Abstract
Worldwide, the average prevalence of spinal cord injury (SCI) is estimated to be 1:1000, and the mean incidence is proposed to be between 4 and 9 cases per 100,000 population per year. Numbers vary substantially for different parts of the world. The mean incidence of SCI in developing countries is estimated to be 25.5/million/year with a range between 2.1 and 130.7/million/year. The incidence of SCI in industrialized countries ranges from 15 in Western Europe to 39/million/year in the USA. Most common causes for traumatic SCI are traffic accidents, falls, and results of violence, whereas the leading causes of non-traumatic SCI (NTSCI) are degenerative diseases and tumors (developed countries) and infections, particularly tuberculosis and HIV (developing countries). The majority of people with traumatic SCI are males (ratio men/women = 3:1), whereas in non-traumatic SCI, genders are almost equally distributed. Worldwide NTSCI increases significantly as well as the number of high-level tetraplegic patients with the need for permanent or artificial ventilation. In general, the percentage of tetraplegic patients has increased and nowadays equals that of paraplegic patients. Additionally, in industrialized countries, the mean age at the time of injury increases continuously, mostly due to older patients also experiencing SCI. The mortality rate in the first phase after SCI is directly linked to the availability and quality of primary care and rehabilitation approaches. Life expectancy is determined by the level of integration into a proper socioeconomic environment after initial treatment and directly related to the availability of qualified medical care in the event of complications such as pressure ulcers or urological problems.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Spinal Cord Injury
- Spinal Cord Injury Patient
- Traumatic Spinal Cord Injury
- Spinal Cord Injury Population
- Spinal Cord Disease
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
In order to understand the sociopolitical, health-related, and socioeconomic implication of spinal cord injury (SCI), knowledge about the frequency of occurrence and etiology is required.
This introductory chapter provides basic numbers on prevalence, incidence, mortality, causes of death, and treatment costs of SCI. In particular, the differences between traumatic and non-traumatic causes of SCI and also between regions with high and low income will be elaborated. A correct interpretation of regional differences is of utmost importance, because it allows for a prognosis of the course of numbers in developing and emerging countries.
The presented results are based on the review of the scientific literature and of reports of public administrations of different countries up to 2015 with a strong focus on the most recent available numbers and information.
2 Challenges in Interpretation of Epidemiological Data
Unfortunately, a central worldwide registry for the collection of epidemiological data regarding SCI does not exist. Additionally, even industrialized countries do not often have a national SCI registry, in which data, at least from SCI centers about new cases, are collected. Population-based surveys for estimation of the percentage of persons with SCI in the general population are very rare [1]. Most of the epidemiological data on incidence and prevalence represent extrapolations based on the numbers collected by a few clinical centers or based on assumptions about the mean life expectancy of individuals after SCI, respectively. Due to the different methodologies of data collection and various assumptions, epidemiological data available from the literature usually have a high variance, which makes it impossible to compare data from different sources. There is very sparse information if patients with lesions at the level of the cauda equina or conus medullaris, which results in lesion of peripheral nerves, are classified as patients with SCI and are included in the epidemiological data analysis or not. Even though the incidence and prevalence of cauda equina lesions is relatively low [2], it might explain some of the variations of the data between different sources. The same applies to congenital SCI (spina bifida, meningomyelocele), for which the incidence is estimated to range between 2 and 58 per 10,000 population per year [1].
Epidemiological data might change very rapidly and numbers, which were valid a decade ago, might be obsolete nowadays. This becomes most apparent in countries with high average income, where life expectancy has dramatically increased over the last two to three decades [3].
Especially the rapid increase of cases with non-traumatic SCI within the last few years shows that the date of data acquisition is of significant importance and, as a further consequence, renders the comparison of data from different sources rather impossible.
Especially, data on prevalence and incidence of individuals with tetraplegia due to high SCI with the need for permanent mechanical ventilation or a phrenic nerve stimulator is poor. One of the reasons is that those patients die early after SCI in many countries, even in those with high average income, because either the required medical-technical care cannot be provided or the social system does not contribute financially to home-based ventilation.
3 Prevalence of SCI
In general, the term prevalence describes the proportion of a population living with a certain condition. It is determined by comparing the number of people found to have the condition with the total number of people studied and is usually expressed as a fraction, as a percentage, or as the number of cases per million people. Point prevalence is the proportion of a population that has the condition at a specific point in time. Period prevalence is the proportion of a population that has the condition at some time during a given period (e.g., 12-month prevalence) and includes people who already have the condition at the start of the study period as well as those who acquire it during that period. Lifetime prevalence is the proportion of a population that at some point in their life have experienced the condition. Lifetime prevalence is the term that is often only called “prevalence” in medicine [4]. It is determined by the number of new cases per year and the life expectancy of people with this condition in years. As a consequence prevalence is, on the one side, an estimate for the hazard potential within a society and, on the other side, an indicator for the effectiveness of secondary preventive measures.
A report of the World Health Organization (WHO) shows that 15 % of the world’s population is affected by disability, 0.1 % by spinal cord injury [1]. Hence, the global prevalence of traumatic SCI is estimated to be 1000/million people [5]. However, this number needs to be treated with caution, because it represents only a rough estimate as valid data are available only for a few countries (Table 1.1). Even less reliable data are available on the prevalence of non-traumatic SCI (Table 1.2).
In general, the incidence of traumatic SCI varies substantially between countries. Among the reasons for these country-level variations are genuine country-level differences in incidence related to differences in risk, standard of living and health-care systems, merging of data from adolescents and children (studies reporting only adult incidence overestimate the overall population rate), and differences attributable to methodological approaches. A big problem arises regarding the representativeness of the data, because only a few, mostly (small) countries, have a country-wide SCI registry system, such as Finland or Scotland, and therefore incidence estimates are extrapolated from city or regional data that may not be representative for the country as a whole [1]. It is remarkable that the overall prevalence of SCI (traumatic and non-traumatic) in Iran is with 318/million population, one of the lowest worldwide [14].
4 Incidence of SCI
While prevalence is a measurement of all individuals affected by a condition at a particular time, incidence is a measurement of the number of new individuals who acquire a condition during a particular period of time. The incidence of SCI describes how many people have acquired an injury of the spinal cord within a predefined period of time. It is therefore a descriptive term for the risk of suffering from a certain condition or disease and represents an indirect indicator for the effectiveness of primary preventive measures.
The incidence of SCI including traumatic and non-traumatic lesions is estimated to be between 40 and 83/million/year, with an absolute estimated annual number of new cases worldwide around 250,000–500,000 [15]. The worldwide incidence of only traumatic SCI is estimated to be between 10.4 and 83/million/year [13].
However, these numbers must be interpreted with caution. The determination of the incidence of SCI is highly dependent on a variety of factors, which results in large variations.
Patients with traumatic SCI who die at the scene of the accident or pass away on their way to an emergency room are normally not included in any statistical data evaluation. This also applies to patients with a malignant disease in its final stage involving an SCI. These facts introduce a systematic bias to the overall incidence of SCI resulting in lower estimate.
Similar to the problem of determining a representative value for the prevalence of SCI, the database for determining the incidence of SCI is incomplete and inconsistent. Technical limitations and a systematic bias may be present in data collection in different countries. As a consequence, there are only rough estimates available.
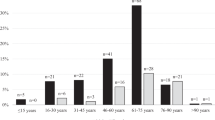
Published data from different countries show enormous differences in the average incidence of SCI [7, 16, 17]. These differences might be explained by different age distributions, hazard potentials, and different levels of emergency treatment. According to a study, the annual incidence of new traumatic SCI rose significantly in persons 55 years and older. The proportion of tetraplegia and of incomplete injuries also increased. Additionally traumatic SCI occurs mostly at a young age, below 30 years [18, 19], whereas non-traumatic spinal cord disease affects people at a higher age, above 55 years.
In war zones or countries with a widespread availability of weapons or a high crime rate, the number of traumatic SCI is high, whereas gunshots or other forms of violence as causes for SCI play only a minor role in countries with restrictive laws on fire arms [20, 21]. The incidence of traumatic SCI in the mentioned countries and regions (Table 1.3) varies between 12 and 53/million [7, 10, 17, 24]. Even if data on the overall incidence are available for a large country, the regional incidence may vary to a large extent due to differences in industrialization and medical infrastructure, e.g., rural areas versus cities.
The incidence of non-traumatic SCI varies between 12 and 76/million population [7, 10, 26–28] (Table 1.4). In western industrial countries, the demographic change toward a dramatic increase in the elderly population has an enormous influence on the etiology of SCI, meaning that the percentage of non-traumatic SCI is constantly growing over the last decade [30].
With regard to gender, men are by far more affected by traumatic SCI [7, 24, 31] (Table 1.5). In case of non-traumatic SCI, the proportion of females is nearly equal to males [12, 29, 35] (Table 1.6). Respective gender proportions are robust and comparable in all countries worldwide.
5 Etiology of Traumatic SCI
The most common global causes for traumatic SCI are road traffic accidents followed by falls and violence. The proportion of road traffic accident-related SCI varies to a great degree for different regions of the world. The number of road traffic accidents is directly related to the population and traffic density but also depends on regionally quite differently developed road safety measures. In Africa, for instance, the proportion of traffic accident-related SCI (57 %) is almost twice as high as in Europe [31, 40], whereas the probability of a fall-related SCI in Europe is nearly twice as high as compared to Africa [31, 35]. A Chinese study shows that rapid progress in industrialization and the associated increase of traffic substantially influence the incidence and causes of traumatic SCI. Between 2000 and 2010, an increase of road traffic accident-related SCI to 51.2 % has been reported [41]. In other developing countries, traffic accidents are by far the most prominent cause of traumatic SCI (77 % in Lagos [42]). With 85 % the highest proportion of traffic accident-related SCI can be found in Saudi Arabia [43].
In children and juveniles, traffic accidents are the most common cause of paralysis worldwide. In the group of children with an age below 12 years, traffic accidents are the most frequent cause of traumatic SCI, higher than all other causes together [18, 19]. In the subpopulation with an age below 45 years, traffic accidents are the most common cause of SCI. However, after the age of 45, falls are the most likely cause for an SCI [20].
However, those numbers need to be seen from the perspective of regionally different populations. As an example, the high percentage of fall-related SCIs in older people in Europe can be easily explained by the demographic population structure in European countries [1]. This development is also found in the USA (“mean age at injury increased 9 years since the 1970s”) [43], in Canada (“significant increase in the mean age at injury from 30.23 to 45.768 years of age”) [44], and in Australia reporting a significantly increasing rate of fall-related injuries in elderly males [45].
People’s recreational and sport-related activities influence both the rate of SCI and the associated patterns of injury. The percentage of sport-related SCI in the overall traumatic SCI population is 1.7 % in Nigeria, 4.0 % in Germany, 10.0 % in the USA, and 14.1 % in the Netherlands [11, 28, 42, 46]. According to the available literature, there are six countries in which sports accounts for over 13 % of SCI (highest to lowest: Russia, Fiji, New Zealand, Iceland, France, and Canada). Diving, skiing, rugby, and horseback riding were identified as individual sports with the highest risk for SCI. For hockey, skiing, diving, and American football, almost all injuries are located at the cervical spinal cord level, while over half of horseback riding and snowboarding injuries are at the thoracic or lumbosacral level [47].
The number of traumatic SCI caused by firearms varies to a large extent in different countries. In Northern Europe the percentage is below 1 % of the overall traumatic SCI population, whereas in Brazil injuries of the spinal cord by the use of firearms are a common cause accounting for 16.9 % of all traumatic SCI cases [48].
As mentioned above the incidence represents, among other things, a good indicator in terms of effectiveness of primary measures for the prevention of SCI. For the validity of this statement, there are both positive and negative examples: in Germany the costs of treatment after accidents during work will be covered by a separate statutory accident insurance (workmen’s compensation). This is somehow a unique approach in the international context. The data from Germany show that the proportion of SCI caused by workplace accidents has decreased from 22 to 7 % of the total traumatic SCI population from 1985 to 2013 [11]. This can be attributed both to the lower risks for workplace-related injuries due to the general trend toward a modern industrial and information society with more indoor work places and also to the implementation of stricter occupational safety regulations. The latter is without doubt an example of successful primary prevention.
However, in another cause of traumatic SCI, diving into shallow water, primary preventive measures seem to be less effective. Data from Germany show that the percentage of cervical lesions resulting from shallow water diving persists on a constant level from 1985 to 2013 [11]. The proportion of SCI related to shallow water diving accounts for approximately 4 % of traumatic SCI. The introduction of several prevention campaigns did not yield a lower incidence. In contrast, prevention programs in the USA and Canada have been reported to successfully promote reduced rates of diving into shallow water accidents [49].
6 Etiology of Non-traumatic SCI
Few studies provide epidemiological data on non-traumatic SCI. Non-traumatic SCI has received more and more attention over the recent decades, whereas until the mid of the twentieth century, the percentage of traumatic SCI was reported to be more than 90 % with only few cases due to non-traumatic causes. The increase of non-traumatic SCI – a disease of the elderly – can, for the most part, be explained by the increase in life expectancy of the population in developed countries. This trend is normally linked to the occurrence of age-related diseases such as cardiovascular disorders, tumors, and infections of the spinal column or spinal cord itself. Developing countries tended to have a higher proportion of infections, particularly tuberculosis and HIV, although a number also reported tumors as a major cause [27].
A detailed analysis of over 1000 cases of non-traumatic SCI in 2012 in Germany attributed 26 % to tumors compressing the spinal cord, 20 % to infectious disease, and 16 % to ischemia. The most common non-traumatic cause (41 %) was degenerative spine diseases with associated spinal canal stenosis [11]. These proportions are comparable for all industrialized countries [26].
Non-traumatic SCI results much more often in incomplete paralysis compared to traumatic SCI [9, 11, 12, 26, 28, 29, 41, 42] (Tables 1.7 and 1.8).
7 Trends, Mortality, and Life Expectancy in SCI
Until the beginning of the twentieth century, an SCI was a devastating condition leading to death due to pneumonia, pressure sores, or lower and upper urinary tract infections within days to months depending on the lesion level and severity. In particular, in high cervical cord lesions very soon after the injury, pneumonia occurred due to the impairment of respiratory function, which in the long run, led to death due to the lack of therapeutic interventions. The progress in the second half of the twentieth century in the development of surgical stabilization options and intensive care medicine as well as a strong desire to not accept the unavoidable fate of SCI victims, resulted in the introduction of dedicated rehabilitative and neurological therapies. These factors promoted a fundamental change in the situation of individuals suffering from the sequels of SCI.
As a consequence, the life expectancy of people with traumatic SCI has continuously increased over the last 70 years [51]. However, compared to the general population, mortality is increased in the SCI population. The life expectancy (LE) of people with SCI is still lower compared to age-matched able-bodied individuals. The highest estimated lost LE was associated with chronic pressure ulcers (50.3 %), followed by amputations (35.4 %), one or more recent hospitalizations (18.5 %), and the diagnosis of probable major depression (18 %). Symptoms of infections were associated with a 6.7 % reduction in LE for an increase in infectious symptoms [52]. For patients with traumatic SCI, the highest mortality risk is during the first year after the date of injury and the onset of SCI [53, 54].
The mortality rate and life expectancy after SCI differ substantially in different parts of the world mainly due to enormous differences in the standard of care. This includes, on the one hand, the availability and effectiveness of emergency units and, on the other hand, the quality of lifelong care [55]. The quality of emergency and primary care and the subsequent medical-rehabilitative therapy affect mortality rates to a great extent. Particularly in low-income countries, many people today still die from complications that could easily be avoided with a higher standard of care.
In addition to the level and severity of the SCI, the presence and extent of concomitant injuries and trauma strongly influence the mortality risk. Age substantially influences the prognosis of survival due to the presence of comorbidities [56].
The mean life expectancy of people with tetraplegia is lower than of persons with paraplegia. A complete SCI results more often in earlier death than an incomplete SCI. This was shown in a number of countries by comparing mortality rates with the general population [53, 57].
Several studies show that in people with paraplegia, the causes of death become similar to those of the general population [53, 58]. Most common causes of death are nowadays ischemic events such as cardiac arrest or stroke, tumors, and chronic obstructive pulmonary disease (COPD). However, approximately 15 % of SCI patients still die because of pressure sores and their medical consequences [58, 59].
The causes of death in people with tetraplegia are very different to those with paraplegia. In the international literature, high numbers of pulmonary complications are found consistently to be a leading cause of death in people with tetraplegia [30, 60–62]. This is obvious and, particularly in case of very high lesions with an extended paralysis, unavoidable to some extent. In any case, patients suffering from very high cervical SCI require permanent mechanical ventilation and form a special group. Unlike any other group, their mortality depends on the availability of medical-technical equipment and nursing care. Therefore, the mortality rate of these very high-lesioned patients may serve as an indicator of how much a society is technically and economically able to provide a high-level of community-based care [63].
Independent from the severity and the level of the lesion, there is evidence that the incidence of suicide as a cause of death is higher in the SCI population than in the general population [64]. This might be related to the fact that a suicide attempt was quite often the cause of the SCI [65].
Other typical paralysis-related causes of death are chronic obstipation related to neurogenic bowel dysfunction and urosepsis as consequences of neurogenic bladder dysfunction. Not infrequently, urothelial carcinoma of the bladder can represent a death-related cause in SCI patients [50].
The notable shift in traumatic SCI toward older patients has a huge impact on rehabilitation approaches, because older people have age-associated comorbidities limiting their rehabilitation potential [46, 66, 67]. This problem will become even further apparent due to the ongoing demographic change in industrial countries. A German population of over 3.000 SCI patients collected over a 25-year period showed that 84 % of the patients suffered from comorbidities such as cardiovascular diseases and tumors, which required additional treatment [11].
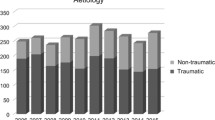
Trends in the growth of the proportion of non-traumatic SCI can be seen in the German database, to which all German SCI centers contribute. In the beginning of data acquisition (1976), the proportion of non-traumatic SCI was 14 %. In 2012, the percentage of non-traumatic SCI was 54 % [11], with an average of 37 % between 1976 and 2012.
8 Costs of SCI
SCI does not only put additional burden on to affected individuals, but it generates substantial costs for health care and professional reintegration. In many instances, the severity of the functional impairments with required lifelong care substantially contributes to this figure. The costs on the social system are very high due to permanent paralysis. Here, one has to differentiate between costs directly related to the injury and the expenses of the treatment of the lifelong consequences of the SCI impairment, which also include financial commitments of social reintegration.
Basically, direct costs in the acute phase after the injury consist of:
-
Expenses resulting from rescue and emergency services in the case of traumatic SCI
-
Costs for inpatient surgical and conservative treatments and care
-
Costs for outpatient care, medication, physical/occupational therapy, assistive devices such as wheelchairs, and consumables such as catheters
Costs related to comprehensive care are mainly generated by:
-
Setup of an accessible home and eventually also a working environment
-
Loss of tax and/or welfare expenses in case professional reintegration is not successful
It is clear that both the severity of the functional impairment and the outcome of the primary medical treatment and the medical and professional rehabilitation have an impact on both direct and indirect costs. The highest costs occur during the first year after injury, whereas the total costs are determined by the life expectancy.
Published data regarding lifetime costs of SCI are inconsistent and often untransparent regarding the method of estimation [1]. The available numbers often seem to be outdated and in any case need to be interpreted with caution. Therefore, no precise numbers are provided within this chapter.
Conclusions
Epidemiological data on incidence, prevalence, and etiology of traumatic and non-traumatic SCI are subject to substantial regional variations. These numbers are influenced by multiple factors, most importantly the level and availability of emergency and life-saving services as well as SCI-specific surgical, rehabilitative, and home care institutions. Trends in the incidence of traumatic SCI over time may serve as an indicator for the success of preventive measures. The increase in life expectancy of the general population in societies with high average income results in an increase of non-traumatic SCI. More population-based studies are needed to obtain more reliable data about SCI epidemiology and trends over time.
References
World Health Organization (WHO) (2013) International perspectives on spinal cord injury. http://apps.who.int/iris/bitstream/10665/94190/1/9789241564663_eng.pdf. Accessed on 07 July 2016
Podnar S (2007) Epidemiology of cauda equina and conus medullaris lesions. Muscle Nerve 35(4):529–531. doi:10.1002/mus.20696
World Health Organization (WHO) (2015) World report on ageing and health. http://www.who.int/ageing/events/world-report-2015-launch/en/. Accessed on 07 July 2016
Rothman KJ (2012) Epidemiology: an introduction, 2nd edn. Oxford University Press, Oxford
Singh A, Tetreault L, Kalsi-Ryan S, Nouri A, Fehlings MG (2014) Global prevalence and incidence of traumatic spinal cord injury. Clin Epidemiol 6:309–331. doi:10.2147/CLEP.S68889
Lee BB, Cripps RA, Fitzharris M, Wing PC (2014) The global map for traumatic spinal cord injury epidemiology: update 2011, global incidence rate. Spinal Cord 52(2):110–116. doi:10.1038/sc.2012.158
Noonan VK, Fingas M, Farry A, Baxter D, Singh A, Fehlings MG, Dvorak MF (2012) Incidence and prevalence of spinal cord injury in Canada: a national perspective. Neuroepidemiology 38(4):219–226. doi:10.1159/000336014
Hagen EM, Eide GE, Rekand T, Gilhus NE, Gronning M (2010) A 50-year follow-up of the incidence of traumatic spinal cord injuries in Western Norway. Spinal Cord 48(4):313–318. doi:10.1038/sc.2009.133
Dahlberg A, Kotila M, Leppanen P, Kautiainen H, Alaranta H (2005) Prevalence of spinal cord injury in Helsinki. Spinal Cord 43(1):47–50. doi:10.1038/sj.sc.3101616
O’Connor PJ (2005) Prevalence of spinal cord injury in Australia. Spinal Cord 43(1):42–46. doi:10.1038/sj.sc.3101666
Thietje R, Kowald B, Hirschfeld S (2011) Woran sterben Querschnittgelähmte heute-eine Nachuntersuchung von 102 Fällen. JournalDie Rehabilitation 50, 251–4
New PW, Farry A, Baxter D, Noonan VK (2013) Prevalence of non-traumatic spinal cord injury in Victoria, Australia. Spinal Cord 51(2):99–102. doi:10.1038/sc.2012.61
Razdan S, Kaul RL, Motta A, Kaul S, Bhatt RK (1994) Prevalence and pattern of major neurological disorders in rural Kashmir (India) in 1986. Neuroepidemiology 13(3):113–119
Jazayeri SB, Ataeepour M, Rabiee H, Motevalian SA, Saadat S, Vaccaro AR, Rahimi-Movaghar V (2015) Prevalence of spinal cord injury in Iran: a 3-Source Capture-Recapture Study. Neuroepidemiology 45(1):28–33. doi:10.1159/000435785
Wyndaele M, Wyndaele JJ (2006) Incidence, prevalence and epidemiology of spinal cord injury: what learns a worldwide literature survey? Spinal Cord 44(9):523–529. doi:10.1038/sj.sc.3101893
Ahoniemi E, Alaranta H, Hokkinen EM, Valtonen K, Kautiainen H (2008) Incidence of traumatic spinal cord injuries in Finland over a 30-year period. Spinal Cord 46(12):781–784. doi:10.1038/sc.2008.53
Albert T, Ravaud JF, Tetrafigap G (2005) Rehabilitation of spinal cord injury in France: a nationwide multicentre study of incidence and regional disparities. Spinal Cord 43(6):357–365. doi:10.1038/sj.sc.3101717
DeVivo MJ, Vogel LC (2004) Epidemiology of spinal cord injury in children and adolescents. J Spinal Cord Med 27(Suppl 1):S4–S10
Vogel LC, Betz RR, Mulcahey MJ (2012) Spinal cord injuries in children and adolescents. Handb Clin Neurol 109:131–148. doi:10.1016/B978-0-444-52137-8.00008-5
McCaughey EJ, Purcell M, McLean AN, Fraser MH, Bewick A, Borotkanics RJ, Allan DB (2016) Changing demographics of spinal cord injury over a 20-year period: a longitudinal population-based study in Scotland. Spinal Cord 54(4):270–276. doi:10.1038/sc.2015.167
Rodriguez-Meza MV, Paredes-Cruz M, Grijalva I, Rojano-Mejia D (2016) Clinical and demographic profile of traumatic spinal cord injury: a mexican hospital-based study. Spinal Cord 54(4):266–269. doi:10.1038/sc.2015.164
New PW, Baxter D, Farry A, Noonan VK (2015) Estimating the incidence and prevalence of traumatic spinal cord injury in Australia. Arch Phys Med Rehabil 96(1):76–83. doi:10.1016/j.apmr.2014.08.013
Koskinen EA, Alen M, Vaarala EM, Rellman J, Kallinen M, Vainionpaa A (2014) Centralized spinal cord injury care in Finland: unveiling the hidden incidence of traumatic injuries. Spinal Cord 52(10):779–784. doi:10.1038/sc.2014.131
van Asbeck FW, Post MW, Pangalila RF (2000) An epidemiological description of spinal cord injuries in The Netherlands in 1994. Spinal Cord 38(7):420–424
Cripps RA, Lee BB, Wing P, Weerts E, Mackay J, Brown D (2011) A global map for traumatic spinal cord injury epidemiology: towards a living data repository for injury prevention. Spinal Cord 49(4):493–501. doi:10.1038/sc.2010.146
Milicevic S, Bukumiric Z, Nikolic AK, Babovic R, Jankovic S (2012) Demographic characteristics and functional outcomes in patients with traumatic and nontraumatic spinal cord injuries. Vojnosanit Pregl 69(12):1061–1066
New PW, Cripps RA, Bonne Lee B (2014) Global maps of non-traumatic spinal cord injury epidemiology: towards a living data repository. Spinal Cord 52(2):97–109. doi:10.1038/sc.2012.165
Nijendijk JH, Post MW, van Asbeck FW (2014) Epidemiology of traumatic spinal cord injuries in The Netherlands in 2010. Spinal Cord 52(4):258–263. doi:10.1038/sc.2013.180
van den Berg ME, Castellote JM, Mahillo-Fernandez I, de Pedro-Cuesta J (2012) Incidence of nontraumatic spinal cord injury: a Spanish cohort study (1972–2008). Arch Phys Med Rehabil 93(2):325–331. doi:10.1016/j.apmr.2011.08.027
NSCISC (2015) The 2015 annual statistical report for the model spinal cord injury care system. National SCI Statistical Center. www.uab.edu/NSCISC. Accessed 07 July 2016
Nwadinigwe CU, Iloabuchi TC, Nwabude IA (2004) Traumatic spinal cord injuries (SCI): a study of 104 cases. Niger J Med 13(2):161–165
Zhou Y, Wang XB, Kan SL, Ning GZ, Li YL, Yang B, Li Y, Sun JC, Feng SQ (2015) Traumatic spinal cord injury in Tianjin, China: a single-center report of 354 cases. Spinal Cord. doi:10.1038/sc.2015.173
Jain NB, Ayers GD, Peterson EN, Harris MB, Morse L, O’Connor KC, Garshick E (2015) Traumatic spinal cord injury in the United States, 1993–2012. JAMA 313(22):2236–2243. doi:10.1001/jama.2015.6250
New PW, Simmonds F, Stevermuer T (2011) A population-based study comparing traumatic spinal cord injury and non-traumatic spinal cord injury using a national rehabilitation database. Spinal Cord 49(3):397–403. doi:10.1038/sc.2010.77
Lenehan B, Street J, Kwon BK, Noonan V, Zhang H, Fisher CG, Dvorak MF (2012) The epidemiology of traumatic spinal cord injury in British Columbia, Canada. Spine (Phila Pa 1976) 37(4):321–329. doi:10.1097/BRS.0b013e31822e5ff8
Hart C, Williams E (1994) Epidemiology of spinal cord injuries: a reflection of changes in South African society. Paraplegia 32(11):709–714. doi:10.1038/sc.1994.115
Ibrahim A, Lee KY, Kanoo LL, Tan CH, Hamid MA, Hamedon NM, Haniff J (2013) Epidemiology of spinal cord injury in Hospital Kuala Lumpur. Spine (Phila Pa 1976) 38(5):419–424. doi:10.1097/BRS.0b013e31826ef594
McKinley WO, Seel RT, Hardman JT (1999) Nontraumatic spinal cord injury: incidence, epidemiology, and functional outcome. Arch Phys Med Rehabil 80(6):619–623
Quintana-Gonzales A, Sotomayor-Espichan R, Martinez-Romero M, Kuroki-Garcia C (2011) Nontraumatic spinal cord injury: etiology, demography and clinics. Rev Peru Med Exp Salud Publica 28(4):633–638
Smith E, Brosnan M, Comiskey C, Synnott K (2014) Road collisions as a cause of traumatic spinal cord injury in Ireland, 2001–2010. Top Spinal Cord Inj Rehabil 20(2):158–165. doi:10.1310/sci2002-147
Hua R, Shi J, Wang X, Yang J, Zheng P, Cheng H, Li M, Dai G, An Y (2013) Analysis of the causes and types of traumatic spinal cord injury based on 561 cases in China from 2001 to 2010. Spinal Cord 51(3):218–221. doi:10.1038/sc.2012.133
Obalum DC, Giwa SO, Adekoya-Cole TO, Enweluzo GO (2009) Profile of spinal injuries in Lagos, Nigeria. Spinal Cord 47(2):134–137. doi:10.1038/sc.2008.93
DeVivo MJ, Chen Y (2011) Trends in new injuries, prevalent cases, and aging with spinal cord injury. Arch Phys Med Rehabil 92(3):332–338. doi:10.1016/j.apmr.2010.08.031
McCammon JR, Ethans K (2011) Spinal cord injury in Manitoba: a provincial epidemiological study. J Spinal Cord Med 34(1):6–10. doi:10.1179/107902610X12923394765733
O’Connor PJ (2006) Trends in spinal cord injury. Accid Anal Prev 38(1):71–77. doi:10.1016/j.aap.2005.03.025
Devivo MJ (2012) Epidemiology of traumatic spinal cord injury: trends and future implications. Spinal Cord 50(5):365–372. doi:10.1038/sc.2011.178
Chan CW, Eng JJ, Tator CH, Krassioukov A, Spinal Cord Injury Research Evidence Team (2016) Epidemiology of sport-related spinal cord injuries: a systematic review. J Spinal Cord Med 39(3):255–264. doi:10.1080/10790268.2016.1138601
Bellucci CH, Castro Filho JE, Gomes CM, Bessa Junior J, Battistella LR, Souza DR, Scazufca M, Bruschini H, Srougi M, Barros Filho TE (2015) Contemporary trends in the epidemiology of traumatic spinal cord injury: changes in age and etiology. Neuroepidemiology 44(2):85–90. doi:10.1159/000371519
Barss P, Djerrari H, Leduc BE, Lepage Y, Dionne CE (2008) Risk factors and prevention for spinal cord injury from diving in swimming pools and natural sites in Quebec, Canada: a 44-year study. Accid Anal Prev 40(2):787–797. doi:10.1016/j.aap.2007.09.017
Alshahri SS, Cripps RA, Lee BB, Al-Jadid MS (2012) Traumatic spinal cord injury in Saudi Arabia: an epidemiological estimate from Riyadh. Spinal Cord 50(12):882–884. doi:10.1038/sc.2012.65
Middleton JW, Dayton A, Walsh J, Rutkowski SB, Leong G, Duong S (2012) Life expectancy after spinal cord injury: a 50-year study. Spinal Cord 50(11):803–811. doi:10.1038/sc.2012.55
Krause JS, Saunders LL (2011) Health, secondary conditions, and life expectancy after spinal cord injury. Arch Phys Med Rehabil 92(11):1770–1775. doi:10.1016/j.apmr.2011.05.024
Ahoniemi E, Pohjolainen T, Kautiainen H (2011) Survival after spinal cord injury in Finland. J Rehabil Med 43(6):481–485. doi:10.2340/16501977-0812
Lidal IB, Snekkevik H, Aamodt G, Hjeltnes N, Biering-Sorensen F, Stanghelle JK (2007) Mortality after spinal cord injury in Norway. J Rehabil Med 39(2):145–151. doi:10.2340/16501977-0017
Nwankwo OE, Uche EO (2013) Epidemiological and treatment profiles of spinal cord injury in southeast Nigeria. Spinal Cord 51(6):448–452. doi:10.1038/sc.2013.10
Seguin P, Godard A, Le Maguet P, Launey Y, Laviolle B, Malledant Y (2012) Impact of age on mortality in patients with acute traumatic spinal cord injury requiring intensive care. Ann Fr Anesth Reanim 31(3):196–202. doi:10.1016/j.annfar.2011.10.019
O’Connor PJ (2005) Survival after spinal cord injury in Australia. Arch Phys Med Rehabil 86(1):37–47
Thietje R, Pouw MH, Schulz AP, Kienast B, Hirschfeld S (2011) Mortality in patients with traumatic spinal cord injury: descriptive analysis of 62 deceased subjects. J Spinal Cord Med 34(5):482–487. doi:10.1179/2045772311Y.0000000022
Rabadi MH, Mayanna SK, Vincent AS (2013) Predictors of mortality in veterans with traumatic spinal cord injury. Spinal Cord 51(10):784–788. doi:10.1038/sc.2013.77
Garshick E, Kelley A, Cohen SA, Garrison A, Tun CG, Gagnon D, Brown R (2005) A prospective assessment of mortality in chronic spinal cord injury. Spinal Cord 43(7):408–416. doi:10.1038/sj.sc.3101729
Hagen EM, Lie SA, Rekand T, Gilhus NE, Gronning M (2010) Mortality after traumatic spinal cord injury: 50 years of follow-up. J Neurol Neurosurg Psychiatry 81(4):368–373. doi:10.1136/jnnp.2009.178798
Krause JS, Saunders LL (2010) Risk of mortality and life expectancy after spinal cord injury: the role of health behaviors and participation. Top Spinal Cord Inj Rehabil 16(2):53–60. doi:10.1310/sci1602-53
Hirschfeld S, Exner G, Luukkaala T, Baer GA (2008) Mechanical ventilation or phrenic nerve stimulation for treatment of spinal cord injury-induced respiratory insufficiency. Spinal Cord 46(11):738–742. doi:10.1038/sc.2008.43
Cao Y, Massaro JF, Krause JS, Chen Y, Devivo MJ (2014) Suicide mortality after spinal cord injury in the United States: injury cohorts analysis. Arch Phys Med Rehabil 95(2):230–235. doi:10.1016/j.apmr.2013.10.007
McCullumsmith CB, Kalpakjian CZ, Richards JS, Forchheimer M, Heinemann AW, Richardson EJ, Wilson CS, Barber J, Temkin N, Bombardier CH, Fann JR, Investigators P (2015) Novel risk factors associated with current suicidal ideation and lifetime suicide attempts in individuals with spinal cord injury. Arch Phys Med Rehabil 96(5):799–808. doi:10.1016/j.apmr.2014.12.017
Chen Y, Tang Y, Allen V, DeVivo MJ (2015) Aging and spinal cord injury: external causes of injury and implications for prevention. Top Spinal Cord Inj Rehabil 21(3):218–226. doi:10.1309/sci2103-21810.1310/sci2103-218
Ragnarsson KT (2012) Medical rehabilitation of people with spinal cord injury during 40 years of academic physiatric practice. Am J Phys Med Rehabil 91(3):231–242. doi:10.1097/PHM.0b013e3182489f5e
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Thietje, R., Hirschfeld, S. (2017). Epidemiology of Spinal Cord Injury. In: Weidner, N., Rupp, R., Tansey, K. (eds) Neurological Aspects of Spinal Cord Injury. Springer, Cham. https://doi.org/10.1007/978-3-319-46293-6_1
Download citation
DOI: https://doi.org/10.1007/978-3-319-46293-6_1
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-46291-2
Online ISBN: 978-3-319-46293-6
eBook Packages: MedicineMedicine (R0)