Abstract
The discovery of lithium has important lessons for psychiatry at several levels: in relation to strategies for drug discovery, in understanding the bipolar phenotype, in how insight into lithium’s mechanism of action and unique pharmacology relates to its positive actions on the one hand and its adverse effects on the other. Lithium’s pharmacology remains of interest, and a lithium mimetic is overdue. All these elements continue to place lithium at the heart of future research in bipolar disorder, just as it has occupied this place in its past. Moreover, findings on neuroprotection may herald new future indications and applications.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
FormalPara Key Points-
Lithium’s efficacy may hold the key to developing new and effective treatments for bipolar disorder.
-
Lithium’s unique mechanisms of action may provide novel insights into the neurobiology of bipolar disorder.
-
Lithium should not be forgotten in future research.
1 Introduction
The discovery of lithium remains one of the most intriguing stories of modern and not so modern medicine. As this volume illustrates, it has important lessons for psychiatry at several levels. This final chapter summarizes snapshots of the key issues for the future.
2 Drug Discovery
Lithium illustrates the phenomenon of serendipity in the discovery of novel treatments. This is important because we face an immediate future where major pharmaceutical companies have, with only a few notable exceptions, withdrawn from research and development in psychiatric disorders. That means that there could well be nothing that is really new for a generation. It reflects a failure of the preceding two decades of brain research to generate the concrete scientific understanding that best underpins applied research in our field.
In the future we will continue to need what I like to call ‘guided serendipity’. In other words, discovery that is fortuitous, but nevertheless guided by approximate hypotheses that are plausible and science led. The unexpected use of ketamine to treat depression is the most recent really interesting example. Ketamine is a drug with an established indication that is being ‘repurposed’, to use the jargon buzzword. There will continue to be innovations in neuroscience, targeted mainly at neurodegeneration. This may be primarily as ‘biologicals’, such as antibodies, aptamers, RNA antagomirs and cell therapy. However, for all we know, these approaches and the development of more familiar types of drug may offer treatments that turn out to work in psychiatric indications. Guided serendipity, having served us well in the past, may yet do so again.
For this to happen, however, we must be free to experiment in the spirit of John Cade. Much modern regulation throttles experiment and hence innovation. It does so by demanding standards of safety or certainty that are impossible, or impossibly expensive, to satisfy. Too often as a Principal Investigator, I have found myself engaged in the pointless exercise of being required to guarantee to prevent from happening something that has never happened before or to collect detailed data on things that we know have happened before and that are bound to happen again, such as adverse effects.
3 The Bipolar Phenotype
Quite apart from the generic regulatory barriers to conducting experimental medicine, bipolar disorder presents a particular additional challenge because it is defined to be an episodic disorder. Studying relatively infrequent severe episodes is very challenging. It means either trials in acutely ill patients or relapse-prevention studies that require years rather than weeks of follow-up. There is thus currently no accepted way to do small-scale, short-term, proof-of-concept studies in bipolar patients, and I would argue considerable pessimism about innovation primarily for this reason. This is not a new situation of course. It partly explains why the risk of developing a drug for a bipolar indication is usually only undertaken by industry for products (e.g. antipsychotics and anticonvulsants) that already have indications.
The episodic view of bipolar disorder often assumes that mood returns to normal between episodes. This clinical view is based on retrospective, and often informal, assessment of mood, which has limited reliability. New methods for prospective intensive mood monitoring are revealing a different and more complex picture, in which chronic mood instability is much more typical of most patients. An emerging hypothesis is that mood instability is a core abnormality of bipolar disorder, underlying persistent functional impairments and creating vulnerability to full episodes of depression or mania. This instability is conceded for patients at risk of relapse, and monitoring mood is recommended as a standard of care in many guidelines. But mood instability as a phenomenon is strangely unexplored and poorly understood. We do not know, for example, what the key bandwidths are over which mood homeostasis is mainly regulated. How does the clinical observation of weekly variations in mood relate to daily, or within day, variations, which also clearly occur? Can such timescales in turn be related to much shorter mechanistic loops amenable to analysis with neurophysiological precision?
A more precise understanding of mood stability would give us a potential target on which to test novel treatments in well-designed, short-term experimental studies. Moreover, mood instability may be of trans-diagnostic significance. It is a relatively common complaint in population studies, beyond the formal diagnoses of bipolar disorder and borderline personality disorder, and is predictive of significant morbidity, including suicide. A major goal of future research must be to define the status of mood instability: as a clinical phenomenon, as a possible emergent property of neural networks expressed by defined genotypes, as a pathophysiological construct and for its therapeutic implications.
4 Lithium’s Mechanism of Action
Lithium has a remarkable efficacy, but continuing safety concerns. It has long been obvious that a lithium mimetic might improve the benefit/harm ratio. A recent suggestion is that an orphan drug approach could work. This is based on the principle that the structure of putative targets for lithium’s action (like inositol monophosphatase) may allow the identification of candidate molecules predicted to interact with the target protein. Ebselen is a drug from the National Institutes of Health Clinical Collection, a chemical library of bioavailable drugs, considered clinically safe but without proven use. It represents a partial lithium mimetic that has the potential, on the one hand, to validate inositol monophosphatase inhibition as a treatment for bipolar disorder and on the other to act as a treatment in itself (Singh et al. 2013).
However, those aspects of lithium’s unique pharmacology that relate to its positive actions, on the one hand, and its adverse effects on the other, are still poorly distinguished. Quite simply, we have a way to go in understanding lithium’s mechanism(s) of action. Studies of human cells offer an emerging way to improve our capacity to understand molecular pathology in functional disorders of the brain. This is being accelerated by the use of pluripotent stem cells. Fibroblasts from patients with known genetic variants can be grown in culture and transformed to different cell types. The properties of these cells may allow us to define the underlying abnormality in bipolar disorder and to understand how, for example, a drug like lithium exerts its unique profile of effect (Haggarty and Perlis 2013). Such assay systems should also allow us to identify novel drug targets and new drugs.
Even if these exciting possibilities are fruitful, the traditional approach to drug development by industry is, unfortunately, widely perceived to be failing. That failure threatens innovation in many disorders. An important solution may come through precompetitive public/private partnership to identify new targets and ligands (Norris et al. 2014). This may be the only way that we will see a lithium replacement in the foreseeable future.
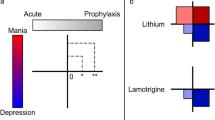
5 Lithium’s Clinical Efficacy
In purely practical terms, we need to refine and improve the use of lithium in defined indications. It remains a first-line choice for bipolar I disorder, but we still need to improve our prospectively collected safety data. So far, it appears that some risks have been either overstated (e.g. the risk of foetal malformation) or over conservatively interpreted (the risk of impaired renal function) (see Chap. 16), although we need to understand better the risks from higher doses of lithium in both cases.
Database studies have yielded another fascinating finding: the possibility that lithium acts to prevent the onset of dementia (Kessing et al. 2010). This possibility needs replication and strengthening. However, it has a possible explanation because lithium inhibits the enzyme glycogen synthase kinase-3β (GSK-3β), which will have putative downstream effects to reduce both tau protein phosphorylation and amyloid-β42 production (Diniz et al. 2013). Additional neuroprotective effects have also been attributed to reduced pro-inflammatory status and decreased oxidative stress. Whether neuroprotection turns out to be yet another unexpected advantage of lithium treatment remains to be seen.
6 Naturalistic Outcomes
Pharmacoepidemiology offers a long-neglected way of using naturalistic data to establish drug efficacy and to investigate societal value. For antipsychotics and mood stabilizers, this has been demonstrated very recently using Swedish databases (Fazel et al. 2014). The outcome was documented violence. This is a good outcome to select for several reasons. Violence is not uncommon in psychiatric populations; it is a proxy for severity of illness and it has obvious clinical and societal relevance. As an outcome, it can be recurrent (e.g. unlike death), which means that patients act as their own controls before, during and after treatment, and observation can be made over long time periods. The reduction in risk with antipsychotics was 50 % and with mood stabilizers 20 %, during active treatment. Lithium had effects that were confined to patients with bipolar diagnoses. So the study demonstrated large effects of treatment with lithium that were specific to the bipolar group. The negative finding in the non-bipolar group is important because mood stabilizers are often used in non-bipolar patients judged to be at risk of violence. This kind of study moves us beyond the artificial world of the randomized clinical trial. We need this kind of innovation and other real-world measures to prove what we see when we treat patients successfully with lithium and other medicines.
7 Summary
When I lecture about lithium, I like to spin a corny introductory line: it is an old drug, 14 billion years old, synthesized 20 min after the Big Bang. It is also old in terms of its discovery (actually rediscovery) for use in modern psychopharmacology. But it has not received the investment in research and development that many less interesting compounds have had. Its use in medicine has also never been driven by effective marketing. Perhaps these are the reasons it seems still able to surprise us. I hope it can continue to do so.
References
Diniz BS, Machado-Vieira R, Forlenza OV (2013) Lithium and neuroprotection: translational evidence and implications for the treatment of neuropsychiatric disorders. Neuropsychiatr Dis Treat 9:493–500
Fazel S, Zetterqvist J, Larsson H, Långström N, Lichtenstein P (2014) Antipsychotics, mood stabilisers, and risk of violent crime. Lancet 384(9949):1206–1214
Haggarty SJ, Perlis RH (2013) Translation: screening for novel therapeutics with disease-relevant cell types derived from human stem cell models. Biol Psychiatry 75(12):952–960
Kessing LV, Forman JL, Andersen PK (2010) Does lithium protect against dementia? Bipolar Disord 12(1):87–94
Norris SMP, Pankevich DE, Davis M, Altevogt BM (2014) Opportunities to improve and accelerate the drug development pipeline http://www.ncbi.nlm.nih.gov/books/NBK195041/
Singh N, Halliday AC, Thomas JM, Kuznetsova OV, Baldwin R, Woon EC, Aley PK, Antoniadou I, Sharo T, Vasudevan SR, Churchill GC (2013) A safe lithium mimetic for bipolar disorder. Nat Commun 4:1332–1339
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Goodwin, G.M. (2017). Lithium in the Twenty-First Century. In: Malhi, G., Masson, M., Bellivier, F. (eds) The Science and Practice of Lithium Therapy. Springer, Cham. https://doi.org/10.1007/978-3-319-45923-3_21
Download citation
DOI: https://doi.org/10.1007/978-3-319-45923-3_21
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-45921-9
Online ISBN: 978-3-319-45923-3
eBook Packages: MedicineMedicine (R0)