Abstract
Multi-criteria decision analysis (MCDA) has the potential to support better healthcare decision making. But a number of challenges need to be overcome before it can achieve its potential. These are both technical – which weighting methods are most appropriate and how should uncertainty be dealt with – and political, the need to work with decision makers to get their support for such approaches. This collection is a first attempt to identify and address these challenges by bringing together MCDA practitioners from what has to date been a relatively fragmented research community. This introductory chapter describes the potential of MCDA in healthcare; provides an outline of the chapters in the collection, the process of developing the collection; and identifies key question, the answers to which will determine the future direction of MCDA in healthcare.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1.1 Introduction
Increased awareness of how multi-criteria decision analysis (MCDA) can support healthcare decision making has resulted in an increased interest in and application of MCDA in healthcare. As with any new technique, however, achieving the potential of MCDA in healthcare faces a number of challenges. To those unfamiliar with MCDA, the diversity of approaches and uses can often be a barrier to its use, making it difficult to understand what it is and how it can best be used. This obstacle is compounded by the fragmented nature of the MCDA research community, with practitioners coming from different academic and policy backgrounds, recommending different approaches and there being no space for this community to meet, share ideas, learn from each other and develop a more coherent vision for the application of MCDA in healthcare. We envisioned this collection of papers as a first step in overcoming some of these obstacles.
MCDA is the collective heading for several analytical techniques used to support decision making in the context of multiple, conflicting criteria (Belton and Stewart 2002). These techniques support decision makers to agree which assessment criteria are relevant, the importance attached to each and how to use this information to assess alternatives. By doing so, they can help increase the consistency, transparency and legitimacy of decisions.
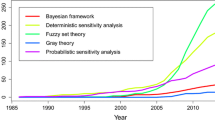
MCDA comprises a broad set of methodological approaches, originating from operations research, yet with a rich intellectual grounding in other disciplines (Kaksalan et al. 2011). They are widely used in both public- and private-sector decisions on transport, immigration, education, investment, environment, energy, defence, etc. (Dodgson et al. 2009). The healthcare sector has been relatively slow to apply MCDA. But as more researchers and practitioners have become aware of the techniques, there has been a sharp increase in its healthcare application (Diaby et al. 2013; Marsh et al. 2014).
The application of MCDA to healthcare should be seen as a natural extension of evidence-based medicine (EBM) and associated practices, such as health technology assessment. Over the past 40 years, the provision of healthcare has been revolutionised by the use of EBM – the systematic reviewing, appraisal and use of clinical research to aid the delivery of optimum clinical care to patients (see Belsey 2009). Whilst the achievements of EBM are not to be underestimated, it has to date only addressed part of the challenge facing healthcare decision making – the rigorous measurement of the performance of alternatives. This emphasis of EBM is continued by MCDA. But MCDA also provides a set of techniques for determining which elements of performance should be measured, how stakeholder preferences for changes performance should be elicited and how data on performance and preferences should be combined to assess alternatives. By doing so, MCDA allows the rigour which EBM has brought to the quantification of performance to be extended to the understanding of stakeholders preferences (Weernink et al. 2014).
Healthcare decisions are rarely simple, involving multiple factors, multiple options, imperfect information and diverse stakeholder preferences. EBM has established the importance of rigorous measurement of alternatives against multiple factors. Using this information can, however, still involve significant cognitive burden. Decision makers have difficulty processing and systematically evaluating relevant information, a process that involves trading off between multiple factors. In these circumstances, relying on informal processes or judgements can lead to suboptimal decisions (Baltussen and Niessen 2006). MCDA provides support and structure to the decision-making process to overcome such challenges.
A challenge for users of MCDA, however, is that there are many different MCDA methods available; the current field is fragmented, with methods being selected based on researchers’ background and previous experience, rather than a systematic consideration of the ‘best’ approach; and there is little guidance on how to choose between the available approaches (Marsh et al. 2014). The objective of this collection is to support the use of MCDA in healthcare by, for the first time, bringing together researchers specialising in numerous approaches and healthcare decisions and giving the reader the benefit of this rich experience. To support the reader to select between MCDA techniques, we illustrate and critically appraise this diversity of MCDA approaches as applied to healthcare, summarise the ethical and theoretical foundations of MCDA and offer good practice guidelines when using MCDA in healthcare to help the reader select between MCDA techniques.
1.2 Process of Developing the Book
We were approached by Springer in April 2014 to produce a collection of papers on MCDA, specifically ‘Healthcare Decisions Supported by Multi-Criteria Decision Analysis’. Our first steps were to put together an outline of the book (see below), develop a brief description of each chapter and identify authors who we would ideally want to lead the writing of each chapter. We were delighted at the response from our lead authors, who were all enthusiastic about contributing to the collection.
In what is quite unusual for most books, we were able to organise a face-to-face workshop to bring authors together to present and discuss their chapters. The workshop was held in Amsterdam late June 2015 and was made possible by funding from Radboud University Medical Center, through a personal VICI grant obtained by Rob Baltussen from the Netherlands Organisation for Scientific Research (NWO). There was a great turnout, with all but one of the chapters being represented by an author. All the chapters were presented, received comments from a nominated discussant (lead author from another chapter) and discussed by the attendees. This workshop provided everyone with a better idea of how the collection is structured, where their chapters fits in, and with comments to take on board as they finalised their chapters. We would like to thank Evelinn Mikkelsen for her support in organising this workshop.
1.3 Outline of the Book
This book is organised into different sections, each with a different emphasis. Before we get into the detail, it should be noted that most of the examples presented in the book are weighted-sum MCDA models (value measurement approaches). Whilst we acknowledge that there are other MCDA approaches (see Chapter 15 for an overview of these non-value measurement methods), most of the applications of MCDA in healthcare are value measurement methods, and thus, this has also been the focus of this book.
Section one presents the foundations of MCDA as it is applied to healthcare decisions, providing guidance on the ethical and theoretical underpinnings of MCDA, and how to select MCDA methods appropriate to different decision settings. Chapter 2 presents the theoretical foundations, and Chapter 3 presents the ethical aspects of MCDA in healthcare. Chapter 4 highlights the diversity of weighting/scoring methods in MCDA and addresses their relative merits and weaknesses. Chapter 5 considers alternative approaches for dealing with uncertainty in MCDA.
Section two comprises a collection of case studies spanning the decision continuum, including portfolio development, benefit-risk assessment, health technology assessment, priority setting, resource optimisation, clinical practice and shared decision making. Chapter 6 presents optimisation of a robotics research and development portfolio using MACBETH. Chapter 7 illustrates the use of MCDA for benefit-risk analysis of drugs. Chapter 8 presents the experiences of Health Technology Assessment (HTA) agencies with MCDA in Colombia, Italy and Belgium. Chapter 9 presents the experiences of using MCDA for priority setting in low- and middle-income countries. Chapter 10 presents a case study of the use of MCDA for resource allocation in South Yorkshire, UK. Chapter 11 presents the use of conjoint analysis and analytic hierarchy process for shared decision making in clinical settings. Chapter 12 highlights the similarities between health research priority setting and health intervention priority setting and presents suggestions for future methodological research. Chapter 13 presents applications of MCDA for clinical practice guidelines and clinical research prioritisation.
Section three explores future directions in the application of MCDA to healthcare. Chapter 14 highlights the issues and opportunities associated with the use of MCDA within HTA. Chapter 15 presents the non-value-based measurement methods and when conditions under which they would be appropriate. Finally, Chapter 16 presents the good practice general principles that need consideration during the design, conduct and analysis of MCDA in healthcare.
1.4 Future Direction
This collection presents the current state of reflection, knowledge and applications on MCDA for healthcare decision making worldwide. Future developments rest on providing clear answers to simple questions: Why do we need MCDA in healthcare? What can it bring? Is it worth it?
As healthcare users, providers and payers around the world are facing critical ethical dilemmas, current decision-making approaches are reaching their limits. EBM was developed to ensure best choices at a clinical level, health economics to ensure informed allocation of resources and HTA to ensure best choices and health system sustainability. However, the need to go beyond these approach is highlighted by the controversy on an ‘acceptably cost-effective’ treatment for hepatitis C, which is challenging the sustainability of healthcare systems worldwide (Neuman and Cohen 2015) and issues raised by the reimbursement of treatments for patients with rare diseases which require consideration of many aspects that are not formally contained in current HTA methods (Wagner et al. 2016). Our time calls for ways to define value of interventions based on the social values on which healthcare systems are founded to guide prioritisation and investment in interventions with highest value and disinvestment of those with low value. MCDA is poised to build on EBM and HTA to provide an integrative methodology to help tackle these current challenges and transition into healthcare of the twenty-first century.
As illustrated in the present collection, MCDA offers a structured approach to support reasonable and accountable decision making (Daniels and Sabin 1997). Doing this at either individual or collective levels, it can support many decisions to improve population outcomes and promote sustainability, including shared decision making, clinical research, clinical practice guidelines, portfolio development, health technology assessment, priority setting and resource optimisation.
Transitioning to a wider use of MCDA will require some adaptation to address healthcare specificities. Technical aspects of MCDA will have to be developed with the end of healthcare decision makers in mind. This will require answer to the following questions: Whose preference matter for different decisions? Which weighting methods are most appropriate for different decisions? How can uncertainty in MCDA be dealt with to support decision makers? How can opportunity cost be measured in a MCDA framework? Research and debates are required on best approaches to tackle these issues.
Beyond the technical questions, further work is required to manage decision makers’ concerns about the function of MCDA. Specifically, decision makers may have the perception that MCDA is a way to replace reflection and to algorithmically make decisions. It is important to educate decision makers that MCDA is designed to support reflection to ensure balanced and accountable decision-making processes. Decision makers should also be engaged on the principles that inform decision making and how these relate to the assumptions underlying alternative MCDA approaches.
In conclusion, MCDA can help us develop a healthcare system focused on what truly matters to patients and populations, in a fair and sustainable manner. Given this potential, the time has come for MCDA developers and users to answer the above questions and demonstrate the value that these methods can bring. We hope this collection is a first step in the process, demonstrating where MCDA has been used in healthcare to date, drawing the lessons from this experience and identifying the research agenda required for MCDA to achieve its potential.
References
Baltussen R, Niessen L (2006) Priority setting of health interventions: the need for multi-criteria decision analysis. Cost Eff Resour Alloc 4:14
Belsey J (2009) What is evidence-based medicine? Hayward Medical Communications, London
Belton V, Stewart TJ (2002) Multiple criteria decision analysis: an integrated approach. Kluwer Academic Publishers, Boston
Daniels N, Sabin J (1997) Limits to health care: fair procedures, democratic deliberation, and the legitimacy problem for insurers. Philos Public Aff 26(4):303–350
Diaby V, Campbell K, Goeree R (2013) Multi-criteria decision analysis (MCDA) in health care: a bibliometric analysis. Oper Res Health Care 2(1–2):20–24
Dodgson J, Spackman M, Pearman A, Phillips L. (2009) Multi-criteria analysis: a manual. Department for Communities and Local Government. London. http://www.communities.gov.uk/documents/corporate/pdf/1132618.pdf
Kaksalan M, Wallenius J, Zionts S (2011) Multiple criteria decision making from early history to the 21st century. World Scientific, Singapore
Neuman P, Cohen J (2015) Measuring the value of prescription drugs. N Engl J Med 20:1–4
Marsh K, Lanitis T, Neasham D et al (2014) Assessing the value of health care interventions using multi-criteria decision analysis: a review of the literature. Pharmacoeconomics 32(4):345–65
Wagner M, Khoury H, Willet J, Rindress D, Goetghebeur M (2016) Can the EVIDEM framework tackle issues raised by evaluating treatments for rare diseases: analysis of issues and policies, and context-specific adaptation. Pharmacoeconomics 34(3):285–301
Weernink MGM, Janus SIM, van Til JA, Raisch DW, van Manen JG, Ijzerman MJ (2014) A systematic review to identify the use of preference elicitation method in healthcare decision making. Pharm Med 28:175–185
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this chapter
Cite this chapter
Marsh, K., Goetghebeur, M., Thokala, P., Baltussen, R. (2017). Introduction. In: Marsh, K., Goetghebeur, M., Thokala, P., Baltussen, R. (eds) Multi-Criteria Decision Analysis to Support Healthcare Decisions. Springer, Cham. https://doi.org/10.1007/978-3-319-47540-0_1
Download citation
DOI: https://doi.org/10.1007/978-3-319-47540-0_1
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-47538-7
Online ISBN: 978-3-319-47540-0
eBook Packages: MedicineMedicine (R0)