Abstract
Esophageal cancer limited to the mucosa and low-risk submucosal adenocarcinoma, are associated with a low risk of lymph node and distant metastasis. For these early esophageal cancers, endoscopic treatment has evolved as a minimally invasive and organ preserving alternative to surgery. Endoscopic resection (ER) is the cornerstone of endoscopic therapy. ER not only removes neoplastic lesions, it also provides a substantial tissue specimen enabling accurate histological staging. Histological assessment of infiltration depth, grade of differentiation and presence of lymphovascular invasion are crucial in selecting patients who are eligible for further endoscopic management.
In patients with early adenocarcinoma arising in Barrett’s esophagus, a number of techniques are available to eradicate all Barrett’s mucosa after focal removal of early neoplastic lesions. Removal of all residual Barrett’s mucosa is advised to minimize the risk of metachronous lesions during follow-up.
In this book chapter we will give an overview of the indications for endoscopic treatment, different techniques that are available for endoscopic resection, management of the patient after focal removal of early cancer, and future perspectives on the place of endoscopic treatment for early esophageal cancer.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Esophageal cancer limited to the mucosa and low-risk submucosal adenocarcinoma, are associated with a low risk of lymph node and distant metastasis. For these early esophageal cancers, endoscopic treatment has evolved as a minimally invasive and organ preserving alternative to surgery. One of the largest series of 963 patients treated endoscopically for early esophageal adenocarcinoma demonstrated a long-term complete remission rate of 94%, with only two Barrett’s cancer related deaths [1]. Endoscopic resection is also well-established for patients with early squamous cell neoplasia of the esophagus, with cause-specific 5-year survival rates exceeding 85% [2]. Endoscopic resection (ER) is the cornerstone of endoscopic therapy. ER not only has a therapeutic goal, by removing neoplastic lesions, it also has important diagnostic value since it provides a substantial tissue specimen enabling accurate histological staging. Whereas surgical resection allows for removal of the affected organ and lymphadenectomy, ER is limited to local removal of neoplasia. Selection of patients suited for curative endoscopic therapy is therefore of the utmost importance and is aimed at identifying patients with a minimal risk of lymph node metastases. For this, accurate histological assessment of infiltration depth, grade of differentiation, presence of lymphovascular invasion and radicality of the resection at the deep resection margins in an ER-specimen are crucial.
ER was pioneered in Japan, where it is still mainly applied in the treatment of early gastric cancer and early squamous neoplasia of the esophagus [3]. During the last decades, endoscopic treatment has also been accepted as the treatment of choice in most Western countries, where it is mainly used in the management of patients with early neoplasia arising against a background of Barrett’s esophagus [1, 4].
In patients with Barrett’s neoplasia treated by ER, the residual Barrett’s mucosa is still at risk for metachronous lesions, which are found in up to 30% of patients during 5-year follow-up [4]. Therefore, additional treatment of residual Barrett’s mucosa after focal ER of neoplasia is advisable. For this, different approaches are available, of which thermal ablation using radiofrequency ablation (RFA) is currently most widely used [5, 6].
In this book chapter we will give an overview of the indications and principles of endoscopic treatment, different techniques that are available for endoscopic resection, management of the patient after focal removal of early cancer, and future perspectives on the place of endoscopic treatment for early esophageal cancer (Video 3.1).
2 Indications for Endoscopic Treatment
2.1 Adenocarcinoma Arising in Barrett’s Esophagus
Based on multiple high quality, international studies on ER for high-grade dysplasia (HGD) and mucosal adenocarcinoma (T1a), there is solid evidence that ER for mucosal adenocarcinoma is safe and associated with a minimal risk of lymph node metastasis [1, 4]. Therefore, ER has become first choice treatment for this indication in most countries [7].
Traditionally, the risk of lymph node metastasis in submucosal adenocarcinoma (T1b) was considered too high to offer these patients endoscopic follow-up after radical ER. However, this risk of lymph node metastases was mainly based on historical surgical series, from a period when exact depth of infiltration was of little clinical relevance for patient management [8]. Surgical specimens are generally cut in 5 mm slices; consequently, the area with the deepest tumour infiltration may have been missed, resulting in underestimation of the infiltration depth correlated with lymph node metastases if present. Endoscopic resection specimens are smaller and cut in 2 mm slices, resulting in more accurate assessment of tumour infiltration depth. Based on more recent studies in endoscopically treated patients, the risk of lymph node metastasis associated with submucosal cancer appears to be lower than generally assumed [9,10,11,12,13]. For low-risk submucosal adenocarcinoma, defined as radically resected submucosal adenocarcinoma limited to the upper 500 μm of the submucosa (T1sm1), well to moderately differentiated, without lymphovascular invasion, the risk of lymph node metastasis appears to be <2% [9, 10]. This is lower than the 0–4% mortality risk of esophagectomy in expert centres and low-risk submucosal cancer is therefore considered a relative indication for endoscopic treatment [9, 10].
For patients with T1sm1 adenocarcinoma but other high risk histological features (poor differentiation, lymphovascular invasion), or deeper submucosal adenocarcinoma (>500 μm, T1sm2-sm3), the exact risk of lymph node metastasis is unknown, but still considered too high to justify endoscopic therapy. However, a number of recent studies assessing infiltration depth in ER-specimens, suggest a risk of lymph node metastasis of 16–30% in patients with T1sm2-sm3 adenocarcinoma [11,12,13]. The gold standard in patients with T1sm2-sm3 adenocarcinoma is still surgical treatment, although based on these numbers >70% of these patients will undergo unnecessary esophagectomy. In the future better risk stratification of these patients taking other risk factors for metastatic disease such as differentiation and lymphovascular invasion into account may possibly result in a more tailored approach, only referring high-risk patients for surgery.
In Barrett’s esophagus the Paris classification is used to describe the morphological appearance of a lesion, which is related to infiltration depth of a lesion. Protruded lesions (Paris type 0-Is or 0-Ip) are defined as being higher than a closed biopsy forceps (2.5 mm), slightly elevated lesions (Paris type 0-IIa) are less high than a closed biopsy forceps and slightly depressed lesions (Paris type 0-IIc) are less deep than one cup of an open biopsy forceps [14]. In a study evaluating the relation between macroscopic appearance and infiltration depth, protruded lesions and slightly depressed lesions significantly more often infiltrated the submucosa (25–26%), than slightly elevated lesions (9%), or completely flat (Paris type 0-IIb) lesions (0%). None of the Paris type 0-I or type 0-II lesions are associated with a very high risk of submucosal invasion and diagnostic ER therefore appears indicated and safe for these lesions [15]. No good data are available on rate of submucosal invasion in type 0-III lesions, probably since the ulceration present in these lesions prohibits safe and radical ER of these lesions.
2.2 Early Squamous Cell Cancer of the Esophagus
Squamous cell cancer invades deeper and spreads to lymph nodes at an earlier stage when compared to esophageal adenocarcinoma, perhaps due to infiltration via the submucosal glandular structures, which are lined with squamous epithelium [16]. The indication for endoscopic treatment in patients with early squamous cell neoplasia is therefore more limited compared to early adenocarcinoma. Patients with high-grade intraepithelial neoplasia (HGIN) have no risk of lymph node metastasis and in case of cancer limited to the lamina propria (T1m1/m2) the risk of lymph node metastasis is minimal (0–5%) [16, 17]. These patients are candidates for curative endoscopic treatment. The risk of lymph node metastasis for squamous cell cancer invading the muscularis mucosae (T1m3) is about 0–12%, and in case of invasion into the superficial submucosa (T1sm1, <200 μm) the risk is about 20% [17]. For patients with T1m3/sm1 disease, endoscopic treatment may be considered if the patient suffers from significant comorbidity. Deeper submucosal invasion (T1sm2/3) is associated with >50% risk of lymph node metastasis and therefore warrants more aggressive therapy such as surgery or chemoradiation [17].
Just as in early esophageal adenocarcinoma, the macroscopic appearance of squamous cell neoplasia is described using the Paris classification, although lesion types are defined using different cut-off levels for elevation and depression. Macroscopic appearance can be used in deciding if a lesion is suited for ER. Excavated lesions (Paris type 0-III, deeper than half the cup of an open biopsy forceps) and more protruding lesions (Paris type 0-I, higher than the cup of an open biopsy forceps) are associated with deep submucosal invasion in >80% and should not be targeted for endoscopic resection. True flat type lesions (Paris type 0-IIb) are limited to the lamina propria in about 69% of cases, slightly depressed lesions (Paris type 0-IIc) in about 39% of cases and slightly elevated lesions (Paris type 0-IIa) are limited to the lamina propria in only 20% of cases [14]. Diagnostic endoscopic resection can therefore be considered for flat type squamous cell neoplasia.
3 Endoscopic Treatment Algorithm
After endoscopic detection of an early neoplastic lesion in the esophagus, endoscopic assessment of the morphological appearance of a lesion should guide the decision if ER is feasible, as described above. Biopsies can be obtained to confirm the diagnosis of cancer, but biopsies are not required, since the finding of a macroscopic abnormality warrants diagnostic ER to obtain a definite histological diagnosis. Additional imaging and staging with endoscopic ultrasound (EUS), CAT or PET scan prior to ER is generally not very useful during work-up for early esophageal neoplasia. EUS is not reliable in the differentiation between T1a and T1b cancers, and even discriminating T1 from T2 lesions may be challenging. And given the very low risk of lymph node and distant metastasis associated with early esophageal neoplasia, the yield of finding these with CAT or PET scanning is very low. The most important step during work-up of early esophageal neoplasia is therefore diagnostic ER, which provides a large tissue specimen, enabling accurate histological assessment of risk factors associated with lymph node metastasis. If there are no risk factors, the patient can be managed further endoscopically. If a patient is at high risk for lymph node metastasis based on the outcome of the diagnostic ER, additional staging can still be performed to decide on optimal further treatment. Optimal management for high-risk patients should be discussed during a multidisciplinary team meeting, including a gastroenterologist, surgeon and an oncologist.
After focal ER of early neoplasia arising in Barrett’s esophagus, the residual Barrett’s mucosa is at risk for recurrence [4]. Therefore additional treatment of the residual Barrett’s mucosa is advisable. This can be done by complete ER of the residual Barrett’s segment during subsequent ER sessions. This approach has been proven effective in patients with Barrett’s esophagus limited to 5 cm in length, however, complete radical ER is associated with a high risk of esophageal stenosis of up to 80% [18]. Thermal ablation of the Barrett’s mucosa is an alternative method to eradicate all mucosa at risk. Radiofrequency ablation (RFA) is the most extensively studied technique for this purpose [5, 6, 18].
Despite promising results of radiofrequency ablation (RFA) for true flat early squamous cell neoplasia (MGIN or HGIN) [19], no long-term follow-up data on this approach are available so far, and RFA is therefore not routinely used for this indication. Endoscopic management after focal removal of squamous cell neoplasia mainly consists of endoscopic follow-up at regular intervals to detect recurrences at an early stage.
4 Principles of Endoscopic Resection
4.1 Delineation and Marking of the Target Lesion
To ensure radical ER of a suspicious lesion with a disease free margin, it is important to delineate the extent of a lesion prior to ER. Advanced imaging techniques, such as virtual chromoendoscopy (e.g. narrow-band imaging, blue-laser imaging), zoom-endoscopy and chromoendoscopy (e.g. Lugol staining in case of early squamous neoplasia), may be helpful to assess the extent of a lesion. Since the endoscopic view during ER is often impaired by the use of distal attachment caps, submucosal lifting and bleeding, the target lesion is delineated by placing coagulation markings around its lateral margins. Especially for lesions that require piecemeal resection, demarcation with markings may be useful to achieve complete resection with a tumour free margin.
4.2 En-Bloc Resection Vs. Piecemeal Endoscopic Resection
Most conventional cap-based ER techniques allow for en-bloc resection of lesions with a maximum diameter of 2 cm. Larger lesions require resection in multiple pieces during a so-called “piecemeal” procedure. Piecemeal resections are technically more demanding, time-consuming and have a higher risk of complications. Piecemeal resection is also associated with a higher risk of local recurrence of neoplasia. However, this may be less relevant in patients with early neoplasia arising in Barrett’s esophagus, since the majority of these patients will undergo additional thermal ablation of their Barrett’s esophagus, minimizing risk of local recurrence [5, 6]. Piecemeal resections result in multiple resection specimens that cannot be easily pieced together and therefore histological evaluation of the radicality of a resection at the lateral resection margins is usually not reliable. Marking the lesion prior to ER and careful endoscopic assessment of the radicality of the resection after ER is therefore pivotal.
4.3 Endoscopic Resection Techniques
4.3.1 Lift-Suck-Cut Technique
Inoue et al. first described a cap-based ER technique, using a transparent distal attachment cap [3]. For this technique a transparent ER-cap with a distal rim is placed on the tip of an endoscope. The target lesion is lifted from the deeper esophageal wall layers by submucosal injection of saline. A crescent shaped snare is prelooped in the distal rim of the cap. After suctioning the lifted mucosa into the cap, the snare is closed and the captured mucosa can then be resected using electrocautery. ER-cap resections can be performed using a standard gastroscope and one assistant is needed to aid with the submucosal lifting and handling of the snare. A drawback of the ER-cap technique is that it is a technically demanding and time consuming procedure, especially when used for piecemeal resections. Prelooping the snare in the distal rim of the cap can be challenging, and for piecemeal resections submucosal lifting needs to be repeated for every resection.
4.3.2 Ligate-and-Cut Technique
The currently most widely used cap-based ER technique in the esophagus is the ligate-and-cut technique (Fig. 3.1). This technique is an easier alternative to the lift-suck-cut technique. For the ligate-and-cut technique a distal attachment cap, holding one or more rubber bands, is attached to the tip of the endoscope. The target lesion is sucked into the cap and by releasing a rubber band the mucosa is captured. This pseudo-polyp can then be resected with a snare. The ligate-and-cut technique can be performed using the multi-band mucosectomy device (Duette®, Wilson Cook, Limerick, Ireland), which has a transparent cap that holds six rubber bands and allows for passage of a snare through the accessory channel of the cranking device alongside the releasing wires, allowing resection after ligation without having to remove the endoscope [20]. The more recently developed Captivator™ Endoscopic Mucosal Resection Device (Boston Scientific Endoscopy, Marlborough, MA, USA) is a comparable device allowing ligate-and-cut ER. An advantage of the ligate-and-cut technique over the lift-suck-cut technique is that no submucosal lifting is required, since the rubber bands are not strong enough to hold in the deeper esophageal wall layers. This makes the ligate-and-cut technique easier and quicker to apply, especially when used for piecemeal procedures [20]. Despite the lack of submucosal lifting, the ligate-and-suck technique does not appear to be associated with a higher risk of complications as has been demonstrated in a randomized study comparing both techniques [20], and in a prospective registration of 1060 resections performed with the multiband mucosectomy device [21].
Endoscopic resection of an early cancer in a Barrett’s segment using the multiband mucosectomy technique. (a) Endoscopic view on a Paris type 0-Ia-IIb lesion. (b) The lateral margins of the lesion are marked using electrocoagulation markings. (c) View through the cap of the Duette multiband mucosectomy device holding the rubber bands. In the esophagus a pseudopolyp is created by suctioning the mucosa into the cap and releasing a rubber band. This pseudopolyp can subsequently be resected using an electrocautery snare. (d) View on the resected area, which shows that all markings have been removed, resulting in an endoscopically radical resection
4.3.3 Endoscopic Submucosal Dissection
Endoscopic submucosal dissection (ESD) is a technique that overcomes the problem of piecemeal ER for larger neoplastic lesions, and allows for a better-targeted resection of a lesion (Fig. 3.2). The concept of ESD is to incise the mucosa around a lesion, regardless how large, and then remove the lesion by visual submucosal dissection using an electrosurgical knife instead of blind snaring using a snare [22].
Endoscopic submucosal dissection (ESD) of an early squamous cell cancer. (a) Widespread, circumferential early squamous cell cancer. (b) Delineation of the most proximal extent of the lesion using electrocoagulation markings. (c) Delineation of the most distal extent of the lesion. (d) Submucosal lifting of the mucosa. (e) Circumferential incision of the proximal delineation margin. (f) Submucosal dissection using a dual-knife. (g–i) Result after extensive circumferential ESD
After careful delineation of a lesion and placement of coagulation markers around the margins of the lesion, the margins of the lesion are lifted by submucosal injection of fluid. Using an electrosurgical knife, the incision line can then be incised circumferentially around the lesion, while constantly repeating submucosal lifting to ensure a safe submucosal fluid cushion. When the incision around the lesion has been completed, the submucosa underneath the lesion can be dissected under constant visualisation, until the target lesion is removed in one piece. A range of different electrosurgical knifes are available for ESD.
Although ESD allows for en-bloc resection of neoplasia, it is technically demanding, time consuming and has a higher risk of complications. Therefore, ESD should only be applied in selected cases by experienced endoscopists with adequate training.
4.4 Histological Evaluation of ER Specimens
Endoscopic resection specimens are pinned down on cork or paraffin before fixating them in formalin. After fixation, specimens are routinely cut in 2 mm slices and embedded in paraffin. The tissue blocks are then sectioned, put on glass slides and stained with haematoxylin and eosin. In case of cancer, the pathologist will assess the following criteria:
-
1.
Tissue type (squamous, columnar).
-
2.
Presence of dysplasia or cancer, and in case of dysplasia the degree of dysplasia according to the Vienna classification [23].
-
3.
In case of invasive cancer, infiltration depth should be described as follows: infiltration into the lamina propria (T1m2); infiltration into the muscularis mucosae (T1m3); infiltration into the submucosa measured in microns. In surgical resection specimens, the submucosa is pragmatically divided into three equal parts (T1sm1 to T1sm3). However, ER specimens do not contain the whole thickness of the original submucosal layer. Therefore, the following cut-off levels are defined to describe depth of submucosal invasion in ER specimens: adenocarcinoma limited to the upper 500 μm of the submucosa is considered T1sm1, cancer infiltrating deeper than 500 μm is referred to as T1sm2/3; in squamous cancer the cut-off between T1sm1 and T1sm2/3 infiltration is 200 μm [14].
-
4.
Grade of differentiation (well, moderate, poor, undifferentiated).
-
5.
Presence of lymphovascular invasion.
-
6.
Radicality at the deep (vertical) resection margin.
-
7.
In case of en-bloc resection: worst histology at the lateral resection margins.
5 Endoscopic Ablation Techniques
5.1 Radiofrequency Ablation
Radiofrequency ablation (RFA) is the most widely studied thermal ablation method for Barrett’s esophagus (Fig. 3.3). RFA has demonstrated to result in complete eradication of intestinal metaplasia (89–92%) and neoplasia (95–96%), with or without prior ER of focal neoplastic lesions, with sustained complete remission of neoplasia and intestinal metaplasia in 90% of patients at 5 years [4, 5].
Radiofrequency ablation (RFA) of a long segment Barrett’s esophagus with high-grade dysplasia. (a) Long segment Barrett’s esophagus. (b) Circumferential RFA with the balloon-based catheter results in thermal ablation of the Barrett’s tissue. (c) After 3 months the esophagus has healed with neosquamous epithelium, and only a few small residual islands of Barrett mucosa remain. (d) Focal RFA of residual Barrett’s mucosa using the cap-based electrode fitted on the tip of the endoscope. (e, f) Three months after focal RFA, the esophagus is completely lined with normal appearing neosquamous mucosa
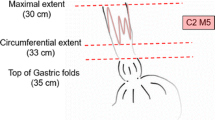
RFA is performed using a catheter with a bipolar electrode. Two main types of devices exist for RFA: a balloon-based ablation system (Barrx360, Medtronic, Minneapolis, MN, USA), which is inserted over a guide-wire and followed by the endoscope in a side-to-side manner. This system allows for circumferential ablation of Barrett’s mucosa, but requires a preliminary step of measurement of the esophageal inner diameter using a sizing balloon. A newly designed self-sizing RFA catheter (Barrx 360 Express, Medtronic, Minneapolis, MN, USA) has been developed in order to perform circumferential ablation without the need of the sizing step. For circumferential ablation using the balloon-based systems, the electrode is positioned 1 cm above the proximal extent of the Barrett’s mucosa. After inflation of the balloon, radiofrequency ablation is activated via a foot-pedal. One ablation results in a circumferentially treated area of 3–4 cm. By repositioning the ablation catheter in the esophagus, multiple ablations can be performed to treat the whole length of residual Barrett’s mucosa.
The second type of ablation system is a focal ablation catheter, attached to the tip of the endoscope, and designed to ablate tongues or islands of BE. Various sizes of focal RFA devices exist, but the Barrx90, allowing for a 90° ablation is the most commonly used. Depending on the length of the Barrett’s segment, patients are generally treated once with a circumferential RFA device followed by a median of two focal ablation sessions [4, 5].
5.2 Argon Plasma Coagulation
Argon plasma coagulation (APC) uses ionization of a jet of argon gas that is sprayed through a probe that is passed into the esophagus via the endoscope. The advantages of argon plasma coagulation (APC) are its easy availability and low costs. Disadvantages are that it is very operator-dependent, time-consuming and labour intensive approach, especially when used for treatment of a large surface of Barrett’s mucosa. Therefore, APC is mainly used to ablate small islands or tongues of Barrett’s mucosa. Recently, a modified APC probe called Hybrid APC (Erbe Elektromedizin, Tübingen, Germany) was introduced. This APC probe has a water-jet channel integrated into the probe, which allows for injection of saline into the submucosal space. By lifting the submucosa prior to thermal ablation, higher energy settings can be used, possibly increasing efficacy, while improving safety [24].
5.3 Photodynamic Therapy
Photodynamic therapy (PDT) is an endoscopic ablation technique that was applied to ablate Barrett’s mucosa with dysplasia in the past. PDT uses intra-venous administration of a photosensitizing drug that accumulates in the target tissue. Subsequent application of light (usually laser light) of an appropriate wavelength and the presence of oxygen results in a photodynamic reaction, which generates oxygen radicals causing delayed cell death, which usually becomes apparent after 12–24 h. However, due to disappointing efficacy results, high stricture rate and side-effects such as photosensitivity, PDT has become abundant, since better ablative alternatives are available nowadays.
5.4 Cryoablation
Cryoablation using either application of compressed CO2 gas via a cryospray catheter, or application via a balloon-based system, uses application of liquid nitrous oxide to freeze the esophageal mucosa. Deep freezing and slow thawing of the target area causes disruption of cells, vascular ischemia, and thrombosis, resulting in necrosis of the superficial esophageal layers. In contrast to heat-based ablation, cryoablation leaves the tissue architecture intact, and may result in less stricture formation. The balloon-based cryoablation device (C2 Therapeutics, Redwood City, California, USA) has recently proved feasible and safe in a prospective multicentre study in patients with Barrett’s esophagus [25].
Currently available data on hybrid-APC ablation and balloon-based cryoablation are still preliminary. Larger, multicentre studies will be required to define the place of these ablation techniques in the future management of patients with esophageal neoplasia.
6 Quality of Life
Endoscopic therapy is less invasive than surgery, but little is known about how this organ preserving approach influences quality of life. One study prospectively evaluated the effect of endoscopic treatment for early Barrett’s neoplasia on quality of life and fear of cancer (recurrence) and compared this with the effect of Barrett’s surveillance and surgery for early Barrett’s neoplasia and surgery for advanced esophageal adenocarcinoma [26]. The endoscopic treatment group reported significantly better physical and mental quality of life, and less esophageal cancer related symptoms compared to both surgical groups, as might be expected. However, the endoscopic treatment group reported significant more worry for cancer recurrence compared to the early surgical group. In fact, endoscopically treated patients worried about cancer and recurrence as much as patients treated surgically for advanced esophageal cancer. Further studies in this field are necessary to improve quality of life and counselling of patients undergoing endoscopic treatment.
7 Future Prospects of Endoscopic Therapy for Early Esophageal Cancer
The past decades the indication for endoscopic treatment has extended from high-grade dysplasia to mucosal cancer and even low-risk submucosal cancer. Small retrospective studies have shown that the risk of lymph node metastasis in deeper submucosal cancer may be <30%, implying that the majority of these patients will undergo unnecessary additional esophagectomy. Diligent prospective studies on endoscopic treatment in patients with submucosal cancer will hopefully result in better understanding of the true risk of lymph node metastasis associated with submucosal cancer. Risk stratification based on submucosal infiltration depth and other tumour characteristics may be of future use to select patients who would benefit from adjuvant surgery, and who can safely be kept under endoscopic surveillance.
Another development that may improve management of patients with submucosal cancer is use of a sentinel node procedure. Interesting studies in this field are currently being performed.
ESD will be performed more frequently, when the indication for endoscopic treatment is extended to more high-risk early esophageal cancers, where en-bloc resection should be aimed at. ESD is still technically demanding and should be performed by well-trained and experienced endoscopists. In the future, novel developments may facilitate ESD procedures.
Endoscopic management should be centralized in expert centres. Although ER and ablation benefit from technological developments, making the techniques easier to apply, these are just part of the overall endoscopic management of patients. The most important step is selecting the right patients for endoscopic management, starting with experience in detecting and delineating early esophageal neoplasia. After ER, also adequate histological evaluation of ER specimens is required to allow for adequate selection of low-risk patients. Furthermore, patient management should be discussed in a multidisciplinary team meeting, including gastroenterologists, surgeons and oncologists. Therefore, endoscopic management should be centralized in centres with multidisciplinary expertise in this field.
References
Pech O, May A, Manner H, et al. Long-term efficacy and safety of endoscopic resection for patients with mucosal adenocarcinoma of the esophagus. Gastroenterology. 2014;146:652–60.
Ono S, Fujishiro M, Niimi K, et al. Long-term outcomes of endoscopic submucosal dissection for superficial esophageal squamous cell neoplasms. Gastrointest Endosc. 2009;70:860–6.
Inoue H, Endo M, Takeshita K, et al. A new simplified technique of endoscopic esophageal mucosal resection using a cap-fitted panendoscope (EMRC). Surg Endosc. 1992;6:264–5.
Peters FP, Kara MA, Rosmolen WD, et al. Endoscopic treatment of high-grade dysplasia and early stage cancer in Barrett’s esophagus. Gastrointest Endosc. 2005;61:506–14.
Shaheen NJ, Sharma P, Overholt BF, et al. Radiofrequency ablation in Barrett’s esophagus with dysplasia. N Engl J Med. 2009;360:2277–88.
Phoa KN, Pouw RE, van Vilsteren FG, et al. Remission of Barrett’s esophagus with early neoplasia 5 years after radiofrequency ablation with endoscopic resection: a Netherlands cohort study. Gastroenterology. 2013;145:96–104.
Fitzgerald RC, di Pietro M, Ragunath K, et al. British Society of Gastroenterology guidelines on the diagnosis and management of Barrett’s oesophagus. Gut. 2014;63:7–42.
Westerterp M, Koppert LB, Buskens CJ, et al. Outcome of surgical treatment for early adenocarcinoma of the esophagus or gastro-esophageal junction. Virchows Arch. 2005;446:497–504.
Alvarez Herrero L, Pouw RE, van Vilsteren FG, et al. Risk of lymph node metastasis associated with deeper invasion by early adenocarcinoma of the esophagus and cardia: study based on endoscopic resection specimens. Endoscopy. 2010;42:1030–6.
Manner H, Pech O, Heldmann Y, et al. The frequency of lymph node metastasis in early-stage adenocarcinoma of the esophagus with incipient submucosal invasion (pT1b sm1) depending on histological risk patterns. Surg Endosc. 2015;29:1888–96.
Boys JA, Worrell SG, Chandrasoma P, et al. Can the risk of lymph node metastases be gauged in endoscopically resected submucosal esophageal adenocarcinomas? A multi-center study. J Gastrointest Surg. 2016;20:6–12.
Schölvinck DW, Künzli HT, Meijer SL, et al. Management of patients with T1b esophageal adenocarcinoma: a retrospective cohort study on patient management and risk of metastatic disease. Surg Endosc. 2016;30:4102–13.
Manner H, Wetzka J, May A, et al. Early-stage adenocarcinoma of the esophagus with mid to deep submucosal invasion (pT1b sm2–3): the frequency of lymph-node metastasis depends on macroscopic and histological risk patterns. Dis Esophagus. 2016 [Epub ahead of print].
The Paris endoscopic classification of superficial neoplastic lesions: esophagus, stomach, and colon: November 30 to December 1, 2002. Gastrointest Endosc. 2003;58:S3–43.
Peters FP, Brakenhoff KP, Curvers WL, et al. Histologic evaluation of resection specimens obtained at 293 endoscopic resections in Barrett’s esophagus. Gastrointest Endosc. 2008;67:604–9.
Araki K, Ohno S, Egashira A, et al. Pathologic features of superficial esophageal squamous cell carcinoma with lymph node and distal metastasis. Cancer. 2002;94:570–5.
Yoshii T, Ohkawa S, Tamai S, Kameda Y. Clinical outcome of endoscopic mucosal resection for esophageal squamous cell cancer invading muscularis mucosa and submucosal layer. Dis Esophagus. 2013;26:496–502.
Van Vilsteren FG, Pouw RE, Seewald S, et al. Stepwise radical endoscopic resection versus radiofrequency ablation for Barrett’s oesophagus with high-grade dysplasia or early cancer: a multicentre randomised trial. Gut. 2011;60:765–73.
He S, Bergman J, Zhang Y, et al. Endoscopic radiofrequency ablation for early esophageal squamous cell neoplasia: report of safety and effectiveness from a large prospective trial. Endoscopy. 2015;47:398–408.
Pouw RE, van Vilsteren FG, Peters FP, et al. Randomized trial on endoscopic resection-cap versus multiband mucosectomy for piecemeal endoscopic resection of early Barrett’s neoplasia. Gastrointest Endosc. 2011;74:35–43.
Alvarez Herrero L, Pouw RE, van Vilsteren FG, et al. Safety and efficacy of multiband mucosectomy in 1060 resections in Barrett’s esophagus. Endoscopy. 2011;43:177–83.
Terheggen G, Horn EM, Vieth M, et al. A randomised trial of endoscopic submucosal dissection versus endoscopic mucosal resection for early Barrett’s neoplasia. Gut. 2016 [Epub ahead of print].
Schlemper RJ, Riddell RH, Kato Y, et al. The Vienna classification of gastrointestinal epithelial neoplasia. Gut. 2000;47:251–5.
Manner H, May A, Kouti I, et al. Efficacy and safety of hybrid-APC for the ablation of Barrett’s esophagus. Surg Endosc. 2016;30:1364–70.
Schölvinck DW, Künzli HT, Kestens C, et al. Treatment of Barrett’s esophagus with a novel focal cryoablation device: a safety and feasibility study. Endoscopy. 2015;47:1106–12.
Rosmolen WD, Nieuwkerk PT, Pouw RE, et al. Quality of life and fear of cancer recurrence after endoscopic treatment for early Barrett’s neoplasia: a prospective study. Dis Esophagus. 2016 [Epub ahead of print].
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
1 Electronic Supplementary Material
EMR (MP4 218688 kb)
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this chapter
Cite this chapter
Pouw, R.E., Weusten, B.L.A.M. (2017). Endoscopic Treatment of Early Esophageal Cancer. In: Cuesta, M. (eds) Minimally Invasive Surgery for Upper Abdominal Cancer. Springer, Cham. https://doi.org/10.1007/978-3-319-54301-7_3
Download citation
DOI: https://doi.org/10.1007/978-3-319-54301-7_3
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-54300-0
Online ISBN: 978-3-319-54301-7
eBook Packages: MedicineMedicine (R0)