at 3–4 month intervals over years, the risks associated with repeated exposure to ionizing radiation are significant, especially in children.
Ultrasound (US): US is the most common imaging-based guidance technique for chemodenervation procedures including BoNT. Its increasing use is related to a number of factors including;
-
Convenience: The portability, accessibility, and relatively low cost of US equipment, making office US feasible
-
Safety: US does not expose patients to ionizing radiation. There are no identified safety concerns with frequent or repeated exposure to muscle or other US for chemodenervation.
-
Cost: US entails lower cost when compared with fluoroscopy or CT guidance
-
Patient comfort: US entails minimal patient discomfort. Patients quickly become familiar with US and readily accept its use.
Ultrasound Guidance for Chemodenervation Procedures
In the last decade, the development of small portable US machines, high frequency linear transducers, physician familiarity/training, and the recognized utility of US for procedural guidance has increased the use of US guidance for invasive interventions including chemodenervation procedures [19, 39, 40, 42, 46,47,48,49,50,51,52,53,54,55,56]. US has an advantage over electrodiagnostic techniques (EMG/E-stim) as it is useful not only for identifying muscle targets, but it can also be used for injections of BoNT into non-muscle targets such as salivary glands or prostate as well as for diagnostic or neurolytic nerve blocks [57, 48].
US guidance for chemodenervation procedures requires an ultrasound instrument (Fig. 2e, f), linear, curvilinear and/or specialty transducers (for prostate injections) of various frequencies (typically 3–17 MHz) (Fig. 2g), gel, transducer covers (if desired), hypodermic needles of various lengths (1–2.5 in., 30–25 g) as well as injection, equipment cleaning, and maintenance supplies. If combining US guidance with EMG or E-Stim, a portable EMG amplifier or combined portable EMG-E-Stim unit, insulated injecting needle electrodes of various lengths, and associated supplies are also required. Additional information on US equipment can be found below.
Basic physics for US Scanning: The following section provides a brief review of US physics and imaging. For additional information , readers are referred to several book chapters or articles which review these topics in more detail [39,40,41,42, 49, 58].
Piezoelectric Crystals
The high-resolution images obtained with US scanning are made possible by piezoelectric crystals, devices which are responsible for converting electrical pulses into mechanical vibrations and vice-versa. Piezoelectric crystals are placed into arrays within a transducer, the device used for US scanning. When the transducer is placed in contact with the patient, some of the mechanical vibrations or sound waves generated by the piezoelectric crystals are transmitted through the patient’s skin. These sound waves are then transmitted through superficial tissues and on to deeper structures within the body where they are either scattered, refracted, or reflected at tissue interfaces. Those mechanical sound waves reflected back to the transducer are then converted back to electrical pulses by the piezoelectric crystals, transmitted to the US machine, and processed into real-time grey scale images visualized on the display screen using a time-distance co-efficient [58].
Transducer /Ultrasound Frequency
The frequency of the sound waves generated by the piezoelectric crystals within the transducer determines image resolution and the depth of penetration of the generated US waves. The frequency of the sound waves emitted by a given transducer thus determines the structures that can be visualized when scanning. High-frequency sound waves (12–18 MHz) have a higher sampling rate permitting improved lateral resolution and thus better discrimination of adjacent structures. However, while higher US frequency provides better resolution, this is at the expense of reduced depth of penetration of the US waveforms. Soft tissues (muscles, adipose tissue, glands, etc.) absorb the high-frequency US waves, leaving fewer waveforms available to travel onto deeper structures compromising imaging of these deep structures. Lower frequency (3–5 mHz) US waves travel through soft tissues, allowing them to penetrate to deeper structures, but the images created will have a lower resolution and appear grainer due to reduced lateral resolution. To at least partially mitigate these limitations , commercial US transducers all emit a mix of sound wave frequencies (15-4, 5-3 MHz etc.), which allows imaging of tissues at various depths [41, 58]. However, it remains important that the sonographer chose a transducer with the frequencies providing adequate visualization of the target and nearby structures in the region of interest.
Sonoacoustic Properties of Tissues
The impedance of and speed of sound waves in tissues determines their sonoacoustic appearance, i.e., echogenicity or US appearance (Figs. 1a, b, 3a, 4a–c, 5a, b, 6a, b, and 7). When sound waves travel through the body and encounter tissue interfaces of differing acoustic impedances, sound waves are reflected, refracted, or scattered off these interfaces [58, 59]. If only a few sound waves are reflected back to the transducer, then the image on the screen will be dark or hypoechoic (Figs. 1a, b and 3a). If a tissue interface is highly reflective of US, then most of the waveforms are reflected back to the transducer and the image will appear bright or hyperechoic (Figs. 1a, b and 3a). Tissues with higher water content are relatively hypoechoic . Those with low water content and those with a higher content of fibro-connective tissue or calcium (bone cortex) will appear hyperechoic [59] (Figs. 1a, b and 3a). Sound wave cannot penetrate all tissue types, for example bone, and therefore structures deep to these tissues cannot be visualized with US. This is one of several important imaging issues or artifacts that are encountered with US imaging which include;
-
Posterior acoustic shadow; as noted above, this artifact occurs when US waves encounter a tissue that reflects all of the sound waves (bone, metal) preventing the US from travelling through this tissue and onto tissues below the structure. The reflection of all the sound waves by these US mirror like structures leads to an anechoic area or shadow deep to these tissues [41, 58, 59] (Fig. 1b).
-
Posterior acoustic enhancement; this artifact is encountered when imaging a tissue that is located deep to a fluid-filled structure, such as a cyst or full urinary bladder. In this circumstance, the majority of the sound waves encounter minimal or no resistance and travel through the fluid-filled structure and then onto the deeper tissues. As a result, more of the sound waves reach the deeper structures, making the deeper tissues underlying fluid-filled structures appear artifactually bright or hyperechoic [41, 58, 59] (Fig. 3b). When performing fetal US, obstetricians take advantage of this fluid artifact and scan the fetus through a full bladder which enhances visualization of the fetus
-
Anisotropy; is a characteristic of some types of tissue (including tendons and nerves) whereby the appearance of the tissue on US is affected by the incidence angle of sound waves relative to the tissue [58]. When US waves are perpendicular to a tendon, the tendon fibers will appear highly echogenic or hyperechoic. If the same structure is imaged with the transducer positioned where the incidence angle of the sound waves is at less than 90°, the structure will appear artifactually hypoechoic (Figs. 4a and 5b). This artifact is important when performing diagnostic US because an inexperienced clinician may conclude that a hypoechoic tendon represents a partial or full thickness tear of a tendon when in reality the structure is intact and only appeared hypoechoic because it was not imaged at 90°. Anisotropy is useful, however, as it can be used to help distinguish various tissues from one another. For example, nerves which are less anisotropic can be differentiated from tendons which are highly anisotropic (Fig. 5a, b).
As noted above, tissues are described by their sonoacoustic properties including their internal echo-texture and relative echogenicity. Most organs and structures in the human body are comprised of several tissue types, for example, a muscle is comprised of the surrounding fascia (highly echogenic/hyperechoic), contractile elements/fascicles (hypoechoic), and intramuscular connective tissue/tendons (hyperechoic) (Figs. 1a and 6a, b). In contrast to muscle, glandular tissues such as salivary gland or thyroid are homogenous in composition, with a resulting uniform grey-scale echotexture sonoacoustic appearance with US imaging [58, 59] (Fig. 7).
The appearance of some tissues, like muscle or nerve, will vary with the scanning plane, i.e., in whether the transducer is placed longitudinally vs. transversely on the skin over the structure. For example, when scanned with the transducer placed parallel to the longitudinal plane of the muscle, muscle has the appearance of long, thin, hypoechoic bands (contractile fascicles) that are surrounded by or interspersed with linear hyperechoic bands (non-contractile fibro-connective tissue/intramuscular tendons) (Fig. 6b). In contrast, in a transverse view, muscles have a speckled appearance, representing the internal mix of hypoechoic contractile fascicles and hyperechoic and hyperechoic intramuscular connective tissue (Figs. 1a, b and 6a). On B-mode scans, blood vessels will appear hypoechoic, tendons are highly echogenic/hyperechoic and fibrillar, whereas nerves have a more mixed hyperechoic, hypoechoic appearance [59] (Figs. 5a, b and 6b).
US Procedural Guidance Techniques for BoNT Injections: As with other instrumented guidance techniques, an US-guided BoNT procedure begins with a physical examination, including evaluation of muscle tone and a functional assessment, external inspection of the body part to be treated (including skin integrity), palpation, PROM and AROM to identify which are the optimal targets for injection. The area of the body to be scanned/injected is then exposed to reveal the region of interest and the patient positioned to allow access to this region. Proper positioning typically requires the assistance of other staff, especially for patients who have significant spasticity, involuntary movements, or ROM limitations as well as for those who have difficulty cooperating or following directions. The patient and the examination or treatment room should be set up in a manner that permits the injector to access both the patient and US machine controls and transducers, with an unobstructed view of the US screen. The room may need to be darkened so that the screen images can be seen more easily.
Once the US machine is turned on, the patient data is entered (this is required on most machines in order for still or video cine-loops to be saved). Most machines have preset parameters for imaging different tissues or body territories. Before staring the US examination, the injector should assure that the correct machine preset is selected, such as that for musculoskeletal, gland, or nerve. This is accompanied by selection of the most appropriate transducer for scanning the region of interest (which should be the transducer of the highest frequency which provides an adequate field of view/depth). The sonographer must adjust various machine settings to optimize imaging including [49] adjustment of the
-
Scanning Mode: B or Brightness Mode, Color Doppler, Power Doppler.
-
Depth.
-
Number of and position of focal zones.
-
Overall gain.
B-mode and Color Doppler are the most commonly used scanning modes for US-guided chemodenervation procedures. B-mode scanning provides real-time grey scale images of structures and continuous visualization of the
-
Target.
-
Structures to be avoided.
-
Needle.
-
Toxin or other injectate as it is injected.
Color Doppler is useful in identifying blood vessels in the field of view, differentiating arteries from veins and in discriminating vessels from large nerve trunks so as to avoid these non-targets when inserting the needle and directing it into the muscle (Fig. 8a, b).
After cleaning the transducer , gel is applied to the transducer to reduce impedance to sound waves at the air/skin interface, thereby enhancing sound transmission through the skin. The transducer, with an adequate layer of gel, is placed in contact with the patient’s skin and the sonographer scans the region of interest in transverse and longitudinal imaging planes (Fig. 9a, b) to determine the depth, location, and safest path to the target. The US beam emitted from the transducer is only 1–2 mm wide, approximately the width of a credit card and therefore only a small slice of the region of interest is visualized if the transducer remains in a static position [41, 58]. To scan the entire region of interest (including the target, structures to be avoided, and path to the target) the entire region must be scanned thoroughly by dynamic imaging. This is accomplished by using different scanning planes/transducer orientations and by moving the transducer in various directions over the region of interest.
Muscles are identified based on their position in the body (based on an understanding of anatomy), and based on their unique pattern, i.e., recognition of each muscle’s characteristic shape, contour lines and relationship to identifiable nearby structures such as bones, nerves, vessels, or other muscles (Figs. 1a, b and 6a, b). Identification of muscles on US can often also be verified by observing muscle contraction on US with voluntary contraction by the patient, for those who are able to selectively activate muscles.
Once the muscle’s or target’s position and depth have been identified, the physician chooses the most appropriate needle and injection technique . There are two techniques for needle insertion when utilizing US guidance; in-plane (Fig. 10a) or out-of-plane (Fig. 10b) [60]. For the in-plane technique, the needle is inserted down the length of the transducer and the entire needle, including the needle tip, is visualized (Fig. 10a). In contrast, when using an out-of-plane technique , the needle is inserted across the short axis of the transducer and the needle is scanned in cross-section and therefore is visualized as a hyperechoic dot (Fig. 10b). Since the entire needle is scanned in cross section, it appears on the screen as a hyperechoic dot along its entire length, including the tip. Because the entire needle cannot be visualized when using an out-of-plane technique, physicians must use a “walk-down” technique to track the needle to the target [37, 41, 42, 60]. This is accomplished by inserting the needle through the skin, then advancing the needle in very small, brief rapid increments, similar to the technique used when listening for insertional activity during a diagnostic EMG. When using the walk-down technique, the physician should closely observe the movement of the needle through the tissues as it passes from superficial to deep. Once the target muscle or structure is reached, the toxin is injected. To distribute the toxin throughout the muscles or targets, the needle may be repositioned under US guidance to allow for multiple injection sites.
Equipment : Performing US-guided BoNT injections requires an US machine. Machines are available with a range of features, resolution, and portability (Fig. 2e, f). A portable US machine is sufficient for most office-based chemodenervation procedures. If possible, a variety of linear or curvilinear transducers should be available to accommodate imaging the few range of muscles and structures that may require injection. Linear or curvilinear 5-3 MHz transducers are used for the most deeply situated muscles, transducers with a frequency range of 12-5 MHz are used for less deeply seated muscles, and 18-7 MHz transducers are utilized for the most superficial muscles or structures, as well as when scanning small, thin children. A hockey stick linear transducer with a small footprint is frequently best for imaging irregular surfaces such as the hand, in small patients, and for salivary gland injections.
Other supplies for scanning include ultrasound gel (sterile, non-sterile), sterile transducer covers if needed, a manufacturer’s approved transducer cleaner, and tissues or towels to remove the gel after the procedure is completed. The use of sterile transducer covers is typically reserved for sterile procedures such as joint injections (including BoNTs) and for joint aspirations. There is no standard recommendation for the use of a non-sterile transducer cover when performing chemodenervation procedures. While some physicians use non-sterile transducer covers for all injections, others rarely or never use these covers when performing chemodenervation procedures [17, 40].
Supplies for injection included syringes, hypodermic needles of narrow gauge, and various lengths. If performing simultaneous US and EMG or E-Stim, then monopolar-insulated injection electrodes, surface needles, surface electrodes, and an EMG machine, EMG amplifier, or E-Stim unit are also required. It is important to note that alcohol-based products must be avoided when cleaning US transducers as these products will damage the transducer membrane and void the product warranty [37, 49].
Advantages and Limitations of US to Guide BoNT Injections
There are a number of advantages and disadvantages or limitations to the use of US guidance for chemodenervation procedures including BoNT injections [17, 37, 39, 41, 42].
Advantages
-
US provides a detailed view of the location and depth of the target, structures to be avoided, and the safest path to injection target to avoid penetration or injection of un-intended targets.
-
It also allows the needle to be tracked to the target and visual confirmation of the location of the injectate.
-
During the procedure, the volume of injectate can be visualized and needle position adjusted to prevent excessive volume administration at any one site.
-
When performed by an experienced clinician, US may speed localization of the target.
-
US scanning is painless and requires no ionizing radiation.
-
Standard hypodermic needles may be used for US-guided procedures, which may be less painful than insulated monopolar-injecting electrodes.
-
Watching the US screen provides a helpful distraction during the procedure for some patients.
-
Pediatric patients may require no sedation for US-guided BoNT procedures.
Disadvantages of US Guidance for BoNT Injections
-
US machines may be costly, which may be a barrier to acquire this equipment.
-
The hands-on training required to become proficient in US-guided chemodenervation procedures may be inaccessible, expensive, or require time away from one’s medical practice.
-
There may be a steep learning curve when learning US guidance skills and pattern recognition of the relevant structures.
-
Until one becomes proficient, the use of US may increase the time required for these procedures.
-
While US provides very accurate information about the location of the target and position of the needle, it generally does not provide information on the activity level of a muscle target and therefore whether it is contributing to the patient’s disability and requires injection. US may need to be combined with EMG to provide the information related to muscle activity.
-
US guidance alone is not adequate for nerve or motor point blocks. US used with E-Stim is recommended for these procedures [48].
Caveats: Of the available guidance techniques for chemodenervation procedures, US guidance provides the most anatomically correct information about the location, depth of the target, structures to be avoided, and the safest path to the target.
Guidance Techniques for BoNT Procedures, What Is the Evidence?
Studies Comparing Guidance Techniques
There are a limited number of large and well-controlled trials comparing head-to-head the accuracy or efficacy of all of the available guidance techniques . However, there is an increasing body of literature from high-quality controlled and blinded trials comparing the accuracy and/or efficacy of two or three of the available techniques. All studies, to date, which compared the accuracy of needle placement or outcomes of chemodenervation procedures concluded that procedures guided solely by anatomic means are less accurate and/or less effective than when instrumented guidance techniques of EMG, E-Stim, or US are utilized. The following is a selective review of the available studies:
-
Anatomic guidance vs. EMG for Limb Muscles : A 2013 randomized controlled trial (RCT) of 27 adult patients with spasticity from an upper motor neuron syndrome (brain injury or spinal cord injury) compared the efficacy of BoNT injections in upper and lower limb muscles guided by anatomic landmarks to injections with EMG guidance [20]. Outcome measures included spasticity rated using the Modified Ashworth Scale (MAS) and a functional outcome assessment using the Modified Barthel Index. Although spasticity and function were improved in all subjects, the degree of improvement in both outcome measures was lower in the group where the injections were based on only anatomic guidance. The authors concluded that EMG guidance was superior to anatomic guidance for BoNT procedures in limb muscles. A 2002 study of adults with focal hand dystonia study compared the accuracy of needle placement by either EMG or anatomic techniques. The authors concluded that EMG was superior to anatomic methods in assuring injection into selected muscles [2].
-
Anatomic Guidance vs. EMG for Cervical Dystonia : A 2016 RCT compared the outcome of injections using EMG guidance to injections based on palpation for adult patients with cervical dystonia (CD) [61]. The patients in the group receiving injections guided by EMG had a greater improvement in the primary endpoint, Tsui score for CD, at 16 weeks. No between-group differences were noted in their secondary endpoints of pain on a visual analog scale (VAS) or on other secondary endpoints including the Hospital Anxiety and Depression Scale (HADS) and the Clinical and Patient Global Impression of Change (CGIC and PGIC). When comparing adverse events, the group injected with EMG guidance had significantly more injection site pain, but, importantly, significantly lower incidence of dysphagia than the palpation guidance group.
-
Anatomic guidance vs. E-Stim : A 2009 study in children with hemiplegic or diplegic CP compared the efficacy of BoNT injections guided either by palpation or E-Stim. At 3 months, patients who had injections guided by E-Stim had a statistically greater reduction in MAS scores and Composite Spasticity Scale scores and greater improvement in PROM and Gross Motor Function Measure (GMFM) than patients injected using manual guidance alone [62]. A 2005 study of 226 children with CP investigated the accuracy of manual needle for BoNT injections for 1376 needle insertions in upper and lower limb muscles [22]. Surface anatomy, depth estimated by limb size, and PROM were used for manual placement of the needle. Following manual placement, the position was evaluated using E-Stim with the inserted needle to see whether the muscle that twitched was the target or another muscle . The accuracy of manual placement was as follows: gastrocnemius-soleus 78%, hip adductors 67%, medial hamstrings 46%, tibialis posterior 11%, biceps brachii 62%, pronator teres 22%, flexor carpi radialis (FCR) 13%, flexor carpi ulnaris (FCU) 16%, and adductor pollicis 35%. Thus, the authors concluded that manual placement was adequately accurate only in the gastrocnemius. They postulated that inaccurate muscle targeting could be responsible, at least in part, for a lack of insufficient clinical response following BoNT injections in children with CP.
-
Anatomic placement checked by ultrasound in limb muscles : All of the studies, to date, comparing the accuracy and/or efficacy of manual needle placement to US guidance have concluded that US guidance is more accurate in limb muscles [54, 56]. The reported accuracy of manual placement in children with CP ranged from 46–64% in the lateral and 87–93% in the medial gastrocnemius [56], leading authors of the latter study to conclude that supplementary localization techniques should be considered for the medial gastrocnemius muscle in younger patients and for the lateral gastrocnemius for all patients. In another 2009 study of 54 children with CP, the authors evaluated the effect of a number of variables on the efficacy of lower limb BoNT procedures. The authors reported a greater efficacy of injections guided by US when patients were younger than 6 years of age or older than 12 years of age and when the hamstrings or gastrocnemii were targeted. The authors concluded that their study confirmed the usefulness of US guidance for BoNT injections in lower limb muscles [54].
-
Manual placement, E-Stim, and Ultrasound : A 2012 RCT evaluated the efficacy of a fixed dose and dilution of onabotulinum toxinA in the gastrocnemius muscle of 49 adult patients with PSS comparing three localization techniques, manual/anatomic placement, E-Stim, and US [19]. At 4 weeks after injection, the US guidance group had a greater reduction in MAS scale score than the manual guidance group. The US group also had a greater increase in PROM when compared with the E-Stim and manual injection groups. There was no significant difference in the Tardieu Scale score between the three groups. The authors concluded that, for PSS in the gastrocnemius muscles, US guidance for BoNT provided both a greater reduction in spasticity and greater clinical benefit than injections guided with manual needle placement or E-Stim.
-
Identifying Muscle Fascicle Location by Anatomic Reference Guides compared to US Localization : A 2010 study of patients with forearm flexor muscle spasticity assessed the location of forearm muscles and of individual muscle fascicles. The authors used published anatomic reference guides to estimate the location of the muscle or muscle fascicles and then identified the actual muscle or fascicle position using US. There were significant differences between the estimated position of the muscle or muscle fascicles when compared to position visible on US for the flexor carpi radialis (FCR) , flexor pollicis longus (FPL) , and for fascicles of the flexor digitorum superficialis (FDS) [52].
-
EMG vs. Ultrasound for Cervical Dystonia : In a 2012 study, Hong et al. assessed the incidence of dysphagia following BoNT injections guided by EMG compared to those guided by US. The incidence of dysphagia was 34.7% in patients where the procedure was guided by EMG and 0% in the same patients when the procedure was guided by US [53].
Cadaver studies assessing the accuracy of anatomic guidance for injections or manual needle or wire placement using EMG surface anatomy reference guides
-
Anatomic guidance checked by dissection : A 2012 study assessed the accuracy of palpation and surface landmarks to guide injections into the gastrocnemius muscles of 30 cadavers. Injections of ink, performed by 121 physicians, were followed by dissection [63]. The authors reported that 43% of the injections were within the target muscles and 57% of the injections were outside of the gastrocnemius, either in the soft tissue superficial to the muscle (19.8%) or in the soleus muscle deep to the target (37.2%).
-
A 2011 masked study compared “blind” (anatomic) versus US placement of a wire into 14 lower limb muscles in fresh cadavers. Two clinicians (a resident with 6 months of EMG training and an attending physician with more than 10 years of EMG experience) performed the needle insertions. The accuracy was then verified by CT and assessed by a third clinician [64]. The overall accuracy with anatomic guidance was 39% (range 0–100%), while the accuracy for US guidance was 96% (range 50–100%). When using anatomic guidance, the only muscles where wire placement was 100% accurate were the tibialis anterior and short head of the biceps femoris. Using US guidance, the only muscle targeted with less than 100% accuracy of wire placement was the semitendinosus muscle. Unexpectedly, the accuracy of blind anatomic wire placement was 0% for needle insertions into semitendinosus, rectus femoris, and extensor hallicus longus. Interestingly, there was no significant difference in the accuracy of needle placement between the less experienced and more experienced clinician. The only significant difference between the two clinicians was that the trajectory of the wire path towards the target was more accurate in the experienced clinician.
-
A 2003 study assessed the accuracy of wire placement during 263 insertions into 36 lower limb muscles using placement landmarks cited in three standard EMG anatomic reference books; those of Gieringer, Perotto, and Delagi. The wire insertions were performed by three physicians with varying degrees of EMG experience. The location was checked by anatomical dissection by an anatomist. The authors reported that 57% of wire insertions penetrated the target muscle, but that the tip of the wire was located in the target muscle in only 45% of attempts. There was significant variability in the accuracy of targeting for different muscles, ranging from 100% accuracy for vastus medialis to 0% for 12 attempts to place a wire in the hip flexors. The authors also studied the proximity of the wire to undesirable structures, with 17% of insertions either penetrating or passing within 5 mm of a nerve, tendon, artery, vein, or joint. The authors concluded that the accuracy of blind wire placement using EMG reference guides was quite variable and recommended that safer strategies be developed [51].
Systematic Reviews of Guidance Techniques for BoNT Injections
In recent years, several systematic reviews articles on chemodenervation specifically focused on guidance techniques or at least included information on them.
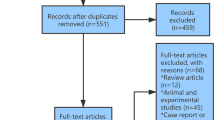
A 2016 systematic review of clinical trials reported on guidance techniques (anatomic, EMG, E-Stim, US techniques, motor end-plate targeting techinques), and toxin dilution [65] for limb spasticity injections. The authors identified 9 of 347 reported trials which met their inclusion criteria (all were RCTs comparing two or more BoNT injection techniques with use of similar doses of BoNT between groups; studies with adult participants (⩾16 years old) with upper and/or lower limb spasticity from various causes; studies with unrestricted methods of injection techniques which could include methods to localize, injection sites, use of different injectate volumes, selection of where to inject within muscles; English language studies). Injection methodology issues reviewed included injection localization technique, injection site selection, and injectate volume. The authors found level 1 evidence that US, EMG, and E-Stim are superior to manual needle placement (greater decrease in Modified Ashworth Scale (MAS), improvement in Tardieu Scale (TS), increase in passive range of motion). They also concluded that endplate targeting improved outcomes (MAS, TS, active elbow range of motion) compared to multisite quadrant injections in the biceps brachii and that injections using motor point localization in the gastrocnemius were equivalent in efficacy (MAS, TS, clonus scale, ambulation measure) to injections distal to the motor endplate. In their review of the effects of dilution, the authors reported that using a high volume was not more effective than delivering the same dose in a smaller volume in flexor forearm muscles.
Another study evaluating the effect of volume on the outcomes (mean rectified voltage, MAS, TS, Active ROM) of injections in the biceps brachii found no effect of volume when the site of the injections was non-selective. A third study of BoNT-A injections in the biceps brachii reported that high volume injections that were distant from the motor endplates were more effective (mean rectified voltage, MAS, TS, Active ROM) than low volumes closer to the endplates. When comparing adverse events with the various guidance techniques, eight of the nine studies reviewed reported no adverse events. One of the cited studies [20] reported transient post-injection pain in two subjects, one subject each in the EMG and manual placement groups [65].
In 2015, Grigoui conducted a systematic review of the impact of guidance techniques (anatomic, EMG, E-Stim, and US) on the effectiveness of BoNT injection for spasticity and dystonia [66]. Seven of their ten reviewed studies were RCTs. The authors concluded that there was;
-
1.
Level 1 evidence that instrumented guidance (EMG, E-Stim, US) was more effective than anatomic/manual needle placement for the treatment of cervical dystonia, upper limb spasticity, and spastic equinus in adults with post-stroke spasticity (PSS) and in children with cerebral palsy (CP).
-
2.
Level 1 evidence from three studies showing similar effectiveness of E-Stim compared to US for upper and lower limb PSS and spastic equinus due to CP.
-
3.
Level 2 evidence in focal hand dystonia (writer’s cramp): that while injections under E-Stim guidance were more effective than those using EMG, EMG-guided injections were associated with fewer complaints of weakness in adjacent muscles.
-
4.
Evidence from two studies supported that US-guided injections were more effective than those using E-Stim on two components of the Physician Rating Scale (PRS) including gait pattern at 1 and 3 months post-treatment and hind-foot position at maximum foot or floor contact during stance at 3 months post-treatment in children with CP and on ankle PROM in adults with PSS.
-
5.
In patients with PSS and children with equinus that there was poor evidence or no available evidence on injections with EMG or other instrumented techniques.
Based on their systematic review, the authors concluded that instrumented guidance for BoNT injections using E-Stim or US is strongly recommended for the treatment of spasticity in adults and children and additionally EMG for focal/cervical dystonia. US appears to be more effective than E-Stim for spastic equinus in adults with PSS.
In another 2015 article, (Walker et al. in 2015) the authors reviewed the available evidence for the impact of guidance techniques for BoNT injections including landmark-based anatomic guidance, EMG, E-Stim, and US. Based on their systematic review, the authors concluded that;
-
1.
Anatomic guidance in children and adults was the least accurate method of guidance.
-
2.
The available studies suggested that supplemental guidance with EMG, E-Stim, or US was all more accurate than anatomic guidance alone.
The authors also concluded that additional studies are required to determine which, if any, of the reviewed supplemental guidance techniques are the most accurate and/or lead to better clinical outcomes.
Consensus Statements and Practice Guidelines
In the 2016 American Academy of Neurology (AAN) Practice Guideline, Simpson et al. [70] reviewed the use of BoNT for various causes of muscle overactivity including blepharospasm, cervical dystonia, spasticity, and for headache. With regard to spasticity, the authors also reviewed reports of methods that aimed to optimize the response to BoNT, including dilution and guidance techniques. Based on their evidence-based systematic review of the data, the authors concluded that for upper limb spasticity, high volume/low potency injections and motor point guidance techniques were “probably effective” at enhancing tone reduction. When comparing E-Stim, EMG, and US, the authors found insufficient data to determine whether one technique was superior to another.
Wissel et al., in 2009, published the European consensus table for BoNT-A treatment of adult spasticity. The authors recommended that when the location of motor points is known, such as in the biceps brachii, this information should be used to target the injections into that muscle. The authors also concluded that when the sites of the motor points are not known or are known to be diffusely spread through the muscle, multiple injection sites should be considered. They noted that additional studies were required to determine the optimal localization method for BoNT chemodenervation procedures [67].
Heinen et al., in 2006, published the European consensus table for BoNT-A for pediatric patients. The authors recommended that injections in children should be performed using accurate localization techniques and that, in addition to the traditional methods of EMG and E-Stim, US could fine-tune localization of targets and would be painless [68].
Summary
Clinicians have a number of guidance techniques from which to choose when performing chemodenervation procedures including BoNT injections. Because of the limitations of and inaccuracy of relying solely on anatomic guidance for BoNT procedures, the majority of physicians now combine initial anatomic guidance with one of the available supplemental localization techniques, EMG, E-STIM, or US. The data from presently published studies indicates that US and E-Stim are superior to manual guidance in terms of accuracy and often in terms of outcome efficacy and also better than EMG for patients with upper motor neuron-related spasticity. The recognized advantages of US guidance over other instrumented techniques are that it provides direct visualization of the location and depth of the target, structures to be avoided, and infusion spread of the injectate. While US guidance provides the most anatomically accurate guidance method, additional studies comparing US to other instrumented techniques needed to determine or confirm whether its use provides additional advantages on, for example, improving efficacy or minimizing adverse effects.
References
Schwabe AL. Botulinum toxin in the treatment of pediatric upper limb spasticity. Semin Plast Surg. 2016;30(1):24–8.
Malloy FM, Shill HA, Kaelin-Lang A, Karp BI. Accuracy of muscle localization without EMG: implications for treatment of limb dystonia. Neurology. 2002;58(5):805–7.
Speelman JD, Brans JWM. Cervical dystonia and botulinum treatment: is electromyographic guidance necessary? Mov Disord. 1995;10:802.
Van Gerpen JA, Matsumoto JY, Ahlskog JE, Maraganore DM, McManis PG. Utility of an EMG mapping study in treating cervical dystonia. Muscle Nerve. 2000;23(11):1752–6.
Chu-Andrews J, Johnson RJ. Electrodiagnosis: a clinical and anatomic approach. Baltimore: J.B. Lippincott; 1986.
Delagi EF, Perotto AO, Daniel M. Anatomical guide for the electromyographer: the limbs and trunk. 5th ed. Springfield: Charles C Thomas; 2011.
Jost W, Klaus-Peter V. Pictorial atlas of botulinum toxin injection: dosage, localization, application. 1st ed. Hanover Park: Quintessence Publishing; 2009.
Lee J, DeLisa JA. Manual of nerve conduction study and surface anatomy for needle electromyography. Philadelphia: Lippincott Williams & Wilkins; 2004.
Walker HW, Lee MY, Bahroo LB, Hedera P, Charles D. Botulinum toxin injection techniques for the management of adult spasticity. PM R. 2015;7(4):417–27.
Sebastin SJ, Lim AY, Bee WH, Wong TC, Methil BV. Does the absence of the palmaris longus affect grip and pinch strength? J Hand Surg Br. 2005;30(4):406–8.
Thejodhar P, Potu BK, Vasavi RG. Unusual palmaris longus muscle. Indian J Plast Surg. 2008;41(1):95–6.
BOTOX® Prescribing Information Allergan. www.allergan.com/assets/pdf/botox_pi.pdf.
Dysport PI. [Package insert/prescribing information]. Basking Ridge: Ipsen Biopharmaceuticals, Inc. http://pi.medicis.us/printer_friendly/dysport.pdf.
Myobloc. [Package insert/prescribing information]. Louisville: Solstice Neurosciences (US WorldMeds). http://www.myobloc.com/hp_about/PI_5-19-10.pdf.
O’Brien CF. Injection techniques for botulinum toxin using electromyography and electrical stimulation. Muscle Nerve. 1997;S6:S176–80.
Xeomin PI. [Package insert/prescribing information]. Greensboro: Merz Pharmaceuticals. http://www.xeomin.com/files/Xeomin_PI.pdf.
Alter KE, Munin MC. Comparing guidance techniques for chemodenervation procedures. In: Alter KE, Wilson N, editors. Botulinum neurotoxin injection manual. New York: Demos Medical Publishing; 2014. p. 126–9.
Lim EC, Quek AM, Seet RC. Accurate targeting of botulinum toxin injections: how to and why. Parkinsonism Relat Disord. 2011;11(S1):S34–9.
Picelli A, Tamburin S, Bonetti P, Fontana C, Barausse M, Dambruoso F, Gajofatto F, Santilli V, Smania N. Botulinum toxin type a injection into the gastrocnemius muscle for spastic equinus in adults with stroke: a randomized controlled trial comparing manual needle placement, electrical stimulation and ultrasonography-guided injection techniques. Am J Phys Med Rehabil, 2012;91(11), 957–64.
Ploumis A, Varvarousis D, Konitsiotis S, Beris A. Effectiveness of botulinum toxin injection with and without needle electromyographic guidance for the treatment of spasticity in hemiplegic patients: a randomized controlled trial. Disabil Rehabil. 2014;36(4):313–8.
Gracies JM, Lugassy M, Weisz DJ, Vecchio M, Flanagan S, Simpson DM. Botulinum toxin dilution and endplate targeting in spasticity: a double-blind controlled study. Arch Phys Med Rehabil. 2009;90(1):9–16.
Chin TY, Nattrass GR, Selber P, Graham HK. Accuracy of intramuscular injection of botulinum toxin a in juvenile cerebral palsy: a comparison between manual needle placement and placement guided by electrical stimulation. J Pediatr Orthop. 2005;25(3):286–91.
Kwon JY, Hwang JH, Kim JS. Botulinum toxin a injection into calf muscles for treatment of spastic equinus in cerebral palsy: a controlled trial comparing sonography and electric stimulation-guided injection techniques: a preliminary report. Am J Phys Med Rehabil. 2010;89(4):279–86.
Gooch JL, Patton CP. Combining botulinum toxin and phenol to manage spasticity in children. Arch Phys Med Rehabil. 2004;85(7):1121–4.
Fehlings D, Narayanan U, Andersen J, Beauchamp R, Gorter JW, Kawamura A, Kiefer G, Mason M, McCormick A, Mesterman R, Switzer L, Watt J. Botulinum toxin-a use in paediatric hypertonia: Canadian practice patterns. Can J Neurol Sci. 2012;39(4):508–15.
Childers MK. Targeting the neuromuscular junction in skeletal muscles. Am J Phys Med Rehabil. 2004;83(10):S38–44.
Childers MK. The importance of electromyographic guidance and electrical stimulation for injection of botulinum toxin. Phys Med Rehabil Clin N Am. 2003;14(4):781–92.
Parratte B, Tatu L, Vuillier F, et al. Intramuscular distribution of nerves in the human triceps surae muscle: anatomical bases for treatment of spastic drop foot with botulinum toxin. Surg Radiol Anat. 2002;24(2):91–6.
Van Campenhout A, Molenaers G. Localization of the motor endplate zone in human skeletal muscles of the lower limb: anatomical guidelines for injection with botulinum toxin. Dev Med Child Neurol. 2011;53(2):108–19.
Christensson E. Topography of terminal motor innervation in striated muscles from stillborn infants. Am J Phys Med. 1959;38:65–78.
Coers C. Structural organization of the motor nerve endings in mammalian muscle spindles and other striated muscle fibers. Am J Phys Med Rehabil. 1958;38:166–75.
Saitou K, Masuda T, Michikami D, Michikami D, Kojima R, Okada M. Innervation zones of the upper and lower limb muscles estimated by using multichannel surface EMG. J Hum Ergol (Tokyo). 2000;29(1–2):35–52.
Amirali A, Mu L, Gracies JM, Simpson DM. Anatomical localization of motor endplate bands in the human biceps brachii. J Clin Neuromuscul Dis. 2007;9(2):306–12.
Kim MW, Kim JH, Yang YJ, Ko YJ. Anatomic localization of motor points in gastrocnemius and soleus muscles. Am J Phys Med Rehabil. 2005;84(9):680–3.
Van Campenhout A, Hubens G, Fagard K, Molenaers G. Localization of motor nerve branches of the human psoas muscle. Muscle Nerve. 2010;42(2):202–7.
Hallett M. Explanation of timing of botulinum neurotoxin effects, onset and duration, and clinical ways of influencing them. Toxicon. 2015;107(Pt A):64–7.
Alter KE, Murphy KP. Guidance techniques for Botulinum toxins and other injections. In: Alexander MA, Matthew DJ, editors. Pediatric rehabilitation, principles and practice. 5th ed. New York: Demos Medical Publishing; 2016. p. 153–69.
Shaari CM, Sanders I. Quantifying how location and dose of botulinum toxin injections affect muscle paralysis. Muscle Nerve. 1993;16(9):964–9.
Alter KE, Munin MC. Comparing guidance techniques for chemodenervation procedures. In: Alter KE, Hallett M, Karp B, Lungu C, editors. Ultrasound-guided chemodenervation procedures: Text and atlas. New York: Demos Medical Publishing; 2012. p. 138–54.
Alter KE, Munin MC. US-guided neuortoxin (BoNT) injections: clinical applications. In: Ultrasound-guided chemodenervation procedures: Text and atlas. New York: Demos Medical Publishing; 2012. p. 54–169.
Alter KE. High-frequency ultrasound guidance for neurotoxin injections. Phys Med Rehabil Clin N Am. 2010;21(3):607–30.
Elovic EP, Esquenazi A, Alter KE, Lin JL, Alfaro A, Kaelin DL. Chemodenervation and nerve blocks in the diagnosis and management of spasticity and muscle overactivity. PM R. 2009;1(9):842–51.
Glass GA, Ku S, Ostrem JL, Heath S, Larson PS. Fluoroscopic, EMG-guided injection of botulinum toxin into the longus colli for the treatment of anterocollis. Parkinsonism Relat Disord. 2009;15(8):610–3.
Jordan SE, Ahn SS, Gelabert HA. Combining ultrasonography and electromyography for botulinum chemodenervation treatment of thoracic outlet syndrome: comparison with fluoroscopy and electromyography guidance. Pain Physician. 2007;10(4):541–6.
Lee IH, Yoon YC, Sung DH, Kwon JW, Jung JY. Initial experience with imaging-guided intramuscular botulinum toxin injection in patients with idiopathic cervical dystonia. AJR Am J Roentgenol. 2009;192(4):996–1001.
Alter KE. Ultrasound guidance for botulinum toxin therapy: cervical dystonia. In: Troung D, Hallett M, Zachary C, Dressler D, editors. Manual of botulinum toxin therapy. 2nd ed. New York: Cambridge University Press; 2014. p. 46–59.
Alter KE. Ultrasound guidance for botulinum toxin therapy: thoracic outlet syndrome. In: Eds Troung D, Hallett M, Zachary C, Dressler D, editors. Manual of botulinum toxin therapy. 2nd ed. New York: Cambridge University Press; 2014. p. 269–27.
Alter KE, Lin J. Ultrasound guidance for nerve and motor point blocks. In: Alter KE, Hallett M, Karp BI, Lungu C, editors. Ultrasound guided chemodenervation procedures, Text and atlas. New York: Demos Medical Publishing; 2012. p. 170–84.
Alter KE, Skurow S. Instrumentation and knobology. In: Alter KE, Hallett M, Karp BI, Lungu C, editors. Ultrasound guided chemodenervation procedures; Text and atlas. New York: Demos Medical Publishing; 2012. p. 84–107.
Berweck S, Schroeder AS, Fietzek UM, Heinen F. Sonography-guided injection of botulinum toxin in children with cerebral palsy. Lancet. 2004;363(9404):249–50.
Haig AJ, Goodmurphy CW, Harris AR, Ruiz AP, Etemad J. The accuracy of needle placement in lower-limb muscles: a blinded study. Arch Phys Med Rehabil. 2003;84(6):877–82.
Henzel MK, Munin MC, Niyonkuru C, Skidmore ER, Weber DJ, Zafonte RD. Comparison of surface and ultrasound localization to identify forearm flexor muscles for botulinum toxin injections. PM R. 2010;2(7):642–6.
Hong JS, Sathe GG, Niyonkuru C, Munin MC. Elimination of dysphagia using ultrasound guidance for botulinum toxin injections in cervical dystonia. Muscle Nerve. 2012;46(4):535–9.
Py AG, Zein Addeen G, Perrier Y, Carlier RY, Picard A. Evaluation of the effectiveness of botulinum toxin injections in the lower limb muscles of children with cerebral palsy. Preliminary prospective study of the advantages of ultrasound guidance. Ann Phys Rehabil Med. 2009;52(3):215–23.
Schnabel A, Meyer-Frießem CH, Zahn PK, Pogatzki-Zahn EM. Ultrasound compared with nerve stimulation guidance for peripheral nerve catheter placement: a meta-analysis of randomized controlled trials. Br J Anaesth. 2013;111(4):564–72.
Yang EJ, Rha DW, Yoo JK, Park ES. Accuracy of manual needle placement for gastrocnemius muscle in children with cerebral palsy checked against ultrasonography. Arch Phys Med Rehabil. 2009;90(5):741–4.
Marina MB, Sani A, Hamzaini AH, Hamidon BB. Ultrasound-guided botulinum toxin A injection: an alternative treatment for dribbling. J Laryngol Otol. 2008;122(6):609–14.
Sikdar S. Ultrasound physics. In: Alter KE, Hallett M, Karp BI, Lungu C, editors. Ultrasound guided chemodenervation procedures; Text and atlas. New York: Demos Medical Publishing; 2012. p. 56–83.
Alter KE, Skurow S. Chemodenervation: ultrasound characteristics of relevant tissues. In: Alter KE, Hallett M, Karp BI, Lungu C, editors. Ultrasound guided chemodenervation procedures; text and atlas. New York: Demos Medical Publishing; 2012. p. 124–37.
Smith J, Finnoff JT. Diagnostic and interventional musculoskeletal ultrasound: part 1. Fundamentals. PM R. 2009;1(1):64–75.
Wu C, Xue F, Chang W, Lian Y, Zheng Y, Xie N, Zhang L, Chen C. Botulinum toxin type a with or without needle electromyographic guidance in patients with cervical dystonia. Springerplus. 2016;5(1):1292.
Xu K, Yan T, Mai J. A randomized controlled trial to compare two botulinum toxin injection techniques on the functional improvement of the leg of children with cerebral palsy. Clin Rehabil. 2009;23(9):800–11.
Schnitzler A, Roche N, Denormandie P, Lautridou C, Parratte B, Genet F. Manual needle placement: accuracy of botulinum toxin A injections. Muscle Nerve. 2012;46(4):531–4.
Boon AJ, Oney-Marlow TM, Murthy NS, et al. Accuracy of electromyography needle placement in cadavers: non-guided vs. ultrasound guided. Muscle Nerve. 2011;44(1):45–9.
Chan AK, Finlayson H, Mills PB. Does the method of botulinum neurotoxin injection for limb spasticity affect outcomes? A systematic review. Clin Rehabil. 2017;31(6):713–21.
Grigoriu AI, Dinomais M, Rémy-Néris O, Brochard S. Impact of injection-guiding techniques on the effectiveness of botulinum toxin for the treatment of focal spasticity and dystonia: a systematic review. Arch Phys Med Rehabil. 2015;96(11):2067–78.
Wissel J, Ward TB, Erztgaard P, Bensmail D, Hecht, MJ, Lejeune TM, Schnider P, European consensus table on the use of botulinum toxin type a in adult spasticity. J Rehabil Med. 2009;41:13–25.
Heinen F, Molenaers G, Fairhurst C, Carr LC, Desloovere K, Valayer CE, Morel E, Papavassiliou AS, Tedroff K, Pascual-Pascual SI, Bernert G, Berweck S, Di Rosa, Kolanowski E, Brageloh-Mann I. European consensus table 2006 on botulinum toxin for children with cerebral palsy. Eur J Paediatr Neurol. 2006;10:215–225.
Geiringer SR. Anatomic localization for needle EMG. 2nd ed. New York: Elsevier Medical Publishers; 1999.
Simpson DM, Hallett M, Ashman EJ, Comella CL, Green MW, Gronseth GS, Armstrong MJ, Gloss D, Potrebic S, Jankovic J, Karp BP, Naumann M, So YT, Yablon SA. Practice guideline update summary: botulinum neurotoxin for the treatment of blepharospasm, cervical dystonia, adult spasticity, and headache: report of the guideline Development Subcommittee of the American Academy of Neurology. Neurology. 2016;86(19):1818–26.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG
About this chapter
Cite this chapter
Alter, K.E., Karp, B.I. (2018). Ultrasound, Electromyography, Electrical Stimulation; Techniques Aiding More Effective Botulinum Toxin Therapy. In: Jabbari, B. (eds) Botulinum Toxin Treatment in Clinical Medicine. Springer, Cham. https://doi.org/10.1007/978-3-319-56038-0_15
Download citation
DOI: https://doi.org/10.1007/978-3-319-56038-0_15
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-56037-3
Online ISBN: 978-3-319-56038-0
eBook Packages: MedicineMedicine (R0)