Abstract
Cancer-related pain arises from a variety of different mechanisms. Notable among them are direct local invasion leading to irritation of motor and sensory nerve fibers and post-radiation/post-surgical pain due to nervous system damage. Botulinum neurotoxins (BoNTs) exert their analgesic effect via impeding conduction at the neuromuscular junction as well as inhibition of the release of pain mediators from peripheral nerve endings, dorsal root ganglia, and spinal sensory neurons. One double blind and five open label prospective studies have demonstrated effectiveness of BoNT-As in relieving pain at the site of radiation or surgery for cancer. Single case observations have shown that local intramuscular injection of BoNTs can alleviate chronic and disabling local pain and improve quality of the end of life state among patients with terminal cancer. One blinded study reported that in head and neck cancer, pretreatment of salivary glands with botulinum toxins reduces the incidence of post-radiation damage to the salivary glands.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Botulinum toxin
- Botulinum neurotoxin
- Onabotulinum toxin A (onA)
- Abobotulinum toxin (aboA)
- Incobotulinum toxin (incoA)
- Pain
- Allodynia
- Hyperalgesia
- Cancer
Introduction
As cancer survival has improved due to earlier detection, improved diagnostic procedures, and advanced surgical and radiotherapeutic treatments, new challenges have surfaced in survivors. After treatment, many cancer survivors return to their baseline functional state, but a sizeable number continue to suffer from the long-term side effects of treatment (s) [1]. Chronic pain , a disabling complaint in cancer patients, has a prevalence of approximately 30% that can increase with increased survival [2]. Severity and persistence of pain exerts a negative effect on overall well-being of patients [3]. While pain can be caused by the primary malignancy, different treatment options have been shown to contribute to its origin and chronicity through a variety of mechanisms.
Advanced cancer and end of life state is associated with moderate to severe pain in 70–80% of patients [4], compared to 41–77% and 34–77% reported for non-malignant, advanced medical disorders such as heart disease and chronic obstructive pulmonary disease, respectively [5, 6]. Palliative treatment of this form of pain is often difficult and side effects of analgesic medications are poorly tolerated by debilitated patients [7].
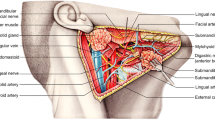
Damage to salivary glands is common in patients with head and neck cancer after radiotherapy. The submandibular glands are often more severely involved due to the proximity of these glands to jugulo-digastric nodes as well as the recent practice of image-guided radiotherapy, which spares a good part of the parotid glands [8]. Dysfunction of salivary glands after radiotherapy for cancer leads to serious complications such as irreversible xerostomia, impaired sense of taste, dysphagia, infectious diseases of the oral and pharyngeal mucosa as well as dental and periodontal diseases [9].
This chapter will start with a discussion of the pathophysiology and therapy of post-radiation and post-surgical pain in cancer patients, followed by descriptions of the available evidence for botulinum neurotoxin (BoNT) effect on preventing and alleviating such pain. Sample case reports relevant to these issues will be provided from the senior author’s experience. A brief account on the potential role of botulinum toxins on relieving intractable pain of advance cancer is also provided. The second part of the chapter discusses the available literature on potential benefit of botulinum toxin therapy in preventing damage to the salivary glands following radiation to the face and neck.
Focal Pain After Head and Face Radiation in Cancer Patients
The pathophysiology of radiation-induced pain is not well-understood. However, radiation-induced fibrosis leading to nerve compression along with direct axonal damage and demyelination along with blood vessels ischemia following capillary network failure have been suggested to be the main culprits for such pain [10,11,12]. List and Bilir [13] have attributed the post-radiation pain observed in 15–30% of patients with head and neck cancer to the development of fibrosis, scar, and keloid. Severe local pain after radiation may require potent systemic analgesic medications such as opioids which, although effective, often cause undesirable side effects. Among the multitude of side effects with these agents are nausea, somnolence, and constipation, each noted in more than 20% of the patients [14]. Topical application of trolamine, hyaluronic acid, and lidocaine patch may provide transient relief [15,16,17], but sustained relief is uncommon and was noted in only 25% of patients who applied lidocaine patch to the allodynic region [18].
Focal Pain After Surgery
Etiology of pain related to surgery is multifactorial and in most cases depends on the site and type of procedure. For example, the subpectoral tissue expansion phase of breast reconstruction surgery that uses an expander to provide a precise pocket over several months to contain the permanent implant can be associated with severe discomfort and pain. The pain can start immediately after the procedure and continue throughout this phase [18]. In other surgical procedures, damage to sensory nerves can cause persistent neuropathic pain, while in others, focal pain in the area of surgery may be related to the development of muscle spasms and increased tone.
Among all cancer types, prevalence of moderate to severe pain is highest in head/neck cancer patients (70%; 95% CI 51–88%) [19]. A review of literature shows that 48% of patients undergoing surgery for malignant head and neck disease reported a pain intensity greater than four (out of ten) at visual analogue scale (VAS) [20]. The current practice in management of pain after surgery is based on surgical complexity and includes: (1) for minor surgeries: NSAIDS (ketoprofen of ketorolac), paracetamol, or tramadol. (2) for medium or major surgeries: opioids (morphine), NSAIDs in elastomeric pump (i.e., ketoprofen)± paracetamol [21]. However, as mentioned earlier, most of these medications have sedative side effects and, in most cases, lead to suboptimal pain management.
Botulinum Neurotoxin Therapy for Post-radiation/Post-surgical Pain in Cancer Patients
The literature on this subject includes one double blind study and eight open label case series (Table 1) as well as a few case reports. Among eight open label studies, five were prospective and three were retrospective. The data collectively indicate that local injection of BoNTs into areas of pain (muscle or skin) significantly alleviates this form of pain in cancer patients.
Randomized, Double Blind, Placebo-Controlled Study (1)
Gabriel et al. [22] investigated the effect of the injection of onabotulinum toxinA into pectoralis muscle in 30 patients (15 toxin, 15 saline) who had undergone mastectomy with immediate expander or acellular dermal matrix reconstruction. A total of 40 units of onabotulinum toxin A was injected into each pectoralis muscle. The saline group received a comparable volume. Patients in the toxin group demonstrated significant improvement of VAS score for pain and were able to tolerate more volume of expansion per visit (p < 0.05). The toxin group also showed a significant decrease in the use of narcotics from the post-injection day 7–45 (p < 0.05).
Prospective Studies (5)
Wittekindt et al. [23] examined the efficacy of BoNT-A (type not specified) in 23 patients who reported neuropathic pain in the neck and shoulder following neck dissection for squamous cell carcinoma of upper “aero-digestive tract .” Patients were divided into low-dose (80–120 units) and high-dose (160–240 units) groups. Patients and physicians were blinded to the dose of injections. Injections were performed in 8–12 locations subcutaneously into targeted neck and shoulder regions. Patients’ response to BoNT injection was measured by visual analog scale (VAS) at baseline prior to injections and at day 28 after injections. The mean baseline pain was 4.3 on VAS (0–10) scale. The quality of life was evaluated by a questionnaire from the European Organization for Research and Treatment of Cancer (EORTC) , specifically prepared for head and neck cancers, at the same time frames. At day 28, mean VAS score for the low-dose group changed from 4.3 to 3.6 (P < 0.05), but the change for the high-dose group was not statistically significant. Furthermore, the low-dose group also showed a trend for improvement of quality of life.
In another prospective study [24], the efficacy of onabotulinum toxinA (OnaA ) and abobotulinum toxinA (AboA ) was assessed in 19 patients with nasopharyngeal and oropharyngeal cancer who developed severe spasm of masseter muscles and trismus, on the average, 5.6 years after radiotherapy for cancer. Eleven patients had received chemotherapy in addition to radiation. The location of cancers was in the nasopharynx (n = 3), oropharynx (n = 9), oral cavity (n = 2), oral cavity and nasopharynx (n = 1), larynx (n = 3), and parotid gland (n = 1). Each masseter muscle was injected at two points, with the total dose of 50 units (onaA) or 250 units (aboA). At 4 weeks post-injection, pain, spasms, and functional score (measured in a 20 subset questionnaire) all improved significantly compared to baseline (P = 0.002, P = 0.004, P = 0.04, respectively). No difference was noted between onaA and AboA .
Voung et al. [25] studied the effect of BoNT injection into the rectal wall immediately after high dose-rate-endorectal brachytherapy (HDREBT) in 15 patients with prostatic cancer and used non-injected patients as controls. The patients who received 100 units of onaA into the rectal wall had a lower incidence of acute radiation prostatitis with significant reduction of bowel frequency and urgency (P < 0.05) and lesser degrees of pain (P = 0.07).
More recently, the Yale group published their experience with patients who had head, neck, and breast cancer and suffered from moderate to severe pain (VAS 5 or more) at the site of cancer resection or radiation [26]. Patients were prospectively enrolled in an open label study. A total of up to 80–100 units of incobotulinum toxin A, diluted in 1 cc of saline, was injected into the area of local pain indicated by the patient. The injections were subcutaneous or intramuscular depending on the type of pain, neuropathic (subcutaneous), or focal muscle spasm (intramuscular). The efficacy of treatment was assessed via VAS, Patient Global Impression of Change (PGIC), and American Chronic Pain Association questionnaire (Quality of Life Scale for pain), at 4, 6, 8, 10, 12 weeks post-injection. The primary outcome was two grades or more improvement in VAS score plus subject satisfaction expressed in the PGIC at 6 weeks. The secondary outcome was improvement of quality of life at 6 weeks. Twenty-five patients were screened and 12 were enrolled in the study. Two patients died during the study from complications of cancer and two were too sick to attend the follow-up sessions. Eight subjects, 31–70 years of age—four female four males—completed the study. Their baseline mean pain score in VAS was 7.4 (range 5–10). Four had breast cancer, two tonsillar, one base of the tongue, and one dermal squamous cell carcinoma of the neck.
At 4 weeks, all eight subjects reported significant pain relief with the mean baseline VAS of 7.4 dropping to 3.8 (P < 0.05). Five of eight patients maintained the same degree of pain relief at 12 weeks. Seven of eight patients reported their pain as much improved or very much improved on the PGIC assessment. Three of eight patients reported significant improvement of the quality of life at 6 weeks.
Bach et al. [27] prospectively followed nine patients with post-surgical contracture of sternocleidomastoid or pectoralis major muscle related to head and neck cancer. AbobotulinumtoxinA was injected into the sternocleidomastoid (100–400 units) and into the pectoralis major flap (125–200 units). All patients expressed pain relief. The cervical disability score fell from 33 to 23 (P < 0.01). There were no side effects.
Retrospective Studies (3)
In the study of Van Daele et al. [28], injection of onabotulinum toxin A into the tight and painful sternocleidomastoid muscle relieved the pain and tightness in four of six patients. All patients had received radiotherapy for head and neck cancer. The injected dose was 20–25 units administered at one or two points into the sternocleidomastoid muscle.
Stubblefield et al. [29] also found BoNT-A injection helpful in relieving focal pain caused by radiation fibrosis. In this retrospective study of 23 patients, 30% had painful trismus and 43% had trigeminal and cervical plexus neuralgia.
Mittal et al. [30] reviewed the results of onabotulinum toxinA treatment in eight patients with head and neck and breast cancer. Injection of 80–100 units of onA into the painful region alleviated muscle spasms and neuropathic pain in these patients. Five of eight patients reported treatment as “very satisfactory” in the Patient Global Impression of Change (PGIC) .
The following case reports describe two patients who have participated in the Yale protocol assessing the effect of BoNT therapy on cancer-related pain.
Case 1—Carcinoma of the Base of the Tongue Associated with Painful Upper Neck Spasms and Burning Pain Interfering with Speaking and Swallowing
A 47 year old, right-handed gentleman was referred to the Yale Neurotoxin Treatment Clinic for evaluation of right upper neck pain, difficulty in swallowing, and speaking of 5 years duration. Six years ago, he was found to have a tumor at the base of the tongue and cervical lymphadenopathy on the right side. He underwent resection of the tumor with removal of lymph nodes and neck muscles on the right side. The tumor was a squamous cell carcinoma. Shortly after resection, he received radiotherapy to the base of the tongue and right side of the neck. A few months later, he experienced tingling and pulling of the base of the tongue which gradually evolved into painful spasms and burning sensation below the angle of the right jaw interfering with speaking and eating. Treatment with a variety of analgesic drugs was only minimally helpful.
General medical and neurological examinations were normal except for loss of muscles on the right side of the neck and mild weakness of the tongue. A vertical surgical scar was visible on the right side of the neck extending from lower neck to the lower edge of the mandible. Several areas of induration and keloid formation were present, the hardest and most painful being located anterior to and slightly below the angle of the right jaw.
Twenty units of Onabotulinum toxin A was injected into each of the three areas of indurated, scar tissue on the right side of the neck (Fig. 1). The dilution was 100 units/cc. A ¾ inch long, 27.5 gauge needle was used for injections. After a week, patient reported total cessation of muscle spasms and burning pain as well as marked improvement of his swallowing and speech. He reported no side effects. The pain and discomfort returned after 6 months. Patient reported the same favorable results over 8 years of follow-up with slightly higher doses of onaA (30, 30, and 20 units) applied in the last 3 years.
Case 2—Intense Left Cervical Pain Following Laryngectomy and Neck Dissections for Squamous Cell Carcinoma of the Piriform Sinus
A 48-year-old man underwent laser supraglottic laryngectomy with bilateral neck dissections for squamous cell carcinoma of the left piriform sinus. This was followed by courses of chemotherapy and radiation. Two years later, patient developed intense left cervical pain and left shoulder pain beginning with spasms of the left sternocleidomastoid (SCM) muscle . The pain was described as deep and aching, but at times sharp and jabbing. A variety of medications including fentanyl 25 μg/h. patch and hydromorphone 2 mg tablets, given as needed, provided no significant pain relief. He was then injected with a total dose of 200 units of Onabotulinum toxin A into the left cervical and shoulder muscles: left SCM, left trapezius, left splenius, and left levator scapulae muscles at several points, 15–20 units per site (Fig. 2). After a week, he reported marked reduction of pain (from VAS 8 to 1); on PGIC, he expressed the outcome as “very satisfactory.” The response continued over a period of 3 years with repeat injections performed every 4 months. The patient did not report any side effects.
Palliative Effects of Botulinum Toxins in Patients with Terminal Cancer and Recalcitrant Pain
Pain can be a major issue in cancer patients close to end of life. Such fragile patients often poorly tolerate potent analgesics. Anectodal observations attest to the analgesic and palliative action of BoNTs in the end of the life pain [31]. The patient reported below was treated by the senior author of this chapter for pain relief.
Case 1: Severe Jaw Pain and Trismus Due to the Direct Invasion of Masseter Muscle and Jaw Bone by a Non-small Cell Cancer of the Lung
A 69-year-old female with non-small cell carcinoma of the lungs (stage IV) and metastasis to the bones (femur, petrous) and brain underwent multiple courses of radiation and chemotherapy. Three months after the completion of radiotherapy, she complained of jaw stiffness, inability to open the mouth fully, and right masseter pain when attempting to open the mouth. Over the next few weeks, the pain reached a point that she refrained from eating. Administration of oxycodone (10 mg, twice daily) and fentanyl (25 μg patch every 72 h) provided partial pain relief, but did not alleviate the trismus. An MRI showed enlargement of right masseter due to neoplastic involvement (Fig. 3).
Injection of onabotulinum toxinA (50 units) into the right masseter and 20 units into the right temporalis decreased the right masseter pain and improved jaw opening for 6 weeks. Subsequent injections of a larger dose of onaA into the right masseter (70 units) with additional injection into the left masseter (30 units) improved her quality of life (pain relief, less eating difficulty) over the next 18 months before her demise from complications of cancer.
Comment
Botulinum neurotoxins can influence and reduce pain via a variety of mechanisms [32,33,34]. These include inhibition of pain mediator (CGRP, SP, glutamate) release from nerve endings, dorsal root ganglia, and spinal neurons as well as reduction of local inflammation. Further mechanisms involve inhibition of sodium and purinergic channels (ATP), decreased discharge of sympathetic neurons, and muscle spindles [32,33,34]. These effects collectively subdue peripheral and ultimately central sensitization, the principal factors of pain chronicity. Intra-lesional injection of botuliumtoxinA into keloids formed at the site of surgery or radiation softens and reduces the volume of keloids in a manner similar to steroid injection and is superior to steroids in regard to symptom relief (including pain) [35].
Cancer-related pain is hard to treat and introduction of a novel therapeutic modality with a safe and low side effect profile is welcome, given the fragility of the patients and their higher propensity for developing side effects. Although current literature in this area does not include high-quality clinical trials, the available data collectively support a place for all three types of BoNTs (onaA, incoA, and AboA ) in the treatment of cancer-related pain.
The Role of BoNTs in Prevention of Post-radiation Damage to the Salivary Glands
As was mentioned in the introduction, radiation to the face and neck damages the salivary glands and leads to a variety of unpleasant symptoms caused by salivary glands dysfunction [9]. The submandibular gland is often more damaged as it is less protected than parotid gland by the modern radiotherapeutic techniques [8]. Submandibular glands provide 60–67% of the unstimulated and 50% of stimulated saliva. There is evidence in animals and human that injection of BoNTs into the salivary gland prior to radiotherapy reduces the damage to these glands substantially.
Teymoortash et al. [36] showed that injection of BoNT-A or B into submandibular glands of the rat before irradiation of the gland prevented the marked radiation-induced parenchymal loss and acinar fibrosis compared to the saline-injected rats. The weight of submandibular gland after radiation was also markedly reduced in the saline-injected rats, but not in the BoNT-injected rats (P = 0.008).
In another study of irradiated salivary glands, at third day post-irradiation, mice pre-injected with BoNT-A demonstrated 25% reduction in the flow of saliva compared to 50% reduction in the BoNT-untreated mice (P < 0.05). Local neutrophil infiltration, detected by myeloperoxidase staining, was threefold lower for the BoNT-treated mice. At 4 weeks post-irradiation, the saline (control) group showed a 40% reduction in basal SMG weight, compared with 20% in weight reduction in the BoNT group. Histologically, BoNT-pretreated glands showed relative preservation of acinar structures after radiation [37].
In a recent prospective, randomized, placebo-controlled, double-blinded study conducted in human subjects affected by head and neck cancer, investigators assessed safety of BoNT A and B injection into the submandibular gland prior to radiotherapy. Subjects were divided into four groups, each consisting of three subjects. The injected doses were 20 units for type A and 750 units for the type B toxin. Injections were safe, but authors found no difference between BoNTs (A or B) and placebo regarding the gland’s uptake of technetium pertechnetate or regarding the salivary excretion fraction. The authors concluded that due to the small number of patients, further investigation of various doses and timing of BoNT injection is required for a more precise analysis of toxin’s efficacy in humans [38].
Chapter Conclusion
Several studies in human indicate that local injection of BoNTs into the scar and keloid tissue and into adjacent muscles substantially reduces the post-surgical pain in cancer patients after surgery and radiation. Case observations strongly suggest that local injection of BoNTs can ease the pain in some terminal cancer patients with recalcitrant local pain. Data in animals indicate that injection of BoNTs into the submandibular gland prior to irradiation of the gland prevents paranchymal damage, gland atrophy, and reduction of salivation. In human, additional studies are needed for assessing the efficacy of BoNTs in this setting.
References
Stein KD, Syrjala KL, Andrykowski MA. Physical and psychological long-term and late effects of cancer. Cancer. 2008;112:2577–92. doi:10.1002/cncr.23448.
Brown MR, Ramirez JD, Farquhar-Smith P. Pain in cancer survivors. Br J Pain. 2014;8:139–53. doi:10.1177/2049463714542605.
Elliott J, Fallows A, Staetsky L, Smith PW, Foster CL, Maher EJ, Corner J. The health and well-being of cancer survivors in the UK: findings from a population-based survey. Br J Cancer. 2011;105(Suppl 1):S11–20. doi:10.1038/bjc.2011.418.
Caraceni A, Hanks G, Kaasa S, Bennett MI, Brunelli C, Cherny N, Dale O, De Conno F, Fallon M, Hanna M, Haugen DF, Juhl G, King S, Klepstad P, Laugsand EA, Maltoni M, Mercadante S, Nabal M, Pigni A, Radbruch L, Reid C, Sjogren P, Stone PC, Tassinari D, Zeppetella G. Use of opioid analgesics in the treatment of cancer pain: evidence-based recommendations from the EAPC. Lancet Oncol. 2012;13:e58–68. doi:10.1016/s1470-2045(12)70040-2.
Harris DG. Management of pain in advanced disease. Br Med Bull. 2014;110:117–28. doi:10.1093/bmb/ldu010.
Solano JP, Gomes B, Higginson IJ. A comparison of symptom prevalence in far advanced cancer, AIDS, heart disease, chronic obstructive pulmonary disease and renal disease. J Pain Symptom Manag. 2006;31:58–69. doi:10.1016/j.jpainsymman.2005.06.007.
Borsook D. Neurological diseases and pain. Brain J Neurol. 2012;135:320–44. doi:10.1093/brain/awr271.
Cannon DM, Lee NY. Recurrence in region of spared parotid gland after definitive intensity-modulated radiotherapy for head and neck cancer. Int J Radiat Oncol Biol Phys. 2008;70:660–5.
Bansal M, Mohanti BK, Shah N, et al. Radiation related morbidities and their impact on quality of life in head and neck cancer patients receiving radical radiotherapy. Qual Life Res. 2004;13:481–8.
Kehlet H, Jensen TS, Woolf CJ. Persistent postsurgical pain: risk factors and prevention. Lancet. 2006;367:1618–25. doi:10.1016/s0140-6736(06)68700-x.
Kanner RM, Foley KM. Patterns of narcotic drug use in a cancer pain clinic. Ann N Y Acad Sci. 1981;362:161–72.
Delanian S, Lefaix JL, Pradat PF. Radiation-induced neuropathy in cancer survivors. Radiother Oncol. 2012;105:273–82. doi:10.1016/j.radonc.2012.10.012.
List MA, Bilir SP. Functional outcomes in head and neck cancer. Semin Radiat Oncol. 2004;14:178–89. doi:10.1053/j.semradonc.2003.12.008.
Straube C, Derry S, Jackson KC, Wiffen PJ, Bell RF, Strassels S, Straube S. Codeine, alone and with paracetamol (acetaminophen), for cancer pain. Cochrane Database Syst Rev. 2014;Cd006601. doi:10.1002/14651858.CD006601.pub4.
Fisher J, Scott C, Stevens R, Marconi B, Champion L, Freedman GM, Asrari F, Pilepich MV, Gagnon JD, Wong G. Randomized phase III study comparing best supportive care to Biafine as a prophylactic agent for radiation-induced skin toxicity for women undergoing breast irradiation: Radiation Therapy Oncology Group (RTOG) 97-13. Int J Radiat Oncol Biol Phys. 2000;48:1307–1310.
Chargari C, Fromantin I, Kirova YM. Importance of local skin treatments during radiotherapy for prevention and treatment of radio-induced epithelitis. Cancer Radiother. 2009;13:259–66. doi:10.1016/j.canrad.2009.04.003.
Kirova YM, Fromantin I, De Rycke Y, Fourquet A, Morvan E, Padiglione S, Falcou MC, Campana F, Bollet MA. Can we decrease the skin reaction in breast cancer patients using hyaluronic acid during radiation therapy? Results of phase III randomised trial. Radiother Oncol. 2011;100:205–9. doi:10.1016/j.radonc.2011.05.014.
Fleming JA, O’Connor BD. Use of lidocaine patches for neuropathic pain in a comprehensive cancer centre. Pain Res Manag. 2009;14:381–8.
van den Beuken-van Everdingen MH, de Rijke JM, Kessels AG, Schouten HC, van Kleef M, Patijn J. Prevalence of pain in patients with cancer: a systematic review of the past 40 years. Ann Oncol. 2007;18:1437–49. doi:10.1093/annonc/mdm056.
Sommer M, Geurts JW, Stessel B, Kessels AG, Peters ML, Patijn J, van Kleef M, Kremer B, Marcus MA. Prevalence and predictors of postoperative pain after ear, nose, and throat surgery. Arch Otolaryngol Head Neck Surg. 2009;135:124–30. doi:10.1001/archoto.2009.3.
Bianchini C, Malago M, Crema L, Aimoni C, Matarazzo T, Bortolazzi S, Ciorba A, Pelucchi S, Pastore A. Post-operative pain management in head and neck cancer patients: predictive factors and efficacy of therapy. Acta Otorhinolaryngol Ital. 2016;36:91–6. doi:10.14639/0392-100x-499.
Gabriel A, Champaneria MC, Maxwell GP. The efficacy of botulinum toxin A in post-mastectomy breast reconstruction: a pilot study. Aesthet Surg J. 2015;35:402–9. doi:10.1093/asj/sjv040.
Wittekindt C, Liu WC, Preuss SF, Guntinas-Lichius O. Botulinum toxin A for neuropathic pain after neck dissection: a dose-finding study. Laryngoscope. 2006;116:1168–71. doi:10.1097/01.mlg.0000217797.05523.75.
Hartl DM, Cohen M, Julieron M, Marandas P, Janot F, Bourhis J. Botulinum toxin for radiation-induced facial pain and trismus. Otolaryngol Head Neck Surg. 2008;138:459–63. doi:10.1016/j.otohns.2007.12.021.
Vuong T, Waschke K, Niazi T, Richard C, Parent J, Liberman S, Mayrand S, Loungnarath R, Stein B, Devic S. The value of Botox-A in acute radiation proctitis: results from a phase I/II study using a three-dimensional scoring system. Int J Radiat Oncol Biol Phys. 2011;80(5):1505–11.
Rostami R, Mittal SO, Radmand R, Jabbari B. Incobotulinum toxin-A improves post-surgical and post-radiation pain in cancer patients. Toxins. 2016;8(1):22. doi:10.3390/toxins8010022.
Bach CA, Wagner I, Lachiver X, Baujat B, Chabolle F. Botulinum toxin in the treatment of post-radiosurgical neck contracture in head and neck cancer: a novel approach. Eur Ann Otorhinolaryngol Head Neck Dis. 2012;129:6–10. doi:10.1016/j.anorl.2011.07.002.
Van Daele DJ, Finnegan EM, Rodnitzky RL, Zhen W, McCulloch TM, Hoffman HT. Head and neck muscle spasm after radiotherapy: management with botulinum toxin A injection. Arch Otolaryngol Head Neck Surg. 2002;128:956–9.
Stubblefield MD, Levine A, Custodio CM, Fitzpatrick T. The role of botulinum toxin type A in the radiation fibrosis syndrome: a preliminary report. Arch Phys Med Rehabil. 2008;89:417–21. doi:10.1016/j.apmr.2007.11.022.
Mittal S, Machado DG, Jabbari B. Onabotulinum toxin A for treatment of focal cancer pain after surgery and/or radiation. Pain Med. 2012;13:1029–33. doi:10.1111/j.1526-4637.2012.01437.x.
Fu J, Ngo A, Shin K, et al. Botulinum toxin injection and phenol nerve block for reduction of end-of-life pain. J Palliat Med. 2013;16:1637–40.
Aoki RK, Francis J. Update on the nociceptive mechanism hypothesiss and related disorders. Parkinsonism Relat Disord. 2011;17:S28–33.
Brown EA, Schutz SG, Simpson DM. Botulinum toxin for neuropathic pain and spasticity: an overview. Pain Manag. 2014;4:129–51.
Mittal SO, Safarpour D, Jabbari B. Botulinum toxin treatment of neuropathic pain. Semin Neurol. 2016;36:73–83.
Shaarawy E, Hegazy RA, Abdel Hay RM. Intralesional botulinum toxin type A equally effective and better tolerated than intralesional steroid in the treatment of keloids: a randomized controlled trial. J Cosmet Dermatol. 2015;14:161–6.
Teymoortash A, Müller F, Juricko J, Bieker M, Mandic R, Librizzi D, Höffken H, Pfestroff A, Werner JA. Botulinum toxin prevents radiotherapy-induced salivary gland damage. Oral Oncol. 2009;45:737–9.
Zeidan YH, Xiao N, Cao H, Kong C, Le QT, Sirjani D. Botulinum toxin confers radioprotection in murine salivary glands. Int J Radiat Oncol Biol Phys. 2016;94:1190–7.
Teymoortash A, Pfestroff A, Wittig A, Franke N, Hoch S, Harnisch S, Schade-Brittinger C, Hoeffken H, Engenhart-Cabillic R, Brugger M, Strauch K. Safety and efficacy of botulinum toxin to preserve gland function after radiotherapy in patients with head and neck cancer: a prospective, randomized, placebo-controlled, double-blinded phase I clinical trial. PLoS One. 2016;11(3):e0151316. doi: 10.1371/journal.pone.0151316. eCollection 2016.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG
About this chapter
Cite this chapter
Safarpour, D., Jabbari, B. (2018). The Role of Botulinum Toxins in Treatment of Cancer-Related Issues: Post-radiation and Post-surgical Pain and Radiation-Induced Damage to the Salivary Glands. In: Jabbari, B. (eds) Botulinum Toxin Treatment in Clinical Medicine. Springer, Cham. https://doi.org/10.1007/978-3-319-56038-0_14
Download citation
DOI: https://doi.org/10.1007/978-3-319-56038-0_14
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-56037-3
Online ISBN: 978-3-319-56038-0
eBook Packages: MedicineMedicine (R0)