Abstract
In performing routine or complex phacoemulsification (i.e., pupil-dilating devices, capsular staining, zonulopathy requiring capsular tension rings/segments with suturing, iris/scleral sutured IOL), the reader is advised to refer to the appropriate chapters in this textbook. One of the challenges during cataract surgery is dealing with the vitreous gel when it presents itself intraoperatively. Given that the scope of vitreous and lens management cannot be covered in any great detail within one single operative template, this chapter focuses on essential surgical steps one needs to take in managing intraoperative complications when the posterior capsule (PC) is violated (Table 23.1). The farther vitreous travels from the vitreal cavity (categories 1–3, Table 23.1), the greater the traction on the vitreous base with increased risk for a retinal tear or detachment (Arbisser et al., Ophthalmol Clin N Am 19:495-506, 2006; Arbisser, Suppl Cataract Refract Surg Today, 2012). The concepts have been simplified to familiarize the reader in dealing with vitreous. A number of references are provided for further in-depth reading to surgically build upon the basic outline provided in this chapter (Arbisser et al., Ophthalmol Clin N Am 19:495-506, 2006; Arbisser, Suppl Cataract Refract Surg Today 2012; Oetting, http://www.eyerounds.org/tutorials/anterior-vitrectomy/index.htm; Kent, Rev Ophthalmol, 2009).
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Posterior capsule (PC)
- Vitreous loss
- Vitreous prolapse
- Bimanual vitrectomy
- Dispersive ophthalmic viscosurgical device (OVD)
- Triesence
- Anterior chamber
- Optic capture
- Sulcus IOL
- ACIOL
Vision-threatening sequelae (See section heading “Complications” below) are not directly result from vitreous loss but due to its inappropriate management. It is important to recognize the potential for complications preoperatively based upon diagnosis and history (Table 23.2). The type and location of intraocular lens implanted and option for optic capture is a function of the integrity of the capsule and zonular status (Table 23.1). It is important to make a watertight wound construction to maintain a stable anterior chamber and PC integrity at all times during surgery (a normotensive globe) [1] in order to minimize zonular stress, iris prolapse, or sudden surge. Signs of PC tear need to be recognized (Table 23.3). If vitreous is suspected, it is paramount not to withdraw the phaco handpiece out of the AC as this will create a drop in IOP to further vitreous prolapse anteriorly and vitreous loss through the path of least resistance via the keratome incision. Through the sideport incision, dispersive OVD should be injected under any lens fragments if present to displace them anterior to the iris plane, and in front of the presumed PC tear. This will displace and compartmentalize the vitreous posteriorly and create a barrier between the vitreal cavity and the lens fragments. Second, barricade the dispersive OVD with a cohesive OVD [1]. This will also serve to pressurize the AC. Only then, should the phaco handpiece be carefully withdrawn. It is prudent not to chase after any lens fragments that have become displaced posterior to the PC with the phaco probe beyond the PC tear , as this can lead to retinal tears [2, 3]. Inform the patient of the possibility of subsequent need for a three-port pars plana vitrectomy and lensectomy by a retina specialist. There should be a backup emergency plan in place for operating room personnel to assist the surgeon in transitioning to set up for vitrectomy in a timely and smooth manner. The essential steps during vitrectomy are to maintain a stable AC and to use biaxial instrumentation [4]. In order to achieve this, abandon and suture the main keratome incision closed and create a new sideport incision < 180° from the original sideport incision that will accommodate the vitrector needle [1].
In biaxial pars plana vitrectomy where the vitrector is introduced via the pars plana and the irrigation cannula is introduced anteriorly via a limbal corneal incision is ideal in removing vitreous from the anterior chamber. This approach enables the prolapsed vitreous to be drawn back into the vitreal cavity posterior to the PC tear and avoids further prolapse into the AC given the resultant lower pressure posteriorly [1]. However since most cataract surgeons do not have the required retinal training to undertake this approach with associated inherent retinal risks (retinal tear or detachment) and lack of familiarity in performing indirect ophthalmoscopy with scleral depression [3], a limbal approach for anterior vitrectomy will be discussed here. Those interested in the pars plana approach are referred to an excellent write-up of this procedure [1, 2].
The goal of vitrectomy is to remove all prolapsed vitreous from the AC back to posterior aspect of the PC. When performing bimanual vitrectomy, one needs to be familiar with the vitrectomy settings and the corresponding foot positions for a given phaco machine. With the infusion line in place, introduce the vitrector in the cut IA setting (cutting precedes aspiration) where vitrectors can cut as high as 5000 cuts per minute [1]. Unlike phacoemulsification where the vitreous can clog the phaco tip during aspiration with risk for tractional retinal detachment (RD), the rapid cut rate, the lowest effective vacuum depending on gauge (150–350) with low flow (around 15–20 cc/min) and the bottle height balanced to provide a normotensive eye [1], prevents such clogging and allows for efficient vitreous lysis and safe removal of the prolapsed vitreous reducing vitreous traction. Irrigation encourages the vitreous to remain posterior by maintaining higher pressure in front of the eye. The vitrector can be entered beyond the PC tear to encourage the vitreous back posteriorly . Care should be taken to focus in the vicinity of the corneal incisions to sever any vitreous strands entrapped within the wounds that may have a posterior connection [2].
Once the vitreous is cleared, any remaining lens fragments or cortex can then be removed in the IA cut mode (aspiration precedes cutting) that enables high suction with a lower cut rate to draw the remaining fragments toward the cutter. Commercially available Triesence (non-preserved triamcinolone) [1] can be used to stain any residual vitreous to facilitate its proper identification and removal once enough OVD is removed which will block adherence of the particles to vitreous. One should avoid sweeping the AC with any instrument such as a cyclodialysis spatula or perform surgical Wek-Cel (Beaver-Visitec, Waltham, MA) vitrectomy [1, 2] as both maneuvers can result in vitreous strands tugging on the retina with risk for RD. Once the vitreous has been amputated from the posterior segment, cellulose sponges can be then used to remove the anterior vitreal fragments via the corneal incisions without fear of traction on the retina [1].
It is important to maintain the AC by leaving the infusion cannula in place, but the infusion must be off (foot position zero), while the cutter is removed to prevent pushing vitreous out the incision on exit and causing incarceration of vitreous in the wound site. The appropriate cohesive OVD should then be placed to prevent collapse of chamber and vitreous representation. In the presence of a posterior continuous curvilinear capsulorrhexis (CCC) , one can place a single-piece IOL into the capsular bag. Alternatively, if the posterior CCC is centered and of a smaller diameter (4–5 mm) than the optic diameter, consider placing a three-piece IOL with optic capture via the posterior CCC into Berger’s space [1].
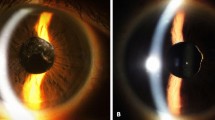
If IOL placement in the bag is not viable, in the presence of an intact anterior CCC, a three-piece sulcus IOL can be introduced with the haptics final resting place within the sulcus and the optic displaced through the anterior capsulorrhexis to achieve optic capture. Optic capture will ensure proper centration and lens stability [1] when conducted either via an anterior or posterior CCC. If the capsulorrhexis is too large or there is presence of an anterior radial tear, one can still place an appropriate three-piece IOL of at least 13 mm length (haptic-optic-haptic) within the sulcus provided there is zonular support 180° apart [1, 2]. As there is no measuring of the sulcus and many haptics lose memory, consideration may be given to placing a single iris suture to prevent late lens subluxation. Single-piece IOLs are inappropriate in the ciliary sulcus and can lead to posterior iris chaffing and pigmentary glaucoma [5]. Finally, if there is significant zonular dialysis , inadequate capsular support, or poor visibility due to corneal edema, placement of an ACIOL is appropriate provided that a surgical iridectomy is conducted to prevent pseudophakic pupillary block. It is also not unreasonable to leave the patient aphakic if it is not safe to place an IOL at the time of surgery and plan for a staged procedure.
Drawback to the anterior approach is that following vitrectomy , the pressure will be lower in the anterior segment encouraging more vitreous prolapse, and any vitreous encouraged forward will enlarge the capsular or zonular tear. Therefore, throughout the procedure and after the posterior capsule is breached, it is paramount to keep the AC pressurized with watertight wound closure to prevent any further vitreous prolapse anteriorly [3]. Injection of acetylcholine not only constricts the pupil in order to identify any residual vitreous strands as noted by peaking of the pupillary sphincter but it also helps to further compartmentalize any residual vitreous within the posterior chamber and vitreal cavity. Given the increased risk for endophthalmitis when the anterior hyaloid is violated, appropriate intracameral and subconjunctival antibiotics should be given, and the patient should be placed on nonsteroidal anti-inflammatory drops for several weeks to prevent cystoid macular edema [3]. Postoperatively, consideration should also be given to refer the patient for a careful retina evaluation to rule out retinal tears or impending RD [3]. Additionally, consider placing patients on ocular hypotensive medications to control IOP spikes that may arise from the presence of residual OVD in the AC and taper appropriately over time.
Indications
-
Vitreous management is something that is surgically unplanned. Those at intraoperative risk for a PC rupture (Table 23.2) should be informed of this potential complication as a part of their informed consent and that appropriate measures will be taken to contain the vitreous with the possible need for additional surgery including pars plana vitrectomy and lensectomy .
Essential Steps
-
The surgeon should have a high degree of suspicion during cataract surgery for signs of a PC tear (Table 23.3 ) and be equipped to deal with the associated intraocular complication (Table 23.1 ). If PC tear is suspected during phacoemulsification or aspiration of cortical material, do the following:
-
1.
Maintain handpiece within the eye in irrigation mode.
-
2.
Inject dispersive OVD via sideport incision to compartmentalize the PC tear and stabilize the AC.
-
3.
Remove handpiece.
-
4.
If PC tear occurs with an intact hyaloid, inject cohesive OVD into Berger’s space through the PC tear. Create a posterior capsulorrhexis [1].
-
5.
If PC tear is accompanied by vitreous prolapse into the AC, compartmentalize the vitreous posteriorly, viscoelevate the lens fragments anterior to the iris plane, and remove with phacoemulsification using a slow-motion technique [6].
-
6.
Inject Triesence (triamcinolone acetonide injectable suspension, Alcon Laboratories Inc., Dallas TX) to stain the vitreous via the sideport incision. (Note: This is only possible once the OVD is removed with initial vitrectomy since OVD will block vitreous identification.)
-
7.
Abandon main keratome incision.
-
8.
Create a new sideport incision <180° away from initial sideport incision to fit the gauge of the vitrector needle.
-
9.
Introduce infusion line and vitrector into the AC for biaxial vitrectomy.
-
10.
Use a high-cut I/A setting with low aspiration and vacuum to lyse and aspirate vitreous keeping the eye normotensive with appropriate bottle height.
-
11.
If vitreous loss is present with peaking of the pupil margin, lyse any vitreous strands from the corneal incisions to sever any extension beyond the PC tear .
-
12.
Use I/A cut setting to remove cortex and residual lens material.
-
13.
Maintain the AC by injecting with a viscocohesive OVD in preparation for IOL implantation.
-
14.
If a posterior CCC is present, place a single-piece IOL into the bag or optic capture it with a three-piece IOL into the CCC.
-
15.
If anterior CCC is present, place a three-piece IOL in the sulcus with optic capture or entirely within the sulcus (if uncaptured consider an iris suture to prevent late subluxation).
-
16.
If significant zonulopathy , inadequate capsular support, or corneal edema is present, place ACIOL and perform a surgical iridectomy.
-
17.
If poor view, consider leaving aphakic at the time of surgery.
-
18.
Use IA cut to aspirate viscoelastic and to cut any residual vitreous strands.
-
19.
Pressurize AC to prevent any further vitreous prolapse making certain all incisions are watertight.
-
20.
Inject intracameral antibiotic of choice for endophthalmitis prophylaxis. Administer IV Diamox (if no sulfa allergy) to prevent post-op IOP spike if residual OVD is present in the AC.
-
1.
Complications
-
Choroidal detachment
-
Corneal edema
-
Cystoid macular edema (CME)
-
Endophthalmitis
-
Intraocular pressure elevation
-
Lens dislocation
-
Dropped lens
-
Retinal detachment
-
Suprachoroidal hemorrhage
-
Retained nuclear or cortical material
-
Zonular dehiscence
Template Operative Dictation
Note: The template has been simplified and does not focus on the use of capsular staining or the use of pupil-dilating devices. Please refer to the appropriate chapters in this book dealing with complex cataract surgery. Three distinct scenarios are presented here to simplify concepts to guide the reader on how to surgically handle intraoperative complications in the setting of a PC tear for each category outlined in Table 23.1 . One should give consideration for converting to an extracapsular cataract extraction if profound zonular dialysis or phacodonesis is present. Complications related to zonulopathy such as suturing of the capsule to the sclera or sutured IOLs will not be addressed here and are covered in accompanying chapters in this textbook. It is beyond the scope of this template to cover all possibilities that may arise in between. The hope is that this will serve as a base by which additional surgical skill sets can be built upon.
Preoperative diagnosis: Mature senile cataract (OD/OS)
Procedure: Cataract extraction (OD/OS) with anterior vitrectomy and placement of (PCIOL [single piece or three piece]/ACIOL) (OD/OS)
Postoperative diagnosis: Complicated cataract extraction with violation of posterior capsule (with vitreous prolapse/loss)
Indication: A (nuclear/cortical/posterior subcapsular) cataract was noted affecting daily activities of living. The patient was motivated to improve vision aiming for (distance/near) correction. The patient was informed of the risks inherent with cataract surgery that include but are not limited to loss of vision, infection, need for additional surgery, vitreous loss, vitreous hemorrhage, retinal detachment, and retinal tear.
Description of the procedure: After discussing risks, benefits, alternatives and obtaining consent, the (right/left) eye was marked with a marking pen in the pre-op holding area, and the appropriate (ASC/hospital based) approved ophthalmic drops to the (right/left) eye were administered for the procedure followed by placement of 2 % lidocaine jelly for topical anesthesia . Following initiation of intravenous sedation, patient was taken to the operating room and placed in a supine position and connected to the monitoring apparatus. The operative eye was prepped and draped in the usual sterile fashion. A proper time-out was performed verifying correct patient, procedure, site, positioning, and special equipment prior to starting the case.
A ___ mm sideport incision was made at ____ clock hours and non-preserved lidocaine was injected followed by a soft-shell technique of a dispersive OVD to coat the endothelium followed by a deeper second layer of cohesive OVD to create space and flatten the anterior capsule. A ____ mm keratome incision was made temporally. A standard anterior capsulorrhexis was conducted, followed by hydrodissection (and hydrodelineation). Sculpting was initiated with the phaco handpiece. A divide and conquer technique was employed to remove the endonucleus.
If the PC ruptured at this stage, with some lens fragments dislocating into the posterior segment, follow template below (otherwise proceed to *)—During this maneuver, a sudden deepening of the AC was noted with some fragments becoming displaced into the posterior segment. At this juncture, the phaco handpiece was maintained within the eye in irrigation mode. Via the sideport incision, a dispersive OVD was injected into the AC in front of the PC tear to compartmentalize and displace the vitreous posteriorly. The remaining fragments were viscoelevated anterior to the iris plane. No attempt was made to phacoemulsify the fragments beyond the PC tear. A slow-motion phaco technique (flow 25 cm 3 /min; vacuum 250 mmHg; short bursts of phaco to facilitate lens followability) [1] was employed to remove the lens fragments within the AC.
The OR personnel were advised to prepare for biaxial anterior vitrectomy, and the patient was informed of the complication and reassured that all measures are being taken to stabilize the eye. The handpiece was carefully removed, and the keratome incision was sutured closed to maintain a closed chamber. A second sideport corneal incision was created (supero/inferotemporal) to the keratome incision approximately _ 180 _ ° from the first sideport incision to accommodate the vitrector needle.
Triesence was injected to bind to the vitreous and provide guidance during vitrectomy whenever OVD was not blocking uptake. The irrigation line and a __ gauge disposable vitrectomy probe were introduced via the respective sideport incisions into the AC. The vitrector needle was advanced into the eye while in foot position 2 (irrigation and cutting). Using cut I/A setting with a high cut rate of ___ cuts per minute, anterior vitrectomy was initiated in cut mode (foot position 3) with the infusion line held anteriorly to maintain a positive pressure and to displace the vitreous posteriorly. The lysed vitreous was removed with a low aspiration rate of ____ cc/min in foot position 3 (irrigation, cutting, and aspiration). This cycle was continued with the vitrector tilted down and advanced through the PC tear to facilitate additional removal of vitreous back posteriorly. The bottle height was adjusted to ___ cm in order to maintain a normotensive state. Once there was no clinical evidence of vitreous prolapse noted, the irrigation cannula was removed holding the vitrector in place while simultaneously keeping foot position zero. Additional Triesence was injected followed by reintroducing irrigation to disperse the Triesence in order to confirm complete removal of prolapsed vitreous from the AC. The AC was always maintained thereafter.
If vitreous strands are extending to the corneal incisions — Using cut I/A mode, the vitrector was used to engage and amputate the vitreous strands entrapped within the corneal wounds from their posterior origin in order to avoid traction on the retina. Care was taken to avoid sweeping the AC with any secondary instruments. As appropriate, the irrigation cannula and vitrector needle lines were interchanged to lyse vitreous strands from the incisions as indicated.
The cortex was removed from the capsular fornix using the I/A cut setting in foot position 2 (aspiration) at _____ cuts per minute and a flow rate of _____ cc/min. If residual vitreous was encountered, foot position 3 was utilized to lyse the residual vitreous.
Prior to removing the (I/A or vitrector) handpiece, a cohesive OVD was injected via the sideport incision into the AC to prevent vitreous prolapse by pressurizing the eye.
(*The cortical/epinuclear material was removed with the I/A handpiece. A PC tear was noted, and a dispersive viscoelastic OVD was injected over the defect followed by gentle injection of a cohesive OVD into Berger’s space to displace and stabilize the anterior hyaloid. An edge of the posterior capsule was grasped with capsulorrhexis forceps, and a CCC was created. Prior to removing the (I/A or vitrector) handpiece, a cohesive OVD was injected via the sideport incision into the AC to prevent vitreous prolapse by pressurizing the eye.)
[Choose one for lens placement and capsular integrity]:
If the posterior capsule was intact — Additional viscoelastic was injected to deepen the capsular bag and a foldable IOL ____ diopters, serial # _____, was injected and centered in the bag. I/A was then conducted to remove the viscoelastic material.
If there was an intact central posterior CCC — Additional viscoelastic was injected to deepen the capsular bag and a three-piece foldable IOL ____ diopters, serial # _____, was injected, and the optic was displaced posteriorly through the posterior CCC into Berger’s space to achieve optic capture. I/A was then conducted to remove the viscoelastic material. Acetylcholine was injected into the AC to constrict the pupil. ( Microscissors were used to lyse the vitreous strands when peaking of the sphincter was noted.)
If there was no viable posterior capsule with an intact anterior CCC— Additional viscoelastic was injected within the ciliary sulcus between the iris plane and the anterior capsule to create a buffer and a foldable three-piece IOL _ diopters, serial # _____, was injected with the leading haptic directed toward the sulcus. The trailing haptic was tucked underneath the iris plane, and the optic was displaced into the capsular bag via the anterior CCC to achieve optic capture. I/A was then conducted to remove the viscoelastic material. Acetylcholine was injected into the AC to constrict the pupil. (Microscissors were used to lyse the vitreous strands when peaking of the sphincter was noted.)
If there was no viable PC and an anterior CCC with a radial tear— Additional viscoelastic was injected within the ciliary sulcus between the iris plane and the anterior capsule to create a buffer, and a foldable three-piece IOL ____ diopters, serial # _____, was injected with the leading haptic directed toward the sulcus . The trailing haptic was tucked underneath the iris plane placing the entire IOL within the sulcus . I/A was then conducted to remove the viscoelastic material. Acetylcholine was injected into the AC to constrict the pupil. (Microscissors were used to lyse the vitreous strands when peaking of the sphincter was noted.)
If there was marked zonulopathy , absence of capsular support or corneal edema obscuring view— Acetylcholine was injected into the AC to constrict the pupil. ( Microscissors were used to lyse the vitreous strands when peaking of the sphincter was noted.) The original keratome incision was then opened by cutting the suture and enlarged appropriately to accommodate a sheets glide and additional viscoelastic. An ACIOL ____ diopters, serial # _____, was introduced along the slide scaffold with the leading haptic secured in the angle. The training haptic was then tucked in the subincision space and adjusted as appropriate for proper placement. I/A was then conducted to remove the viscoelastic material . The keratome incision was re-sutured with a 10-0 nylon mattress suture , and stromal hydration of the corneal wounds ensured a watertight closure.
Appropriate subconjunctival and intracameral antibiotics were administered for endophthalmitis prophylaxis, and IV Diamox 500 mg was given to counter any residual OVD within the AC to prevent post-op IOP spikes. The IOL was found to be centered in position. The pupil was round and the chamber was formed. Eyelid speculum and drape were removed. Maxitrol eye ointment was placed in the inferior fornix, as well as steroid and antibiotic drops, followed by a shield placed over the (right/left) eye. The patient was transferred to the post anesthesia care unit in stable condition.
References
Arbisser LB. When the room gets quiet. Comprehensive strategies for unplanned vitrectomy for the anterior segment surgeon. Suppl Cataract Refract Surg Today. 2012.
Arbisser LB, Charles S, Howcroft M, Werner L. Management of vitreous loss and dropped nucleus during cataract surgery. Ophthalmol Clin N Am. 2006;19:495–506.
Kent C. When the capsule breaks: strategies for success. Rev Ophthalmol. 2009. http://www.reviewofophthalmology.com/content/i/1217/c/22934/dnnprintmode/true/?skinsrc=[l]skins/rp2010/pageprint&containersrc=[l]containers/rp2010/blank .Accessed 3 June 2016.
Oetting T. Anterior vitrectomy. University of Iowa Health Care Ophthalmology and Visual Sciences. http://www.eyerounds.org/tutorials/anterior-vitrectomy/index.htm. Accessed 3 June 2016.
Chang DF, Masket, Miller KM, et al. ASCRS Cataract Clinical Committee. Complications of sulcus placement of single-piece acrylic intraocular lenses: recommendations for backup IOL implantation following posterior capsular rupture. J Cataract Refract Surg. 2009;35(8):1445–58.
Osher RH. Slow motion phacoemulsification approach. J Cataract Refract Surg. 1993;19(5):667.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Shareef, S., Arbisser, L.B. (2017). Cataract Extraction Requiring Vitrectomy due to Violation of the Posterior Capsule with Lens Implantation (Optic Capture, in the Bag, Sulcus, and ACIOL). In: Rosenberg, E., Nattis, A., Nattis, R. (eds) Operative Dictations in Ophthalmology. Springer, Cham. https://doi.org/10.1007/978-3-319-45495-5_23
Download citation
DOI: https://doi.org/10.1007/978-3-319-45495-5_23
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-45494-8
Online ISBN: 978-3-319-45495-5
eBook Packages: MedicineMedicine (R0)