Abstract
Newer mitral valve repair techniques have emerged in recent years and long term results of these are needed. The indications for these repair techniques in addition to mitral valve annuloplasty also need to be better defined. The role of myocardial viability in guiding management of this condition also needs further investigation. Longer term follow up is also needed in studies comparing mitral valve repair versus replacement in functional ischaemic mitral regurgitation. Further studies are also needed on the role of ventricular restoration surgery in those with very dilated left ventricles as well as the longer term results of percutaneous treatment of mitral regurgitation.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Functional ischemic mitral regurgitation
- Mitral annuloplasty
- Mitral valve replacement
- Myocardial viability
- Percutaneous mitral valve repair
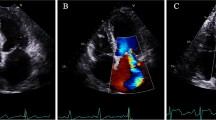
Functional ischemic mitral regurgitation is one of the most challenging conditions to manage. Unlike organic mitral regurgitation where there is purely a mechanical problem, and correcting the mitral regurgitation either by mitral valve repair or replacement, results in a cure for most patients, functional ischemic mitral regurgitation has many pathologies, each of which must be adequately addressed to achieve the best outcome for the patient. These include the coronary artery disease, myocardial ischemia and myocardial infarction, left ventricular dilatation, dysfunction and scarring, and the tethering of the mitral valve apparatus, in addition to the mitral regurgitation. The problem is that not all of the pathologies can be effectively treated in every patient, and unlike in degenerative mitral regurgitation where excellent and durable valve repair techniques are in existence, in functional ischemic mitral regurgitation, a consistent, durable valve repair for every patient remains elusive. Although the technique of mitral valve repair by mitral annuloplasty is well established, and is efficacious in many cases of ischaemic mitral regurgitation, particularly if the mitral regurgitation is not too severe and the leaflets not too severely restricted, several studies have reported limited durability of this valve repair technique in cases of very severe mitral regurgitation, those with severe tethering of the mitral valve leaflets, and those with severely dilated left ventricles [1, 2]. Newer repair techniques on the subvalvular apparatus are in use to address the severely tethered leaflets, e.g., papillary muscle repositioning, but long term results of this is still awaited and studies comparing it to conventional mitral annuloplasty are needed [3].
Functional ischaemic mitral regurgitation is a disease of the left ventricle (LV). However, adequate assessment of the LV is usually not performed in many studies on ischaemic mitral regurgitation and in clinical practice. A recent randomised controlled trial reported similar outcomes in patients with moderate functional ischemic mitral regurgitation receiving coronary artery bypass grafting alone and in those receiving combined coronary artery bypass grafting and mitral annuloplasty [4]. However, there was no assessment of LV viability in this study and it is likely that most patients in this study had non-infarcted viable left ventricles which recovered its function with successful coronary artery revascularisation. On the contrary, another randomised trial reported better outcomes in those who received combined coronary artery bypass graft surgery and mitral annuloplasty [1]. In this study, LV viability assessment was done on all patients and most had non-viable scarred myocardium in the inferior LV wall. Further studies are needed to determine if the assessment of myocardial viability or presence of scar tissue may help distinguish those who would improve with successful coronary artery revascularisation alone, and those in whom a concomitant valve repair is needed.
Recent studies have suggested that mitral valve replacement may be superior to mitral valve repair in those with very severe mitral regurgitation and dilated left ventricles in terms of valve durability [2]. However, many of these patients received a bioprosthetic valve which is known to have a limited durability, and longer term results beyond 10 years are needed to truly determine if mitral valve replacement or repair is better, or if the two surgical treatments are equivalent. Comparisons with other repair techniques besides mitral annuloplasty are also needed particularly in those with severely restricted leaflets where papillary muscle procedures may be beneficial.
Further studies are also needed on the use of left ventricular restoration surgery in patients with severe functional ischaemic mitral regurgitation and very dilated left ventricles. It has been reported that long term survival is not as good in this group of patients compared to those with less dilated left ventricles when CABG and mitral annuloplasty alone are used [5]. It has been suggested that this group of patients would benefit from adding LV restoration surgery but further more objective studies are needed including randomised trials comparing the two procedures directly.
Percutaneous techniques have been developed and are showing promise in functional ischemic mitral regurgitation. However, there is a continuing problem with residual or recurrent mitral regurgitation. Randomised trials are also needed to determine if it is beneficial compared to optimal medical therapy and conventional valve repair or replacement operations.
References
Chan KMJ, Punjabi PP, Flather MF, Wage R, Symmonds K, Roussin I, Rahman-Haley S, Pennell DJ, Kilner PJ, Dreyfus GD, Pepper JR. Coronary artery bypass surgery with or without mitral valve annuloplasty in moderate functional ischemic mitral regurgitation: final results of the Randomized Ischemic Mitral Evaluation (RIME) Trial. Circulation. 2012;126:2502–10.
Acker MA, Parides MK, Perrault LP, Moskowitz AJ, Gelijns AC, Voisine P, Smith PK, Hung JW, Blackstone EH, Puskas JD, Argenziano M, Gammie JS, Mack M, Ascheim DD, Bagiella E, Moquete EG, Ferguson TB, Horvath KA, Geller NL, Miller MA, Woo YJ, D’Alessandro DA, Ailawadi G, Dagenais F, Gardner TJ, O’Gara PT, Michler RE, Kron IL, CTSN. Mitral valve repair versus replacement for severe ischemic mitral regurgitation. N Engl J Med. 2014;370:23–32.
Kron IL, Green GR, Cope JT. Surgical relocation of the posterior papillary muscle in chronic ischemic mitral regurgitation. Ann Thorac Surg. 2002;74:600–1.
Smith PK, Puskas JD, Ascheim DD, Voisine P, Gelijns AC, Moskowitz AJ, Hung J, Parides MK, Ailawadi G, Perrault LP, Acker MA, Argenziano M, Thourani V, Gammie JS, Miller MA, Page P, Overbey JR, Bagiella E, Dagenais F, Blackstone EH, Kron IL, Goldstein DJ, Rose EA, Moquete EG, Jeffries N, Gardner TJ, O’Gara PT, Alexander JH, Michler RE. Surgical treatment of moderate ischemic mitral regurgitation. N Engl J Med. 2014;371:2178–88.
Braun J, van de Veire NR, Klautz RJM, Versteegh MIM, Holman ER, Westenberg JM, Boersma E, van der Wall EE, Bax JJ, Dion RAE. Restrictive mitral annuloplasty cures ischemic mitral regurgitation and heart failure. Ann Thorac Surg. 2008;85:430–7.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Chan, K.M.J. (2017). Future Directions in Functional Mitral Regurgitation. In: Chan, K. (eds) Functional Mitral and Tricuspid Regurgitation. Springer, Cham. https://doi.org/10.1007/978-3-319-43510-7_17
Download citation
DOI: https://doi.org/10.1007/978-3-319-43510-7_17
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-43508-4
Online ISBN: 978-3-319-43510-7
eBook Packages: MedicineMedicine (R0)