Abstract
Prevention of behavioral health problems is integral to promoting worldwide health. Alarmingly, many behavioral health problems occur early in life, significantly disrupting normal developmental processes. Most people that require intervention never engage in care and symptoms worsen over time. This chapter articulates a viable solution—integration of behavioral health prevention and treatment into primary care well-child health maintenance visits. Readers are provided with an empirically based argument for this novel practice as well as a formulation of how this approach may improve lifetime treatment engagement.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Well-child care
- Pediatric health maintenance
- Treatment engagement
- Treatment adherence priimary prevention
- Secondary prevention
- Pediatric integrated care
Behavioral health problems occur at a significant rate and have large impact across all age groups (SAMHSA-HRSA Center for Integrated Health Solutions , 2013). The Substance Abuse and Mental Health Services Administration reported (2013) that approximately one in four adults suffer from a diagnosable behavioral health problem in a given year (e.g., depression, panic disorder). Furthermore, those with a behavioral health problem, that receive treatment in the public mental health system, have a shortened life expectancy of 11–15 years on average when compared to the general population (SAMHSA-HRSA Center for Integrated Health Solutions, 2013). The burden of behavioral health problems is considerable and oftentimes this burden begins at a young age.
Kessler and colleagues found that behavioral health problems begin very early in life (Kessler et al., 2005). Half of all lifetime cases begin by age 14, and three-quarters have begun by age 24 (Collins, Hewson, Munger, & Wade, 2010; Kessler et al., 2005). In fact, one in five children have at least one behavioral health problem that interferes with daily functioning (Barnett, Griffin, Muse, Moreland, & Mian, 2008). For example, anxiety disorders often begin in late childhood and mood disorders in late adolescence (Substance Abuse and Mental Health Services Administration , 2013). Unlike chronic disease such as heart disease or most cancers, young people with behavioral health problems suffer disability when they are in the prime of life; which also serves as a platform for critical future development. Behavioral health problems such as treatment nonadherence, lack of proper diet and exercise, anxiety, depression, engaging in risk behavior, and bipolar disorder truly are the chronic diseases of early life (Centers for Disease Control and Prevention, 2012).
Treatment Access and Engagement
Germane to the early onset of most behavioral health problems is the fact that there are very long delays (sometimes decades) between first onset of symptoms and when people seek treatment or receive treatment (Substance Abuse and Mental Health Services Administration , 2013; World Health Organization, 2008). The National Comorbidity Survey (NCS) , for example, estimated that approximately 80 % of all people in the United States with a mental disorder eventually seek treatment, but that the median delay between first onset of the disorder and first treatment contact is nearly a decade (Wang, Berglund, et al., 2005; Wang, Lane, et al., 2005). Evidence shows that the current behavioral health system fails to engage a significant number of people with behavioral health problems for a myriad of reasons such as limited access to quality care, stigma, and geographical and financial constraints (Kazdin & Blase, 2011; McGuire & Miranda, 2008; World Health Organization, 2008). Furthermore, those it does reach often drop out or get insufficient, uncoordinated care (World Health Organization, 2008), and sometimes even unsafe care (Lilienfeld, 2007).
Alarmingly, when individuals do seek care they are often not treated with evidence-based assessment or treatment (Institute of Medicine, 2006). Instead psychometrically problematic assessment instruments are used and providers deliver lengthy, less than effective care (Wang, Bergland, & Kessler, 2000). Implementing less-effective therapies can create problems that require further expensive treatment, which results in unnecessary suffering (Institute of Medicine, 2006; Lilienfeld, 2007). An additional complicating factor is the considerable reliance on psychotropic medications , yet significant concerns with safety and efficacy persist (Brown et al., 2006). Despite the fact that there are very effective behavioral health interventions, those with behavioral health problems are still severely disadvantaged and unnecessarily suffer due to inadequate care (Collins et al., 2010).
This limited engagement in quality, coordinated care leads to more difficult-to-treat behavioral health problems and can contribute to the development of comorbid problems. Early-onset behavioral health problems that are left untreated are associated with a host of adverse events including school failure, teenage pregnancy, chronic medical problems, unstable employment, early marriage, and marital instability and violence (Substance Abuse and Mental Health Services Administration , 2013). Detecting and treating cases early could prevent enormous disability, before the illness becomes more severe. Early detection and treatment engagement could also intervene before co-occurring behavioral health problems develop, which only become more difficult to treat as they accumulate (Substance Abuse and Mental Health Services Administration, 2013). These concerns highlight the importance of prevention and early detection of behavioral health problems.
Disparities in Access to Care
Traditionally underserved groups, such as the young, the elderly, racial/ethnic minorities, and those with low income or without insurance, have the greatest unmet need for treatment (World Health Organization, 2008). Inverse relationships between socioeconomic status and health risk behaviors such as tobacco smoking, physical inactivity, and poor nutrition have been demonstrated (Pampel, Krueger, & Denney, 2010). Unfortunately, low socioeconomic status is also associated with significantly less anticipatory guidance provided in primary care (Irwin, Adams, Park, & Newacheck, 2009). Therefore, it can be argued that underprivileged populations, including underprivileged pediatric populations, not only have restricted access to care but also are in greater need of prevention and intervention. Additional barriers to access to care include financial constraints and a lack of ethnic diversity amongst providers (Cabassa, Zayas, & Hansen, 2006; McGuire & Miranda, 2008; Wang, Berglund, et al., 2005; Wang, Lane, et al., 2005). These disparities in access to care must be resolved in order to systematically address national unmet behavioral health need .
The Problem of Prevention
In addition to the significant barriers in access to quality care, behavioral health prevention efforts have been largely ineffective. Attempts at prevention have primarily been large-scale nomothetic public health interventions such as Project D.A.R.E. and anti-smoking campaigns (Ridenour, Pineo, Molina, & Lich, 2013). Some of these preventative efforts have been iatrogenic and most have modest efficacy, if any at all (Werch & Owen, 2002). We are currently unable to prevent behavioral health problems before they manifest, and this severely undermines our ability to lessen the overall burden of behavioral health problems. The fact that behavioral health prevention has been unsuccessful is an indication that a novel approach is warranted.
The Need for Integrated Care
Integrating behavioral health services into a primary care setting is the most viable and efficient way of delivering prevention and ensuring that people have access to needed behavioral health services (SAMHSA-HRSA Center for Integrated Health Solutions , 2013; World Health Organization, 2008). Most people first bring their behavioral health concerns to their regular doctor (Nielsen, 2013) and while patients typically present with a physical health complaint, data suggest that underlying behavioral health or substance abuse issues are often triggering these visits. In fact, as many as 70 % of primary care visits stem from psychosocial issues (O’Donohue & Cucciare, 2005; Robinson & Reiter, 2007). Unfortunately, most primary care doctors are ill equipped or lack the time to fully address the wide range of psychosocial issues that they encounter in practice (Collins, Hewson, Munger, & Wade, 2010). Most receive little training, are less interested in treating these problems, and have little time in a short medical appointment (15 min) to cover these potential problems.
Integrated care refers to a service delivery system that is coordinated so that both physical health and behavioral health problems can be addressed in one setting (O'Donohue, Cummings, Cucciare, Runyan, & Cummings 2006). Therefore, complex relationships between physical and behavioral health can be more effectively recognized and treated (Zeiss & Karlin, 2008). Patients receive one treatment plan with both physical health and behavioral health elements (Collins, Hewson, Munger, & Wade, 2010). Integrated care does not diminish the role of behavioral health providers in the community, as more chronic cases are referred to these providers, but assimilates important behavioral health resources into primary care. Behavioral health care delivered in an integrated setting can help to minimize stigma and discrimination, while increasing opportunities to improve overall health outcomes (Collins, Hewson, Munger, & Wade, 2010; Zeiss & Karlin, 2008).
Furthermore, evidence shows that quality of behavioral health care is superior when delivered by a collocated behavioral health practitioner, relative to other types of primary care providers. Patients with behavioral health problems or substance abuse disorders were more likely to get treatment from a primary care physician/nurse or other general medical doctor (22.8 %), or from a nonpsychiatrist behavioral health specialist (16 %), such as a psychologist, social worker, or counselor, than from a psychiatrist (12 %), though adequacy of treatment is best when provided by behavioral health practitioners in a primary care setting (Layard, 2006; Substance Abuse and Mental Health Services Administration , 2013). Patients also prefer treatment by a behavioral health professional and go more often, relative to behavioral health care delivered by primary care providers (PCPs; Seligman, 1995). The superior provision of care and patient preference for behavioral health providers strengthens the argument for behavioral health integration in primary care.
Most importantly, integrated care has been shown to enhance overall health outcomes (World Health Organization, 2008; Zeiss & Karlin, 2008). Specifically, brief targeted behavioral interventions have been shown to reduce medical and surgical costs far beyond the cost of providing the behavioral interventions (Cummings, O’Donohue, & Cummings, 2009). Patients receiving care in an integrated system have also been shown to linearly improve across behavioral treatment sessions, with patterns that mirror the early stages of traditional outpatient psychotherapy. These patients also have been shown to maintain improvements in global mental health functioning at 2-year follow-up, regardless of additional behavioral health treatment (Ray-Sannerud et al., 2012). Moreover, patients prefer to receive behavioral health treatment in a primacy care setting (Zeiss & Karlin, 2008). Integrated care improves physical health and behavioral health outcomes, increases access to care, and provides a forum for prevention efforts.
The Importance of Stepped Care
In order for integrated care to be most effective and efficient, care should be organized in a stepped fashion (Von Korff, Glasgow, & Sharpe, 2002). Specifically, more complex and expensive interventions should only be used when simpler interventions have been demonstrated to be inadequate (O’Donohue & Draper, 2011; Von Korff, Glasgow, & Sharpe, 2002). Stepped care posits that providers offer care that, (1) causes the least disruption in the patient’s life, (2) is the least extensive required for positive results, (3) is the least intensive for positive results, (4) is the least expensive for positive results, and (5) is the least expensive in terms of staff training required to provide effective service (O’Donohue & Draper, 2011). Successful integrated care protocols utilize stepped care (Zeiss & Karlin, 2008), which is consistent with usual primary care practice.
An example of stepped care. Consider the case of an adolescent patient that did not display psychological impairment on screening measures but reported low mood, not accompanied by additional symptoms of clinical depression. Stepped care intervention would include: (1) increasing health literacy (educating the patient as to what symptoms are indicative of increased intervention, how low mood is maintained/alleviated, etc.), (2) idiographic prevention (i.e., support of healthy coping strategies and discouragement of use of avoidance coping), (3) referral to evidence-based bibliotherapy/eHealth options, (4) strengthening of the provider/patient relationship (specifically, informing the patient that should her symptoms worsen that the provider will be available to provide consultation and care), and (5) provision of a printed integrated care plan following the patient’s visit with the PCP. Additionally, the BCP would enter information regarding identified low mood and intervention into the patient’s EHR, in conjunction with discussing these findings with the patient’s PCP in order to achieve the goal of coordinated care.
In the event that the patient’s symptoms of low mood did not remit, a brief evidence-based cognitive behavioral intervention would be implemented in the primary care setting. If the patient’s symptomology did not remit following brief intervention, a referral to an appropriate community provider through the behavioral health provider’s (BCP’s) accountable relationships with other entities would be appropriate.
Stepped care is an effective, cost-effective treatment modality that facilitates the provision of integrated care.
Integrated Pediatric Care
It has been over a decade since the U.S. Surgeon General called for pediatric primary care practice to expand their scope of practice to include behavioral health treatment and there has been increasing recognition of the importance of integrated pediatric care (Van Cleve, Hawkins-Walsh, & Shafer, 2013). In pediatric integrated care, there is greater focus on identifying early onset of behavioral health problems in children and youth (SAMHSA-HRSA Center for Integrated Health Solutions , 2013). However, a significant portion of pediatric primary care centers do not implement integrated care and evidence shows that pediatric PCPs recognize only approximately one-third of patients with behavioral health dysfunction in their practice (Kuhlthau et al., 2011). Although the need for integrated pediatric care has been recognized, technologies to support implementation are still needed.
Is Screening Sufficient?
The argument can be made that proper screening would address the problem of at least detecting pediatric behavioral health concerns in primary care. In fact, there is evidence that behavioral screening during well-child visits results in a threefold increase in the detection of children at risk for a behavioral health condition (Kuhlthau et al., 2011). Unfortunately, even when this increase of detection was reported, results indicated that nearly half of the well-child visits still did not include behavioral screening (Kuhlthau et al., 2011). Furthermore, effective screening does not necessarily result in an appropriate level of intervention. Screening alone is simply not the answer and greater integration efforts are required to increase access to pediatric behavioral health care.
The Importance of the Well-Child Visit
The well-child visit is an important point of intervention in pediatric integrated care. Well-child visits are routine visits that should occur once per year until the patient is 21 years old (National Institutes of Health, 2015). These encounters account for more than 30 % of physician visits for those patients 15 years and younger (Moyer & Butler, 2013). Broadly, the purpose of these encounters is the maintenance of health and prevention of disease—particularly physical disease. Well-child encounters are the context in which pediatric prevention and routine assessment is conducted, and the specific functions of these visits are discussed below. The well-child visit is a preexisting pediatric primary care practice that can aid in the implementation of integrated care by providing a forum for coordinated behavioral health wellness checkups. Well-child visits have typically been delivered and conceptualized in terms of fractionated care in which physical care is emphasized. The question becomes, what would an integrated well-child visit look like in which behavioral health concerns are also emphasized—and would it have superior outcomes to the traditional well-child visit ?
Implementing a Solution
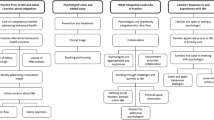
In order for integrated care to function successfully PCPs not only need education in regards to proper detection measures (i.e., behavioral health screens), but behavioral health specialists must also be available to support primary care. It is the behavioral health specialist’s role to provide effective and efficient interventions and referrals when problems are found on screening measures (World Health Organization, 2008). Although competencies for pediatric integrated care systems have been set forth (APA Task Force on Mental Health, 2010; SAMHSA-HRSA Center for Integrated Health Solutions , 2013), the most effective methods of implementing these core competencies in integrated care are still under investigation. More specifically, there is very little evidence regarding how best to achieve these competencies in the context of health maintenance well-child visits (SAMHSA-HRSA Center for Integrated Health Solutions, 2013). Creating space in these visits to deliver coordinated behavioral health wellness exams is critical to increasing preventative efforts and access to care.
An opportunity for a novel approach to prevention of behavioral health problems.
Integrated well-child visits can offer a remedy for current nomothetic behavioral health prevention efforts. We propose that an individualized approach to prevention and the use of a medical/behavioral health team has the potential to produce superior outcomes, relative to nomothetic approaches. Physical medicine began to advance such prevention in well-child visits more than a decade ago (American Pediatrics Task Force on Mental Health, 2010) and the behavioral health field can learn from this model .
An idiographic approach to prevention could provide more specific, and therefore, theoretically more effective prevention. For example, consider the case of a 13-year-old male patient that presented for a well-child visit and had recently begun to gain weight. A nomothetic approach would simply provide him with guidelines regarding a healthy diet and daily exercise. With this particular patient, idiographic assessment revealed that he had discontinued regular walks with his family because he felt that he did not get enough individual attention from his mother due to her focus on his younger sisters. An idiographic preventative intervention included eliciting a commitment from both the patient and his mother that they would walk together at least once per week without the rest of the family. The patient reported that this intervention would help him increase his exercise while helping to remediate the low mood he felt due to his perceived lack of family attention. It is likely that without uncovering the specific reason for this patient’s individual weight gain that standardized prevention efforts would not have resulted in necessary behavior change.
Furthermore, this idiographic prevention has the potential to be more powerful when implemented by a medical/behavioral health team. For example, an integrated care team has the advantage of providing the patient with expert behavior modification techniques and is able to monitor progress towards treatment goals (i.e., weight, Body Mass Index). Whether an integrated care approach to idiographic prevention is more effective than standard nomothetic prevention is an open empirical question, and one that merits significant attention from the behavioral health field. An integrated well-child visit is an ideal forum in which to test the assumption that idiographic prevention is a superior approach.
Existing Clinical Guidelines
With the goal of utilizing well-child visits as a primary pediatric integrated care intervention point, existing clinical guidelines for nonintegrated well-child visits must be considered. Clinical preventive service guidelines for well-child visits have been issued by several professional medical and government organizations, including the American Academy of Pediatrics (AAP), the American Medical Association, the American Academy of Family Practitioners, and the Maternal and Child Health Bureau. In the late 1990s, the AAP consolidated these guidelines into an updated edition of Bright Futures (Irwin et al., 2009). It is now standard in the field to utilize the Bright Futures Guidelines (SAMHSA-HRSA Center for Integrated Health Solutions , 2013). These guidelines include recommended ways that PCPs should address physical health, as well as recommendations for PCP-administered behavioral health care, and are not tailored to provision of integrated care.
Bright Futures Guidelines
Bright Futures is a national health promotion and disease prevention initiative that seeks to address children's health needs in the context of family and community. These principles, guidelines, and tools are used in pediatric practice nationally (American Academy of Pediatrics 2013a, 2013b, 2013c). Bright Futures clinical guidelines are categorized by target of intervention (e.g., “Healthy Weight,” “Oral Health”) and by patient age (e.g., four stages: “Infancy,” “Early Childhood,” “Middle Childhood,” “Adolescence”) (American Academy of Pediatrics 2013a, 2013b, 2013c). These guidelines are “evidence-based,” meaning that they were developed based on existing empirical evidence and constructed by a panel of experts. However, there are little to no data regarding whether these guidelines improve health outcomes in clinical practice (Moyer & Butler, 2004).
Lack of Empirical Data
Although a panel of experts created the Bright Futures guidelines, the guidelines have not been evaluated as to whether they adequately assess health functioning or contribute to enhanced outcome in any age group (e.g., increased treatment adherence or successful treatment of disease) (Barnett, Griffin, Muse, Moreland, & Mian, 2008; Irwin et al., 2009; Solberg, Nordin, Bryant, Kristensen, & Maloney, 2009). In fact, Irwin et al. (2009) found that only 10 % of well-child visits addressed all recommended categories of behavioral and physical health anticipatory guidance. Moreover, limited direct evidence was found to support any of the recommended interventions in well-child visits according to a review done by Moyer & Butler (2004). A literature search for manuscripts that cited this important (although arguably dated) review revealed no recent evidence that well-child visit guidelines have been demonstrated to enhance clinical outcomes.
Part of the reason for such lack of empirical data may be the nature of the guidelines themselves. Several goals outlined by the aforementioned guidelines are difficult to operationalize, which inherently limits testability of outcomes. For example, Bright Futures identifies, “engages in a positive way in the life of the community” as a marker of a healthy adolescent. This outcome would be difficult to evaluate given the fact that there is no further clarification regarding what exactly an adolescent might do to meet this goal. Moreover, as Schor (2004) suggested, unrealistic expectations about the content of well-child care may also contribute to the lack of empirical support for current well-child interventions.
This is startling and problematic due to the fact that inclusion of ineffective (or even potentially iatrogenic) aspects of well-child visits limit other, potentially more effective, elements that could be addressed during these routine encounters. There is a need for evaluation of both the components and the whole of well-child care (Moyer & Butler, 2004); in addition to assessment of how best to conduct these visits in the context of integrated care.
Opportunity for Change
Recent legislation such as the Affordable Care Act (ACA) mandates quality improvement initiatives in healthcare that include, but are not limited to, free preventative care and a focus on youth health care services (U.S. Department of Health & Human Services, 2015). The ACA also mandates that behavioral health prevention efforts are included in well-child visits. These and other measures within the Act are designed to reform health care services to achieve efficiencies by increasing access, and making the services more affordable and safe. To this end, the ACA covers well-child visits and depending on particular insurance plan, these visits may be provided at no cost to the patient (U.S. Department of Health & Human Services, 2015). Due to the implementation of these new mandates, well-child visits must routinely achieve a higher standard of care and integrated care can arguably achieve that goal.
Re-envisioning Well-Child Visits in the Context of Integrated Care
Development of pediatric integrated care behavioral health wellness exam that is systematically integrated into well-child visits could increase engagement in behavioral health treatment. The promise involves the following factors:
-
1.
Yearly wellness visits allow more opportunities for case finding and thus decrease the likelihood that problems will go undetected.
-
2.
Yearly wellness visits can allow lower levels/earlier stages of problems to be detected and thus patients may be more optimistic about the likelihood of change.
-
3.
If patients do not engage in 1 year, each subsequent year is an opportunity to problem-solve their lack of engagement.
-
4.
The physician-led team will likely contribute to the credibility of recommendations to initiate and continue to engage in treatment.
-
5.
When the problem is uncovered in the context of routine care, it is reasonable to hypothesize that patients will be more likely to see that the problem is well defined and acceptable.
-
6.
The healthcare team can jointly present treatment alternatives and problem-solve any lack of patient engagement.
-
7.
The team can offer the patient a broader range of treatment options, which can increase the likelihood of patient engagement.
-
8.
Because of yearly wellness visits the team can track and respond to any relapse.
Broad implications for patients and families include increased access to routine behavioral health care, an opportunity to catch emerging behavioral health problems early before they become problematic, and access to improved behavioral health prevention efforts without the burden of pursuing a separate appointment with a specialty provider. This access to a behavioral health expert and reduction of wait time during the well-child encounter delivers increased value to the pediatric patient and their family. This shift in the delivery of well-child visits could arguably solve the lack of early behavioral health treatment engagement and subsequently promote better population health.
References
American Academy of Pediatrics. (2013a). Adolescence: 11 to 21 years. Retrieved from http://brightfutures.aap.org/pdfs/Guidelines_PDF/18-Adolescence.pdf.
American Academy of Pediatrics. (2013b). Bright futures. Retrieved from http://brightfutures.aap.org/.
American Academy of Pediatrics. (2013c). Bright futures in practice: Mental health. Retrieved from http://www.brightfutures.org/mentalhealth/pdf/01BFMHFrontMatter.pdf.
American Pediatrics Task Force on Mental Health. (2010). Enhancing pediatric mental health care: Algorithms for primary care. Pediatrics, 125, S09. doi:10.1542/peds.2010-0788F.
Barnett, S., Griffin, S., Muse, N., Moreland, S., & Mian, A. (2008). Integrating child and adolescent mental health into primary care. Austin, TX, USA: Texas Medical Association.
Brown, R., Antonuccio, D. O., DuPaul, G., Fristad, M., King, C., & Pelham, W. (2006). Psychopharmacological, psychosocial, and combined interventions for childhood disorders: Evidence base, contextual, factors, and future directions. Report of the Working Group on Psychoactive Medications for Children and Adolescents, American Psychological Association.
Cabassa, L. J., Zayas, L. H., & Hansen, M. C. (2006). Latino adults’ access to mental health care: A review of epidemiological studies. Administration and Policy in Mental Health and Mental Health Services Research, 33(3), 316–330.
Centers for Disease Control and Prevention. (2012). Youth risk behavior surveillance—United States, 2011. Surveillance summaries, MMWR 2012;61(No. SS04); 1–162.
Collins, C., Hewson, D. L., Munger, R., & Wade, T. (2010). Evolving models of behavioral health integration in primary care. Milbank Memorial Fund.
Cummings, N. A., O’Donohue, W. T., & Cummings, J. L. (2009). The financial dimension of integrated behavioral/primary care. Journal of Clinical Psychology in Medical Settings, 16(1), 31–39.
Institute of Medicine. (2006). Strengthening the evidence base and quality improvement infrastructure. In Improving the quality of health care for mental and substance-use conditions: Quality chasm series. Washington, DC: The National Academies Press.
Irwin, C. E., Adams, S. H., Park, M. J., & Newacheck, P. W. (2009). Preventive care for adolescents: Few get visits and fewer get services. Pediatrics, 123(4), 565–572.
Kazdin, A. E., & Blase, S. L. (2011). Rebooting psychotherapy research and practice to reduce the burden of mental illness. Perspectives on Psychological Science, 6(1), 21–37.
Kessler, R. C., Berglund, P., Demler, O., Jin, R., Merikangas, K. R., & Walters, E. E. (2005). Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry, 62(6), 593.
Kuhlthau, K., Jellinek, M., White, G., VanCleave, J., Simons, J., & Murphy, M. (2011). Increases in behavioral health screening in pediatric care for Massachusetts Medicaid patients. Archives Pediatric Adolescent Medicine, 165(7), 660–664. Retrieved from http://archpedi.ama-assn.org/cgi/content/abstract/165/7/660.
Layard, R. (2006). Health policy: The case for psychological treatment centres. BMJ: British Medical Journal, 332(7548), 1030.
Lilienfeld, S. O. (2007). Psychological treatments that cause harm. Perspectives on Psychological Science, 2(1), 53–70.
McGuire, T. G., & Miranda, J. (2008). New evidence regarding racial and ethnic disparities in mental health: Policy implications. Health Affairs, 27(2), 393–403.
Substance Abuse and Mental Health Services Administration, Results from the 2013 National Survey on Drug Use and Health: Mental Health Findings, NSDUH Series H-49, HHS Publication No. (SMA) 14–4887. Rockville, MD: Substance Abuse and Mental Health Services Administration, 2014.
Moyer, V. A., & Butler, M. (2004). Gaps in evidence for well-child care: A challenge to our profession. Pediatrics, 114(6), 1511–1521.
National Institutes of Health. (2015). Well-child Visits. Retrieved from https://medlineplus.gov/ency/article/001928.htm.
Nielsen, M. (2013). Mental Health and Primary Care Integration-PCPCC Letter to Senate Finance Committee. Retrieved from http://www.pcpcc.org/2013/09/30/mental-health-and-primary-care-integration-pcpcc-letter-senate-finance-committee.
O’Donohue, W., & Cucciare, M. A. (2005). The role of psychological factors in medical presentations. Journal of Clinical Psychology in Medical Settings, 12(1), 13–24.
O’Donohue, W. T., & Draper, C. (2011). The case for evidence-based stepped care as part of a reformed delivery system. In Stepped care and e-health (pp. 1–16). New York: Springer.
O'Donohue, W. T., Cummings, N. A., Cucciare, M. A., Runyan, C. N., & Cummings, J. L. (2006). Integrated behavioral health care: A guide to effective intervention. Amherst, NY: Humanity Books.
Pampel, F. C., Krueger, P. M., & Denney, J. T. (2010). Socioeconomic disparities in health behaviors. Annual Review of Sociology, 36, 349.
Ray-Sannerud, B. N., Dolan, D. C., Morrow, C. E., Corso, K. A., Kanzler, K. E., Corso, M. L., & Bryan, C. J. (2012). Longitudinal outcomes after brief behavioral health intervention in an integrated primary care clinic. Families, Systems, & Health, 30(1), 60.
Ridenour, T. A., Pineo, T. Z., Molina, M. M. M., & Lich, K. H. (2013). Toward rigorous idiographic research in prevention science: Comparison between three analytic strategies for testing preventive intervention in very small samples. Prevention Science, 14(3), 267–278.
Robinson, P., & Reiter, J. (2007). Behavioral consultation and primary care: A guide to integrating services. New York: Springer.
Schor, E. L. (2004). Rethinking well-child care. Pediatrics, 114(1), 210–216.
Seligman, M. E. (1995). The effectiveness of psychotherapy: The Consumer Reports study. American Psychologist, 50(12), 965.
Solberg, L. I., Nordin, J. D., Bryant, T. L., Kristensen, A. H., & Maloney, S. K. (2009). Clinical preventive services for adolescents. American Journal of Preventive Medicine, 37(5), 445–454.
U.S. Department of Health and Human Services. (2015). Preventative Care. Retrieved from http://www.hhs.gov/healthcare/about-the-law/preventive-care/index.html.
Van Cleve, S. N., Hawkins-Walsh, E., & Shafer, S. (2013). Integrating mental health in pediatric primary care. Journal for Nurse Practitioners, 9(4), 243–248.
Von Korff, M., Glasgow, R. E., & Sharpe, M. (2002). ABC of psychological medicine: Organising care for chronic illness. BMJ: British Medical Journal, 325(7355), 92.
Wang, P. S., Berglund, P., & Kessler, R. C. (2000). Recent care of common mental disorders in the United States. Journal of General Internal Medicine, 15(5), 284–292.
Wang, P. S., Berglund, P., Olfson, M., Pincus, H. A., Wells, K. B., & Kessler, R. C. (2005). Failure and delay in initial treatment contact after first onset of mental disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry, 62(6), 603.
Wang, P. S., Lane, M., Olfson, M., Pincus, H. A., Wells, K. B., & Kessler, R. C. (2005). Twelve-month use of mental health services in the United States: Results from the National Comorbidity Survey Replication. Archives of General Psychiatry, 62(6), 629.
Werch, C. E., & Owen, D. M. (2002). Iatrogenic effects of alcohol and drug prevention programs. Journal of Studies on Alcohol and Drugs, 63(5), 581.
World Health Organization. (2008). Integrating mental health into primary care: A global perspective. Geneva, Switzerland: WHO Press.
Zeiss, A. M., & Karlin, B. E. (2008). Integrating mental health and primary care services in the Department of Veterans Affairs health care system. Journal of Clinical Psychology in Medical Settings, 15(1), 73–78.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this chapter
Cite this chapter
Snipes, C., O’Donohue, W. (2017). The Integrated Well-Child Visit: Behavioral Health Treatment Engagement in Pediatric Primary Care. In: O'Donohue, W., James, L., Snipes, C. (eds) Practical Strategies and Tools to Promote Treatment Engagement. Springer, Cham. https://doi.org/10.1007/978-3-319-49206-3_8
Download citation
DOI: https://doi.org/10.1007/978-3-319-49206-3_8
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-49204-9
Online ISBN: 978-3-319-49206-3
eBook Packages: Behavioral Science and PsychologyBehavioral Science and Psychology (R0)