Abstract
Cardiovascular disease is the leading cause of death in the Western world. One of the major underlying pathologies of cardiovascular disease is atherosclerosis. Atherogenesis is a multifactorial process; hypercholesterolemia represents a major risk factor for atherosclerotic changes. Hypolipidemic drugs including statins have paramount importance in managing patients with chronic cardiovascular disease.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Coronary Artery Bypass Grafting
- Acute Kidney Injury
- Statin Therapy
- Coronary Artery Bypass Grafting Surgery
- Noncardiac Surgery
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
16.1 General Principles
Cardiovascular disease is the leading cause of death in the Western world. One of the major underlying pathologies of cardiovascular disease is atherosclerosis. Atherogenesis is a multifactorial process; hypercholesterolemia represents a major risk factor for atherosclerotic changes. Hypolipidemic drugs including statins have paramount importance in managing patients with chronic cardiovascular disease.
Statins reduce the risk of myocardial infarction (MI), stroke, and death due to the reduction of plasma cholesterol levels. Other pharmacodynamic effects exerted by statins, commonly recognized as “pleiotropic,” include improving endothelial function, attenuating vascular and myocardial remodeling, reducing inflammation in vascular wall, inhibiting platelets, and stabilizing atherosclerotic plaques, thus preventing their rupture [1]. These underpinning mechanisms form the basis for the use of statins aimed at reducing morbidity and mortality associated with surgery.
The majority of studies published hitherto clearly favored the use of statins during perioperative period. However, recent data lessen this enthusiasm, revealing that statins may worsen renal function in cardiac surgical patients. For these reasons, the recent Consensus Conference Update on the reduction of perioperative mortality did not include statins among the drugs with proven survival benefit [2, 3]. Taking into consideration the frequent use of statins among patients scheduled for major surgical procedures, extensive discussion of current and coming data can be expected. This chapter is built on currently (June 2016) available evidence including international guidelines.
16.2 Main Evidences
Many clinical studies demonstrated that perioperative therapy with statins reduces not only morbidity but also mortality associated with the surgery.
One of the first prospective randomized controlled trials (RCTs) in cardiac surgery showed that simvastatin (20 mg/day for 4 weeks) administered before coronary artery bypass grafting (CABG) in patients with hypercholesterolemia decreased not only LDL (low-density lipoproteins)-cholesterol and total serum cholesterol levels before the surgery, but significantly lowered the occurrence of thrombocytosis, renal failure, and MI in postoperative period [4].
A double-blind RCT with fluvastatin started before vascular surgery and continued for at least 30 days afterward showed a reduced occurrence of myocardial ischemia (10.8 vs. 19.0 %) and composite of death from cardiovascular causes and nonfatal MI (4.8 vs. 10.1 %) [5].
A retrospective analysis of data from 16,192 patients (≥40 years) undergoing CABG explored the association of various preoperative cardiovascular medications with perioperative outcomes [6]. Statins were the most prevalent drug used (85.1 %), even more than beta-blockers (72.8 %). Preoperative statin administration was associated with reduced postoperative mortality (0.4 vs. 0.8 %, odds ratio adjusted to various confounders 0.26–0.35). Analysis of different statins and their doses revealed interesting fact that only simvastatin 40 mg was protective. This could be ascribed to smaller number of other statins.
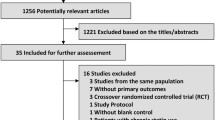
Another meta-analysis (16 RCTs, 2,275 patients) examined the influence of perioperative statin therapy on postoperative outcomes in patients without long-term statin therapy [7]. This approach significantly reduced mortality (1.8 vs. 3.4 %) and the incidence of MI (4.1 vs. 8.9 %). The incidence of stroke was not significantly reduced (1.0 vs. 1.7 %). Moreover, statin therapy significantly reduced the incidence of postoperative atrial fibrillation (AF) (12.1 vs. 23.4 %) and in-hospital length of stay (LOS). Most of included RCTs were from CABG patients, two studies were from vascular surgery, and only one from non-cardiovascular surgery. Subgroup analysis of noncardiac surgical patients revealed significant reduction in mortality and MI, but not in stroke, AF, or hospital LOS. Subanalysis exploring duration of statin therapy showed significant reduction in mortality and the incidence of MI only when statin administration was started more than 1 week before surgery.
16.3 Pharmacological Properties
Statins are competitive inhibitors of 3-hydroxy-3-methylglutaryl-coenzyme A (HMG-CoA) reductase, which is the rate-limiting step in the biosynthesis of cholesterol. Inhibition of this enzyme reduces plasma levels of total and LDL-cholesterol by 17–35 % and 24–49 %, respectively [8]. Moreover, plasma level of triglycerides also reduces and plasma level of HDL (high-density lipoproteins)-cholesterol increases.
Statins differ in their pharmacokinetic and pharmacodynamic properties. Lipophilic statins (active at hepatic and extrahepatic sites) include atorvastatin, fluvastatin, lovastatin, simvastatin, and cerivastatin. Hydrophilic statins (active mainly in the liver) are represented by rosuvastatin and pravastatin [9]. Regarding potency for reducing LDL-cholesterol levels, statins can be classified as highly potent (atorvastatin and rosuvastatin) and low potent (simvastatin, fluvastatin, lovastatin, and pravastatin) [10]. The major enzymatic pathway in statin pharmacokinetics includes cytochrome (CYP) P450 enzymes family in the liver, except rosuvastatin and pravastatin. Coadministration of drugs with a higher affinity for CYP3A4 isoenzyme increases plasma levels and bioavailability of statins with associated risk of side effects. Simvastatin, lovastatin, and atorvastatin have the strongest potential for pharmacological interactions [9]. Statins are administered orally; intravenous formulation is not available. Statins with long half-life (atorvastatin) or extended-release formulations (lovastatin) can be preferred before the surgery if a prolonged break in postoperative oral intake is expected [11]. After initiation of statin therapy, full hypolipidemic potential is achieved after 4–6 weeks, with 75 % of effect seen after 2 weeks [12]. Other beneficial effects (e.g., improved endothelial function) could be seen within days.
Statins can induce class-related adverse reactions. Muscle-related side effects (1.5–5 % of patients) range from myalgia, myopathy, and myositis to myonecrosis with increases of creatinine kinase or even clinically significant rhabdomyolysis with acute renal failure [13]. An isolated increase in liver enzymes is usually benign. Adverse reactions are more frequent with higher doses, advanced age, small body surface area, and chronic conditions as renal failure, liver dysfunction, and alcoholism.
16.4 Therapeutic Use
16.4.1 Cardiac Surgery
In cardiac surgery, the ACC/AHA guidelines (2011) recommend statin therapy for all hyperlipidemic patients undergoing CABG surgery. In patients presenting for urgent/emergent CABG, statins should be initiated immediately. Discontinuation of statin therapy is not recommended [14].
16.4.1.1 CABG
Pooled analysis of data from 13 studies (19,542 patients) demonstrated a statistically significant 45 % reduction in postoperative all-cause mortality with preoperative statin therapy relative to control [15].
In a large retrospective evaluation of multiple cardiovascular drugs used in cardiac patients, statins appear consistently protective against perioperative mortality (statins 0.4 % vs. non-statins 0.8 %) from CABG surgery in multiple models. Simvastatin 40 mg was the only statin in a given dose from those tested that showed protective effects [6]. The salutary effects on mortality are consistent with prior meta-analyses [16, 17].
In contrast, a contemporary Cochrane review of six studies in CABG patients concluded that preoperative statin therapy reduced the odds of postoperative AF and shortened the ICU and hospital LOS but had no influence on perioperative mortality, stroke, MI or renal failure [18]. Another meta-analysis (12 RCTs, 1,116 patients) confirmed beneficial effects on decreased incidence of AF and hospital LOS, with more robust effects after CABG vs. heart valve surgery [19]. Lower rates of AF and perioperative MI after cardiac surgery were also reported with only short-term pretreatment with statins (<3 weeks). In-hospital mortality and stroke rate were also lower with statin therapy although non-significantly [20].
16.4.1.2 Valvular Surgery
In high-risk non-emergent isolated heart valve surgery, preoperative statin therapy had beneficial effect on postoperative mortality [21]. These results were upheld in a recent meta-analysis of ten observational studies (22,518 patients). A significant reduction by statin therapy also was observed for AF, but not for postoperative stroke, MI, or renal failure [22].
16.4.1.3 Heart Transplantation
In a small longitudinal study, heart transplant recipients were treated with pravastatin or control from the time of surgery. Importantly, the majority of control patients were switched to pravastatin during the ten-year follow-up. In an intention-to-treat analysis, pravastatin group compared with control had increased survival and appeared to have reduced development of cardiac allograft vasculopathy [23].
16.4.1.4 Kidney Injury After Cardiac Surgery
Analysis of previously available data did not suggest that preoperative statin use is associated with decreased incidence of acute kidney injury (AKI) in adults after CABG [24, 25]. Patients undergoing CABG might benefit from preoperative statin treatment due to the reduction in the need for postoperative renal replacement therapy and mortality. The effects of reno-protective efficacy of preoperative statin therapy in patients undergoing isolated heart valve surgery remain uncertain [25].
Two recent major RCTs investigating the effects of statins in cardiac surgical patients revealed negative effect of statins on postoperative renal function. In Statin AKI Cardiac Surgery RCT [26], short-term high-dose atorvastatin was started before cardiac surgery. Overall, AKI occurred in 20.8 % of patients in the atorvastatin group compared to 19.5 % in the placebo group; among patients without chronic statin administration, AKI occurred in 21.6 % of patients treated by atorvastatin vs. 13.4 % in the placebo group. None of these differences reached statistical significance and the study was stopped prematurely for futility. The STICS (Statin Therapy in Cardiac Surgery) RCT [27] randomized 1,922 cardiac surgical patients to 20 mg of rosuvastatin daily or placebo. Statin therapy was initiated shortly before the surgery, with maximum duration of up to 8 days. Primary outcomes, i.e., the rate of postoperative AF within 5 days after the surgery and extent of myocardial injury, did not significantly differ between the groups. However, statin administration was associated with a significant absolute 5 % increase in the occurrence of postoperative AKI at 48 h. The effects at delayed timepoints or the need for renal replacement therapies were not reported.
16.4.2 Vascular Surgery
Patients with peripheral artery disease represent a unique target population in which statin therapy could be beneficial. Indeed, in a nonoperative management of patients with lower limb atherosclerotic arterial disease, statin therapy seems to be effective in reducing all-cause mortality and the incidence of cerebrovascular events [28].
Several studies investigated the effects of statins in patients undergoing vascular surgery. Perioperative fluvastatin therapy was associated with an improvement in postoperative cardiac outcome [5]. Recently published meta-analysis compared short-term statin therapy, either commenced de novo or with existing users randomly assigned to different dosages, in adult participants undergoing elective and emergency noncardiac arterial surgery, including both open and endovascular procedures. Evidence was insufficient to allow to conclude whether statin therapy resulted in either a reduction or an increase in any of the outcomes recorded. Pooled results from three studies (178 participants) showed mortality of 6.7 % in the statin group vs. 13.7 % in the control group [29].
In a retrospective analysis of patients undergoing carotid endarterectomy, statins significantly decreased death rates in diabetic patients and tended to decrease both death and stroke rates in patients with diabetes and with hypercholesterolemia but had no effect on post-procedural restenosis [30].
16.4.3 Noncardiac Surgery
Regarding noncardiac surgery, the ACC/AHA guidelines on perioperative cardiovascular evaluation and management (2014) recommend continuing statins in patients who are currently under this treatment. Perioperative initiation of statin therapy is reasonable in patients undergoing vascular surgery and may be considered in patients with a clinical risk factor undergoing high-risk procedures [31]. Similar guidelines developed by European scientific societies ESC and ESA (2014) state that perioperative continuation of statins is recommended, favoring statins with a long half-life or extended-release formulation. Preoperative initiation of statins should be considered in patients undergoing vascular surgery, ideally at least 2 weeks before the surgery [11].
In a large randomized prospective multicentric study in noncardiac surgery, preoperative statin treatment was independently associated with a lower risk of composite cardiovascular outcomes (all-cause mortality, myocardial injury, or stroke) at 30 days after the surgery. Statins were also associated with a significantly lower risk of all-cause mortality (relative risk 0.58), cardiovascular mortality (relative risk 0.42), and myocardial injury (relative risk 0.86). However, there were no statistically significant differences in the risk of MI or stroke [32]. Meta-analysis of studies exploring the effects of statins on AKI after major surgery showed that preoperative statin therapy was associated with a significant risk reduction for postoperative AKI and need for renal replacement therapy. These benefits were, however, not observed when restricting the analysis only to available RCTs [31].
In kidney transplant recipients, statins may reduce cardiovascular events. Statins had uncertain effects on overall mortality, stroke, kidney function, and toxicity outcomes [33].
Conclusion
Statins are effective hypolipidemic agents with other important “pleiotropic” effects. They have well-established role in primary and secondary prevention of cardiovascular disease.
In cardiac surgery, preoperative statin therapy reduces the odds of postoperative AF and reduces ICU and in-hospital LOS. The effects on MI and stroke are generally positive, with some reports showing benefits on individual outcome parameters but none showing harm. Results from patients undergoing CABG are more robust than after other cardiac surgical procedures such as valvular or aortic surgery. However, recent studies revealed an increased occurrence of AKI associated with statins in cardiac surgical patients. Furthermore, ongoing studies including robust meta-analyses will shed the light on the issue of statin-associated changes in perioperative mortality.
Statins decreased mortality in nonsurgically managed patients with peripheral vascular disease. The effects in patients with vascular surgery were not consistent, but some studies suggested improved outcomes including mortality in patients with specific comorbidities. In patients undergoing major noncardiac surgery, statins may decrease mortality.
Taking into account currently available evidence, continued statin administration in the patients receiving statins preoperatively is recommended. Commencement of statin therapy before cardiac, vascular, and major noncardiac surgery should be considered with caution as recent studies have pointed out the risks associated with statins.
References
Zhou Q, Liao JK (2010) Pleiotropic effects of statins. Basic research and clinical perspectives. Circ J 74:818–826
Landoni G, Rodseth RN, Santini F et al (2012) Randomized evidence for reduction of perioperative mortality. J Cardiothorac Vasc Anesth 26:764–772
Landoni G, Pisano A, Lomivorotov V et al (2016) Randomized evidence for reduction of perioperative mortality: an updated consensus process. J Cardiothorac Vasc Anesth. 2016 Aug 2. pii: S1053-0770(16)30281-6. doi:10.1053/j.jvca.2016.07.017. [Epub ahead of print]
Christenson JT (1999) Preoperative lipid-control with simvastatin reduces the risk of postoperative thrombocytosis and thrombotic complications following CABG. Eur J Cardiothorac Surg 15:394–399
Schouten O, Boersma E, Hoeks SE et al (2009) Fluvastatin and perioperative events in patients undergoing vascular surgery. N Engl J Med 361:980–989
Venkatesan S, Okoli GN, Mozid AM et al (2016) Effects of five preoperative cardiovascular drugs on mortality after coronary artery bypass surgery: a retrospective analysis of an observational study of 16 192 patients. Eur J Anaesthesiol 33:49–57
de Waal BA, Buise MP, van Zundert AA (2015) Perioperative statin therapy in patients at high risk for cardiovascular morbidity undergoing surgery: a review. Br J Anaesth 114:44–52
Edwards JE, Moore RA (2003) Statins in hypercholesterolaemia: a dose-specific meta-analysis of lipid changes in randomised, double blind trials. BMC Fam Pract 4:18
Gazzerro P, Proto MC, Gangemi G et al (2012) Pharmacological actions of statins: a critical appraisal in the management of cancer. Pharmacol Rev 64:102–146
Conly J, Clement F, Tonelli M et al (2011) Cost-effectiveness of the use of low- and high-potency statins in people at low cardiovascular risk. CMAJ 183:E1180–E1188
Kristensen SD, Knuuti J, Saraste A et al (2014) 2014 ESC/ESA guidelines on non-cardiac surgery: cardiovascular assessment and management. The Joint Task Force on non-cardiac surgery: cardiovascular assessment and management of the European Society of Cardiology (ESC) and the European Society of Anaesthesiology (ESA). Eur J Anaesthesiol 31:517–573
Biccard BM (2008) A peri-operative statin update for non-cardiac surgery. Part I: the effects of statin therapy on atherosclerotic disease and lessons learnt from statin therapy in medical (non-surgical) patients. Anaesthesia 63:52–64
Rosenson RS, Baker SK, Jacobson TA et al (2014) An assessment by the statin muscle safety task force: 2014 update. J Clin Lipidol 8:S58–S71
Hillis LD, Smith PK, Anderson JL et al (2011) 2011 ACCF/AHA guideline for coronary artery bypass graft surgery. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Developed in collaboration with the American Association for Thoracic Surgery, Society of Cardiovascular Anesthesiologists, and Society of Thoracic Surgeons. J Am Coll Cardiol 58:e123–e210
Takagi H, Kawai N, Umemoto T (2009) Preoperative statin therapy reduces postoperative all-cause mortality in cardiac surgery: a meta-analysis of controlled studies. J Thorac Cardiovasc Surg 137:e52–e53
Kuhn EW, Liakopoulos OJ, Stange S et al (2013) Meta-analysis of patients taking statins before revascularization and aortic valve surgery. Ann Thorac Surg 96:1508–1516
Kuhn EW, Liakopoulos OJ, Stange S et al (2014) Preoperative statin therapy in cardiac surgery: a meta-analysis of 90,000 patients. Eur J Cardiothorac Surg 45:17–26
Kuhn EW, Slottosch I, Wahlers T et al (2015) Preoperative statin therapy for patients undergoing cardiac surgery. Cochrane Database Syst Rev (8):CD008493
Rezaei Y, Gholami-Fesharaki M, Dehghani MR et al (2016) Statin antiarrhythmic effect on atrial fibrillation in statin-naive patients undergoing cardiac surgery: a meta-analysis of randomized controlled trials. J Cardiovasc Pharmacol Ther 21:167–76, pii: 1074248415602557
Patti G, Bennett R, Seshasai SR et al (2015) Statin pretreatment and risk of in-hospital atrial fibrillation among patients undergoing cardiac surgery: a collaborative meta-analysis of 11 randomized controlled trials. Europace 17:855–863
Allou N, Augustin P, Dufour G et al (2010) Preoperative statin treatment is associated with reduced postoperative mortality after isolated cardiac valve surgery in high-risk patients. J Cardiothorac Vasc Anesth 24:921–926
Cheng X, Hu Q, Liu Z, Tang X (2015) Preoperative statin therapy decreases early mortality in patients undergoing isolated valve surgery: result from a meta-analysis. J Cardiothorac Vasc Anesth 29:107–114
Kobashigawa JA, Moriguchi JD, Laks H et al (2005) Ten-year follow-up of a randomized trial of pravastatin in heart transplant patients. J Heart Lung Transplant 24:1736–1740
Lewicki M, Ng I, Schneider AG (2015) HMG CoA reductase inhibitors (statins) for preventing acute kidney injury after surgical procedures requiring cardiac bypass. Cochrane Database Syst Rev (3):CD010480
Singh I, Rajagopalan S, Srinivasan A et al (2013) Preoperative statin therapy is associated with lower requirement of renal replacement therapy in patients undergoing cardiac surgery: a meta-analysis of observational studies. Interact Cardiovasc Thorac Surg 17:345–352
Billings FT IV, Hendricks PA, Schildcrout JS et al (2016) High-dose perioperative atorvastatin and acute kidney injury following cardiac surgery: a randomized clinical trial. JAMA 315:877–888
Zheng Z, Jayaram R, Jiang L et al (2016) Perioperative rosuvastatin in cardiac surgery. N Engl J Med 374:1744–1753
Antoniou GA, Fisher RK, Georgiadis GS et al (2014) Statin therapy in lower limb peripheral arterial disease: systematic review and meta-analysis. Vascul Pharmacol 63:79–87
Sanders RD, Nicholson A, Lewis SR et al (2013) Perioperative statin therapy for improving outcomes during and after noncardiac vascular surgery. Cochrane Database Syst Rev (7):CD009971
AbuRahma AF, Srivastava M, Stone PA et al (2015) Effect of statins on early and late clinical outcomes of carotid endarterectomy and the rate of post-carotid endarterectomy restenosis. J Am Coll Surg 220:481–487
Fleisher LA, Fleischmann KE, Auerbach AD et al (2014) 2014 ACC/AHA guideline on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 130:e278–e333
Berwanger O, Le Manach Y, Suzumura EA et al (2016) Association between pre-operative statin use and major cardiovascular complications among patients undergoing non-cardiac surgery: the VISION study. Eur Heart J 37:177–185
Palmer SC, Navaneethan SD, Craig JC et al (2014) HMG CoA reductase inhibitors (statins) for kidney transplant recipients. Cochrane Database Syst Rev 2014;(1):CD005019
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Summary Table
Summary Table
Clinical summary | ||||
|---|---|---|---|---|
Indications | Cautions | Side effects | Dose | Notes |
Hypercholesterolemia Primary and secondary prevention of cardiovascular disease | Muscle-related (myalgia, myopathy, myonecrosis, rhabdomyolysis) in 1.5–5 % of the patients Isolated increase in liver enzymes (usually benign) | Depending on particular statin: 10–80 mg once daily | Statin therapy should be continued in perioperative period | |
Reducing perioperative risk in cardiac, vascular, and major noncardiac surgery | Possible increased occurrence of postoperative AKI and ambiguous effect on mortality | Existing statin therapy should be continued; commencement of new statin therapy treatment before the surgery (1–3 weeks) could be considered with appropriate caution | ||
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this chapter
Cite this chapter
Riha, H., Drabek, T. (2017). Statins and Perioperative Mortality. In: Landoni, G., Ruggeri, L., Zangrillo, A. (eds) Reducing Mortality in the Perioperative Period. Springer, Cham. https://doi.org/10.1007/978-3-319-46696-5_16
Download citation
DOI: https://doi.org/10.1007/978-3-319-46696-5_16
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-46695-8
Online ISBN: 978-3-319-46696-5
eBook Packages: MedicineMedicine (R0)