Abstract
Thorough evaluation of pediatric wrist and scaphoid fractures includes open versus closed status, neurovascular status, associated injuries, displacement, and physeal involvement.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
Overview
Thorough evaluation of pediatric wrist and scaphoid fractures includes open versus closed status, neurovascular status, associated injuries, displacement, and physeal involvement.
What to Ask
-
1.
Are there any open wounds (possible open fracture, often from ulnar styloid)?
-
2.
Are there any associated injuries? Fractures and dislocations about the ipsilateral elbow are common, and make reduction and immobilization more challenging.
-
3.
What is the patient’s neurovascular status?
-
4.
Can the patient’s jewelry be removed, and is their IV access on contralateral arm?
What to Request
-
1.
Ensure arm is stabilized, elevated, and iced immediately.
-
2.
X-rays of the wrist, forearm, and elbow. Scaphoid views are appropriate if suspicious for injury.
-
3.
If the fracture is displaced and requires reduction, ask for conscious sedation.
When to Escalate
-
1.
Open fractures should be irrigated in ED and receive antibiotics (will require formal irrigation and debridement in OR).
-
2.
Paresthesia: Acute CTS may require emergent fixation and release if it persists after reduction.
Imaging
-
1.
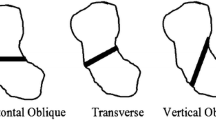
AP, oblique, and lateral views of the wrist are necessary for evaluation.
-
2.
Radiographs of the contralateral wrist may be helpful.
-
3.
Postreduction X-rays of the wrist (AP and lateral).
Effective Communication
-
1.
Open versus closed
-
2.
Neurovascular compromise
-
3.
Associated injuries
-
4.
Displaced/non-displaced
-
5.
Physeal involvement
Key Exam Pearls
-
1.
Sensation of hand (median/radial/ulnar nerves).
-
2.
Motor (EPL/FPL/EDC/FDS/FDP/IO).
-
3.
Evaluate all wounds: Dermal violation raises suspicion for open fracture.
-
4.
Snuffbox tenderness should be treated as an occult scaphoid fracture. See thumb spica splint, Chapter 6.
Reduction [1]
Minimally displaced “buckle” or “torus” fractures (see Fig. 16.1) often are within acceptable limits to leave unreduced and only require casting to help protect the healing bone. For reduction of distal radius physeal fractures (see Fig. 16.2), apply constant gentle longitudinal traction to the forearm with the aid of an assistant or finger traction. This often leads to spontaneous reduction of the fracture. If the fracture does not reduce, apply gentle force over the fracture site while maintaining traction. Once reduced, a long-arm cast with a three-point mold is applied. The distal point should be broad and smooth over the distal fracture fragment. The MCP joints must be left free. Aggressive flexion of the hand and wrist should be avoided.
Adequate Reduction Parameters [1]
-
1.
In children less than 10 years old, less than 15o of angulation in the sagittal plane is acceptable; if the child is older than 10, less than 10° is acceptable if the physes of the radius are still open.
Follow-Up
-
1.
Remain non-weight bearing and continue to ice and elevate.
-
2.
See an orthopedic surgeon within 1 week.
Reference
Egol KA, Joval KJ, Zuckerman JD. Handbook of fractures. 4th ed. Philadelphia: Lippincott Williams & Wilkins; 2010.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this chapter
Cite this chapter
Gil, J.A. (2017). Pediatric Wrist and Scaphoid Fractures. In: Hodax, J., Eltorai, A., Daniels, A. (eds) The Orthopedic Consult Survival Guide. Springer, Cham. https://doi.org/10.1007/978-3-319-52347-7_16
Download citation
DOI: https://doi.org/10.1007/978-3-319-52347-7_16
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-52346-0
Online ISBN: 978-3-319-52347-7
eBook Packages: MedicineMedicine (R0)