Abstract
Staphylococcus infection-associated glomerulonephritis (SAGN) is a well-recognized disease entity, and over the last decade has been seen with increasing frequency in western countries. The associated Staphylococcal infections tend to be quite aggressive and invasive and the affected population is primarily elderly patients with one or more preexisting comorbidities, which can make this a difficult disease to treat. Furthermore, the diagnosis can be challenging due to subtle clinical presentation of the underlying infection, varied histopathological features, and occasional positive ANCA serology. Importantly, the glomerulonephritis either coincides with the onset of infection or occurs during the course of the infection, which is in contrast to post-streptococcal glomerulonephritis which typically occurs after a distinct latent period following complete resolution of the infection. This chapter succinctly describes the wide spectrum of histologic features, immunofluorescence staining patterns and ultrastructural features in SAGN along with diagnostic pitfalls. The last section gives a brief overview of the microbiologic and immunologic aspects of Staphylococcus.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Iga-dominant Staphylococcus infection-associated glomerulonephritis
- Superantigen
- Methicillin-resistant Staphylococcus aureus (MRSA)
- Methicillin-sensitive Staphylococcus aureus (MSSA)
- Staphylococcus epidermidis
Introduction
Historically, glomerulonephritis due to underlying Staphylococcus infection was mostly seen in the setting of endocarditis, deep-seated visceral abscess, or infection associated with ventriculoatrial shunt. In fact, prior to the 1990s, only a few small studies had reported glomerulonephritis associated with an acute Staphylococcus infection involving other sites [1–7]. However, in more recent years, a number of publications have drawn attention to glomerulonephritis related to Staphylococcus infections involving a variety of sites, including cellulitis, osteomyelitis, and pneumonia, among others [8–24]. The earliest reports came from Japan and were subsequently followed by reports from the United States [8–26]. Most of the Staphylococcus infections were due to coagulase positive Staphylococcus aureus. Much less frequently, strains of coagulase negative Staphylococcus epidermidis have been implicated. Both methicillin-resistant (MRSA) and methicillin-sensitive (MSSA) strains have been reported. Pathogenetic mechanisms are still poorly understood, but Staphylococcal enterotoxins acting as superantigens are thought to play an important role by causing activation of large populations of T lymphocytes and massive cytokine release that results in immune complex glomerulonephritis occasionally accompanied by leukocytoclastic vasculitis [8, 9]. IgA and C3 immune complex deposition is frequently present.
Recent literature has used a variety of terms for glomerulonephritis associated with Staphylococcus infection, including IgA-dominant postinfectious glomerulonephritis or post-staphylococcal glomerulonephritis [19, 20, 22, 23], staphylococcal infection-associated glomerulonephritis mimicking IgA nephropathy [21], or staphylococcal superantigen-associated glomerulonephritis [8, 9]. It is probably best to not use the prefix ‘post’ so as to avoid confusion with post-streptococcal infection-associated glomerulonephritis (PSAGN), which is a distinct disease entity with defined epidemiology, treatment, and prognosis that differs from glomerulonephritis associated with Staphylococcus infections. We prefer the term Staphylococcus infection-associated glomerulonephritis (SAGN).
Over the recent years, SAGN has gained a lot of interest among both nephrologists as well as nephropathologists. The main reasons are as follows:
-
1.
In developed countries, SAGN is becoming more common. The rise in SAGN is likely primarily due to (i) the emergence of virulent, drug-resistant staphylococcal strains in both nosocomial and community-acquired settings [27, 28] and (ii) the increasing population of elderly patients (above 60 years old) with underlying comorbidities such as diabetes mellitus, malignancy, and postoperative status, which is the primary population at risk for SAGN [26, 29–31].
-
2.
In SAGN, the infection is frequently ongoing at the time the glomerulonephritis develops; thus, timely detection and treatment of the infection is most important since these infections are not self-limiting [32, 33]. In fact, typically the infection is persistent and difficult to treat, such as infected foot ulcers in diabetic patients, endocarditis, and osteomyelitis. Effective treatment usually requires early diagnosis and treatment with appropriate antibiotics possibly for a prolonged period of time.
-
3.
Clinical presentation is variable, and in some cases the clinical picture is confounded by lack of obvious signs of an active infection. In such cases, patients may present with nonspecific signs and symptoms such as worsening hypertension, lower extremity edema, fatigue, and renal dysfunction, and the possibility of an occult infection is only raised after review of a kidney biopsy that shows features suspicious for SAGN [32].
-
4.
By kidney biopsy findings alone, SAGN can be difficult to differentiate from IgA nephropathy and Henoch–Schönlein purpura (HSP) [11, 34–38]. However, distinction is critical because of treatment implications since treating SAGN with immunosuppressive therapy, including corticosteroids, is considered contraindicated in most instances due to the risk of sepsis [14, 34].
Epidemiology: Incidence and Demographics
The exact incidence of SAGN is difficult to estimate. At The Ohio State University Wexner Medical Center, we identified 78 cases of culture-proven SAGN out of a total of 9500 native kidney biopsies from January 2004 to April 2016 [39]. Thus, our data show that SAGN is infrequent (0.8% of native kidney biopsies); however, the true incidence is probably higher for a variety of reasons. One reason is that microbiological culture results are often delayed and unavailable at the time of the kidney biopsy. In fact, we found at least 30 additional kidney biopsies in our records with histologic and clinical findings highly suspicious for SAGN, but the cases were not included in our cohort since definitive culture results were not available. Additionally, incidence is difficult to define since many of the patients are treated early and empirically with antibiotics, which can result in subsequent negative cultures. Lastly, in many cases, the patient has an “occult” infection that is not clinically apparent; thus, evaluation for an underlying infection is delayed.
Similarly, other studies have reported an overall relatively low incidence of infection-associated glomerulonephritis in adults. Nasr et al. [20] identified five cases of IgA-dominant SAGN out of 4600 biopsy samples (0.1%) between 2000 and 2002. In a subsequent study, Nasr et al. [26] identified 93 cases (out of 10,080 biopsies; 0.9%) of “postinfectious” glomerulonephritis in elderly patients (great than or equal to 65 years) over a period of eleven years from 2000 to 2010. In this study, staphylococcal (50/109) as well as non-staphylococcal, including Streptococcus, Pneumococcus, Pseudomonas, and Enterococcus, infections were included. In 34% of the patients the infectious agent was unknown. In a report by Haas et al. [22], of the 6334 renal biopsies examined over a period of 4 years (2004–2007), 13 (0.2%) showed IgA-dominant infection-associated glomerulonephritis. Documented staphylococcal infection was present in 6 of 13 cases. Worawichawong et al. [23] reported an incidence of 0.8% (7 of 905) for IgA-dominant infection-associated glomerulonephritis, of which 4 of 7 had a proven underlying staphylococcal infection.
The majority of the patients with SAGN are older with a mean age of 55 ± 12 years; however, young adults with intravenous drug abuse are also a significant at risk group [39]. The age range in our cohort of 78 patients was 21–91 years. In our experience, men were affected more commonly than females (M:F ratio 3.5:1), and 95% of the patients were Caucasian with the remaining being African American or Asian. Rare case reports of SAGN in children also exist [40, 41].
Clinical Presentation and Laboratory Findings
Clinical and laboratory findings in our cohort of 78 patients with SAGN are listed in Table 2.1. SAGN is frequently seen in older patients with comorbidities such as long-standing diabetes mellitus, malignancy, severe trauma, recent surgery, indwelling catheter, chronic infections (including hepatitis C virus), and/or severe coronary artery disease requiring catheterization, bypass arterial grafting or stent placements. Intravenous drug abuse is also an important risk factor. In our study of 78 patients with SAGN, 32 (41%) had diabetes mellitus and 22 (28%) had hepatitis C virus infection. The association with hepatitis C virus infection may reflect the subset of patients that were intravenous drug abusers [39]. Although most patients with SAGN present with signs and symptoms indicative of an underlying infection, it is important to recognize that in some cases overt signs of infection may not be present. Patients may present with nonspecific symptoms such as worsening hypertension, increased swelling in lower extremities, fatigue, and/or poor appetite. Or perhaps the signs of an active infection are masked by other comorbidities such as congestive heart failure or diabetic complications. Sometimes the infection comes to attention only after the renal biopsy is performed for renal dysfunction [32]. According to the largest series from Japan, the average duration from detection of the infection to the glomerulonephritis is 5.4 weeks [10]. However, in patients with chronic open wounds such as cutaneous ulcers in diabetic patients or in surgical patients with open wounds, it can be difficult to determine when the infection started.
A variety of underlying infections have been described in patients with SAGN, including osteomyelitis [23], septic arthritis [3], discitis [15], pneumonia [6, 20], infected leg ulcers [17], skin infection, rectal abscess, other deep-seated abscesses, peritonitis, and pancreatitis [3, 7, 21] as well as unknown primary site of infection with positive blood cultures [7–9]. In our study of 78 patients with SAGN, 18 had endocarditis, 10 had bacteremia with unclear primary site of infection, 17 had osteomyelitis, one had septic arthritis, six had pneumonia, and 17 had an infected skin ulcer, most of which were diabetic patients [39]. The remaining ten patients had various other infections: post-surgical site infection, urinary tract infection, abdominal mesh infection, indwelling tunnel catheter infection, infected wounds related to motor vehicle accident, and deep-seated abscess (epidural abscess, scrotal abscess, and hip abscess). Five of the patients had multiple sites of infection at the same time, for example, endocarditis, pneumonia, and paraspinal abscess or pneumonia and abdominal abscess. In our experience, in diabetic patients with cutaneous ulcers, amputation, and/or gangrene, osteomyelitis can be an overlooked complication.
MRSA is the most frequently encountered infective organism in SAGN [3, 7–12]. In our study of 78 cases of SAGN, 42 patients had MRSA infection; 17 patients had MSSA infection; 3 patients had methicillin-resistant Staphylococcus epidermidis (MRSE); and 2 patients had methicillin-sensitive Staphylococcus epidermidis (MSSE) [39]. In the remaining patients, the exact speciation was not available (7 patients) or it was a mixed bacterial infection including Staphylococcus (7 patients). Positive blood cultures are commonly found with staphylococcal endocarditis infection. However, in other sites of infection, blood cultures are often negative. Culture studies from the actual site of infection tend to be more useful. Out of the 78 cases in our study, 38 (49%) had positive blood cultures, 43 (55%) had positive wound cultures, and 4 patients had both blood and wound cultures positive.
On physical exam, the patient’s blood pressure is typically moderately increased. Additionally, a subset of patients with SAGN present with a purpuric skin rash mimicking HSP, also termed IgA vasculitis [11, 34–38]. In our study of 78 patients, 16 (21%) patients with SAGN had a purpuric lower extremity skin rash [39]. Of note, skin biopsies show a leukocytoclastic vasculitis with mild IgA deposits [34]. Given the similarities to HSP, this presentation is a potential diagnostic pitfall (see differential diagnosis section).
Regarding laboratory findings, the most common presentation is acute renal failure with increased serum creatinine, microscopic hematuria, and proteinuria. Proteinuria can be nephrotic range with reports of greater than 10 g/day. Eight of the ten patients described by Koyama et al. [8] had nephrotic range proteinuria at one point during their disease course. Nasr et al. [26] reported proteinuria in the majority of their cohort of elderly patients with postinfectious glomerulonephritis, which was commonly nephrotic range (43%) with full nephrotic syndrome in 26% of patients. Patients usually have an active urine sediment with numerous red blood cells. Gross hematuria is not very common but can occur. Rarely, SAGN can be associated with a positive cryoglobulin test. We previously reported a case of SAGN with IgA/IgG-containing cryoglobulin-like deposits with circulating cryoglobulins, raising the possibility of IgA/IgG mixed cryoglobulin deposits [21]. Serum complement levels (especially C3) may be decreased, but can be normal. Among our 78 patients, complement data was available for 64 patients, and of those low C3 levels were seen in 19 patients (30%) and low C4 levels were seen in 9 patients (14%) [39]. Nasr et al. [26] reported hypocomplementemia in up to 72% of the patients in their series. Low C3 is more common than low C4. Lastly, ANCA serologies can be positive in SAGN [39, 42–49]. SAGN with ANCA positivity are typically cases with underlying endocarditis; however, cases with other sites of infection have been identified [39]. Boils et al. [42] reported ANCA positivity in 28% (8 out of 29 patients tested) of patients with endocarditis-associated glomerulonephritis. ANCA specificities can be pANCA (myeloperoxidase), cANCA (proteinase-3), dual specificity with both pANCA and cANCA, or atypical ANCA without known specificity. In our cases of SAGN, 22% (9 of 41) of the patients tested for ANCA had positive serology [39].
Kidney Biopsy Findings
Light Microscopy
Glomerular lesions in SAGN are those of an immune complex-mediated glomerulonephritis, but histomorphology can be variable and nonspecific. The light microscopic findings are usually that of mesangioproliferative (mesangial hypercellularity without closure of the capillary loops) and/or endocapillary proliferative immune complex glomerulonephritis with or without crescents as shown in Fig. 2.1. In our series of 78 patients, mesangial proliferation was the most commonly seen glomerular lesion with or without segmental endocapillary proliferation [39]. The glomerular mesangial hypercellularity can vary from mild and segmental to prominent and diffuse [5–7]. Of note, the mesangial hypercellularity may in some cases be masked by nodular mesangial matrix expansion secondary to underlying diabetic glomerulosclerosis (Fig. 2.1c). Based on the literature review and our experience, the light microscopic appearance of the glomeruli, including the degree of glomerular hypercellularity, and the clinical activity do not show a good correlation.
Spectrum of light microscopic morphology of glomerular lesions in SAGN. a Mesangial hypercellularity (H&E 400×). b Mesangial and segmental endocapillary hypercellularity (H&E 400×). c Underlying nodular diabetic glomerulosclerosis with superimposed mesangial hypercellularity (H&E 200×). d Intracapillary hypercellularity with predominance of neutrophils “exudative lesion” (Periodic Acid Schiff 40×). e Crescent formation (Jones methenamine silver 400×)
Endocapillary hypercellularity was seen in 47/78 (60%) SAGN biopsies in our cohort (Table 2.2) [39]. Out of these 47 biopsies, 26 had diffuse endocapillary hypercellularity with polymorphonuclear leukocytes (exudative lesions) resembling PSAGN (Fig. 2.1d). Some biopsies can show a membranoproliferative glomerulonephritis (MPGN)-type pattern of injury with thickening and duplication of capillary loops [20–23, 26, 29]. Crescent formation can occur, and approximately one-third of the SAGN cases in our study had crescents, ranging from small subtle segmental necrotizing lesions to large cellular crescents [21–23, 26, 29, 39], Fig. 2.1e. In the study of infection-associated glomerulonephritis by Nasr et al., 37% (40/109) of the biopsies had crescents with the majority of cases showing focal crescent formation [26].
Admixed fibrocellular crescents may also be seen, but they are much less common given the acute nature of the disease. Typically in SAGN with crescents, the glomeruli without crescents will be hypercellular. However, we identified a few cases characterized by crescents and/or necrotizing glomerular lesions in which the uninvolved glomeruli were not hypercellular [39]. Additionally, these cases had only mild immune complex deposition, overall reminiscent of ANCA-associated glomerulonephritis, which is a potential diagnostic pitfall (see differential diagnosis section). We have not seen vasculitis or fibrinoid necrosis in arteries in SAGN even in the presence of glomerular necrotizing lesions. Rarely, there can be extensive endocapillary hypercellularity with glomerular “hyalin thrombi”, reminiscent of cryoglobulinemia; however, the deposits in such cases lack microtubular substructure on ultrastructural examination.
Acute tubular necrosis (ATN) is seen in almost all cases, and red blood cell casts are frequently seen. Interstitial inflammation, although active-appearing, tends to be mild to moderate. Interstitial fibrosis and tubular atrophy depend on the underlying condition of the kidney. The tubulointerstitial findings do not always correlate with glomerular lesions. For example, there may be only mild mesangial hypercellularity without conspicuous endocapillary hypercellularity or crescents with numerous red blood cell casts and ATN. Vacular changes, if present, are secondary to underlying comorbidities (hypertension and diabetes mellitus).
Immunofluorescence Microscopy
SAGN characteristically contains IgA-dominant or codominant immune complex deposits [5–7, 11, 16, 17, 20–23, 29, 30, 32]. There is typically concurrent C3 staining and occasionally IgG (Fig. 2.2). This staining pattern is also seen in IgA nephropathy (Berger’s disease) and HSP (IgA vasculitis), creating a potential diagnostic pitfall (see differential diagnosis section). The IgA immunofluorescence staining in SAGN is granular in appearance, but the intensity and extent can vary. The staining intensity can range from trace (less than 1+) to strong. The majority of biopsies in our cohort showed mild to moderate (1 to 2+) IgA and moderate to strong (2 to 3+) C3 staining (Fig. 2.3) [39]. Of note, in a subset of cases of SAGN, the IgA staining is trace or negative (25% of SAGN biopsies in our study) (Figs. 2.5 and 2.6). IgA staining is seen predominantly in the mesangium but can also be seen segmentally along the glomerular capillary loops. IgA staining can also vary from one glomerulus to another within the same biopsy. Thus, in the presence of appropriate clinical history and morphologic findings, trace or even absent IgA staining does not exclude the possibility of SAGN. Fortunately, C3 staining is almost always present even when IgA staining is weak. C3 staining alone was seen in 11/78 (14%) of the biopsies in our series [39]. C3 staining tends to be strong, coarsely granular, and abundant, similar to that seen in PSAGN (Figs. 2.2, 2.3 and 2.4); however, there are cases of SAGN with mild to absent C3 staining (14% of cases in our study) as depicted in Figs. 2.5 and 2.6. Early components of the complement cascade, such as C1q and C4, are usually not seen. Particularly in diabetic patients, IgA and C3 staining can be strong, but by electron microscopy the deposits appear scant and/or are seen only along peripheral capillary loops around the expanded nodular mesangium.
Codominant granular IgG staining is seen in 40% of the SAGN biopsies in our study [39]. In diabetic patients, there is frequently smudgy IgG staining in the mesangium or linear staining along the glomerular capillary loops, which is a nonspecific staining pattern seen in diabetic glomerulosclerosis. Mesangial granular fluorescence for lambda light chain tends to be stronger than for kappa light chain in most cases, which is similar to IgA nephropathy. Staining for IgM tends to be quite inconspicuous. Strong fibrinogen staining can help identify focal segmental necrotizing lesions or crescents. Rarely, there is concomitant weak staining for all three immunoreactants (IgG, IgA and C3), which we label as “pauci-immune pattern” (13% in our study) [39].
We encountered three biopsies containing globular cryoglobulin-like glomerular capillary hyaline thrombi that lacked microtubular substructure on electron microscopy. In two of these biopsies the deposits showed strong staining for IgA and C3 with no IgG, and in the third biopsy there was strong IgG and C3 staining with no IgA.
Electron Microscopy
The degree of electron-dense immune complex deposition is variable. Most commonly, there are electron-dense deposits in the mesangium (Fig. 2.7a); however, subepithelial and occasional subendothelial deposits can also occur (Fig. 2.7b) [13, 17, 21, 26, 29, 30]. Mesangial electron-dense deposits can vary from a few scattered deposits to several easily identified deposits. These may be accompanied by small scattered intramembranous and/or subendothelial deposits. Rarely, large intraluminal and/or subendothelial electron-dense deposits are present, resembling cryoglobulin; however, these deposits lack microtubular substructure [21]. “Humps”, defined as large subepithelial deposits bulging outward beyond the boundary of the glomerular capillary basement membrane toward the Bowman’s space, are characteristic of PSAGN but are also seen in SAGN (Fig. 2.5c) [29]. Some studies have suggested that the presence of “humps” be a requirement for the diagnosis of SAGN; however, in our 78 cases of SAGN, “humps” were detected in only 31% of the biopsies [39]. Thus, we feel that “humps” are not required for a diagnosis of SAGN, and that the absence of “humps” does not exclude the possibility of SAGN. Of note, “humps” are not specific to infection-associated glomerulonephritides since they can be seen in other glomerular diseases such as C3 glomerulopathy, proliferative glomerulonephritis with monoclonal IgG deposition disease and, rarely, in lupus nephritis. Also, subepithelial “humps” may be seen in infection-associated glomerulonephritis caused by other pathogens as well, such as Gram negative bacteria and non-bacterial pathogens [29].
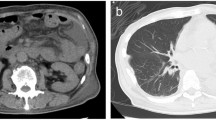
a 56 year old male with diabetes mellitus and infected leg ulcer and osteomyelitis. Biopsy showed numerous mesangial electron-dense immune-type deposits on ultrastructural examination (uranyl acetate and lead citrate fixation, 20,000×). b 47 year old male with MRSA and Pseudomonas infection and motor vehicle accident and multiple wounds. Biopsy showed mesangial and subendothelial electron-dense immune-type deposits on ultrastructural examination (uranyl acetate and lead citrate fixation, 5000×)
Etiology and Pathogenesis
In the 1970s Sato et al. [7] detected Staphylococcus aureus antigens within mesangial immune complex deposits in a small number of cases of diffuse proliferative glomerulonephritis. These patients also had antibodies against staphylococcal antigens (antistaphylolysin antibodies) in the sera, prompting the proposal that S. aureus has a pathogenic role in a small subset of diffuse proliferative glomerulonephritides. One hypothesis is that staphylococcal enterotoxins, typically enterotoxin C, A, or toxic shock syndrome toxin-1, act as superantigens that stimulate proliferation of resting T cells, resulting in exuberant T cell activation and ultimately B cell activation and immune complex formation [5, 7, 9, 12, 50]. Superantigens activate T cells by binding directly to the MHC class II molecules on antigen-presenting cells and then binding to the T cell receptor (TCR) Vβ region of T cells irrespective of TCR antigen specificity. As a result of this nonspecific binding, there is activation of large subsets of polyclonal T cells leading to a “cytokine storm”. Activated T cells then stimulate B cell proliferation and antibody production. In fact, in SAGN, polyclonal elevation of serum IgA and IgG, as well as circulating immune complexes, are frequently detected [5, 7, 11]. Hirayama et al. [36] studied six patients with “staphylococcus infection-induced HSP-like (IgA vasculitis) clinical syndrome with acute glomerulonephritis”, which can be considered cases of SAGN. These six patients with SAGN demonstrated skewed TCR Vβ chain usage (Vβ 5.2, 5.3 and 8) compared to normal controls and to patients whose S. aureus infection had improved. Additionally, they reported increased serum levels of cytokines (interleukins 1β, 2, 6, 8, and tumor necrosis factor-alpha) in patients with SAGN compared to normal individuals, and the cytokine levels normalized with resolution of the staphylococcal infection.
Staphylococcal enterotoxins acting as superantigens are also implicated in other diseases such as staphylococcal toxic shock syndrome. Of note, staphylococcal antigens may also play a role in IgA nephropathy. Koyama et al. [15] found the S. aureus cell envelope antigen in 68% of renal biopsy specimens from patients with IgA nephropathy and proposed that this antigen is a pathogenetic factor in the development of IgA nephropathy. The same group from Japan developed an experimental model of IgA nephropathy in mice following biweekly immunization of the animals with antigens derived from S. aureus mixed with Freund’s adjuvants [51]. Lastly, the comorbidities commonly present in patients with SAGN are likely contributing factors to pathogenesis by compromising the host immune response, which enables persistent infections/bacteremia and antigenemia that increases the likelihood of developing large antigen-antibody complexes that then accumulate in the glomerulus [26, 29, 30, 32].
Differential Diagnosis
Detailed clinical data are essential for a diagnosis of SAGN, and the main differential diagnostic considerations are:
-
1.
IgA nephropathy.
-
2.
Henoch–Schönlein purpura (HSP) or IgA vasculitis.
-
3.
Post-streptococcal glomerulonephritis (PSAGN).
-
4.
ANCA vasculitis.
-
5.
Other immune complex glomerulonephritides including C3 glomerulopathy, lupus nephritis, cryoglobulinemic glomerulonephritis.
-
6.
Warfarin-related nephropathy.
This is also shown in Table 2.3. Distinguishing between SAGN and idiopathic IgA nephropathy can be quite difficult using kidney biopsy findings alone since both entities frequently show mesangial hypercellularity with IgA and C3 dominant/codominant immune complex deposits. However, the clinical findings can be very helpful. A history of a staphylococcal infection with positive cultures or clinical features suspicious for an infection accompanied by acute renal failure, recent onset nephrotic range proteinuria, and/or hematuria with active urine sediment should raise the possibility of SAGN. IgA nephropathy is rarely associated with acute renal failure, unless it is crescentic IgA nephropathy or an advanced-stage IgA nephropathy with superimposed acute kidney injury due to other causes. In typical cases of progressive IgA nephropathy, the patients have a protracted, slowly progressive clinical course with long-standing microscopic hematuria, hypertension, and gradually worsening proteinuria. The “synpharyngitic” presentation of IgA nephropathy is characterized by episodic gross hematuria following upper respiratory tract infections (typically viral) and most of these patients lack acute kidney injury and nephrotic range proteinuria. If the kidney biopsy shows chronic glomerular lesions, such as segmental or global glomerular sclerosis, adhesions, or old fibrous crescents, IgA nephropathy can be favored since such chronic lesions are unusual in SAGN with the exception being when the chronic lesions are unrelated to SAGN (for example, glomerular changes of diabetic glomerulosclerosis). Endocapillary hypercellularity can be seen in both SAGN and IgA nephropathy, however, it is significantly more common in SAGN. In our study [39], it was present in 60% of the SAGN biopsies and 10% of the IgA nephropathy biopsies (Table 2.2). Focal segmental glomerular sclerosis (FSGS) lesions on the other hand are more frequently seen in IgA nephropathy (49% of the biopsies) as compared to SAGN (2.5% biopsies). Also, the intensity of IgA and C3 staining is different between SAGN and IgAN. Although there is a spectrum of staining in SAGN as mentioned previously, the IgA staining intensity tends to be mild to moderate (1+ to 2+) and C3 tends to be moderate to strong (2+ to 3+) in SAGN while in IgAN staining for IgA is more frequently moderate to strong (2+ to 3+) and C3 staining is mild to moderate (1+ to 2+) [39].
Since a subset of patients with SAGN develop a purpuric rash with leukocytoclastic vasculitis, it can be difficult to distinguish SAGN from HSP (IgA vasculitis) [18, 34–38]. Similar to IgA nephropathy, the kidney biopsy findings can be indistinguishable between the two entities. Again a detailed clinical history, particularly the presence of an underlying staphylococcal infection, is imperative. Also, since HSP is a rare disease in adults, in our experience, it is more common to see SAGN with purpuric skin lesions rather than HSP. Therefore, if an adult patient presents with symptoms of HSP vasculitis and a renal biopsy shows IgA-dominant glomerulonephritis, an underlying Staphylococcus infection should be excluded prior to initiation of immunosuppressive therapy since such treatment in the setting of an active infection can result in sepsis [11, 34–38].
It is important to recognize the differences between SAGN and PSAGN. In developed countries, the incidence of PSAGN has declined due to successful treatment of acute streptococcal infections with antibiotics; however, SAGN is becoming more common. One of the major differences in SAGN and PSAGN, other than the causative bacterial organism, is that in SAGN the infection is frequently ongoing at the time the glomerulonephritis develops. Conversely, in PSAGN the glomerulonephritis develops after the streptococcal infection has completely resolved, either spontaneously or after antibiotic treatment [32, 33]. Although the light microscopic and ultrastructural findings can be similar in SAGN and PSAGN, especially in cases of SAGN with “humps”, the presence of IgA in the immune deposits would be unusual in PSAGN. The overall frequency of “humps” is much less in SAGN (only 31% in our cohort) compared to PSAGN, where such lesions are characteristic [39]. Lastly, there is general agreement that the renal prognosis in cases of “glomerulonephritis with active infection” is guarded in sharp contrast to the good prognosis associated with PSAGN in children [13, 21–23, 26, 29, 30].
SAGN can have crescents and/or segmental necrotizing glomerular lesions sometimes with very minimal immune complex deposition; thus, pauci-immune or ANCA-associated crescentic and necrotizing glomerulonephritis can be included in the differential diagnosis [39, 52]. Furthermore, SAGN can be associated with positive ANCA serologies, particularly in cases with underlying endocarditis [39, 42–49]. Boils et al. [42] recently studied endocarditis-associated glomerulonephritis of which 53% were associated with S. aureus (23% Streptococcus species, 9% culture negative, and the remaining were associated with Bartonella henselae, Coxiella burnetti, Cardiobacterium hominis, or Gemella species). Crescents and/or segmental necrotizing lesions were seen in 53% of the kidney biopsies. Additionally, 28% of patients had a positive ANCA serology. In our case series of SAGN, 35% (27/78) of the biopsies had focal crescents and/or segmental necrotizing lesions [39]. Six of these 27 also showed a pauci-immune pattern by immunofluorescence and electron microscopic examination. One biopsy showed both crescents and a pauci-immune pattern accompanied by positive ANCA serology, thus closely mimicking ANCA-associated glomerulonephritis.
There have been similar reports of pauci-immune crescentic and necrotizing glomerulonephritis associated with staphylococcal infections [10, 15]. In fact, the possibility that S. aureus may play a role in the pathogenesis of ANCA-associated granulomatosis with polyangiitis (previously known as Wegener’s granulomatosis) has been proposed [24]. An additional confounding factor relevant to this differential diagnosis is that in 2–3% of kidney biopsies there is incidental, non-pathologic IgA staining; thus, it is possible, albeit infrequent, to have mild IgA staining in pauci-immune ANCA-associated crescentic and necrotizing glomerulonephritis. Of note, the definition of “pauci-immune” can differ slightly between pathologists. Our definition is weak to absent immunofluorescence staining for immunoglobulins (mainly IgG and IgA) and complement C3 in combination with scant to absent electron-dense immune-type deposits on ultrastructural examination. Although some may consider C3 staining alone in the absence of immunoglobulins as “pauci-immune” (described in the endocarditis chapter), we do not label such staining as “pauci-immune”. In fact, 11 of our 78 cases of SAGN contained C3 staining alone. Additionally, rarely, there is discordance between the degree of immunofluorescence staining and deposition of immune-type deposits assessed by ultrastructural examination. In such cases, it is possible that the electron-dense deposits do not stain because of hidden epitopes.
Distinguishing between SAGN and ANCA-associated glomerulonephritis is crucial since immunosuppressive therapy used to treat ANCA-associated glomerulonephritis is contraindicated in the setting of an active S. aureus infection. After the infection is cleared, if renal dysfunction persists and there are active crescents seen in the biopsy, a cautious trial of corticosteroids is recommended by some, but this remains a controversial issue [53, 54]. It is therefore important to interpret the biopsy in light of a detailed clinical history. Also, if the biopsy shows distinct vasculitis and/or fibrinoid necrosis of the arteries, then ANCA vasculitis is favored even if there is mild IgA staining or a few immune-type deposits present. Also, the uninvolved glomeruli tend to be hypercellular in SAGN but not so in ANCA-associated glomerulonephritis.
Since SAGN can have a membranoproliferative glomerulonephritis (MPGN)-type pattern of glomerular injury with immune complex deposition, other immune complex glomerulonephritides with MPGN-type morphology can enter the differential diagnosis, including C3 glomerulopathy, lupus nephritis, and cryoglobulinemic glomerulonephritis. C3 glomerulopathy is characterized by C3 deposits with absent immunoglobulin components, thus, may be confused with cases of SAGN with absent or weak IgA and strong C3 staining. Lupus nephritis typically has a “full house” staining pattern with more IgG, IgM, and C1q staining compared to SAGN. Lastly, hyaline thrombi resembling cryoglobulin deposits can rarely be seen in association with bacterial infections, and the patients may have mixed type III cryoglobulinemia. We identified three biopsies in our series of 78 cases of SAGN that contained large cryoglobulin-like immune complex deposits [21]. These however did not show microtubular substructure as typically seen in cryoglobulinemic glomerulonephritis. Fortunately, in most instances SAGN can be differentiated from other MPGN-type immune complex glomerulonephritides using a combination of kidney biopsy findings, a detailed clinical history (presence of infection, systemic lupus erythematosus, Hepatitis C virus infection, etc.), and thorough laboratory work-up (autoimmune serologies, cryoglobulin testing, rheumatoid factor level, C3 and C4 complement levels, culture results, etc.).
SAGN can be associated with prominent intratubular red blood cells and red blood cell casts; thus, in patients on anticoagulation therapy, warfarin-related nephropathy can be included within the differential diagnosis. If a biopsy from an anticoagulated patient shows prominent ATN and numerous red blood cell casts, but only mild mesangial hypercellularity and a few immune-type deposits, a diagnosis of warfarin-related nephropathy may be rendered when SAGN is the true cause of the renal dysfunction. SAGN with concurrent warfarin-related nephropathy can be difficult to definitively diagnose. Of note, the risk of warfarin-related nephropathy is greater in the presence of a glomerular disease. In such cases, the possibility of concomitant warfarin-related nephropathy should be discussed with the nephrologist and the coagulation parameters should be closely monitored.
Clinical Course and Outcome
The prognosis in adults with SAGN is guarded since a significant proportion of adults does not recover and have persistent renal dysfunction or progress to end-stage renal disease. Persistent renal dysfunction develops in 8–54% of patients and progression to end-stage renal disease in 4–33% of patients as described in several case series [21, 26, 29, 30, 55, 56]. Poor prognostic indicators in adults include older age, higher serum creatinine at biopsy, tubulointerstitial scarring, and presence of underlying debilitating conditions [21–23, 26, 29]. The goal of treatment should be eradication of the underlying S. aureus infection and management of comorbidities that may be present, such as diabetes, hypertension, congestive heart failure, and surgical complications [29, 56, 57]. Regarding treatment of the infection, appropriate antibiotics are crucial and surgical debridement of the infected wound or abscess drainage may also be necessary [14, 58]. In severe cases of diabetes, amputation of the infected lower extremity may be required to bring the infection under control. Of note, some antibiotics commonly used to treat staphylococcal infections, such as vancomycin, can be nephrotoxic, causing acute tubular injury with or without interstitial nephritis. In such instances, it can be difficult to determine the cause of persistent renal dysfunction. Therapeutic monitoring of drug levels, particularly vancomycin levels, may be helpful in the evaluation for drug-induced renal dysfunction.
The role of immunosuppressive therapy, including corticosteroids, in adult patients with ongoing SAGN is highly controversial and considered contraindicated in most instances. There are no randomized prospective clinical trials on the role of corticosteroids in this condition. The available data are based on retrospective studies. Corticosteroid use has been reported in patients with an accompanying leukocytoclastic vasculitic skin rash mimicking HSP (IgA vasculitis) with some reports of resolution of the rash following steroid therapy [34–37]. Also, there are a few case reports that describe good results with the use of corticosteroids in the treatment of infection-associated glomerulonephritis in adults [53, 54]. However, there are also studies that show no improvement or worsening renal function as well as the development of sepsis in patients with SAGN treated with corticosteroids [34]. None of the case series with statistical analyses have found a significant benefit on outcome with the administration of corticosteroids [21, 26, 29, 30, 34, 55, 56]. Thus, based on the absence of any proven benefit and the potential risk of sepsis, immunosuppressive therapy, including corticosteroids, is generally not recommended in adults with SAGN. Treatment of SAGN and other infection–associated glomerulonephritides is discussed in detail in Chap. 5.
Staphylococcus Species—Microbiological and Immunological Aspects
Although there are more than 30 species in the genus Staphylococcus, S. aureus and S. epidermidis are responsible for the majority of staphylococcal infections in man [59]. S. epidermidis is a commensal organism of the skin and has emerged as a potential pathogen primarily due to the use of implantable and indwelling medical devices such as central venous catheters. S. aureus, the more pathogenic of the two species, is a commensal organism colonizing the moist squamous epithelium of the anterior nares as well as the nasopharynx, groin, and perineum [60, 61]. Permanent and transient colonization of S. aureus is noted in approximately 20% and 60% of the population, respectively [60]. S. aureus is exposed to innate and induced immune responses when it colonizes the nasal mucosa, and the immune status as well as other host factors play an important role in nasal colonization [59]. For example, polymorphisms in the glucocorticoid receptor, C-reactive protein, mannose binding lectin, complement factor H, and interleukin 4 gene promoter (which influences mucin secretion) have all been associated with increased or decreased carriage rates [59]. It is thought that S. aureus has intrinsic pathogenic potential due to the acquisition of virulence factors and immune avoidance mechanisms necessary to overcome the innate and induced immune responses present in the nasal-associated lymphoid tissue of the nares [59]. S. aureus can cause mild to severe superficial skin and soft tissue infections such as abscesses or impetigo as well as serious invasive infections, including endocarditis, bacteremia, pneumonia, osteomyelitis, septic arthritis, among others [27, 28]. Colonization by S. aureus is a risk factor for invasive disease both in the hospital and the community [62–64]. Particularly in hospitalized patients, indwelling medical devices, compromised immune system, and/or postoperative status increases risk of infection [28, 65]. In the community setting, poor personal hygiene and a compromised skin barrier likely play important roles in developing S. aureus infections. Transmission of S. aureus from an infected to an uninfected person can occur through direct skin-to-skin contact or through contaminated fomites in public and household settings [66].
Staphylococcus aureus has been implicated in human infections since prehistoric times [67]. Penicillin, introduced in the 1940s, was the first antimicrobial drug effective against staphylococcal infections; however, S. aureus developed penicillin resistance within a few months via a plasmid-encoded beta-lactamase gene capable of cleaving the beta-lactam ring of penicillin [68–71]. Methicillin, a derivative of penicillin resistant to cleavage by beta-lactamase, was introduced in 1959; however, within 2 years, methicillin-resistant strains (MRSA) were identified [28]. Methicillin-resistant strains acquired the mobile genetic element, staphylococcal chromosome cassette mec [SCCmec], which harbors the mecA gene that encodes a penicillin-binding protein with reduced affinity toward methicillin [72–74]. Thus, there is less efficient binding of methicillin to the bacterium, ultimately resulting in reduced capacity to inhibit bacterial cell-wall synthesis. Of note, according to the Centers for Disease Control and Prevention, the definition of methicillin-resistance includes resistance of S. aureus not only to methicillin but also other related and more commonly used antibiotics such as oxacillin and amoxicillin [28]. Furthermore, the mecA gene provides resistance to many beta-lactam antibiotics, including penicillin, and SCCmec elements may also contain genes enabling resistance to a variety of non-beta-lactam antibiotics. Beta-lactams are the typical first line antibiotic in the treatment of staphylococcal infections. However, given the acquisition of resistance to these drugs, treatment of S. aureus infection relies increasingly on non-beta-lactam-based antibiotics [75]. Although vancomycin is most commonly used in the treatment of MRSA infection, other drugs, namely linezolid, daptomycin, and tigecycline, are also effective against MRSA infections [76, 77]. Unfortunately, strains of S. aureus resistant to these drugs have been reported [78–81].
MRSA is the most prominent cause of nosocomial infections caused by a single bacterial pathogen in the USA, and it is estimated that MRSA causes approximately 44% of all hospital-associated infections [28, 82]. MRSA infections were largely health-care associated (HA-MRSA) until the late 1990s, when otherwise healthy individuals in the community began to develop MRSA infections reaching epidemic proportions (community-acquired MRSA [CA-MRSA]) [83]. HA-MRSA infection is defined by the onset of infection occurring after 48 hours of hospital admission while the onset of CA-MRSA infections is within 48 hours of admission to the hospital with no previous history of hospitalization in the past year [84]. While specific strains are typically associated with either HA-MRSA or CA-MRSA infections, the CA-/HA-MRSA definition is clinical, not microbiological, since strains have successfully transferred between the two settings. For example, the highly pathogenic CA-MRSA strain USA300 was first isolated in the year 2000 as a community-associated strain, but has since spread across the globe and represents a major threat in hospital and long-term care facilities as well as the community setting [85–89].
The marked virulence of S. aureus is largely due to:
-
Resistance to a wide spectrum of antimicrobial agents
-
Ability to evade host immunity.
Antimicrobial Resistance
The main determinants of resistance include the plasmid-encoded beta-lactamase gene and the mecA gene encoded on the mobile genetic element SCCmec, as discussed previously. Other molecular determinants of resistance and well as virulence are encoded on other mobile genetic elements; thus, the presence of these factors is highly strain-dependent [28].
Immune Evasion
This is an extensive topic discussed in detail in several review articles [65, 90]. It is beyond the scope of this book to describe the immune evasive mechanism of Staphylococcus in detail, but the important points will be highlighted.
-
1.
Efficient adhesion and colonization
Staphylococcus aureus expresses surface proteins that promote adhesion to damaged tissue and to the surface squamous epithelium [91]. Several surface proteins have been found that promote adhesion of S. aureus to squamous cells in vitro. Critical surface proteins include clumping factor B (ClfB) and iron-regulated surface determinant (Isd) [59]. ClfB can bind to fibrinogen as well as to cytokeratin 10, which is exposed on the surface of squamous cells [92]. Isd is involved in iron acquisition and promotes survival in the iron-deficient environment of the nasal mucosa and skin as well as promotes adhesion to squamous epithelium [59, 93].
There are a few features of certain staphylococcal species that promote survival on the skin. One is the presence of the arginine catabolic mobile element (ACME) that contains a cluster of genes encoding enzymes that produce ammonia that is thought to aid pH homeostasis in the acid environment of the skin [94]. ACME is present in certain strains of S. epidermidis and S. aureus. Additionally, S. aureus produces Isd that essentially protects the bacteria from bactericidal fatty acids present in the sebum of the skin [95].
Staphylococcus epidermidis is normally a harmless commensal of the human skin, however, can be pathogenic due to its ability to colonize implanted medical devices and form biofilms [59]. Biofilms are multilayered, high-density structures that protect bacteria from antibiotics and the human immune system. Initially, S. epidermidis adheres to the biomaterial by surface-associated proteins such as major autolysis AtlE or fibrinogen-binding proteins Fbe/SdrG. S. aureus can also form biofilms via binding to the biomaterial by surface-associated proteins such as clumping factor A (ClfA) and fibronectin-binding proteins. Multilayered biofilms are typically help together by the charged polymer polysaccharide intercellular adhesion (PIA) [96].
Staphylococcus aureus can bind to resting platelets and activate them resulting in platelet aggregation [97]. The bacteria can then grow in platelet-fibrin thrombi where they evade detection by neutrophils. Fibronectin-binding proteins and ClfA are bacterial proteins involved. This process is thought to be an important factor in endovascular infections/infective endocarditis.
-
2.
Inhibition of neutrophil migration and resistance to phagocytosis
Staphylococcus aureus has developed mechanisms that compromise innate, humoral and cell-mediated immunity [65]. S. aureus can secrete several small proteins that interfere with different stages of neutrophil recruitment: staphylococcal superantigen-like (SLL) 5 and SSL11 inhibit neutrophil rolling on activated endothelial cells; MHC class II analog protein (Map) inhibits neutrophil transmigration through endothelial cells (diapedesis); and chemotaxis inhibitory protein of staphylococci (CHIPS) and formyl peptide receptor like-1 inhibitory protein (FLIPr) inhibit chemotactic migration of neutrophils to the site of infection [59]. Efficient phagocytosis of bacteria by neutrophils and macrophages requires recognition of bound complement and antibody. S. aureus can interfere with the complement pathways and antibody deposition, ultimately preventing opsonization and phagocytosis [59]. Staphylococcus complement inhibitor (SCIN) essentially inhibits complement activation and subsequent phagocytosis by preventing production of the C3a chemoattractant peptide and opsonin C3b peptide [98]. S. aureus can also reduce phagocytosis by cleaving/inactivating complement factor C3b as well as IgG molecules that are bound to the surface of opsonized bacterial cells by secreting staphylokinase, a plasminogen activator protein [99]. Additionally, S. aureus can activate factor I, which is a natural downregulator of complement fixation [100]. Other S. aureus proteins, such as Protein A, clumping factor A, and extracellular fibrinogen-binding protein (Efb), also have antiphagocytic effects via various mechanisms [59, 65, 101]. Lastly, the capsule of certain staphylococcal species appears to have anti-opsonic properties, possibly related to the particular capsular polysaccharide as well as PIA.
-
3.
Survival inside the host immune cell
Staphylococcus aureus has multiple mechanisms that enable it to survive in phagosomes [59]. The organism can modify its cell wall teichoic acid and membrane lipids, reducing the surface negative charge and ultimately diminishing the effectiveness of cationic antimicrobial defensin peptides that are secreted into the phagosomes. Secreted factors such as staphylokinase and metalloprotease aureolysin as well as PIA also likely contribute to the neutralization of antimicrobial peptides [102–104]. Furthermore, within the phagosome, S. aureus can neutralize reactive oxygen intermediates formed during the respiratory burst as well as nitric oxide radicals [59]. The bacterial cell wall peptidoglycan is also resistant to lysozyme, a bactericidal protein important in the innate immune response [105]. Not only can S. aureus survive in neutrophils and macrophages, there is evidence that it can invade and survive within nonprofessional phagocytes such as endothelial and epithelial cells, allowing escape from host immunity [59].
-
4.
Toxins produced by S. aureus
Several cytolytic toxins are produced by S. aureus that target and damage the cytoplasmic membranes of host cells [59]. Some of the well-known toxins include α-toxin, γ-toxin (γ-hemolysin), Panton–Valentine leukocidin (PVL), and leukocidin E/D. The γ-toxin can lyse both erythrocytes and leukocytes while PVL targets only leukocytes. S. aureus can secrete several cytolytic peptides that at high concentrations can cause neutrophil lysis. Furthermore, S. aureus can secrete extracellular enzymes, including various proteases, hyaluronidases, lipases and nucleases, which result in tissue destruction and host cell lysis as well as facilitate bacterial spread [65].
-
5.
Immunomodulatory molecules, including superantigens
Staphylococcus aureus can secrete powerful T cell mitogens, termed superantigens, resulting in altered T cell function associated with exuberant T cell activation and proliferation as well as release of pro-inflammatory cytokines, such as tumor necrosis factor-alpha and interleukin (IL)-beta, and T cell mediators, such as IL-2 [59, 106]. Furthermore, superantigen expression can prevent the development of a normal immune response. Superantigens bind to the MHC Class II molecule on the surface of antigen-presenting cells outside of the peptide-binding groove region and then bind to the T cell receptor (TCR) of T helper cells via the variable region of the TCR β-chain [106]. Binding occurs without the need for the MHC Class II molecule to present an antigenic peptide to a suitable T cell. Each superantigen recognizes a specific subset of TCR Vβ chains and therefore has a characteristic Vβ signature. Up to 30% of T cells can become activated in extreme cases leading to very high levels of cytokines causing toxic shock syndrome [59, 107]. Superantigens prevent normal immune response since in the presence of superantigens antigen-specific T cells fail to proliferate in response to antigens that are presented normally by MHC Class II [107, 108]. This superantigen-induced anergy likely contributes to the diminished targeted antibody response and compromised immunological memory associated with S. aureus infections [59, 65]. Of note, protein A, which has antiphagocytic effects, also has immunomodulatory properties by promoting depletion of antibody secreting B cells in the spleen and bone marrow [109].
In summary, staphylococcal organisms, particularly S. aureus, can evade human immune responses through a variety of mechanisms directed toward both innate and acquired immune defenses. Some of them are summarized below.
-
1.
Efficient colonization of skin and mucosal surfaces and formation of biofilms that promote bacterial survival.
-
2.
Binding to and activating platelets to form platelet-fibrin thrombi with subsequent neutrophil evasion, particularly important in the pathogenesis of endocarditis.
-
3.
Interfere with neutrophil recruitment.
-
4.
Resist phagocytosis through surface and secreted anti-opsonic proteins in addition to the polysaccharide capsule.
-
5.
Intracellular survival in the phagosome by neutralizing antimicrobial peptides and reactive oxygen species.
-
6.
Secretion of cytolytic toxins that damage cytoplasmic membranes of immune cells.
-
7.
Immunomodulatory molecules can result in altered T and B cell functions, ultimately preventing the development of normal cell-mediated and humoral immune responses to infection.
References
McIntosh RM, Griswold WR, Chernack WB, Williams G, Strauss J, Kaufman DB, et al. Cryoglobulins. III. Further studies on the nature, incidence, clinical, diagnostic, prognostic, and immunopathologic significance of cryoproteins in renal disease. Q J Med. 1975;44(174):285–307.
Danovitch GM, Nord EP, Barki Y, Krugliak L. Staphylococcal lung abscess and acute glomerulonephritis. Isr J Med Sci. 1979;15(10):840–3.
Maher ER, Hamilton DV, Thiru S, Wheatley T. Acute renal failure due to glomerulonephritis associated with staphylococcal infection. Postgrad Med J. 1984;60(704):433–4.
Salyer WR, Salyer DC. Unilateral glomerulonephritis. J Pathol. 1974;113(4):247–51. doi:10.1002/path.1711130409.
Pola E, Logroscino G, De Santis V, Canducci F, Delcogliano A, Gasbarrini A. Onset of Berger disease after Staphylococcus aureus infection: septic arthritis after anterior cruciate ligament reconstruction. Arthroscopy. 2003;19(4):E29. doi:10.1053/jars.2003.50118.
Spector DA, Millan J, Zauber N, Burton J. Glomerulonephritis and Staphylococcal aureus infections. Clin Nephrol. 1980;14(5):256–61.
Sato M, Nakazoro H, Ofuji T. The pathogenetic role of Staphylococcus aureus in primary human glomerulonephritis. Clin Nephrol. 1979;11(4):190–5.
Koyama A, Kobayashi M, Yamaguchi N, Yamagata K, Takano K, Nakajima M, et al. Glomerulonephritis associated with MRSA infection: a possible role of bacterial superantigen. Kidney Int. 1995;47(1):207–16.
Yoh K, Kobayashi M, Hirayama A, Hirayama K, Yamaguchi N, Nagase S, et al. A case of superantigen-related glomerulonephritis after methicillin-resistant Staphylococcus aureus (MRSA) infection. Clin Nephrol. 1997;48(5):311–6.
Kobayashi M, Koyama A. Methicillin-resistant Staphylococcus aureus (MRSA) infection in glomerulonephritis—a novel hazard emerging on the horizon. Nephrol Dial Transplant. 1998;13(12):2999–3001.
Hirayama K, Kobayashi M, Kondoh M, Muro K, Iwabuchi S, Yoh K, et al. Henoch-Schonlein purpura nephritis associated with methicillin-resistant Staphylococcus aureus infection. Nephrol Dial Transplant. 1998;13(10):2703–4.
Yoh K, Kobayashi M, Yamaguchi N, Hirayama K, Ishizu T, Kikuchi S, et al. Cytokines and T-cell responses in superantigen-related glomerulonephritis following methicillin-resistant Staphylococcus aureus infection. Nephrol Dial Transplant. 2000;15(8):1170–4.
Yamashita Y, Tanase T, Terada Y, Tamura H, Akiba T, Inoue H, et al. Glomerulonephritis after methicillin-resistant Staphylococcus aureus infection resulting in end-stage renal failure. Int Med. 2001;40(5):424–7.
Nagaba Y, Hiki Y, Aoyama T, Sano T, Matsuo T, Shimizu T, et al. Effective antibiotic treatment of methicillin-resistant Staphylococcus aureus-associated glomerulonephritis. Nephron. 2002;92(2):297–303. doi:63309.
Koyama A, Sharmin S, Sakurai H, Shimizu Y, Hirayama K, Usui J, et al. Staphylococcus aureus cell envelope antigen is a new candidate for the induction of IgA nephropathy. Kidney Int. 2004;66(1):121–32. doi:10.1111/j.1523-1755.2004.00714.x.
Griffin MD, Bjornsson J, Erickson SB. Diffuse proliferative glomerulonephritis and acute renal failure associated with acute staphylococcal osteomyelitis. J Am Soc Nephrol. 1997;8(10):1633–9.
Popa ER, Stegeman CA, Kallenberg CG, Tervaert JW. Staphylococcus aureus and Wegener’s granulomatosis. Arthritis Res. 2002;4(2):77–9.
Peel R, Sellars L, Long ED, Bhandari S. A man with backache and renal failure. Am J Kidney Dis. 2003;41(1):E1. doi:10.1053/ajkd.2003.50019.
Handa T, Ono T, Watanabe H, Takeda T, Muso E, Kita T. Glomerulonephritis induced by methicillin-sensitive Staphylococcus aureus infection. Clin Exp Nephrol. 2003;7(3):247–9. doi:10.1007/s10157-003-0240-4.
Nasr SH, Markowitz GS, Whelan JD, Albanese JJ, Rosen RM, Fein DA, et al. IgA-dominant acute poststaphylococcal glomerulonephritis complicating diabetic nephropathy. Hum Pathol. 2003;34(12):1235–41.
Satoskar AA, Nadasdy G, Plaza JA, Sedmak D, Shidham G, Hebert L, et al. Staphylococcus infection-associated glomerulonephritis mimicking IgA nephropathy. Clin J Am Soc Nephrol. 2006;1(6):1179–86. doi:10.2215/CJN.01030306.
Haas M, Racusen LC, Bagnasco SM. IgA-dominant postinfectious glomerulonephritis: a report of 13 cases with common ultrastructural features. Hum Pathol. 2008;39(9):1309–16. doi:10.1016/j.humpath.2008.02.015.
Worawichawong S, Girard L, Trpkov K, Gough JC, Gregson DB, Benediktsson H. Immunoglobulin A-dominant postinfectious glomerulonephritis: frequent occurrence in nondiabetic patients with Staphylococcus aureus infection. Hum Pathol. 2011;42(2):279–84. doi:10.1016/j.humpath.2010.07.009.
Nasr SH, D’Agati VD. IgA-dominant postinfectious glomerulonephritis: a new twist on an old disease. Nephron Clin Pract. 2011;119(1):c18–25; discussion c6. doi:10.1159/000324180.
Ellis A. Natural history of Bright’s disease: clinical, histological and experimental observations. Lancet. 1942;1(1).
Nasr SH, Fidler ME, Valeri AM, Cornell LD, Sethi S, Zoller A, et al. Postinfectious glomerulonephritis in the elderly. J Am Soc Nephrol. 2011;22(1):187–95. doi:10.1681/ASN.2010060611.
Lowy FD. Staphylococcus aureus infections. N Engl J Med. 1998;339(8):520–32. doi:10.1056/NEJM199808203390806.
Chatterjee SS, Otto M. Improved understanding of factors driving methicillin-resistant Staphylococcus aureus epidemic waves. Clin Epidemiol. 2013;5:205–17. doi:10.2147/CLEP.S37071.
Nasr SH, Radhakrishnan J, D’Agati VD. Bacterial infection-related glomerulonephritis in adults. Kidney Int. 2013;83(5):792–803. doi:10.1038/ki.2012.407.
Nasr SH, Markowitz GS, Stokes MB, Said SM, Valeri AM, D’Agati VD. Acute postinfectious glomerulonephritis in the modern era: experience with 86 adults and review of the literature. Medicine. 2008;87(1):21–32. doi:10.1097/md.0b013e318161b0fc.
Kanjanabuch T, Kittikowit W, Eiam-Ong S. An update on acute postinfectious glomerulonephritis worldwide. Nat Rev Nephrol. 2009;5(5):259–69. doi:10.1038/nrneph.2009.44.
Nadasdy T, Hebert LA. Infection-related glomerulonephritis: understanding mechanisms. Semin Nephrol. 2011;31(4):369–75. doi:10.1016/j.semnephrol.2011.06.008.
Glassock RJ, Alvarado A, Prosek J, Hebert C, Parikh S, Satoskar A, et al. Staphylococcus-related glomerulonephritis and poststreptococcal glomerulonephritis: why defining “post” is important in understanding and treating infection-related glomerulonephritis. Am J Kidney Dis. 2015;65(6):826–32. doi:10.1053/j.ajkd.2015.01.023.
Satoskar AA, Molenda M, Scipio P, Shim R, Zirwas M, Variath RS, et al. Henoch-Schonlein purpura-like presentation in IgA-dominant Staphylococcus infection—associated glomerulonephritis—a diagnostic pitfall. Clin Nephrol. 2013;79(4):302–12. doi:10.5414/CN107756.
Montoliu J, Miro JM, Campistol JM, Trilla A, Mensa J, Torras A, et al. Henoch-Schonlein purpura complicating staphylococcal endocarditis in a heroin addict. Am J Nephrol. 1987;7(2):137–9.
Hirayama K, Kobayashi M, Muro K, Yoh K, Yamagata K, Koyama A. Specific T-cell receptor usage with cytokinemia in Henoch-Schonlein purpura nephritis associated with Staphylococcus aureus infection. J Intern Med. 2001;249(4):289–95.
Eftychiou C, Samarkos M, Golfinopoulou S, Skoutelis A, Psarra A. Henoch-Schonlein purpura associated with methicillin-resistant Staphylococcus aureus infection. Am J Med. 2006;119(1):85–6. doi:10.1016/j.amjmed.2005.07.041.
Kitamura T, Nakase H, Iizuka H. Henoch-Schonlein purpura after postoperative Staphylococcus aureus infection with hepatic IgA nephropathy. J Nephrol. 2006;19(5):687–90.
Satoskar AA, Suleiman S, Ayoub I, Hemminger J, Parikh S, Brodsky S, Bott C, Calomeni E, Nadasdy GM, Rovin B, Lee H, Nadasdy T. Staphylococcus infection-associated glomerulonephritis—spectrum of IgA staining and prevalence of ANCA in a single-center. Clin J Am Soc Nephrol. 2017 Jan 6;12(1):39–49. doi:10.2215/CJN.05070516.
Okada M, Sato M, Ogura M, Kamei K, Matsuoka K, Ito S. Central venous catheter infection-related glomerulonephritis under long-term parenteral nutrition: a report of two cases. BMC Res Notes. 2016;9(1):196. doi:10.1186/s13104-016-1997-3.
Kimata T, Tsuji S, Yoshimura K, Tsukaguchi H, Kaneko K. Methicillin-resistant Staphylococcus aureus-related glomerulonephritis in a child. Pediatr Nephrol. 2012;27(11):2149–52. doi:10.1007/s00467-012-2229-2.
Boils CL, Nasr SH, Walker PD, Couser WG, Larsen CP. Update on endocarditis-associated glomerulonephritis. Kidney Int. 2015;87(6):1241–9. doi:10.1038/ki.2014.424.
Chirinos JA, Corrales-Medina VF, Garcia S, Lichtstein DM, Bisno AL, Chakko S. Endocarditis associated with antineutrophil cytoplasmic antibodies: a case report and review of the literature. Clin Rheumatol. 2007;26(4):590–5. doi:10.1007/s10067-005-0176-z.
Tiliakos AM, Tiliakos NA. Dual ANCA positivity in subacute bacterial endocarditis. J Clin Rheumatol. 2008;14(1):38–40. doi:10.1097/RHU.0b013e318164187a.
Hanf W, Serre JE, Salmon JH, Fabien N, Ginon I, Dijoud F, et al. Rapidly progressive ANCA positive glomerulonephritis as the presenting feature of infectious endocarditis. Rev Med Int. 2011;32(12):e116–8. doi:10.1016/j.revmed.2010.12.017 (French).
Uh M, McCormick IA, Kelsall JT. Positive cytoplasmic antineutrophil cytoplasmic antigen with PR3 specificity glomerulonephritis in a patient with subacute bacterial endocarditis. J Rheumatol. 2011;38(7):1527–8. doi:10.3899/jrheum.101322.
Mahr A, Batteux F, Tubiana S, Goulvestre C, Wolff M, Papo T, et al. Brief report: prevalence of antineutrophil cytoplasmic antibodies in infective endocarditis. Arthritis Rheumatol. 2014;66(6):1672–7. doi:10.1002/art.38389.
Ying CM, Yao DT, Ding HH, Yang CD. Infective endocarditis with antineutrophil cytoplasmic antibody: report of 13 cases and literature review. PLoS ONE. 2014;9(2):e89777. doi:10.1371/journal.pone.0089777.
Langlois V, Lesourd A, Girszyn N, Menard JF, Levesque H, Caron F, et al. Antineutrophil cytoplasmic antibodies associated with infective endocarditis. Medicine. 2016;95(3):e2564. doi:10.1097/MD.0000000000002564.
Mourad W, Mehindate K, Schall TJ, McColl SR. Engagement of major histocompatibility complex class II molecules by superantigen induces inflammatory cytokine gene expression in human rheumatoid fibroblast-like synoviocytes. J Exp Med. 1992;175(2):613–6.
Sharmin S, Shimizu Y, Hagiwara M, Hirayama K, Koyama A. Staphylococcus aureus antigens induce IgA-type glomerulonephritis in Balb/c mice. J Nephrol. 2004;17(4):504–11.
Boils CL, Nasr SH, Walker PD, et al. Infective endocarditis-associated glomerulonephritis: a report of 37 cases. Mod Pathol. 2012;Abstract 1657.
Kapadia AS, Panda M, Fogo AB. Postinfectious glomerulonephritis: Is there a role for steroids? Indian J Nephrol. 2011;21(2):116–9. doi:10.4103/0971-4065.82141.
Zeledon JI, McKelvey RL, Servilla KS, Hofinger D, Konstantinov KN, Kellie S, et al. Glomerulonephritis causing acute renal failure during the course of bacterial infections. Histological varieties, potential pathogenetic pathways and treatment. Int Urol Nephrol. 2008;40(2):461–70. doi:10.1007/s11255-007-9323-6.
Moroni G, Pozzi C, Quaglini S, Segagni S, Banfi G, Baroli A, et al. Long-term prognosis of diffuse proliferative glomerulonephritis associated with infection in adults. Nephrol Dial Transplant. 2002;17(7):1204–11.
Montseny JJ, Meyrier A, Kleinknecht D, Callard P. The current spectrum of infectious glomerulonephritis. Experience with 76 patients and review of the literature. Medicine. 1995;74(2):63–73.
Raff A, Hebert T, Pullman J, Coco M. Crescentic post-streptococcal glomerulonephritis with nephrotic syndrome in the adult: Is aggressive therapy warranted? Clin Nephrol. 2005;63(5):375–80.
Riley AM, Wall BM, Cooke CR. Favorable outcome after aggressive treatment of infection in a diabetic patient with MRSA-related IgA nephropathy. Am J Med Sci. 2009;337(3):221–3. doi:10.1097/MAJ.0b013e318184a4a1.
Foster TJ. Colonization and infection of the human host by staphylococci: adhesion, survival and immune evasion. Vet Dermatol. 2009;20(5–6):456–70. doi:10.1111/j.1365-3164.2009.00825.x.
Peacock SJ, de Silva I, Lowy FD. What determines nasal carriage of Staphylococcus aureus? Trends Microbiol. 2001;9(12):605–10.
Schechter-Perkins EM, Mitchell PM, Murray KA, Rubin-Smith JE, Weir S, Gupta K. Prevalence and predictors of nasal and extranasal staphylococcal colonization in patients presenting to the emergency department. Ann Emerg Med. 2011;57(5):492–9. doi:10.1016/j.annemergmed.2010.11.024.
von Eiff C, Becker K, Machka K, Stammer H, Peters G. Nasal carriage as a source of Staphylococcus aureus bacteremia. Study Group. N Engl J Med. 2001;344(1):11–6. doi:10.1056/NEJM200101043440102.
Wertheim HF, Vos MC, Ott A, van Belkum A, Voss A, Kluytmans JA, et al. Risk and outcome of nosocomial Staphylococcus aureus bacteraemia in nasal carriers versus non-carriers. Lancet. 2004;364(9435):703–5. doi:10.1016/S0140-6736(04)16897-9.
Wenzel RP, Perl TM. The significance of nasal carriage of Staphylococcus aureus and the incidence of postoperative wound infection. J Hosp Infect. 1995;31(1):13–24.
Foster TJ. Immune evasion by staphylococci. Nat Rev Microbiol. 2005;3(12):948–58. doi:10.1038/nrmicro1289.
Miller LG, Diep BA. Clinical practice: colonization, fomites, and virulence: rethinking the pathogenesis of community-associated methicillin-resistant Staphylococcus aureus infection. Clin Infect Dis. 2008;46(5):752–60. doi:10.1086/526773.
Moellering RC Jr. Past, present, and future of antimicrobial agents. Am J Med. 1995;99(6A):11S–8S.
Kirby H. Une Faute De Transcription, D’orthographe, Ou D’impression. Science. 1944;100(2602):425–7. doi:10.1126/science.100.2602.425.
Demerec M. Production of Staphylococcus strains resistant to various concentrations of penicillin. Proc Natl Acad Sci USA. 1945;31(1):16–24.
Murray BE, Moellering RC Jr. Patterns and mechanisms of antibiotic resistance. Med Clin North Am. 1978;62(5):899–923.
Abraham EP, Chain E. An enzyme from bacteria able to destroy penicillin. 1940. Rev Infect Dis. 1988;10(4):677–8.
Matsuhashi M, Song MD, Ishino F, Wachi M, Doi M, Inoue M, et al. Molecular cloning of the gene of a penicillin-binding protein supposed to cause high resistance to beta-lactam antibiotics in Staphylococcus aureus. J Bacteriol. 1986;167(3):975–80.
Murakami K, Tomasz A. Involvement of multiple genetic determinants in high-level methicillin resistance in Staphylococcus aureus. J Bacteriol. 1989;171(2):874–9.
Ito T, Katayama Y, Hiramatsu K. Cloning and nucleotide sequence determination of the entire mec DNA of pre-methicillin-resistant Staphylococcus aureus N315. Antimicrob Agents Chemother. 1999;43(6):1449–58.
Hersh AL, Chambers HF, Maselli JH, Gonzales R. National trends in ambulatory visits and antibiotic prescribing for skin and soft-tissue infections. Arch Int Med. 2008;168(14):1585–91. doi:10.1001/archinte.168.14.1585.
Thwaites GE, Edgeworth JD, Gkrania-Klotsas E, Kirby A, Tilley R, Torok ME, et al. Clinical management of Staphylococcus aureus bacteraemia. Lancet Infect Dis. 2011;11(3):208–22. doi:10.1016/S1473-3099(10)70285-1.
Gould IM. Clinical activity of anti-Gram-positive agents against methicillin-resistant Staphylococcus aureus. J Antimicrob Chemother. 2011;66 Suppl 4:iv17–21. doi:10.1093/jac/dkr073.
Weigel LM, Clewell DB, Gill SR, Clark NC, McDougal LK, Flannagan SE, et al. Genetic analysis of a high-level vancomycin-resistant isolate of Staphylococcus aureus. Science. 2003;302(5650):1569–71. doi:10.1126/science.1090956.
Hiramatsu K, Aritaka N, Hanaki H, Kawasaki S, Hosoda Y, Hori S, et al. Dissemination in Japanese hospitals of strains of Staphylococcus aureus heterogeneously resistant to vancomycin. Lancet. 1997;350(9092):1670–3. doi:10.1016/S0140-6736(97)07324-8.
Cui L, Isii T, Fukuda M, Ochiai T, Neoh HM, Camargo IL, et al. An RpoB mutation confers dual heteroresistance to daptomycin and vancomycin in Staphylococcus aureus. Antimicrob Agents Chemother. 2010;54(12):5222–33. doi:10.1128/AAC.00437-10.
Morales G, Picazo JJ, Baos E, Candel FJ, Arribi A, Pelaez B, et al. Resistance to linezolid is mediated by the cfr gene in the first report of an outbreak of linezolid-resistant Staphylococcus aureus. Clin Infect Dis. 2010;50(6):821–5. doi:10.1086/650574.
Gould IM, Reilly J, Bunyan D, Walker A. Costs of healthcare-associated methicillin-resistant Staphylococcus aureus and its control. Clin Microbiol Infect. 2010;16(12):1721–8. doi:10.1111/j.1469-0691.2010.03365.x.
DeLeo FR, Otto M, Kreiswirth BN, Chambers HF. Community-associated meticillin-resistant Staphylococcus aureus. Lancet. 2010;375(9725):1557–68. doi:10.1016/S0140-6736(09)61999-1.
Skov R, Christiansen K, Dancer SJ, Daum RS, Dryden M, Huang YC, et al. Update on the prevention and control of community-acquired meticillin-resistant Staphylococcus aureus (CA-MRSA). Int J Antimicrob Agents. 2012;39(3):193–200. doi:10.1016/j.ijantimicag.2011.09.029.
Tattevin P, Diep BA, Jula M, Perdreau-Remington F. Long-term follow-up of methicillin-resistant Staphylococcus aureus molecular epidemiology after emergence of clone USA300 in San Francisco jail populations. J Clin Microbiol. 2008;46(12):4056–7. doi:10.1128/JCM.01372-08.
Tattevin P, Diep BA, Jula M, Perdreau-Remington F. Methicillin-resistant Staphylococcus aureus USA300 clone in long-term care facility. Emerg Infect Dis. 2009;15(6):953–5. doi:10.3201/eid1506.080195.
Nimmo GR. USA300 abroad: global spread of a virulent strain of community-associated methicillin-resistant Staphylococcus aureus. Clin Microbiol Infect. 2012;18(8):725–34. doi:10.1111/j.1469-0691.2012.03822.x.
Pan ES, Diep BA, Carleton HA, Charlebois ED, Sensabaugh GF, Haller BL, et al. Increasing prevalence of methicillin-resistant Staphylococcus aureus infection in California jails. Clin Infect Dis. 2003;37(10):1384–8. doi:10.1086/379019.
King MD, Humphrey BJ, Wang YF, Kourbatova EV, Ray SM, Blumberg HM. Emergence of community-acquired methicillin-resistant Staphylococcus aureus USA 300 clone as the predominant cause of skin and soft-tissue infections. Ann Int Med. 2006;144(5):309–17.
Otto M. Basis of virulence in community-associated methicillin-resistant Staphylococcus aureus. Annu Rev Microbiol. 2010;64:143–62. doi:10.1146/annurev.micro.112408.134309.
Foster TJ, Hook M. Surface protein adhesins of Staphylococcus aureus. Trends Microbiol. 1998;6(12):484–8.
O’Brien LM, Walsh EJ, Massey RC, Peacock SJ, Foster TJ. Staphylococcus aureus clumping factor B (ClfB) promotes adherence to human type I cytokeratin 10: implications for nasal colonization. Cell Microbiol. 2002;4(11):759–70.
Clarke SR, Brummell KJ, Horsburgh MJ, McDowell PW, Mohamad SA, Stapleton MR, et al. Identification of in vivo-expressed antigens of Staphylococcus aureus and their use in vaccinations for protection against nasal carriage. J Infect Dis. 2006;193(8):1098–108. doi:10.1086/501471.
Diep BA, Stone GG, Basuino L, Graber CJ, Miller A, des Etages SA, et al. The arginine catabolic mobile element and staphylococcal chromosomal cassette mec linkage: convergence of virulence and resistance in the USA300 clone of methicillin-resistant Staphylococcus aureus. J Infect Dis. 2008;197(11):1523–30. doi:10.1086/587907.
Clarke SR, Mohamed R, Bian L, Routh AF, Kokai-Kun JF, Mond JJ, et al. The Staphylococcus aureus surface protein IsdA mediates resistance to innate defenses of human skin. Cell Host Microbe. 2007;1(3):199–212. doi:10.1016/j.chom.2007.04.005.
Mack D, Fischer W, Krokotsch A, Leopold K, Hartmann R, Egge H, et al. The intercellular adhesin involved in biofilm accumulation of Staphylococcus epidermidis is a linear beta-1,6-linked glucosaminoglycan: purification and structural analysis. J Bacteriol. 1996;178(1):175–83.
Moreillon P, Que YA. Infective endocarditis. Lancet. 2004;363(9403):139–49. doi:10.1016/S0140-6736(03)15266-X.
Rooijakkers SH, Ruyken M, Roos A, Daha MR, Presanis JS, Sim RB, et al. Immune evasion by a staphylococcal complement inhibitor that acts on C3 convertases. Nat Immunol. 2005;6(9):920–7. doi:10.1038/ni1235.
Bokarewa MI, Jin T, Tarkowski A. Staphylococcus aureus: Staphylokinase. Int J Biochem Cell Biol. 2006;38(4):504–9. doi:10.1016/j.biocel.2005.07.005.
Hair PS, Ward MD, Semmes OJ, Foster TJ, Cunnion KM. Staphylococcus aureus clumping factor A binds to complement regulator factor I and increases factor I cleavage of C3b. J Infect Dis. 2008;198(1):125–33. doi:10.1086/588825.
Lee LY, Liang X, Hook M, Brown EL. Identification and characterization of the C3 binding domain of the Staphylococcus aureus extracellular fibrinogen-binding protein (Efb). J Biol Chem. 2004;279(49):50710–6. doi:10.1074/jbc.M408570200.
Jin T, Bokarewa M, Foster T, Mitchell J, Higgins J, Tarkowski A. Staphylococcus aureus resists human defensins by production of staphylokinase, a novel bacterial evasion mechanism. J Immunol. 2004;172(2):1169–76.
Sieprawska-Lupa M, Mydel P, Krawczyk K, Wojcik K, Puklo M, Lupa B, et al. Degradation of human antimicrobial peptide LL-37 by Staphylococcus aureus-derived proteinases. Antimicrob Agents Chemother. 2004;48(12):4673–9. doi:10.1128/AAC.48.12.4673-4679.2004.
Vuong C, Voyich JM, Fischer ER, Braughton KR, Whitney AR, DeLeo FR, et al. Polysaccharide intercellular adhesin (PIA) protects Staphylococcus epidermidis against major components of the human innate immune system. Cell Microbiol. 2004;6(3):269–75.
Bera A, Herbert S, Jakob A, Vollmer W, Gotz F. Why are pathogenic staphylococci so lysozyme resistant? The peptidoglycan O-acetyltransferase OatA is the major determinant for lysozyme resistance of Staphylococcus aureus. Mol Microbiol. 2005;55(3):778–87. doi:10.1111/j.1365-2958.2004.04446.x.
Proft T, Fraser JD. Bacterial superantigens. Clin Exp Immunol. 2003;133(3):299–306.
Llewelyn M, Cohen J. Superantigens: microbial agents that corrupt immunity. Lancet Infect Dis. 2002;2(3):156–62.
Lussow AR, MacDonald HR. Differential effects of superantigen-induced “anergy” on priming and effector stages of a T cell-dependent antibody response. Eur J Immunol. 1994;24(2):445–9. doi:10.1002/eji.1830240227.
Goodyear CS, Silverman GJ. Staphylococcal toxin induced preferential and prolonged in vivo deletion of innate-like B lymphocytes. Proc Natl Acad Sci USA. 2004;101(31):11392–7. doi:10.1073/pnas.0404382101.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this chapter
Cite this chapter
Hemminger, J.A., Satoskar, A.A. (2017). Staphylococcus Infection-Associated Glomerulonephritis. In: Satoskar, A., Nadasdy, T. (eds) Bacterial Infections and the Kidney. Springer, Cham. https://doi.org/10.1007/978-3-319-52792-5_2
Download citation
DOI: https://doi.org/10.1007/978-3-319-52792-5_2
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-52790-1
Online ISBN: 978-3-319-52792-5
eBook Packages: MedicineMedicine (R0)