Abstract
GI malignancy covers four main tumour sites: oesophagogastric, hepatobiliary, colorectal and anus with radiotherapy having an important role to play in each of these sites. PET-CT is not standard in the planning procedure for these patients, but research is ongoing and most available data relates to rectal cancer [1, 2].
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
GI malignancy covers four main tumour sites: oesophagogastric, hepatobiliary, colorectal and anus with radiotherapy having an important role to play in each of these sites. PET/CT is not standard in the planning procedure for these patients, but research is ongoing and most available data relates to rectal cancer [1, 2].
2 Rectal Cancer
The potential benefits of PET scanning in rectal RT planning are illustrated by a study comparing CT-PET-, MR-PET- and FDG-PET-based tumour length measurements with pathology in patients receiving short-course RT (5 × 5 Gy) and surgery [3]. Although no significant correlation was found between CT-based measurements with the resection specimen, a modest correlation was detected with MR-based measurements (Pearson’s correlation = 0.55, p < 0.001), and a good correlation was confirmed with manual FDG-PET measurements (Pearson’s correlation = 0.72, p < 0.001), but the best correlation with pathology was observed with automatic PET/CT based measurements (Pearson correlation = 0.91, p < 0.001). An overestimation of the rectal tumour diameter and volume using manual MRI-based measurements compared with PET-based contouring has also been reported [4]. This is an important consideration, especially for low rectal cancers where the caudal border of the treatment volume may be tailored, resulting in avoidance of sphincter irradiation (Fig. 10.1).
MRI and 18F-fluorodeoxyglucose positron emission tomography (FDG-PET) images of a patient with locally advanced rectal cancer prior to chemoradiotherapy. The rectal tumour is demonstrated as an annular mass on axial MRI imaging (a). The most metabolically active part of the tumour extends from the 10 to 4 o’clock position where it abuts the prostate and seminal vesicles (b). Enlarged lymph nodes with mixed signal and irregular borders are observed on MRI (c—white arrow). However, these lymph nodes were of low FDG avidity and were not reliably detected by PET (d), emphasising the importance of using MRI in conjunction with PET for RT planning
The use of FDG-PET/CT has been shown to reduce the interobserver variability in rectal tumour delineation. In a recent study, GTVs generated from automatic contours on PET scan were compared with GTVs manually delineated by multiple observers [2]. GTVs based on PET were more consistent with the PET auto-contouring method. Moreover, the CTV based on PET extended outside of the CTV used in clinical practice in almost a third of patients, suggesting that the integration of PET in the RT planning process in rectal cancer has the potential to avoid geographical misses. This may have important clinical implications for defining the phase II ‘boost’ for rectal tumours with involved circumferential resection margins [5].
3 Oesophageal and Pancreatic Cancer
Radiotherapy planning for oesophagogastric carcinomas is notoriously difficult because of poor tumour delineation on standard imaging. CT demonstrates bulk disease but has limitations in defining longitudinal spread of disease, and endoscopy only gives the luminal dimensions. FDG-PET has been observed to improve intra- and interobserver variability. Using endoscopic ultrasound (EUS) as gold standard, FDG-PET facilitated a more accurate delineation of oesophageal tumour length compared with CT [6]. In pancreatic cancer, the use of FDG-PET fusion with planning CT has resulted in GTVs that were smaller overall compared with CT alone [7] (Figs. 10.2 and 10.3).
CT and 18F-fluorodeoxyglucose positron emission tomography (FDG-PET) images of a patient with oesophageal cancer prior to chemoradiotherapy. The primary tumour is demonstrated as an annular mass on both CT and CT-PET (a and b). Metabolically active hilar lymph nodes are present on PET/CT (d—black arrows). Lymph node spread was not detected on cross-sectional CT
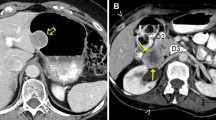
CT and 18F-fluorodeoxyglucose positron emission tomography (FDG-PET) images of a patient with locally advanced pancreatic cancer prior to chemo-RT. A poorly enhancing mass is seen in the body of the pancreas with evidence of vascular encasement (a). FDG avidity is observed to correspond with the mass at the junction between the body and tail of the pancreas (b)
Key Points
-
In GI malignancy, PET/CT is not standard in the planning procedure for these patients, but research is ongoing and most available data relates to rectal cancer.
-
Rectal Cancer
-
An overestimation of the rectal tumour diameter and volume using manual MRI-based measurements compared with PET-based contouring has also been reported.
-
FDG-PET/CT has been shown to reduce the interobserver variability in rectal tumour delineation.
-
Integration of PET in the RT planning process in rectal cancer has the potential to avoid geographical misses.
-
Oesophageal Cancer
-
Radiotherapy planning for oesophagogastric carcinomas is notoriously difficult because of poor tumour delineation on standard imaging.
-
FDG-PET has been observed to improve intra- and interobserver variability.
-
Using endoscopic ultrasound (EUS) as gold standard, FDG-PET facilitated a more accurate delineation of oesophageal tumour length compared with CT.
-
Pancreatic Cancer
-
FDG-PET fusion with planning CT has resulted in GTVs that were smaller overall compared with CT alone.
4 Summary
In the format that’s available to most clinicians at the present time, PET has significant limitations for radiotherapy planning [8]. Patient position, slice thickness and difficulties with co-registration mean that there can be an unrealistic reliance on the imaging available to our diagnostic systems. FDG-PET can be unreliable in distinguishing between benign and pathological lymph nodes because of non-specific FDG uptake within macrophages [9]. The development of PET tracers measuring cell proliferation and hypoxia has the potential to improve tumour specificity. Further work is required to validate their utility in the RT planning process, particularly in the setting of advanced radiotherapy techniques [10].
References
Krengli M, et al. Target volume delineation for preoperative radiotherapy of rectal cancer: inter-observer variability and potential impact of FDG-PET/CT imaging. Technol Cancer Res Treat. 2010;9(4):393–8.
Buijsen J, et al. FDG-PET-CT reduces the interobserver variability in rectal tumor delineation. Radiother Oncol. 2012;102(3):371–6.
Buijsen J, et al. FDG-PET provides the best correlation with the tumor specimen compared to MRI and CT in rectal cancer. Radiother Oncol. 2011;98(2):270–6.
Braendengen M, et al. Delineation of gross tumor volume (GTV) for radiation treatment planning of locally advanced rectal cancer using information from MRI or FDG-PET/CT: a prospective study. Int J Radiat Oncol Biol Phys. 2011;81(4):e439–45.
Seierstad T, et al. MR-guided simultaneous integrated boost in preoperative radiotherapy of locally advanced rectal cancer following neoadjuvant chemotherapy. Radiother Oncol. 2009;93(2):279–84.
Konski A, et al. The integration of 18-fluoro-deoxy-glucose positron emission tomography and endoscopic ultrasound in the treatment-planning process for esophageal carcinoma. Int J Radiat Oncol Biol Phys. 2005;61(4):1123–8.
Dalah E, et al. Variability of target and normal structure delineation using multimodality imaging for radiation therapy of pancreatic cancer. Int J Radiat Oncol Biol Phys. 2014;89(3):633–40.
MacManus M, et al. Use of PET and PET/CT for radiation therapy planning: IAEA expert report 2006–2007. Radiother Oncol. 2009;91(1):85–94.
Kantorova I, et al. Routine (18)F-FDG PET preoperative staging of colorectal cancer: comparison with conventional staging and its impact on treatment decision making. J Nucl Med. 2003;44(11):1784–8.
Roels S, et al. Biological image-guided radiotherapy in rectal cancer: is there a role for FMISO or FLT, next to FDG? Acta Oncol. 2008;47(7):1237–48.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Chong, I., Tait, D. (2017). GI Malignancy. In: Chua, S. (eds) PET/CT in Radiotherapy Planning . Clinicians’ Guides to Radionuclide Hybrid Imaging(). Springer, Cham. https://doi.org/10.1007/978-3-319-54744-2_10
Download citation
DOI: https://doi.org/10.1007/978-3-319-54744-2_10
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-54743-5
Online ISBN: 978-3-319-54744-2
eBook Packages: MedicineMedicine (R0)