Abstract
In vivo implantation of medical devices, prostheses, biomaterials, and tissue-engineered scaffolds initiates the innate immune response consisting of acute inflammation, chronic inflammation, and the foreign body reaction (FBR) within the first 2 weeks following implantation. This chapter focuses on these humoral and cellular events occurring at the implant site immediately following implantation. Following injury/implantation, blood-material interactions occur and the provisional matrix is formed. Acute inflammation consisting predominantly of polymorphonuclear leukocytes follows but resolves quickly, usually within the first week if not sooner, depending on the extent of injury at the implant site. Chronic inflammation consisting of monocytes, macrophages, and lymphocytes follows acute inflammation. This process also resolves quickly with biocompatible materials leaving monocytes and macrophages to interact at the interface of the implanted device or material. The FBR at the interface with biomaterials is composed of macrophages, which may fuse together to form foreign body giant cells (FBGCs). Outside the FBR at the biomaterial interface, fibrosis and fibrous encapsulation occur in the final stages of the healing response to the implanted biomaterial. Numerous challenges including lack of understanding of these responses in vivo currently limit projection to clinical application of the respective medical device, prosthesis, or biomaterial. The end-stage of the innate immune response consisting of the FBR at the interface with fibrous encapsulation has received extensive attention over the past decade. Numerous efforts have been made to downregulate the activity of macrophages and FBGCs at the interface and to decrease/eliminate the fibrous capsule formation. Ultimately, the success or failure of medical devices, implants, biomaterials, and tissue-engineered constructs is modulated by the interaction between their characteristics, patient conditions, and surgical technique.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Acute inflammation
- Chronic inflammation
- Foreign body reaction
- Innate
- Adaptive
- Immune response
- Matrix formation
2.1 Introduction
Acute inflammation , chronic inflammation , and the foreign body reaction are generally considered to be early events occurring in the innate immune response , e.g., the first 2 weeks following implantation of a biomaterial or medical device. Moreover, the humoral and cellular components and their respective interactions in the innate and acquired immune responses must be appreciated within the context of the in vivo environment. This chapter focuses on the humoral and cellular events occurring at the implant site immediately following implantation. As such, the response to injury may predominate and mask specific interactions occurring at the biomaterial surface/tissue interface as they may relate to or impact the development of acquired immune responses.
The most commonly used term to describe appropriate host response to biomaterials used in a medical device is biocompatibility . A simplistic definition of biocompatibility is those materials, which do not induce an adverse tissue reaction. A more helpful definition of biocompatibility is the ability of a material to perform with an appropriate host response in a specific application [1]. This definition is helpful as it links material properties or characteristics with performance, e.g., biological requirements, with a specific application, a specific medical device, or biomaterial used as a medical device. The “appropriate host response ” implies identification and characterization of tissue reactions and responses that could prove harmful to the host and/or lead to ultimate failure of the biomaterial, medical device, or prosthesis through biological mechanisms. Viewed from the opposite perspective, the “appropriate host response” implies identification and characterization of the tissue reactions and responses critical for the successful use of the biomaterial or medical device. Biocompatibility assessment is considered to be a measure of the magnitude and duration of the adverse alterations in homeostatic mechanisms that determine the host response [2]. Safety assessment or biocompatibility assessment of a biomaterial or medical device is generally considered to be synonymous.
Inflammation, wound-healing, and foreign body reaction are generally considered as parts of the tissue or cellular host responses to injury [3]. Table 2.1 lists the sequence/continuum of these events following injury. Overlap and simultaneous occurrence of these events should be considered; e.g., the foreign body reaction at the implant interface may be initiated with the onset of acute and chronic inflammation . From a biomaterials perspective, placing a biomaterial in the in vivo environment requires injection, insertion, or surgical implantation, all of which injure the tissues or organs involved.
The placement procedure initiates a response to injury by the tissue, organ, or body and mechanisms are activated to maintain homeostasis. Obviously, the extent of injury varies with the implantation procedure. The degrees to which the homeostatic mechanisms are perturbed and the extent to which pathophysiologic conditions are created and undergo resolution are a measure of the host response to the biomaterial and may ultimately determine its biocompatibility . Although it is conceptually convenient to separate homeostatic mechanisms into blood-material or tissue-material interactions, it must be remembered that the various components or mechanisms involved in homeostasis are present in both blood and tissue, are inextricably linked, and are a part of the physiologic continuum. Furthermore, it must be noted that the host response is tissue-dependent, organ-dependent, and species-dependent. The similarities and differences between prostheses utilized between cells, tissues, organs, and species must be appreciated in the design of in vitro and in vivo experiments in the determination of biocompatibility and function.
2.2 Blood-Material Interactions/Provisional Matrix Formation
Immediately following injury, changes in vascular flow, caliber, and permeability occur. Fluid, proteins, and blood cells escape from the vascular system into the injured tissue in a process called exudation . The changes in the vascular system , which also include the hematologic alterations associated with acute inflammation , are followed by cellular events that characterize the inflammatory response.
Blood-material interactions and the inflammatory response are intimately linked, and in fact, early responses to injury involve mainly blood and vasculature. Regardless of the tissue or organ into which a biomaterial is implanted, the initial inflammatory response is activated by injury to vascularized connective tissue (Table 2.2).
Inflammation serves to contain, neutralize, dilute, or wall off the injurious agent or process. In addition, the inflammatory response initiates a series of events that may heal and reconstitute the implant site through replacement of the injured tissue by regeneration of native parenchymal cells, may form fibroblastic scar tissue , or a combination of these two processes. Since blood and its components are involved in the initial inflammatory responses, blood clot formation and/or thrombosis also occur. Blood coagulation and thrombosis are generally considered humoral responses and are influenced by homeostatic mechanisms such as the extrinsic and intrinsic coagulation systems, the complement system , the fibrinolytic system, the kinin-generating system, and platelets. Thrombus or blood clot formation on the surface of a biomaterial is related to the well-known Vroman effect , in which a hierarchical and dynamic series of collision, adsorption, and exchange processes, determined by protein mobility and concentration, regulate early time-dependent changes in blood protein adsorption. From a wound-healing perspective, blood protein deposition on a biomaterial surface in tissue is described as provisional matrix formation . Blood interactions with biomaterials are generally considered under the category of hematocompatibility.
Injury to vascularized tissue in the implantation procedure leads to immediate development of the provisional matrix at the implant site. This provisional matrix consists of fibrin and inflammatory mediators, produced by activation of the coagulation and thrombosis and complement systems, respectively, activated platelets, inflammatory cells, and endothelial cells. These events occur early, within minutes to hours following implantation of a medical device and initiate the resolution, reorganization, and repair processes such as fibroblast recruitment. The provisional matrix provides both structural and biochemical components to the process of wound healing. The complex three-dimensional structure of the fibrin network with attached adhesive proteins provides a substrate for cell adhesion and migration. The presence of cytokines, chemokines, and growth factors within the provisional matrix provides a rich milieu of activating and inhibiting substances for cellular proliferative and synthetic processes, mitogenesis, and chemoattraction. The provisional matrix may be viewed as a naturally derived, biodegradable, sustained release system in which these various bioactive molecules are released to orchestrate subsequent wound-healing processes. Although our understanding of the provisional matrix and its capabilities has increased, our knowledge of the key molecular regulators of the formation of the provisional matrix and subsequent wound-healing events is poor. In part, this lack of knowledge is because most studies have been conducted in vitro, and there is a paucity of in vivo studies that provide for a more complex perspective. However, attractive hypotheses have been presented regarding the presumed ability of adsorbed materials to modulate cellular behavior.
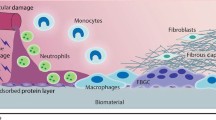
The predominant cell type present in the inflammatory response varies with time (Fig. 2.1). In general, neutrophils predominate during the first several days following injury and exposure to a biomaterial , and then are replaced by monocytes as the predominant cell type. Three factors account for this change in cell type: neutrophils are short lived and disintegrate and disappear after 24–48 h; neutrophil emigration from the vasculature to the tissues is of short duration; and chemotactic factors for neutrophil migration are activated early in the inflammatory response. Following emigration from the vasculature, monocytes differentiate into macrophages and these cells are very long-lived (up to months). Monocyte emigration may continue for day to weeks, depending on the extent of injury and type of implanted biomaterial. In addition, chemotactic factors for monocytes are produced over longer periods of time. In short-term (24 h) implants in humans, administration of both H1 and H2 histamine receptor antagonists greatly reduced the recruitment of macrophages/monocytes and neutrophils on polyethylene terephthalate surfaces [4]. These studies also demonstrated that plasma-coated implants accumulated significantly more phagocytes than did serum-coated implants.
The temporal variation in the acute inflammatory response, chronic inflammatory response, granulation tissue development, and foreign-body reaction to implanted biomaterials . The intensity and time variables are dependent upon the extent of injury created in the implantation and the size, shape, topography, and chemical and physical properties of the biomaterial
The temporal sequence of events following implantation of a biomaterial is illustrated in Fig. 2.2. The size, shape, and chemical and physical properties of the biomaterial may be responsible for variations in the intensity and duration of the inflammatory or wound-healing process, and thus the host response to a biomaterial.
2.3 Acute Inflammation
While injury initiates the inflammatory response , the chemicals released from plasma, cells, or injured tissues mediate the inflammatory response. Important chemical mediators of inflammation are presented in Table 2.3.
Several points must be noted to understand the inflammatory response and its relationship to biomaterials . First, although chemical mediators are classified on a structural or functional basis, complex interactions provide a system of checks and balances regarding their respective activities and functions. Second, chemical mediators are quickly inactivated or destroyed, suggesting that their action is predominantly local (e.g., at the implant site). Third, generally the lysosomal proteases and the oxygen-derived free radicals produce the most significant damage or injury . These chemical mediators are also important in the degradation of certain biomaterials [5–8].
Acute inflammation is of relatively short duration, lasting for minutes to hours to days, depending on the extent of injury and the type of implanted biomaterial . Its main characteristics are the exudation of fluid and plasma proteins (edema) and the emigration of leukocytes (predominantly neutrophils). Neutrophils (polymorphonuclear leukocytes, PMNs) and other motile white cells emigrate or move from the blood vessels into the perivascular tissues and the injury (implant) site. Leukocyte emigration is assisted by “adhesion molecules” present on leukocyte and endothelial surfaces. The surface expression of these adhesion molecules can be induced, enhanced, or altered by inflammatory agents and chemical mediators. White cell emigration is controlled, in part, by chemotaxis, which is the unidirectional migration of cells along a chemical gradient. A wide variety of exogenous and endogenous substances have been identified as chemotactic stimuli. Specific receptors for chemotactic agents on the cell membranes of leukocytes are important in the emigration or movement of leukocytes. These and other receptors also play a role in the transmigration of white cells across the endothelial lining of vessels and activation of leukocytes. Following localization of leukocytes at the injury (implant) site, phagocytosis and the release of proteolytic enzymes occur following activation of neutrophils and macrophages. The major role of the neutrophil in acute inflammation is to phagocytose microorganisms and foreign materials. Phagocytosis is seen as a three-step process in which the stimulus (e.g., damaged tissue, infectious agent, biomaterial) undergoes recognition and neutrophil attachment, engulfment, and killing or degradation. In regard to biomaterials , engulfment and degradation may or may not occur, depending on the properties of the biomaterial.
Although biomaterials are not generally phagocytosed by neutrophils or macrophages because of the disparity in size (e.g., the surface of the biomaterial is greater than the size of the cell), certain events in phagocytosis may occur. The process of recognition and attachment is expedited when the injurious agent is coated by naturally occurring serum factors called “opsonins.” Two major opsonins are immunoglobulin G (IgG) and the complement-activated fragment , C3b. Both of these plasma-derived proteins are known to adsorb biomaterials, and neutrophils and macrophages have corresponding cell-membrane receptors for these opsonins. These receptors may also play a role in the activation of the attached neutrophil or macrophage. Other blood proteins such as fibrinogen, fibronectin , and vitronectin may also facilitate cell adhesion to biomaterial surfaces. Owing to the disparity in size between the biomaterial surface and the attached cell, frustrated phagocytosis may occur; a process that does not involve engulfment of the biomaterial but does cause the extracellular release of leukocyte products in an attempt to degrade the biomaterial.
Henson has shown that neutrophils adherent to complement-coated and immunoglobulin-coated nonphagocytosable surfaces may release enzymes by direct extrusion or exocytosis from the cell [9]. The amount of enzyme released during this process depends on the size of the polymer particle, with larger particles inducing greater amounts of enzyme release. This disparity suggests that the specific mode of cell activation depends, at least in part, upon the size of the implant and whether or not a material is in a phagocytosable form. For example, a powder, particulate, or nanomaterial may provoke a different degree of inflammatory response than the same material in a nonphagocytosable form such as film. In general, materials greater than 5 μm are not phagocytosed, while materials less than 5 μm can be phagocytosed by inflammatory cells, i.e., nanoparticles.
Acute inflammation normally resolves quickly, usually less than 1 week, depending on the extent of injury at the implant site. The presence of acute inflammation (i.e., PMNs) at the tissue/implant interface at time periods beyond 1 week (i.e., weeks, months, or years) suggests the presence of infection.
2.4 Chronic Inflammation
Chronic inflammation has a more heterogeneous histologic appearance than acute inflammation. In general, chronic inflammation is characterized by the presence of macrophages, monocytes , and lymphocytes , with the proliferation of blood vessels and connective tissue . Many factors can modify the course and histologic appearance of chronic inflammation.
Clinically, surgical pathologists commonly use the term chronic inflammation to describe the foreign body reaction . Caution is recommended in the use of this term as it demonstrates the breadth of histological findings that lead to the clinical diagnosis of chronic inflammation. Chronic inflammation that is predominantly composed of monocytes , macrophages , and lymphocytes is most commonly associated with toxicity or infection, whereas the foreign body reaction is most commonly composed of macrophages and foreign body giant cells.
Persistent inflammatory stimuli lead to chronic inflammation. While the chemical and physical properties of the biomaterial in themselves may lead to chronic inflammation, in situ motion of the implant or infection may also produce chronic inflammation. The chronic inflammatory response to biomaterials is usually of short duration and is confined to the implant site. The presence of mononuclear cells, including lymphocytes and plasma cells , is considered chronic inflammation , whereas the foreign-body reaction with the development of granulation tissue is considered the normal wound-healing response to implanted biomaterials (i.e., the normal foreign-body reaction). Chronic inflammation with the presence of collections of lymphocytes and monocytes at extended implant times (weeks, months, years) also may suggest the presence of a long-standing infection. The prolonged presence of acute and/or chronic inflammation also may be due to toxic leachables from a biomaterial [10].
The following example illustrates this point. In vivo subcutaneous implantation studies were conducted in rats and rabbits with naltrexone sustained release preparations that included placebo (polymer only) beads and naltrexone containing beads [11]. Histopathological tissue reactions were determined at days 3, 7, 14, 21, and 28. The only significant histological finding in both rats and rabbits at any time period was the persistent chronic inflammation that occurred focally around the naltrexone containing beads. The focal inflammatory cell density in both rats and rabbits was higher for the naltrexone beads than for the placebo beads at days 14, 21, and 28, respectively. This difference in inflammatory response between naltrexone beads and placebo beads increased with increasing time of implantation . Considering the resolution of the inflammatory response for the placebo beads with implantation time in both rats and rabbits, the more severe inflammatory reaction suggested that the naltrexone drug itself was the causative agent of the focal chronic inflammation present surrounding the naltrexone beads in the implant sites.
The important lesson from this case study is the necessary use of appropriate control materials. If no negative control, i.e., placebo polymer-only material, had been used, the polymer in the naltrexone containing beads also would have been considered a causative agent of the extended chronic inflammatory response. Similar chronic inflammatory responses have been identified with drugs, polymer plasticizers and other additives, fabrication and manufacturing aids, and sterilization residuals. Each case presents its own unique factors in a risk assessment process necessary for determining safety (biocompatibility) and benefit versus risk in clinical application.
Lymphocytes and plasma cells are involved principally in adaptive immune reactions and are key mediators of antibody production and delayed hypersensitivity responses. Although these cells may be present in nonimmunologic injuries and inflammation with biomaterials, their roles in such circumstances are largely unknown [12, 13]. Little is known regarding humoral (or adaptive) immune responses and cell-mediated immunity to synthetic biomaterials. The role of macrophages (cells of the innate humoral response ) must be considered in the possible development of adaptive immune responses to synthetic biomaterials. Macrophages and dendritic cells process and present the antigen to immunocompetent cells and thus are key mediators in the development of adaptive immune reactions.
Monocytes and macrophages belong to the mononuclear phagocytic system (MPS) , also known as the reticuloendothelial system (RES) . These systems consist of cells in the bone marrow, peripheral blood, and specialized tissues. Table 2.4 lists the tissues that contain cells belonging to the MPS or RES .
The specialized cells in these tissues may be responsible for systemic effects in organs or tissues secondary to the release of components or products from implants through various tissue–material interactions (e.g., corrosion products, wear debris, degradation products) or the presence of implants (e.g., microcapsule or nanoparticle drug-delivery systems).
Over the past decade, increasing numbers of studies have identified significant differences in macrophage phenotypic expression. This difference in macrophage function or activation, dictated by different environmental cues, has been classified into various ways. Following on the T-cell literature, macrophages have been classified as M1 macrophages defined as classically activated or pro-inflammatory macrophages and M2 macrophages described as alternatively activated macrophages or anti-inflammatory/pro-wound-healing macrophages [14–16]. Others have attempted to identify three different macrophage classifications: classically activated macrophages, wound-healing macrophages, and regulatory macrophages [17]. In this classification, it is the regulatory macrophage that has anti-inflammatory activity whereas the wound-healing macrophage facilitates tissue repair. Attempts to classify macrophage activity are artificial and can be misleading given the wide variety of environmental cues that may activate macrophages and result in a wide variety of different forms of macrophage polarization, e.g., phenotypic expression. Mantovani best describes macrophage polarization, activity, or phenotypic expression as being a continuum ranging from M1 to M2 [18, 19].
The macrophage is probably the most important cell in chronic inflammation because of the great number of biologically active products it can produce. Important classes of products produced and secreted by macrophages include neutral proteases, chemotactic factors, arachidonic acid metabolites, reactive oxygen metabolites, complement components, coagulation factors, growth-promoting factors, cytokines, and acid. Phagolysosomes in macrophages can have acidity as low as pH of 4 and direct microelectrode studies of this acid environment have determined pH levels as low as 3.5. Moreover, only several hours are necessary to achieve these acid levels following adhesion of macrophages [20–23].
Growth factors such as platelet-derived growth factor (PDGF), fibroblast growth factor (FGF), transforming growth factor-β (TGF-β), TGF-α/epidermal growth factor (EGF), and interleukin-1 (IL-1) or tumor necrosis factor (TNF-α) are important to the growth of fibroblasts and blood vessels and the regeneration of epithelial cells. Effector molecules released by activated macrophages can initiate cell migration, differentiation, and tissue remodeling; and are involved in various stages of wound healing .
2.5 Granulation Tissue
Within 1 day following implantation of a biomaterial (e.g., injury), the healing response is initiated by the action of monocytes and macrophages . Fibroblasts and vascular endothelial cells in the implant site proliferate and begin to form granulation tissue, which is the specialized type of tissue that is the hallmark of healing inflammation. Granulation tissue derives its name from the pink, soft granular appearance on the surface of healing wounds, and its characteristic histologic features include the proliferation of new small blood vessels and fibroblasts. Depending on the extent of injury, granulation tissue may be seen as early as 3–5 days following implantation of a biomaterial.
The new small blood vessels are formed by budding or sprouting of preexisting vessels in a process known as neovascularization or angiogenesis [24, 25]. This process involves proliferation, maturation, and organization of endothelial cells into capillary vessels. Fibroblasts also proliferate in developing granulation tissue and are active in synthesizing collagen and proteoglycans . In the early stages of granulation tissue development, proteoglycans predominate but later collagen , especially type III collagen, predominates and forms the fibrous capsule seen with most biomaterials. Some fibroblasts in developing granulation tissue may have the features of smooth muscle cells, e.g., actin microfilaments. These cells are called myofibroblasts and are considered to be responsible for the wound contraction seen during the development of granulation tissue. In addition to contraction, myofibroblasts can invade and repair injured tissues by secreting an organizing extracellular matrix [26]. Recent studies indicate that myofibroblasts can originate from different precursor cells, the major contribution being from local recruitment of connective tissue fibroblasts ; however, local mesenchymal stem cells, bone marrow-derived mesenchymal stem cells (fibrocytes), and cells derived from the epithelial-mesenchymal transition process may be an alternative source of myofibroblasts [27]. Macrophages are almost always present in granulation tissue. Other cells may also be present if chemotactic stimuli are generated.
The wound-healing response is generally dependent on the extent or degree of injury or defect created by the implantation procedure [28–31]. Wound healing by primary union or first intention is the healing of clean, surgical incisions in which the wound edges have been approximated by surgical sutures. This term does not apply in the context of host response to biomaterials. Healing under these conditions occurs without significant bacterial contamination and with a minimal loss of tissue. Wound healing by secondary union or second intention occurs when there is a large tissue defect that must be filled or there is extensive loss of cells and tissue. In wound healing by secondary intention, regeneration of parenchymal cells cannot completely reconstitute the original architecture and much larger amounts of granulation tissue are formed that result in larger areas of fibrosis or scar formation. Under these conditions, different regions of tissue may show different stages of the wound-healing process simultaneously. Wound healing by second intention is commonly seen with biomaterials and is related to the extent of provisional matrix formed between the implant and tissue.
Granulation tissue is distinctly different from granulomas, which are small collections of modified macrophages called epithelioid cells . Langhans’ or foreign-body-type giant cells may surround nonphagocytosable particulate materials in granulomas. Foreign-body giant cells are formed by the fusion of monocytes and macrophages in an attempt to phagocytose the material .
2.6 Foreign-Body Reaction
The FBR to biomaterials is composed of foreign-body giant cells (FBGCs) and the components of granulation tissue (e.g., macrophages, fibroblasts, and capillaries in varying amounts), depending upon the form and topography of the implanted material [2, 32, 33]. Relatively flat and smooth surfaces such as that found on silicone breast prostheses have a foreign-body reaction that is composed of a layer of macrophages and foreign body giant cells one to two cells in thickness. Relatively rough surfaces such as those found on the outer surfaces of expanded poly tetrafluoroethylene (ePTFE) or Dacron vascular prostheses have a foreign-body reaction composed of macrophages and foreign-body giant cells at the surface. Fabric materials generally have a surface response composed of macrophages and foreign body giant cells, with varying degrees of granulation tissue subjacent to the surface response.
As previously discussed, the form and topography of the surface of the biomaterial determine the composition of the foreign-body reaction [34]. With biocompatible materials, the composition of the foreign-body reaction in the implant site may be controlled by the surface properties of the biomaterial, the form of the implant, and the relationship between the surface area of the biomaterial and the volume of the implant. For example, high-surface-to-volume implants such as fabrics, porous materials, particulate, or microspheres will have higher ratios of macrophages and foreign-body giant cells in the implant site than smooth-surface implants, which will have fibrosis as a significant component of the implant site [35, 36].
The FBR may persist at the tissue–implant interface for the lifetime of the implant. Generally, fibrosis (i.e., fibrous encapsulation) surrounds the biomaterial or implant with its interfacial foreign-body reaction, isolating the implant and foreign-body reaction from the local tissue environment. Early in the inflammatory and wound-healing response, the macrophages are activated upon adherence to the material surface [37].
Although it is generally considered that the chemical and physical properties of the biomaterial are responsible for macrophage activation, the subsequent events regarding the activity of macrophages at the surface are not clear. Tissue macrophages , derived from circulating blood monocytes , may coalesce to form multinucleated foreign-body giant cells . It is not uncommon to see very large foreign-body giant cells containing large numbers of nuclei on the surface of biomaterials. While these foreign-body giant cells may persist for the lifetime of the implant, it is not known if they remain activated, releasing their lysosomal constituents, or become quiescent [38].
Figure 2.2 demonstrates the progression from circulating blood monocyte to tissue macrophage to foreign-body giant cell development that is most commonly observed. Indicated in the figure are important biological responses that are considered to play an important role in FBGC development. Material surface chemistry may control adherent macrophage apoptosis (i.e., programmed cell death) that renders potentially harmful macrophages nonfunctional, while the surrounding environment of the implant remains unaffected. The level of adherent macrophage apoptosis appears to be inversely related to the surface’s ability to promote fusion of macrophages into FBGCs, suggesting a mechanism for macrophages to escape apoptosis. Figure 2.3 demonstrates the sequence of events involved in inflammation and wound healing when medical devices (i.e., biomaterials) are implanted. In general, the PMN predominant acute inflammatory response and the lymphocyte/monocyte predominant chronic inflammatory response resolve quickly (i.e., within 2 weeks) depending on the type and location of the implant. Studies using IL-4 or IL-13, respectively, demonstrate the role for Th2 helper lymphocytes and/or mast cells in the development of the foreign body reaction at the tissue/material interface [39, 40]. Integrin receptors of IL-4-induced FBGCs are characterized by the early constitutive expression of αVβ1 and the later induced expression of α5β1 and αXβ2, which indicate potential interactions with adsorbed complement C3, fibrin(ogen), fibronectin , Factor X, and vitronectin [39–47]. Interactions through indirect (paracrine) cytokine and chemokine signaling have shown a significant effect in enhancing adherent macrophage/FBGC activation at early times, whereas interactions via direct (juxtacrine) cell-cell mechanisms dominate at later times [48–51]. Th2 helper lymphocytes have been described as “anti-inflammatory” based on their cytokine profile, of which IL-4 is a significant component.
Sequence of events involved in inflammatory and wound-healing responses leading to foreign body giant cell formation. This shows the potential importance of mast cells in the acute inflammatory phase and Th2 lymphocytes in the transient chronic inflammatory phase with the production of IL-4 and IL-13, which can induce monocytes/macrophage fusion to form foreign body giant cells
There is a common belief that mononuclear leukocytes , i.e., monocytes and macrophages, can proliferate in the healing response . However, this belief is based on rodent study observations and may not hold for human mononuclear leukocytes in the foreign body reaction to biomaterials [52–54]. No convincing evidence supporting the proliferation of mononuclear leukocytes and macrophages at implant sites in humans has been provided in the literature. This issue of mononuclear leukocyte replication addresses the significant issue of understanding species differences in considering the innate immune response to implanted biomaterials.
In vitro cell culture studies may play a role in determining the interactions of the various cell types involved in the innate immune response with candidate biomaterials for medical devices. However, several key issues must be addressed in the experimental design of these in vitro cell culture studies. Macrophage cell cultures are commonly used to determine the cytotoxicity as well as the capability for foreign body giant cell formation. Unfortunately, the vast majority of macrophage cell cultures utilize tumor-derived macrophage cell lines and rarely are the similarities and differences between these rodent tumor-derived macrophage cell lines compared to primary human blood-derived monocytes presented or discussed. Marked differences in phenotypic expression may be expected when rodent tumor-derived macrophage cell lines are used when compared to primary human monocyte/macrophage cell cultures. Table 2.5 presents a list of commonly utilized tumor-derived macrophage cell lines.
2.7 Fibrosis/Fibrous Encapsulation
The end-stage healing response to biomaterials is generally fibrosis or fibrous encapsulation. However, there may be exceptions to this general statement (e.g., porous materials inoculated with parenchymal cells or porous materials implanted into tissue or bone). As previously stated, the tissue response to biomaterials is in part dependent upon the extent of injury or defect created in the implantation procedure and the amount of provisional matrix.
The ultimate goal of tissue engineering and regenerative medicine is replacement of injured tissue by cells that reconstitute normal tissue and organ structures. Numerous approaches, including stem cells, scaffolds, growth factors, etc., are currently being investigated. However, the relatively rapid responses of inflammation, wound healing, and the foreign body reaction , as well as other significant factors in tissue regeneration, present major challenges to the successful achievement of this goal. This is especially significant with the use of scaffold materials where migration and integration of the scaffold porosity is necessary in tissue engineering approaches.
Repair of biomaterial implant sites can involve two distinct processes: constructive remodeling , which is the replacement of injured tissue by parenchymal cells of the same type, or replacement by connective tissue that constitutes the fibrous capsule. These processes are generally controlled by either (1) the proliferative capacity of the cells in the tissue or organ receiving the implant and the extent of injury as it relates to the destruction, or (2) persistence of the tissue framework (i.e., extracellular matrix) of the implant site.
The regenerative capacity of cells allows them to be classified into three groups: labile, stable (or expanding), and permanent (or static) cells. Labile cells continue to proliferate throughout life; stable cells retain this capacity but do not continuously replicate; and permanent cells cannot reproduce themselves after birth. Perfect repair with restitution of normal structure can theoretically occur only in tissues consisting of stable and labile cells, whereas all injuries to tissues composed of permanent cells may give rise to fibrosis and fibrous capsule formation with very little restitution of the normal tissue or organ structure. Tissues composed of permanent cells (e.g., nerve cells and cardiac muscle cells) most commonly undergo an organization of the inflammatory exudate, leading to fibrosis. Tissues of stable cells (e.g., parenchymal cells of the liver, kidney, and pancreas); mesenchymal cells (e.g., fibroblasts, smooth muscle cells, osteoblasts, and chondroblasts); and vascular endothelial and labile cells (e.g., epithelial cells and lymphoid and hematopoietic cells) may also follow this pathway to fibrosis or may undergo resolution of the inflammatory exudate , leading to restitution of the normal tissue structure.
The condition of the underlying framework or supporting extracellular matrix (ECM) of the parenchymal cells following an injury plays an important role in the restoration of normal tissue structure. Retention of the framework ECM with injury may lead to restitution of the normal tissue structure, whereas destruction of the framework most commonly leads to fibrosis.
It is important to consider the species-dependent nature of the regenerative capacity of cells. For example, cells from the same organ or tissue but from different species may exhibit different regenerative capacities and/or connective tissue repair, as in endothelialization with vascular grafts and stents.
Local and systemic factors play a role in the wound-healing response to biomaterials or implants. Local factors include the anatomic site (tissue or organ) of implantation, the adequacy of blood supply, and the potential for infection. Systemic factors include nutrition, hematologic derangements, glucocorticoid administration, and preexisting diseases such as atherosclerosis, diabetes, and infection.
The end stage of wound healing/tissue repair with implanted medical devices is the fibrous capsule. Initially believed to be produced by infiltrating fibroblasts , it is now known that myofibroblasts and fibrocytes (resident and circulating mesenchymal progenitor cells) play a significant role in producing collagenous fibrosis, the main constituent of the fibrous capsule [55–59].
Finally, the implantation of biomaterials or medical devices may be best viewed from the perspective that the implant provides an impediment or hindrance to appropriate (normal) tissue or organ regeneration and healing. The fibrous capsule surrounding drug delivery devices also has been suggested to be a barrier to drug diffusion and inhibition of the function of drug delivery systems and biosensors (e.g., glucose sensors). However, that view may be short-sighted as recent studies with a wireless controlled drug delivery microchip for the delivery of an osteoporosis inhibitor of approximately 4000 molecular weight have been shown to produce clinically relevant blood levels for inhibition of osteoporosis [60]. Given our current limited ability to control the sequence of events following injury in the implantation procedure, restitution of normal tissue structures with function is rare.
The development of a fibrous capsule surrounding or encapsulating a biomaterial, i.e., scaffold, or medical device, i.e., pacemaker generator, has been commonly viewed as a rejection phenomenon in the end-stage healing of implanted biomaterials or medical devices. This perspective is medical device dependent and the formation of a fibrous capsule may be a positive or negative response. It is not necessarily a rejection phenomenon. Numerous biomaterials and medical devices require the development of an encapsulating fibrous capsule to stabilize the biomaterial or medical device within the tissue. Stabilization of devices within tissue markedly reduces motion of the implant relative to the tissue and has been shown to reduce the chronic inflammatory response produced by such motion when inadequate fibrous capsules have formed surrounding implanted biomaterials or medical devices. Inadequate fibrous capsule formation may lead to migration of a medical device and thus may be a failure mechanism. A classic example of migration as a failure mechanism has been observed with breast implants. Thus, the formation of a fibrous capsule is an important consideration in the design criteria of implanted biomaterials and medical devices.
Current studies directed toward developing a better understanding of the modification of the inflammatory response, stimuli providing for appropriate proliferation of permanent and stable cells, and the appropriate application of growth factors may provide keys to the control of inflammation , wound healing, and fibrous encapsulation of biomaterials.
2.8 Discussion and Perspectives
In spite of the significant advances that have been made in mechanistic understanding of the inflammatory, healing, and foreign body responses to biomaterials and medical devices over the past two decades, numerous challenges, lack of understanding which limit projection to clinical application still exist. The purpose of this discussion/perspectives section is to identify several of these problems that offer challenges/opportunities for the future.
Species differences in the various responses to the implantation of a biomaterial or medical device still exist. The translation from animals to humans is still poorly understood but significant considering that animal studies are a required precursor to clinical application. Current thought regarding the source of macrophages and their fused entity, i.e., foreign body giant cells , suggests that differentiated macrophages may be present due to self-renewal [52]. That is, resident macrophages are capable of proliferation. Studies that support this hypothesis have been conducted in nonhuman mammals and many major macrophage populations have been found to be derived from embryonic progenitors and are capable of renewal independent of hematopoietic stem cells. From a clinical applications perspective, this is a significant question as implant retrieval studies have identified macrophages and foreign body giant cells in the foreign body response to biomaterials and medical devices to be present at the tissue/material interface for approximately 30 years. As there is no compelling evidence that the macrophages in the foreign body reaction to biomaterials and medical devices implanted in humans are capable of self-renewal, i.e., proliferation, the turnover rate of these cells at the interface and the precursor cells that continue to populate the surface of the biomaterial or medical device with implants in humans [52, 61] remain unanswered questions. An example of significant species differences is the fact that human vascular grafts do not endothelialize their luminal surface, whereas higher vertebrates, including chimpanzees and baboons, do provide an endothelial lining in the healing response of vascular grafts. While putative evidence focuses on circulating stem cells in the blood to provide an endothelial lining, no evidence exists today to support this hypothesis.
The lack of a host response to an implanted biomaterial may be desirable in some applications; however, the holy grail of a biomaterial surface that does not adhere proteins or cells remains elusive. As noted earlier, almost immediately upon implantation, the humoral and cellular components of blood come in contact with implanted biomaterials or medical devices resulting in a provisional matrix . Recent studies have focused on inhibition of biomaterial-induced complement activation to reduce the protein adhesion phenomenon on the surface [62–64]. Inhibition of biomaterial-induced complement activation also would be expected to lead to a reduction in monocyte/macrophage adhesion to the biomaterial [40, 44]. However, the adhesion of monocytes /macrophages to biomaterial surfaces is far more complex as monocytes/macrophages express protein adhesion receptors (integrins) with at least three different types of beta chains (β1, β2, β3) that in turn can bind to a wide variety of proteins present in the provisional matrix. These blood-derived proteins include complement C3b fragments, fibrin, fibrinogen, fibronectin , factor X, and vitronectin. Moreover, integrin expression by monocytes/macrophages is time-dependent and β1 integrins are not initially detected on adherent monocytes but begin to appear during macrophage development and are strongly expressed on fusing macrophages that form foreign body giant cells [42, 44]. Thus, monocyte/macrophage adhesion with subsequent macrophage fusion to form foreign body giant cells at the interface is far more complex given the relatively large number of adhesion proteins, their respective monocyte/macrophage receptors, and the time-dependent nature of receptor up-regulation on adherent macrophages and foreign body giant cells. Other mechanisms such as apoptosis or anoikis of adherent cells may be considered to reduce the adherent monocyte/macrophage/foreign body giant cell adhesion to biomaterial surfaces. Apoptosis is programmed cell death while anoikis is a term for apoptosis induced by cell detachment from its supportive matrix. Various biomaterial surface chemistries have identified apoptosis of adherent macrophages both in vitro and in vivo [49, 65–68]. These potential mechanisms for reducing cellular adhesion have been poorly studied and offer an opportunity for controlled and down-regulation of monocyte/macrophage/foreign body giant cell adhesion to biomaterial surfaces.
Regarding development of the fibrous capsule surrounding implants, fibrocytes, a subpopulation of circulating mesenchymal progenitor cells, have been identified as augmenting wound repair as well as producing different fibrosing disorders in humans [59]. Blood circulating fibrocytes can be recruited to sites of tissue or implant injury and differentiate into fibroblasts and myofibroblasts. Myofibroblasts are now considered to be a major contributor to fibrosis and may be responsible for the remodeling of granulation tissue collagen to fibrosis-dependent collagen, i.e., collagen type I . Recent studies have suggested that the mechanical properties of the biomaterial substrate can influence the contractile nature of myofibroblasts [26, 58, 69, 70].
A successful approach to the inhibition of inflammatory adhesion and activation has been the modification of biomaterial surfaces with CD47, a transmembrane molecular marker of “self.” As inflammatory cells do not recognize these surfaces as being foreign, inflammatory cell adhesion is reduced with a down-regulation of expressed cytokines, an up-regulation of matrix metalloproteinases, and involvement of JAK/STAT signaling mechanisms [71, 72]. These findings suggest that both biomaterial degradation and fibrous capsule formation can be reduced with CD47 modification of biomaterial surfaces. Strict control of biomedical polymer morphology and porosity also has provided a means to down-regulate foreign body giant cell formation and fibrous capsule formation [34, 73]. These approaches can be expected to be useful in the development of scaffolds for clinical use.
2.9 Conclusions
Ultimately, the success or failure of medical devices, implants, and tissue-engineered constructs is modulated by the interaction between the characteristics of the biomaterial or medical device, patient conditions or factors, and surgical technique. These conditions may modulate the inflammatory, healing, and foreign body responses to biomaterials and medical devices resulting in their eventual failure. Infection remains a significant factor leading to implant failure. Recent studies suggest that individual patient genomic factors may predispose the patient to implant failure.
In the development of new biomaterials , tissue-engineered scaffolds with or without immunomodulary proteins or cells and new medical devices, the acute and chronic inflammatory response and foreign body reaction must be considered in the context of the materials, proteins, and cells that are utilized as well as the synthetic or native-derived materials that are utilized. These factors and their potential interactions must be considered in the experimental design and the goals and objectives of the study. Strengths and weaknesses of the experimental design should be identified prior to the initiation of any study designed to identify the immune response or the modulation of the immune response in a time-dependent nature. This is of special significance as the response to injury with the development of the acute and chronic inflammatory response usually occurs within the first two weeks following implantation and the foreign body reaction with adherent macrophages and foreign body giant cells , while developing within the first 2 weeks of implantation, are more persistent and in some cases have been identified to be present for the lifetime of the synthetic or biologically derived material. The investigation of tissue-engineered systems is of special significance as they have the potential to significantly modulate the immune response in a time-dependent fashion. It can be expected that each unique tissue-engineered system can lead to unique immune responses in a time-dependent fashion. While the objective of complex tissue-engineered systems is to provide regeneration of the tissue/organ under consideration, further investigation of the immune response and its modulation provides a future challenge in not only determining the relative regenerative capacity of the tissue-engineered system but also its biocompatibility and potential for success or failure.
References
Williams DF (2008) On the mechanisms of biocompatibility. Biomaterials 29(20):2941–2953
Anderson JM (2001) Biological responses to materials. Annu Rev Mater Res 31:81–110
Kumar V, Abbas AK, Fausto N et al (2005) Robbins and Cotran pathologic basis of disease, vol 15, 7th edn. Elsevier Saunders, Philadelphia, p 1525
Zdolsek J, Eaton JW, Tang L (2007) Histamine release and fibrinogen adsorption mediate acute inflammatory responses to biomaterial implants in humans. J Transl Med 5:31
Wiggins MJ, Wilkoff B, Anderson JM et al (2001) Biodegradation of polyether polyurethane inner insulation in bipolar pacemaker leads. J Biomed Mater Res 58(3):302–307
Christenson EM, Soofi W, Holm JL et al (2007) Biodegradable fumarate-based polyHIPEs as tissue engineering scaffolds. Biomacromolecules 8(12):3806–3814
Christenson EM, Dadsetan M, Wiggins M et al (2004) Poly(carbonate urethane) and poly(ether urethane) biodegradation: in vivo studies. J Biomed Mater Res A 69(3):407–416
Christenson EM, Anderson JM, Hiltner A (2004) Oxidative mechanisms of poly(carbonate urethane) and poly(ether urethane) biodegradation: in vivo and in vitro correlations. J Biomed Mater Res A 70(2):245–255
Henson PM (1971) The immunologic release of constituents from neutrophil leukocytes. II. Mechanisms of release during phagocytosis, and adherence to nonphagocytosable surfaces. J Immunol 107(6):1547–1557
Marchant RE, Anderson JM, Dillingham EO (1986) In vivo biocompatibility studies. VII. Inflammatory response to polyethylene and to a cytotoxic polyvinylchloride. J Biomed Mater Res 20(1):37–50
Yamaguchi K, Konishi H, Hara S et al (2001) Biocompatibility studies of titanium-based alloy pedicle screw and rod system: histological aspects. Spine J 1(4):260–268
MacEwan MR, Brodbeck WG, Matsuda T et al (2005) Monocyte/lymphocyte interactions and the foreign body response: in vitro effects of biomaterial surface chemistry. J Biomed Mater Res A 74(3):285–293
Brodbeck WG, Macewan M, Colton E et al (2005) Lymphocytes and the foreign body response: lymphocyte enhancement of macrophage adhesion and fusion. J Biomed Mater Res A 74(2):222–229
Mooney JE, Rolfe BE, Osborne GW et al (2010) Cellular plasticity of inflammatory myeloid cells in the peritoneal foreign body response. Am J Pathol 176(1):369–380
Gordon S, Pluddemann A (2013) Tissue macrophage heterogeneity: issues and prospects. Semin Immunopathol 35(5):533–540
Gordon S (2003) Alternative activation of macrophages. Nat Rev Immunol 3(1):23–35
Mosser DM, Edwards JP (2008) Exploring the full spectrum of macrophage activation. Nat Rev Immunol 8(12):958–969
Mantovani A, Sozzani S, Locati M et al (2002) Macrophage polarization: tumor-associated macrophages as a paradigm for polarized M2 mononuclear phagocytes. Trends Immunol 23(11):549–555
Mantovani A, Sica A, Sozzani S et al (2004) The chemokine system in diverse forms of macrophage activation and polarization. Trends Immunol 25(12):677–686
Silver IA, Murrills RJ, Etherington DJ (1988) Microelectrode studies on the acid microenvironment beneath adherent macrophages and osteoclasts. Exp Cell Res 175(2):266–276
Klebanoff SJ (2005) Myeloperoxidase: friend and foe. J Leukoc Biol 77(5):598–625
Jankowski A, Scott CC, Grinstein S (2002) Determinants of the phagosomal pH in neutrophils. J Biol Chem 277(8):6059–6066
Haas A (2007) The phagosome: compartment with a license to kill. Traffic 8(4):311–330
Nguyen LL, D’Amore PA (2001) Cellular interactions in vascular growth and differentiation. Int Rev Cytol 204:1–48
Browder T, Folkman J, Pirie-Shepherd S (2000) The hemostatic system as a regulator of angiogenesis. J Biol Chem 275(3):1521–1524
Hinz B, Phan SH, Thannickal VJ et al (2012) Recent developments in myofibroblast biology: paradigms for connective tissue remodeling. Am J Pathol 180(4):1340–1355
Micallef L, Vedrenne N, Billet F et al (2012) The myofibroblast, multiple origins for major roles in normal and pathological tissue repair. Fibrogenesis Tissue Repair 5(Suppl 1):S5
Pierce GF (2001) Inflammation in nonhealing diabetic wounds: the space-time continuum does matter. Am J Pathol 159(2):399–403
Mustoe TA, Pierce GF, Thomason A et al (1987) Accelerated healing of incisional wounds in rats induced by transforming growth factor-beta. Science 237(4820):1333–1336
Clark RAF (1996) The molecular and cellular biology of wound repair, vol 23, 2nd edn. Plenum Press, New York, p 611, 611 leaf of plates
Broughton G 2nd, Janis JE, Attinger CE (2006) The basic science of wound healing. Plast Reconstr Surg 117(7 Suppl):12S–34S
Anderson JM, Rodriguez A, Chang DT (2008) Foreign body reaction to biomaterials. Semin Immunol 20(2):86–100
Anderson JM, Cramer S (2015) Perspectives on the inflammatory, healing, and foreign body responses to biomaterials and medical devices. In: Badylak S (ed) Host response to biomaterials. The impact of host response on biomaterial selection. Elsevier, New York, pp 13–36
Bota PC, Collie AM, Puolakkainen P et al (2010) Biomaterial topography alters healing in vivo and monocyte/macrophage activation in vitro. J Biomed Mater Res A 95(2):649–657
Revell PA (2008) The combined role of wear particles, macrophages and lymphocytes in the loosening of total joint prostheses. J R Soc Interface 5(28):1263–1278
Charnley J (1970) The reaction of bone to self-curing acrylic cement. A long-term histological study in man. J Bone Joint Surg Br 52(2):340–353
Purdue PE (2008) Alternative macrophage activation in periprosthetic osteolysis. Autoimmunity 41(3):212–217
Brodbeck WG, Anderson JM (2009) Giant cell formation and function. Curr Opin Hematol 16(1):53–57
McNally AK, DeFife KM, Anderson JM (1996) Interleukin-4-induced macrophage fusion is prevented by inhibitors of mannose receptor activity. Am J Pathol 149(3):975–985
McNally AK, Anderson JM (1994) Complement C3 participation in monocyte adhesion to different surfaces. Proc Natl Acad Sci U S A 91(21):10119–10123
Nilsson B, Ekdahl KN, Mollnes TE et al (2007) The role of complement in biomaterial-induced inflammation. Mol Immunol 44(1–3):82–94
McNally AK, Macewan SR, Anderson JM (2007) alpha subunit partners to beta1 and beta2 integrins during IL-4-induced foreign body giant cell formation. J Biomed Mater Res A 82(3):568–574
McNally AK, Jones JA, Macewan SR et al (2008) Vitronectin is a critical protein adhesion substrate for IL-4-induced foreign body giant cell formation. J Biomed Mater Res A 86(2):535–543
McNally AK, Anderson JM (2002) Beta1 and beta2 integrins mediate adhesion during macrophage fusion and multinucleated foreign body giant cell formation. Am J Pathol 160(2):621–630
Jenney CR, Anderson JM (2000) Adsorbed serum proteins responsible for surface dependent human macrophage behavior. J Biomed Mater Res 49(4):435–447
Hynes RO, Zhao Q (2000) The evolution of cell adhesion. J Cell Biol 150(2):F89–F96
Hynes RO (2002) Integrins: bidirectional, allosteric signaling machines. Cell 110(6):673–687
Kyriakides TR (2015) Molecular events at tissue-biomaterial interface. In: Badylak SF (ed) Host response to biomaterials. The impact of host response on biomaterial selection. Elsevier, New York, pp 81–116
Jones JA, Chang DT, Meyerson H et al (2007) Proteomic analysis and quantification of cytokines and chemokines from biomaterial surface-adherent macrophages and foreign body giant cells. J Biomed Mater Res A 83(3):585–596
Chang DT, Colton E, Anderson JM (2009) Paracrine and juxtacrine lymphocyte enhancement of adherent macrophage and foreign body giant cell activation. J Biomed Mater Res A 89(2):490–498
Anderson JM, Jones JA (2007) Phenotypic dichotomies in the foreign body reaction. Biomaterials 28(34):5114–5120
Sieweke MH, Allen JE (2013) Beyond stem cells: self-renewal of differentiated macrophages. Science 342(6161):1242974
Robbins CS, Hilgendorf I, Weber GF et al (2013) Local proliferation dominates lesional macrophage accumulation in atherosclerosis. Nat Med 19(9):1166–1172
Badylak SF (2016) Tissue regeneration. A scaffold immune microenvironment. Science 352(6283):298
Wynn TA, Ramalingam TR (2012) Mechanisms of fibrosis: therapeutic translation for fibrotic disease. Nat Med 18(7):1028–1040
Wynn TA (2008) Cellular and molecular mechanisms of fibrosis. J Pathol 214(2):199–210
Hinz B, Mastrangelo D, Iselin CE et al (2001) Mechanical tension controls granulation tissue contractile activity and myofibroblast differentiation. Am J Pathol 159(3):1009–1020
Hinz B (2007) Formation and function of the myofibroblast during tissue repair. J Invest Dermatol 127(3):526–537
Bucala R (2012) Review series—inflammation & fibrosis. Fibrocytes and fibrosis. QJM 105(6):505–508
Farra R, Sheppard NF Jr, McCabe L et al (2012) First-in-human testing of a wirelessly controlled drug delivery microchip. Sci Transl Med 4(122):122ra121
Hashimoto D, Chow A, Noizat C et al (2013) Tissue-resident macrophages self-maintain locally throughout adult life with minimal contribution from circulating monocytes. Immunity 38(4):792–804
Morais JM, Papadimitrakopoulos F, Burgess DJ (2010) Biomaterials/tissue interactions: possible solutions to overcome foreign body response. AAPS J 12(2):188–196
Kourtzelis I, Rafail S, DeAngelis RA et al (2013) Inhibition of biomaterial-induced complement activation attenuates the inflammatory host response to implantation. FASEB J 27(7):2768–2776
Ekdahl KN, Lambris JD, Elwing H et al (2011) Innate immunity activation on biomaterial surfaces: a mechanistic model and coping strategies. Adv Drug Deliv Rev 63(12):1042–1050
Shive MS, Brodbeck WG, Anderson JM (2002) Activation of caspase 3 during shear stress-induced neutrophil apoptosis on biomaterials. J Biomed Mater Res 62(2):163–168
Brodbeck WG, Shive MS, Colton E et al (2001) Influence of biomaterial surface chemistry on the apoptosis of adherent cells. J Biomed Mater Res 55(4):661–668
Brodbeck WG, Patel J, Voskerician G et al (2002) Biomaterial adherent macrophage apoptosis is increased by hydrophilic and anionic substrates in vivo. Proc Natl Acad Sci U S A 99(16):10287–10292
Brodbeck WG, Colton E, Anderson JM (2003) Effects of adsorbed heat labile serum proteins and fibrinogen on adhesion and apoptosis of monocytes/macrophages on biomaterials. J Mater Sci Mater Med 14(8):671–675
Klingberg F, Hinz ES, White B (2013) The myofibroblast matrix: implications for tissue repair and fibrosis. J Pathol 229(2):298–309
Hinz B, Gabbiani G (2010) Fibrosis: recent advances in myofibroblast biology and new therapeutic perspectives. F1000 Biol Rep 2:78
Stachelek SJ, Finley MJ, Alferiev IS et al (2011) The effect of CD47 modified polymer surfaces on inflammatory cell attachment and activation. Biomaterials 32(19):4317–4326
Finley MJ, Clark KA, Alferiev IS et al (2013) Intracellular signaling mechanisms associated with CD47 modified surfaces. Biomaterials 34(34):8640–8649
Fukano Y, Usui ML, Underwood RA et al (2010) Epidermal and dermal integration into sphere-templated porous poly(2-hydroxyethyl methacrylate) implants in mice. J Biomed Mater Res A 94(4):1172–1186
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Anderson, J.M., Jiang, S. (2017). Implications of the Acute and Chronic Inflammatory Response and the Foreign Body Reaction to the Immune Response of Implanted Biomaterials. In: Corradetti, B. (eds) The Immune Response to Implanted Materials and Devices. Springer, Cham. https://doi.org/10.1007/978-3-319-45433-7_2
Download citation
DOI: https://doi.org/10.1007/978-3-319-45433-7_2
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-45431-3
Online ISBN: 978-3-319-45433-7
eBook Packages: Chemistry and Materials ScienceChemistry and Material Science (R0)