Abstract
Patients treated with damage control surgery develop a severe systemic inflammatory response associated with a catabolic state compounded by protein losses through the open abdomen. Diligence regarding nutrition provision is essential for optimal outcomes in these patients. Enteral nutrition (EN) should be initiated within 24–36 h of admission, or as soon as gastrointestinal continuity is restored, regardless of resuscitation status. Avoiding hypervolemia and closing the abdomen as soon as possible help to minimize protein losses. Direct peritoneal resuscitation can be useful as an adjunct therapy, facilitating earlier closure of the abdomen. Post-pyloric feeding is preferred, but there is no reason to withhold pre-pyloric feeding if this cannot be achieved. Planning for definitive surgical therapy includes consideration for surgical feeding access as early as postoperative day 1. Keeping an intubated patient “nil per os,” or EN turned off for operative procedures is an archaic practice and potentially detrimental. There are benefits to EN even if administered in amounts that provide less than goal caloric requirements. Suboptimal nutrition due to interruptions in delivery can be mitigated through the use of feeding protocols. EN is superior to parenteral nutrition (PN); but if EN is not providing at least 60–70 % of the calories and protein needed by day 5–7, PN must then be considered. Provision of appropriate and early goal-directed protein and caloric support should be considered an essential component in the management of the patient with an open abdomen.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Open abdomen
- Pancreatitis
- Enteral nutrition
- Parenteral nutrition
- Resuscitation
- Damage control surgery
- Systemic inflammatory response syndrome
- Sepsis
- Trauma
- Immunomodulation
- Guidelines
Introduction
Patients with hemorrhagic shock, severe sepsis, and necrotizing pancreatitis treated with damage control surgery develop a severe systemic inflammatory response characterized by release of pro-inflammatory mediators. Those with open abdomens represent the sickest, most inflamed, and most hypermetabolic cohort of surgical patients. The acute catabolic reaction associated with severe physiologic stress and inflammation results in muscle proteolysis with increased urinary nitrogen excretion and weight loss, compounded by an increased resting energy expenditure attributed to the large open wound. This severe catabolic pro-inflammatory cascade and physical loss of protein continues until the abdomen is closed. Enteral nutrition (EN) provided within 24–36 h after admission to the ICU has been advocated in critically ill surgical patients. This is thought to ameliorate immune suppression which is characterized by the cytokine-generated stress response at the level of the gut. EN is better than parenteral nutrition (PN). However, if PN is started there are fewer associated complications if it is started late, after 5–7 days post admission. In the open abdomen patient, higher protein and calorie requirements are usually present not only because of the hypermetabolic response, but also because of the physical loss of fluid and protein from the open abdomen and negative pressure dressing. Therefore, ongoing diligence regarding nutrition provision (EN, PN, or both) is essential for optimal outcomes in the open abdomen patient.
Admission
Upon entering this patient’s abdomen, even the young surgeon knows that this patient is going to require multiple operative interventions and great attention to detail in all aspects of his critical care. His critical illness and hyperinflammatory or hypercatabolic state is compounded by the significant fluid, electrolyte, and protein losses from exposed viscera [1]. This immediate protein–calorie malnutrition develops with impairment of immune function, and subclinical multiple organ dysfunction will continue at least until his abdomen is closed [2].
Enteral nutrition (EN) provided within 24–36 h after ICU admission or initial operation is advocated. This early but lower than goal EN ameliorates the immune suppression and attenuates the systemic inflammatory response syndrome (Fig. 5.1). In addition, early EN with an open abdomen is associated with increased fascial closure rates, earlier fascial closure, reduced incidence of infectious complications, and a decrease in mortality, especially in patients without bowel injuries [3, 4]. Positive associations in the literature are inconsistent likely due to the heterogenous patient population studied, but there have been no reported adverse outcomes from EN with open abdomens.
The importance of early EN is less about the protein–calorie malnutrition and deficit, more about supporting the gastrointestinal immune structure and battling the systemic inflammatory response syndrome (SIRS) so common in patients with an open abdomen. In addition to nutrition, basic tenants of critical care such as source control and oxygen delivery address the SIRS response [5]
After the debridement and full drainage of the patient’s pancreas, full exploration of the health of the bowel must occur as ischemia of the small bowel and right and transverse colon is at times observed. Regardless, some type of nasoenteric feeding access is a must. At a minimum, a nasogastric or orogastric tube is required. We recommend if at all possible a nasojejunal tube and a nasogastric tube, one in each nostril. Either tube can be palpated at this point due to minimal bowel wall edema that is present day one. Commercial bridle systems can be used to prevent suturing to nasal septum and complications associated with tube securement. At this point, a negative pressure dressing is provided to the abdominal wall and the patient is ready for transport to the ICU.
EN is better than parenteral nutrition (PN), and if PN is started there are fewer associated complications if it is started late. PN should be considered if enteral nutrition is not providing at least 60–70 % of the calories and protein needed by the patient at the day 5–7 mark. Combined EN and PN nutrition support has a role in a selected group of patients [6].
Day 0
After damage control surgery, emphasis of management shifts from the operating room (OR) to the intensive care unit (ICU) where physiologic deficits are corrected in preparation for return to the OR. Goals of resuscitation are to restore physiologic reserve, tissue perfusion, normothermia, acid-base balance, and coagulation. Once euvolemia and hemodynamic stability ± vasopressor therapy are achieved and metabolic acidosis resolved, enteral feeds should be initiated.
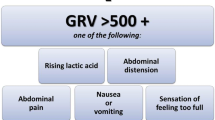
Regarding enteric access at this point, a nasogastric or orogastric tube would be adequate. Traditional teaching is to feed post-pyloric, and nasojejunal tubes have been considered ideal feeding access with pancreatitis. However, clinical trials have demonstrated that feeding either the small bowel or stomach is well tolerated in severe pancreatitis [7]. In addition, the early (less than 24 h from admission) administration of EN is considered an active therapeutic intervention against severe pancreatitis. In general, post-pyloric feeding is preferred when feasible as there is evidence of a 30 % lower rate of pneumonia and an increase in the amount of nutrition delivered [8]. However, if it proves technically difficult, there is no reason to withhold pre-pyloric feeding. Tube feeding formula should be started at a low rate, ~20 mL/h or ~50 % of goal. If there is no evidence of gastroparesis, ileus, or mesenteric ischemia indicated by high residuals, emesis, or rising lactic acid levels, feeds can continue.
Achieving euvolemia with resuscitation is tantamount to the ability to close the abdomen. Hypervolemia causes bowel edema, increased protein losses, and ileus. Fluid resuscitation should cease when hourly urine output reaches 0.5–1 cc/kg/h in normal kidneys. More urine output is not better, and indicative of overresuscitation. There are a number of methods utilized to indirectly measure preload and vascular resistance as well; all are about equal in terms of reliability and accuracy. Direct peritoneal resuscitation can be helpful in terms of fluid balance in a patient with an open abdomen. It is a validated adjunct resuscitation strategy in patients with open abdominal wounds due to sepsis or hemorrhage. The practice consists of suffusing the peritoneal cavity with a 2.5 % glucose-based peritoneal dialysis solution (2.5 % Delflex: 25 g/L d-glucose, 0.567 g/L sodium chloride, 0.392 g/L sodium lactate 0.0257 g/L calcium chloride, 0.0152 g/L magnesium chloride at a pH of 6, osmolality of 486 mOsm/L) concurrent with intravenous resuscitation and negative pressure abdominal wound dressing. Though glucose is present, this would not be considered a part of nutrition provision. Direct peritoneal resuscitation causes microvascular vasodilation and increases visceral and hepatic blood flow, normalizes systemic water compartments [9], accelerates primary abdominal wall closure after damage control surgery, and prevents complications associated with an open abdomen [10, 11]. In addition to observed effects on microcirculation, it has marked ability to decrease visceral edema and normalize body water ratios, decreasing the incidence of ileus and improving enteric nutrition tolerance.
Day 1
Enteral nutrition continues. Usually by this point, EN has been initiated and calorie and protein goals are calculated, usually 35 kcal/kg/day and 2–2.5 g of protein/kg/day. Weight in kg is based on ideal body weight. If the patient demonstrates intolerance in terms of high residuals, emesis, or distension, or even ongoing SIRS, pushing rate to 100 % of goal is not necessary.
Day 1 is time to begin planning re-operation in terms of what needs to be accomplished prior to definitive closure. This includes further debridement if necessary, determining adequate drainage, planning reconstruction if necessary, and definitive feeding access. Even if a third exploration is necessary, surgical feeding access should be established as soon as intestinal continuity is restored. This helps avoid difficulty with positioning feeding tubes and iatrogenic injury related to inflammatory or edematous changes to the bowel wall. A gastrostomy tube is acceptable, but carries some risk of aspiration and pre-pyloric feeding intolerance. A gastrostomy and a jejunostomy tube can be placed to mitigate some of the risk associated with a gastrostomy tube alone, but the jejunostomy tube is traditionally fraught with complications including obstruction, dislodgement, volvulus, and leakage. Our favored approach is a single combination gastrojejunostomy tube, 22Fr soft silicone with retention balloon, inserted through a gastrostomy utilizing the Stamm technique. The distal lumen is guided and positioned toward the ligament of Treitz. Postoperative management is the same as a gastrostomy tube. It provides the option of simultaneous gastric decompression with concurrent post-pyloric feeding, without the additional enterotomy and risks associated with jejunostomy. We have used these tubes even in the presence of gastroduodenal pathology, such as perforated duodenal ulcers, with excellent results.
Day 2–5
Consideration must be given to how much nutrition is delivered versus what was ordered. Underfeeding has been demonstrated in multiple comparative clinical studies, with a fraction of required calories being delivered to critical care populations across multiple ICUs [12]. Several factors contribute to the suboptimal delivery of nutrition, including gastrointestinal intolerance, elective disruptions for transport, radiographic imaging, surgeries, complications related to delivery system, and lack of efficient protocol support for the timely advancement of enteral feeds to goal due to fear of feed-related morbidity (i.e., high gastric residuals, bloating, vomiting, aspiration, and diarrhea). The deleterious effects of underfeeding on outcomes for hospitalized patients have long been recognized. Hypocaloric feeding and negative energy balances have been linked to prolonged ICU length of stay, prolonged mechanical ventilation, increased risk for infectious complications, and higher mortality [6]. Feeding protocols can help mitigate underfeeding, by providing staff with adjustable rates to achieve a 24 h caloric goal [13]. There is no harm in feeding patients who have controlled airways through a trip to the OR, especially if the feeding tube is post-pyloric. Keeping an intubated patient “nil per os,” or EN turned off for operative procedures is an archaic practice and potentially detrimental. During the time period from day 2 to 5, the patient should be improving. The systemic inflammation should be abating, resuscitation end points reached, vasopressor requirement diminishing, and overall the patient is preparing for extubation with the abdomen hopefully closed. During this time, patients should come closer to meeting full protein and calorie goal requirements. Not only should the physician-led team increase the order or delivery of the EN, but the patient will also demonstrate tolerance to this delivery.
Day 5 and Beyond
By hospital day 5 of an open abdomen patient, successful resuscitation is complete. Though the ventilator or vasopressors may still be required, the patient is certainly in a different place than when admitted. There should have been at least numerous attempts to provide enteral nutrition via the potential routes described above. In addition, goal feeds should have been attempted with distal feeds or gastric motility agents if true gastric intolerance is present. The patient is still likely in a systemic inflammatory state and hypermetabolic. With this in mind, attempts to decrease this catabolic state can be attempted with agents such as propranolol. Though no literature describing associations between open abdomens and the use of propranolol exists, burn literature utilizing propranolol to decrease the hypercatabolic state has been noted and may be beneficial in the open abdomen patient [14]. The same can be described for agents such as oxandrolone as an anabolic agent in the open abdomen patient [14].
As illustrated in Fig. 5.2, at some point protein and calorie provision or deficit becomes a priority. Regardless of the reason, unsuccessful provision of enteral nutrition adds to the severe protein–calorie malnutrition that is associated with the critical illness present in patients with an open abdomen. Therefore, if enteral nutrition is not providing at least 60–70 % of the calories and protein needed by the patient at the day 5–7 mark, parenteral nutrition must be considered. In their landmark prospective randomized study examining early (within 48 h of admission to the ICU) vs late (>7 days after admission to ICU) PN in >4600 critically ill adults (89 % of whom were complex surgical patients), Casaer et al. found that patients in the late PN initiation group had fewer ICU infections, a lower incidence of cholestasis, decreased mechanical ventilation days, reduced duration of renal replacement therapy, a mean reduction in health care costs, and an increased likelihood of being discharged alive earlier from the ICU and from the hospital [15]. To specifically address trauma patients, Sena et al. studied trauma patients and examined the effects of early PN use (within first 7 days post-injury) to address caloric deficit. In those patients receiving early PN and a modest amount of EN during the first week (>1000 kcal/kg), there was an increased risk of nosocomial infection, late acute respiratory distress syndrome (ARDS), duration of mechanical ventilation, ICU length of stay, and mortality compared with those patients receiving EN alone. Supplemental PN to achieve nutrition goals within the first week after injury provided worse outcomes in trauma patients. The high risk for or presence of severe protein–calorie malnutrition related to critical illness is associated with poor outcomes; however, supplemental PN was associated with even worse outcomes [16].
In three other recent studies, early PN either demonstrated no change in outcomes or improvement in quality of post-ICU life, fewer ventilator days, fewer infections and less muscle and fat loss [17–19]. However, methodological issues, timing of PN, and ultimately interpretation of results still has not changed the overall message that a delay of 5+ days of PN in the open abdomen patient who presents well nourished is what is most accepted.
To start parenteral nutrition (PN), central access must be present. Options include internal jugular, subclavian, or peripherally inserted central catheters. The femoral vein location should not be used. The tip of the catheter should be located at the superior vena cava/atrial junction to prevent the hyperosmolar load of PN being caustic to smaller veins, thereby increasing the risk of thrombus. Once access is present, ordering the PN usually is performed through central pharmacy. It is imperative that the surgeon be directly involved in the process of PN ordering and administration. The surgeon will better understand the complexity of the pro-inflammatory open abdomen patient, and therefore the higher than expected protein and calorie needs. As noted previously, it is not uncommon to lose at least 30 g of protein per day just from the fluid that is suctioned off the negative pressure device or dressing that is required with the open abdomen patient [2].
Typically, 2.0 g/kg of dosing patient weight per day of protein should be ordered. If the patient is also undergoing continuous renal replacement therapy (CRRT), 2.5 g/kg/day should be ordered as this therapy will pull off protein as well. Carbohydrates in the form of dextrose should also be ordered but started at less than goal for the patient. Typically, 150–200 g of dextrose is a good starting point for the first 24 h. The key is for the patient not to become hyperglycemic beyond approximately 150 mg/dl. It is not uncommon for the open abdomen patient, especially with necrotizing pancreatitis/pancreatic necrosectomy, to be hyperglycemic and receiving an insulin drip via protocol. The PN should not exacerbate this process; therefore, the glucose should be increased to goal as the glucose levels allow. Lipids are typically held from the PN formula for the first seven or so days of initiating PN. Though the data is quite soft, lipid formulas that are currently available in the United States are soy based, have a higher omega-3 to omega-6 ratio, and have potential to be more pro-inflammatory. Therefore, lipids are held until the second week of PN. The potential deficiency of free fatty acids is so uncommon, and there is no significant harm to the patient withholding the lipids.
Every day of this patient’s care should include a plan or an attempt to provide EN, just as every day of ventilator care should include a plan of potential extubation. If PN is needed, the key is providing it safely, as described. In addition, short- and long-term plans should be arranged to transition PN to EN or nutrition per os. The plans could include simply to treat gastroparesis pharmacologically and provide distal feeding access, or to arrange for fistula care and home PN until gastrointestinal reconstruction can be completed. Typically transitions to EN or per os and off of PN should occur when the enteral route reaches 70+ % of the patient’s nutritional goals. In addition, transition off of EN can occur when the oral route provides 70+ % of the patient’s nutritional goals.
Conclusion
In response to DCS and open abdominal decompression for management of ACS, patients being managed with an open abdomen have become increasingly more common in medical and surgical ICUs. Those patients with an open abdomen commonly represent one of the most critically ill patients in the ICU. These patients have a tremendous inflammatory response, are intensely hypermetabolic, and subsequently are at the highest risk for the development of malnutrition.
Only a handful of studies specifically address nutrition and the open abdomen; however, experience by numerous authors and the few studies dealing with this population have demonstrated safety with administration of enteral feeds. In addition, given the morbidity- and mortality-reducing benefits of EN, provision of appropriate and early goal-directed protein and caloric support should be considered an essential component in the management of the patient with an open abdomen. In fact, patients show benefit to early enteral nutrition (though not necessarily at goal) directly and indirectly related to their open abdomen. PN on the other hand should be held for the first 5–7 days of hospital care in most of these patients with an open abdomen, despite the difficulty of delivering EN. Regardless, patients with an open abdomen must have nutrition addressed daily, to ensure appropriate access and nutrition is available, considered, and adjusted as the need for specialized nutrition (EN and PN) will likely continue for weeks to months after the hospital admission.
Example of Nutrition Protocol Guidelines
Initial Nutrition Evaluation
-
Resuscitation goals met?
-
No → Continue resuscitation. Do not start nutrition provision.
-
Yes → Consult nutrition support and start enteral nutrition (EN) (see below, enteral nutrition).
-
All patients should have nutrition regimen within 36 h.
-
EN is preferred over parenteral nutrition (PN) (see protocols below).
-
-
-
Protocols
-
GI stress ulcer prophylaxis.
-
Lab protocol.
-
Obtain pre-albumin and CRP levels at day 2 if anticipated ICU stay is >3 days.
-
Repeat and re-assess every Monday/Thursday.
-
-
Glucose control <150 mg/dl, avoid hypoglycemia.
-
Wound healing protocol (for open abdomen, burns, large wounds, or fistulas).
-
Ascorbic acid (Vitamin C) 500 mg BID PO/PT/IV × 10 days.
-
Vitamin A 10,000 IU, PO/PT/IM × 10 days (Excluded in pregnancy).
-
Zinc 220 mg PO × 10 days PO or PT −50 mg/10 ml elemental oral solution (Excluded in pregnancy).
-
-
Severe cachexia/malnourishment.
-
Consider use of oxandrolone 10 mg po/pt twice daily.
-
-
Enteral Nutrition (EN)
-
Initiation of EN
-
Start EN at 50 % of goal (~25–30 ml/h) within 24–48 h of admission, or when GI continuity restored.
-
Advance as tolerated to goal by day 5 with improvement of SIRS or critical illness.
-
If not at 60 % of goal after 5–7 days, consider PN supplementation (refer to protocol).
-
-
Withhold EN if hemodynamically unstable, increase in pressors, or lactic acidosis.
-
EN Access
-
Placement
-
Begin with blind bedside nasogastric feeding tube.
-
Consider bedside Cortrak ©, endoscopic, fluoroscopic, or intraoperative placement.
-
OGT and NGT placement confirmed by physical exam and X-ray.
-
Small-bore feeding tube placement confirmed by X-ray or Cortrak © placement.
-
-
Gastric access
-
Short term: OGT, NGT, small-bore feeding tube.
-
Long term (>30 days): PEG (initiate TF 4–6 h post PEG placement).
-
-
Post-pyloric access
-
Short term: Consider blind/endoscopic/fluoroscopic/Cortrak©/intra-operative placement.
-
Long term (>30 days): endoscopic placement of PEG/J.
-
Indications
-
Gastroparesis with persistent high (500 ml) gastric residual volume (GRV) despite prokinetic agents or recurrent emesis.
-
Severe active pancreatitis (endoscopic placement for jejunal feeds).
-
Open abdomen.
-
-
-
Parenteral Nutrition (PN)
-
If previously healthy, initiate PN only after the first 5–7 days of hospitalization if EN is not feasible.
-
If severe protein–calorie malnutrition present and EN not feasible, start PN immediately after resuscitation.
-
Weaning TPN when:
-
TFs tolerated at 60 % of goal.
-
Decrease TPN by discontinuing lipids, decrease dextrose and continuing goal dose of amino acids/protein.
-
Wean off TPN as TF rate advances to goal or per clinician judgment.
-
-
POs tolerated at 60 % of meals consumed.
-
Decrease TPN by discontinuing lipids, decrease dextrose and continuing goal dose of amino acids/protein.
-
Wean off TPN as TF rate advances to goal or per clinician judgment.
-
-
Nutritional Goals
-
Dosing weight:
-
Use IBW for height if actual body weight is >IBW.
-
Hamwi method:
-
Men:106# (48 kg)1st 5 ft, then add 6# (2.7 kg) per inch >5ft, ±10 %.
-
Women: 100# (45 kg)1st 5 ft, then add 5# (2.3 kg) per inch >5ft, ±10 %.
-
-
Use actual body weight if weight is <IBW
-
-
Caloric goals:
-
25–35 kcal/kg dosing weight.
-
If BMI >30, use 22–25 kcal/kg IBW.
-
Consider the use of a metabolic cart if accessible every week for re-assessment.
-
-
Protein needs:
-
General: 1.2–2.0 g/kg dosing weight.
-
Obesity
-
BMI of 30–40, use >2 g/kg IBW.
-
BMI >40, use >2.5 g/kg IBW.
-
-
Renal failure (HD/CRRT): 1.2–2.5 g/kg dosing weight.
-
Hepatic failure: 1.2–2.0 g/kg dosing weight.
-
-
Fluid needs—1 ml/kcal baseline.
-
Cover additional losses—(i.e., fever, diarrhea, GI output, and tachypnea).
-
Fluid restriction–CHF, renal failure, hepatic failure with ascites, CNS injury, and electrolyte abnormality.
-
If LOS >7 days and pt has not consistently met near 100 % needs consider nutritional provision from a combination of PO/EN/PN route.
Clinical Scenario
Thirty-eight-year-old male status post pancreatic necrosectomy that was performed for 75 % pancreatic necrosis 2 weeks following initial presentation for severe alcohol associated pancreatitis. He has had two additional reoperations for debridement and hemostasis over the course of 5 days, and currently has an open abdomen.
Author Response: NUTRITION MANAGEMENT IN AN OPEN ABDOMEN FOLLOWING NECROSECTOMY: Early enteral feeds. Provide EN within 24–36 h of admission to ICU, ideally with nasojejunal feeding and concurrent naso- or orogastric decompression. If nasojejunal feeding is not possible, gastric feeding can safely be attempted. Some is better than none. If the patient cannot tolerate tube feeding formula at a rate consistent with caloric goals, feeding formula should be provided at a low rate. Establish surgical feeding access as soon as it is safe to do so. A gastrojejunostomy tube is a useful adjunct for mitigating complications in this type of patient. Consider using a feeding protocol to avoid underfeeding. By postoperative day 5, if attempts to provide EN have failed, PN should be considered. Combination feeding with EN and PN should also be considered at the outset if the patient presents in a malnourished state and it is projected that adequate caloric intake with EN will not be achieved by day 5–7.
Key Questions
-
1.
When do you feed the septic patient?
-
2.
What formula should be selected, should we be focused on 24 h targets or hourly goals?
References
Cheatham ML, Safcsak K, Llerena LE, Morrow CE, Jr., Block EF. Long-term physical, mental, and functional consequences of abdominal decompression. J Trauma. 2004;56(2):237–41; Discussion. 41–2.
Cheatham ML, Safcsak K, Brzezinski SJ, Lube MW. Nitrogen balance, protein loss, and the open abdomen. Crit Care Med. 2007;35(1):127–31.
Burlew CC. The open abdomen: practical implications for the practicing surgeon. Am J Surg. 2012;204(6):826–35.
Burlew CC, Moore EE, Cuschieri J, Jurkovich GJ, Codner P, Nirula R, et al. Who should we feed? Western Trauma Association multi-institutional study of enteral nutrition in the open abdomen after injury. J Trauma Acute Care Surg. 2012;73(6):1380–7; Discussion. 7–8.
Todd SR1, Kozar RA, Moore FA. Nutrition support in adult trauma patients. Nutr Clin Pract. 2006 Oct;21(5):421–9.
Powell NJ, Collier B. Nutrition and the open abdomen. Nutrition in clinical practice: official publication of the American society for parenteral and enteral nutrition. 2012;27(4):499–506.
Marik PE. What is the best way to feed patients with pancreatitis? Curr Opin Crit Care. 2009;15(2):131–8.
Alkhawaja S, Martin C, Butler RJ, Gwadry-Sridhar F. Post-pyloric versus gastric tube feeding for preventing pneumonia and improving nutritional outcomes in critically ill adults. Cochrane Database Syst Rev. 2015;8:CD008875.
Zakaria el R, Matheson PJ, Flessner MF, Garrison RN. Hemorrhagic shock and resuscitation-mediated tissue water distribution is normalized by adjunctive peritoneal resuscitation. Journal of the American College of Surgeons. 2008;206(5):970–80; Discussion. 80–3.
Smith JW, Garrison RN, Matheson PJ, Franklin GA, Harbrecht BG, Richardson JD. Direct peritoneal resuscitation accelerates primary abdominal wall closure after damage control surgery. J Am Coll Surg. 2010;210(5):658–64, 64–7.
Smith JW, Neal Garrison R, Matheson PJ, Harbrecht BG, Benns MV, Franklin GA, et al. Adjunctive treatment of abdominal catastrophes and sepsis with direct peritoneal resuscitation: indications for use in acute care surgery. J Trauma Acute Care Surg. 2014;77(3):393–8; Discussion. 8–9.
McClave SA, Sexton LK, Spain DA, Adams JL, Owens NA, Sullins MB, et al. Enteral tube feeding in the intensive care unit: factors impeding adequate delivery. Crit Care Med. 1999;27(7):1252–6.
Heyland DK, Cahill NE, Dhaliwal R, Sun X, Day AG, McClave SA. Impact of enteral feeding protocols on enteral nutrition delivery: results of a multicenter observational study. JPEN J Parenter Enteral Nutr. 2010;34(6):675–84.
Gauglitz GG, Williams FN, Herndon DN, Jeschke MG. Burns: where are we standing with propranolol, oxandrolone, recombinant human growth hormone, and the new incretin analogs? Curr Opin Clin Nutr Metab Care. 2011;14(2):176–81.
Casaer MP, Mesotten D, Hermans G, Wouters PJ, Schetz M, Meyfroidt G, et al. Early versus late parenteral nutrition in critically ill adults. N Engl J Med. 2011;365(6):506–17.
Sena MJ, Utter GH, Cuschieri J, Maier RV, Tompkins RG, Harbrecht BG, et al. Early supplemental parenteral nutrition is associated with increased infectious complications in critically ill trauma patients. J Am Coll Surg. 2008;207(4):459–67.
Doig GS, Simpson F, Sweetman EA, Finfer SR, Cooper DJ, Heighes PT, et al. Early parenteral nutrition in critically ill patients with short-term relative contraindications to early enteral nutrition: a randomized controlled trial. JAMA. 2013;309(20):2130–8.
Harvey SE, Parrott F, Harrison DA, Bear DE, Segaran E, Beale R, et al. Trial of the route of early nutritional support in critically ill adults. N Engl J Med. 2014;371(18):1673–84.
Heidegger CP, Berger MM, Graf S, Zingg W, Darmon P, Costanza MC, et al. Optimisation of energy provision with supplemental parenteral nutrition in critically ill patients: a randomised controlled clinical trial. Lancet. 2013;381(9864):385–93.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Love, K.M., Collier, B.R. (2017). How to Feed the Open Abdomen. In: Diaz, J., Efron, D. (eds) Complications in Acute Care Surgery. Springer, Cham. https://doi.org/10.1007/978-3-319-42376-0_5
Download citation
DOI: https://doi.org/10.1007/978-3-319-42376-0_5
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-42374-6
Online ISBN: 978-3-319-42376-0
eBook Packages: MedicineMedicine (R0)