Abstract
Children on long-term maintenance dialysis have significantly diminished life expectancy mostly due to cardiovascular disease. In children, cardiac arrest is the most common cause of death, while in adults with childhood onset of ESRD, accelerated and premature coronary artery disease and cardiomyopathy are major causes of cardiac death. Cardiac and vascular abnormalities develop early in the course of chronic kidney disease (CKD) in children and reach a peak when the child enters maintenance dialysis. This is due to an exceptionally high prevalence of traditional and uremia-related cardiovascular risk factors. Aggressive dialysis and kidney transplantation are the best options to prevent development and progression of cardiovascular disease (CVD) in children on dialysis.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Children
- Chronic dialysis
- Chronic kidney disease
- Cardiovascular disease
- Cardiovascular risk
- Hypertension
- Dyslipidemia
- Left ventricular hypertrophy
- Atherosclerosis
- Cardiomyopathy
Case Presentation
A 16-year-old male has been on maintenance hemodialysis (three times per week, 4 h treatment) for the last 6 months as he progressed to end-stage renal disease (ESRD) secondary to focal segmental glomerulosclerosis (FSGS ) . His dialysis course has been complicated by nonadherence: he admits frequently forgetting to take his medications; occasionally, he does not show up for his hemodialysis session.
He presented in the emergency department (ED) complaining of severe headache and vomiting that had developed over the last 24 h. The initial evaluation in ED showed a BP of 180/100 mm Hg, heart rate of 112/min, respiratory rate 32/min, and oxygen saturation 92%. His weight was 6 kg above his estimated dry weight. Physical examination demonstrated bibasilar rales and an S3 gallop, no peripheral edema except eye puffiness. The laboratory results were: Hg 7.9 g/dL, BUN 123 mg/dL, serum creatinine 10.2 mg/dL, K 5.9 mEq/L, HCO3 16 mEq/L, Ca 7.8 mg/dL, P 7.3 mg/dL, and albumin 2.6 mg/dL. Echocardiography showed diffuse chamber enlargement and depressed biventricular function with shortening fraction of 18%. The patient was treated for hypertension in the ED and then admitted to the hospital for acute hemodialysis treatment. His last hemodialysis treatment prior to the ED visit had been 5 days ago.
His routine monthly evaluation 2 weeks before had shown Hg 9.2 g/dL, BUN 93 mg/dL, serum creatinine 12.4 mg/dL, K 5.1 mEq/L, HCO3 18 mEq/L, Ca 8.2 mg/dL, P 8.3 mg/dL, iPTH 560 pg/ml, and albumin 3.1 mg/dL. Lipid profile demonstrated LDL cholesterol 152 mg/dL and triglycerides 274 mg/dL. Over the last few months, BP has been elevated despite two prescribed antihypertensive medications. Echocardiography demonstrated concentric left ventricular hypertrophy (LVH ) . He has no available kidney transplant living donor. Active listing for deceased donor kidney transplantation is currently on hold due to nonadherence.
Clinical Questions
-
1.
Why is monitoring of cardiovascular risk essential in children on maintenance dialysis?
-
2.
How should a child on maintenance dialysis be evaluated for cardiovascular risk? What are the most common cardiovascular abnormalities in children on maintenance dialysis?
-
3.
What are appropriate targets and treatment options to control cardiovascular risk?
-
4.
What is the best strategy to prevent progression of cardiovascular disease (CVD) in pediatric patients on maintenance dialysis?
Diagnostic Discussion
-
1.
Young adults who develop ESRD during childhood have a significantly diminished life expectancy. Upon reaching adulthood, dialysis patients live 40–50 years less compared to the age- and race-matched general population [1]. Cardiovascular disease (CVD) is the leading cause of death in children and young adults on maintenance dialysis, accounting for one third of all causes [2]. However, the causes of death in children are different from those in adults. In young adults with childhood-onset ESRD , coronary artery disease and congestive heart failure due to cardiomyopathy are two leading causes of mortality from CVD [3]. The mortality from these causes is extremely low in pediatric patients. Of the specific causes of cardiovascular deaths in children, cardiac arrest is the most common, followed by arrhythmia and cardiomyopathy.
-
2.
The prevalence of traditional cardiovascular risk factors in children on maintenance dialysis is similar to that in adults on dialysis. Thus, cardiovascular diagnostic evaluation is focused on identifying children with hypertension , dyslipidemia , and obesity. In contrast to adults, diabetes as a cause of ESRD is very rare in children. However, hyperglycemia and insulin resistance could be seen in dialyzed children, especially in the obese and those on steroid therapy.
Hypertension is the most frequent risk but is also the likely modifiable factor. Poor BP control in children on maintenance dialysis is multifactorial, but the major cause is fluid overload. Thus, the first step in the diagnosis and management of hypertension should be evaluation of volume status. Unfortunately, many children on dialysis do not achieve their dry weight. Volume status assessment in very young patients is frequently inaccurate. This is one of the reasons why the frequency of hypertension is higher in young children. In addition, correct assessment of BP is difficult in small children, and consequently it is frequently underdiagnosed and therefore not adequately treated. Another group of children who present with significant fluid overload and hypertension is adolescents, who are almost always non-compliant with fluid and salt restriction. Significant fluid overload, likely due to nonadherence, can lead to acute hypertension and congestive heart failure, as was seen in the case presentation above.
Chronic fluid overload with secondary hypertension (volume and pressure overload) is also a major cause of left ventricular hypertrophy (LVH ) , the most common intermediate cardiovascular abnormality seen in children on maintenance dialysis. As a result of pressure overload that occurs with hypertension , concentric LV remodeling and hypertrophy develop, whereas volume overload and severe anemia result in eccentric LVH (Fig. 27.1). Abnormal mineral metabolism, specifically increased fibroblast growth factor 23 (FGF23), also plays an important role in inducing concentric LVH. Initially, LVH is compensatory and adaptive. However, if untreated, LVH might become maladaptive with development of myocardial fibrosis . All this leads to myocyte death and, finally, to diastolic and systolic dysfunction. If LVH is diagnosed at the time of dialysis initiation, routine echocardiographic monitoring every 6 months is advisable. If the initial echocardiogram is normal, yearly echocardiographic follow-up to reassess cardiac structure and function is suggested.
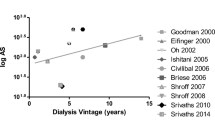
In addition to cardiac changes, children on dialysis might develop intermediate vascular abnormalities such as increased carotid artery intima-media thickness, increased arterial stiffness, and even coronary artery calcification – all markers of early atherosclerosis and arteriosclerosis [3]. In addition to hypertension and dyslipidemia , abnormally high serum phosphorus and increased calcium-phosphorus product are important causes of these vascular abnormalities.
-
3.
The target blood pressure in children with CKD should be less than the 90th percentile adjusted for age, gender, and height, or less than 120/80 mm Hg, whichever is lower [4]. Aggressive management of fluid overload and achievement of dry weight is the most effective treatment of hypertension and LVH in children on chronic dialysis . If BP remains elevated despite adequate volume control, antihypertensive medications should be optimized. Angiotensin-converting enzyme inhibitors or angiotensin II receptor blockers should be considered as a first line of therapy in children on dialysis because of their reno- and cardioprotective effects. Addition of calcium channel blockers or beta-blockers should be tried next. It is important to remember that if effective dry weight is not achieved, antihypertensive meds, especially vasodilators and beta-blockers, will likely not work and may further impair the ability to remove fluid.
The assessment of dyslipidemias should include a complete fasting lipid profile with total cholesterol, LDL, HDL, and triglycerides. The definition of dyslipidemia differs in children and adults. Hyperlipidemia in children is defined as lipid levels greater than the 95th percentile for age and gender. For adolescents with Stage 5 CKD and a level of LDL cholesterol ≥130 mg/dl, KDOQI recommends treatment to reduce LDL to <130 mg/dl. If LDL is <130 mg/dl, fasting triglycerides ≥200 mg/dl, and non-HDL cholesterol (total cholesterol minus HDL) ≥160 mg/dl, treatment should be considered to reduce non-HDL cholesterol to <160 mg/dl [5]. All children with dyslipidemias should follow the recommendations for therapeutic lifestyle changes (TLC) , which include diet modification with reduction in saturated fat intake and increase in fiber intake, and moderate physical activity. Adolescents should be counseled about avoiding smoking.
It is recommended to maintain calcium (Ca) and phosphorus (P) levels within the normal range and the Ca × P product <55 mg2/dl2 in children on chronic dialysis . The use of non-calcium-based phosphate binders, careful monitoring of the serum calcium level, and appropriate adjustment of the dose of vitamin D to avoid hypercalcemia are essential in the management of children on dialysis to prevent development and progression of cardiovascular abnormalities [6].
-
4.
The overall strategy in preventing cardiovascular complications in children with advanced chronic kidney disease is avoidance of long-term dialysis. The goal is to prevent development and delay the progression of cardiomyopathy and atherosclerosis . Even though kidney transplantation poses a continued cardiovascular risk (hypertension, hyperlipidemia, allograft dysfunction), it eliminates many uremia-related risks, reduces the risk of cardiac death by approximately 80%, and prolongs life span by 20–30 years. Graft failure after the first kidney transplantation is associated with an almost five times higher mortality rate as compared to children with a functioning graft. Having maintenance dialysis even for a few months before transplant is also associated with worse survival. Thus, preemptive kidney transplantation should be the ultimate goal to minimize cardiovascular morbidity and mortality.
For those patients who must have long-term dialysis, the strategy is directly linked to the achievement of adequate dialysis outcomes which includes aggressive monitoring and management of hypertension, dyslipidemia , calcium-phosphorus metabolism, anemia, nutrition, systemic inflammation, and other dialysis complications. Unfortunately, achieving recommended Kt/V urea as measurement of adequacy does not necessarily lead to control of the above problems. Longer and more frequent dialysis sessions are typically needed to avoid or reduce cardiovascular complications.
Clinical Pearls
-
1.
Children with ESRD are among the populations with the highest cardiovascular risk due to an extremely high prevalence of traditional and uremia-associated risk factors.
-
2.
LVH is the most common cardiac abnormality found in children on maintenance dialysis. Other early cardiac (LV dysfunction) and vascular abnormalities (increased carotid artery IMT, arterial stiffness, coronary artery calcification) may also be detected, especially in patients with uncontrolled hypertension and abnormal calcium-phosphorus metabolism.
-
3.
Young adults with childhood onset of ESRD and poorly controlled cardiovascular risk frequently develop accelerated cardiovascular disease, the major cause of premature death in this population.
-
4.
Longer and more frequent dialysis sessions are a proven strategy to minimize cardiovascular risk.
-
5.
Kidney transplantation , preferably performed preemptively, is the best treatment option to prevent development and progression of cardiovascular disease in children with ESRD.
References
Renal Data System US. USRDS 2014 annual data report: atlas of chronic kidney disease and end-stage renal disease in the United States. National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases: Bethesda; 2014.
Mitsnefes MM, et al. Mortality risk among children initially treated with dialysis for end-stage kidney disease, 1990-2010. JAMA. 2013;309(18):1921–9.
Mitsnefes MM. Cardiovascular disease in children with chronic kidney disease. J Am Soc Nephrol. 2012;23(4):578–85.
Agarwal R, et al. Assessment and management of hypertension in patients on dialysis. J Am Soc Nephrol. 2014;25(8):1630–46.
KDIGO. Clinical practice guideline for lipid management in chronic kidney disease. Kidney Int Suppl. 2013;3(3):259–305.
Kidney Disease: Improving Global Outcomes (KDIGO) CKD-MBD Work Group. KDIGO clinical practice guideline for the diagnosis, evaluation, prevention, and treatment of chronic kidney disease-mineral and bone disorder (CKD-MBD). Kidney Int Suppl. 2009;76:S1–130.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this chapter
Cite this chapter
Mitsnefes, M.M. (2017). Cardiovascular Disease. In: Warady, B., Schaefer, F., Alexander, S. (eds) Pediatric Dialysis Case Studies. Springer, Cham. https://doi.org/10.1007/978-3-319-55147-0_27
Download citation
DOI: https://doi.org/10.1007/978-3-319-55147-0_27
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-55145-6
Online ISBN: 978-3-319-55147-0
eBook Packages: MedicineMedicine (R0)