Abstract
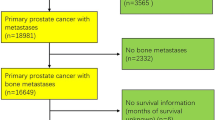
Several studies have attempted to correlate the extent of skeletal metastatic involvement, the number of bone metastases (BMTs) identified by bone scintigraphy or the distribution of BMTs (axial vs appendicular) with survival in patients with advanced prostate cancer (PC) [1, 2]. The number of BMTs has recently been evaluated as a prognostic predictor [3]. Patients with metastatic castration-resistant PC with a higher number of BMTs had a shorter progression-free survival (PFS) and overall survival (OS; hazard ratio 2.0; 95 % confidence interval 1.7–2.4). Patients with 1–4 BMTs have much better PFS and OS than those with 5–20 BMTs [4]. It should, however, be taken into account that among the predictors of prognosis, coexisting non-osseous metastatic disease is an important determinant of prognosis in patients with BMTs [5, 6].
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1.1 Distribution and Preferential Site of Bone Metastasis in Prostate Cancer Patients
Several studies have attempted to correlate the extent of skeletal metastatic involvement, the number of bone metastases (BMTs) identified by bone scintigraphy or the distribution of BMTs (axial vs appendicular) with survival in patients with advanced prostate cancer (PC) [1, 2]. The number of BMTs has recently been evaluated as a prognostic predictor [3]. Patients with metastatic castration-resistant PC with a higher number of BMTs had a shorter progression-free survival (PFS) and overall survival (OS; hazard ratio 2.0; 95 % confidence interval 1.7–2.4). Patients with 1–4 BMTs have much better PFS and OS than those with 5–20 BMTs [4]. It should, however, be taken into account that among the predictors of prognosis, coexisting non-osseous metastatic disease is an important determinant of prognosis in patients with BMTs [5, 6].
It is well known that a BMT most commonly affects the axial skeleton and that patients with BMT confined to the vertebrae have a better prognosis. Several studies have shown that the distribution and sites of predilection were similar in PC and breast cancer, with the ribs, spine and ilium reported to be those for BMT. However, recent data have shown that in early stages of breast cancer and PC the distribution in the thoracic skeleton is higher for the former than for the latter. In PC the distribution is 80 % in the spine and pelvis. In the advanced stages and in cases of extensive BMT, it seems that there are no differences in skeletal distribution between breast and PC, with a high frequency of BMT to the ribs and sternum in patients with PC as well [7, 8]. Interestingly, BMT is rarely observed in the mid-distal bones of the extremities, unlike that reported in a few other studies [9].
1.2 Pathology of Bone Metastasis from Prostate Cancer
Prostate cancer BMT is usually defined as “osteoblastic” by conventional radiographs. However, recent studies have shown a high heterogeneity of lesions, with synchronous osteolysis in BMT of PC, even when the overall character seems to be blastic [10]. Histomorphometric studies have shown that blastic lesions are mixed in nature, with increased activity of both osteoblasts and osteoclasts [11]. In bone biopsies of prostate BMT, an increase in the osteoid surface and osteoid volume and an elevation in the mineral apposition rate, demonstrating an accelerated state of bone formation, have been demonstrated. It was interesting to note that the new bone was formed in the marrow spaces and not adjacent to the bone surface; that is, the bone may form de novo in the marrow without the requirement of pre-existing bone resorption. Spindle-shaped cells or flat cells were seen lining woven osteoid and entrapped as osteocytes in the woven bone [12]. Surprisingly, well-differentiated osteoblasts, defined as cuboidal cells with basophilic cytoplasm lining the osteoid, were rarely observed on the woven bone, but they were observed in areas of bone repair secondary to bone necrosis. The osteoid is not fully mineralised and woven bone is formed, which has a low level of mineral density and a poorly organised lamellar bone. Furthermore, trabecular bone in metastatic lesions showed an increase in connectivity and surface irregularity, suggesting that strong effects of bone resorption and bone formation might occur in osteoblastic BMT [13]. In “osteoblastic” metastases osteoclasts were observed in the usual focal pattern on the surface of woven or lamellar bone or osteoid, and on the eroded surface area the number of osteoclasts was found to have greater than normal values [12]. Despite the osteoblastic nature of BMT, approximately half of 101 biopsies of BMT in bisphosphonate-naive PC patients were osteopaenic and half were osteodense, and this pattern was also reproduced in individual patients [12]. The undermineralised woven bone and the osteopaenic/osteolytic component of BMT may contribute to the histological frailty observed in the skeleton in PC patients, even in dense metastatic lesions (Fig. 1.1).
Histopathology of bone metastasis (BMT) from prostate cancer (PC). In the same patient, BMTs are heterogeneous, with predominantly blastic (1) and predominantly lytic metastases (2). Furthermore, as shown in the histopathological sections in the same specimen of a single metastasis, there is an alternation of predominantly lytic and blastic area (mixed pattern) (3): 2–20 % Bone volume: predominantly lytic area; 50–70 % bone volume: predominantly blastic area (Modified from Roudier et al. [12]). Green bone, red osteoid, grey/pink tumour stroma
Bone metastases in castration-resistant PC patients were characterised according to expression levels of steroidogenic enzyme and androgen receptor splice variants. It was found that increased tumour expression of steroidogenic enzymes in individual patients is associated with advanced tumour stage. Interestingly, there are distinct subgroups of CRPC patients with BMTs expressing high levels of AKR1C3 (that convert circulating dehydroepiandrosterone and androstenedione (synthesised in the adrenals) into 5-androstenediol and testosterone) or expressing high levels of ligand binding domain (LBD)-truncated, constitutively active androgen receptor splice variants (AR-Vs). The possible clinical relevance of this is that patients with high AKR1C3 expression and low AR-V expression may show a good response to treatment with abiraterone acetate (Cyp17 inhibition) and/or would benefit from drugs targeting AKR1C3, whereas patients with a high expression of constitutively active AR-Vs will probably not respond to abiraterone acetate or to any therapy targeting androgen synthesis or the LBD of the AR [14].
1.3 Pathophysiology of Bone Metastasis
1.3.1 Pathophysiological Heterogeneity
The osteoblastic lesion is a very complex multistep process that is not fully understood in detail. It is the result of releasing osteoblast-promoting factors such as bone morphogenetic protein (BMP), Wnt family ligand, endothelin-1 and PDGF from PC cells and of a closed interaction with bone matrix, stroma cells and bone cells. Another characteristic of BMT from PC is the biological and pathophysiological heterogeneity. The high level of heterogeneity of the BMTs in PC from the pathological point of view reflects the great complexity of the biology and molecular regulation that underlie their pathophysiology. Lytic and blastic metastases share many molecular mechanisms that give an account of similar therapeutic outcome treating them with bone-modifying agents such as zoledronic acid and denosumab. The complexity of the bone response in PC invasion is underscored by the variety of soluble factors, signalling pathways and transcriptional regulators involved. The abnormal bone response is further promoted by the potential for osteomimicry of the tumour cells signalling in a paracrine fashion within the bone environment and an autocrine signalling cascade of the bone cells themselves. These interactions between the PC cells and bone cells often yield a predominantly osteoblastic response. However, the formation of osteoblastic bone is also often associated with a significant osteolytic component, leading to a mixed, woven bone response in the same patient at different metastatic sites.
Bone remodelling proteins and transcripts in human specimens of PC BMTs were analysed in detail [15]. The main bone remodelling proteins that were recognised were assessed in lytic and blastic BMTs: BMP-2, BMP-7, dickkopf-related protein 1 (DKK-1), receptor tyrosine-protein kinase erbB-3 (ErbB3), endothelin-1 (ET-1), NEL-like protein 1 (NELL-1), tumour necrosis factor receptor superfamily 11B (OPG), phosphoglycerate kinase 1 (PGK1), sclerostin, substance P, a putative osteoblastic factor EMI domain-containing protein 1 (Emu1) and two putative osteolytic factors, matrix metalloproteinase-12 (MMP-12) and secreted frizzled-related protein 1 (SFRP1). Interestingly, many of these proteins and transcripts were equally expressed in lytic and blastic BMTs, such as BMP-2, BMP-7, DKK-1 and sclerostin. Instead, expression of some of these, such as OPG, Emu1, PGK1 and substance P, was higher in prevalent blastic lesions than in lytic lesions, but not the transcripts. OPG, PGK1 and substance P have been proven to inhibit osteoclastogenesis and induce osteoblastic differentiation. Emu1 has been shown to be prevalent in the epithelium during embryonic development and it has been hypothesised that Emu1 in PC aids adhesion The single proteins are probably not the unique drivers for conditioning the evolution towards a blastic phenotype of the metastasis, and a possible explanation for the characteristic “predominantly osteoblastic phenotype” is that PC expresses a disproportionate number of pro-osteoblastic and pro-osteolytic factors and the relative prevalence of the former will determine the pathological aspect of the lesion [15, 16].
1.3.2 The Role of Osteoclasts in Blastic and Mixed Bone Metastases
Independently from the phenotype of the lesion, osteoclasts, mainly in the first phases of BMT development, are principally responsible for the initiation, development and clinical consequences such as pain, fracture and hypercalcemia of the evident bone lesion (Fig. 1.2).
Physiopathology of blastic bone metastasis (BMT). Osteoclasts (yellow cells) reabsorbing bone facilitate the expansion of PC metastasis and make available in the bone microenvironment factors promoting penetration and growth of metastasis (TGF beta, osteopontin, FGF, PDGF, VEGF, IGF-1 and IGF-1 are described in detail in the text). In turn, PC cells express cytokines (RANKL, DKK-1 and hormone such as PTHrP) that maintain osteoclast activity and cytokine and factors such as uPA and ET-1, inducing osteoblast bone formation. In the micro-environment of a BMT site, the high bone turnover is characterised by the alternation of osteoclast (lytic) areas and osteoblastic (woven bone) areas, resulting in a disorganised and frail bone structure
Osteoclasts have two pivotal functions in the development of bone lesions: they reabsorb the bone, creating the necessary space for the penetration and development of metastasis into the bone, and they enrich, as a direct consequence of the bone matrix breakdown, the bone micro-environment of a plethora of growth factors and tumour-seeking factors that sustain the proliferation of the cancer cells, which is essential during the first phases of metastasis. These mechanisms are the basis of the “seed and soil” concept, where the bone micro-environment factors represent the fertile ground (the soil) and the “seed” represents cancer cell growth.
Physiologically, bone resorption and bone formation in skeletal remodelling are almost always tightly coupled. The bone resorption by osteoclasts is regulated by the RANK/RANKL/OPG axis, where osteoblasts expressing RANKL induce recruitment, differentiation and activation of osteoclasts, binding and activating of RANK, and conversely expressing OPG, the RANKL decoy receptor, and osteoblasts inhibit the excess osteoclastogenesis. The ratio RANKL/OPG in bone micro-environment drives the equilibrium between bone formation and resorption.
Expression of RANKL by stromal cells/osteoblasts and osteocytes is regulated by cytokines and paracrine hormones that stimulate bone resorption [17] such as interleukin-1 (IL-1), IL-6, IL-11, IL-17, prostaglandin E2 (PGE2), parathyroid hormone (PTH) and parathyroid hormone-related peptide (PTHrP), which stimulate osteoblasts or their progenitors to express RANKL and/or to downregulate the expression of OPG [18]. Recently, the role of osteocytes through the Wnt/DKK-1 and sclerostin pathway has been elucidated (Fig. 1.2) [19].
The tumour cells co-opting the normal process that regulates bone resorption interfere with the balance of the RANKL/RANK/OPG axis. The tumour/bone interface is replete with factors that stimulate bone resorption directly produced by tumour cells themselves, by macrophages and T cells associated with metastasis or by stromal cells influenced by metastasising cells. PTHrP, IL-8 and PGE2 have been shown to increase expression of RANKL and downregulate OPG expression either in vitro in the osteoblast/tumour cell coculture or in vivo using the BMT model [17–20].
Parathyroid hormone-related peptide is not physiologically present in the circulation, but it has been found to be widely distributed in most fetal and adult tissues [21], suggesting that it might act in an autocrine/paracrine manner. This peptide plays an important role in regulating many tissues including cancer tissue [22]. PTHrP is expressed by many types of cancer cells, such as breast cancer and PC, and has been proposed as an antigen for cancer immunotherapy [23–26]. PTHrP, as PTH in physiology, stimulates osteoblasts expressing PTHR1 receptor to express RANKL, which activates osteoclasts [27]. Interestingly, it has been found that T cells also express PTHR1 and are activated by PTH and PTHrP [28, 29], contributing to osteoclast activation via RANKL. It has been demonstrated that in mice bone resorption may be prevented by the immunosuppressor abatacept, a CTLA4-Ig preventing T-cell activation [30].
In addition to PTHrP, IL-8 plays an important role in the activation of osteoclasts. IL-8 is the human homologue to murine MIP-2 belonging to the family of chemokine CXC and is constitutively produced by osteoblasts [31]. IL-8 is overexpressed in the breast cancer cell line [32], and it is believed that it acts before PTHrP in the early stages of breast cancer metastasis stimulating osteoclasts via RANKL [32, 33] and then initiating the vicious cycle that maintains osteolysis in cancer metastasis. It has been suggested that IL-8 might also directly stimulate osteoclasts [33], increase angiogenesis and suppress osteoblast activity [34, 35].
Cancer cells in BMT produce many factors that activate T cells, as discussed above. T cells of patients with breast, prostate and lung cancer support osteoclastogenesis by secreting TNF alpha and expressing RANKL. In addition, T cells suppress the osteoprotegerin action secreting TRAIL (TNF-related apoptosis-inducing ligand), therefore inhibiting the anti-osteoclastogenic effect of osteoprotegerin [36]. In turn, cancer cells produce many factors such as PTHrP, IL-7 and IL-,8 which could recruit or activate T cells with the consequence of further stimulating osteoclastic bone resorption. These mechanisms contribute to the imbalance towards the osteolytic phenotype of the bone lesion.
Studies using RANKL inhibitors have shown the almost complete dependence of tumour-mediated osteoclastogenesis on RANKL. Treatment of mice with OPG-Fc prevented the progression of osteolysis induced by the breast cancer cell line MDA-MB-231 [37]. RANKL inhibition has been shown to prevent the implantation and development of osteolytic lesions in the PC3 cell line in animals [38, 39]. The efficacy of RANKL inhibition was also demonstrated in mixed BMTs in animals, where OPG-Fc blocked the establishment and progression of bone lesions [40, 41]. Recent data indicate that cathepsin G activity at the tumour–bone interface plays an important role in tumour-induced osteolysis and suggest that cathepsin G might be a potentially novel therapeutic target in the treatment of BMT. In a mouse model that mimics osteolytic changes associated with breast cancer-induced BMTs, it has recently been demonstrated that cathepsin G, cooperating with MMP9 and MMP13, is able to cut the extracellular domain of RANKL, generating active soluble RANKL, which is critical for widespread differentiation and activation of osteoclast precursors [42].
Furthermore, some RANKL-independent ways for osteoclast activation in BMT have been found. Some cancer cells, such as PC and breast cancer, may express RANKL and directly activate osteoclasts [43, 44]. Breast cancer cells, myeloma cells and other cancer cells could directly activate osteoclasts in the early stages of BMT via IL-8 production and via MIP-1, a member of the CXC chemokine family that is naturally secreted by osteoblasts and is primarily associated with cell adhesion and migration. It is chemotactic for monocytes and monocyte-like cells, including osteoclast precursors. It directly stimulates osteoclast formation and differentiation in a dose-dependent manner, through the receptors CCR1 and CCR5 expressed by osteoclasts. Moreover, neutralising antibody against MIP-1 blocks MIP-1-induced osteoclast activation [45, 46].
1.3.3 The Role of Osteoblasts in Blastic and Mixed Bone Metastases
In blastic metastases the number and activity of osteoblasts are amplified. Osteoblast differentiates from bone marrow mesenchymal stem cells. A variety of factors contribute to osteoblast formation, including insulin-like growth factor, endothelin-1, BMPs and sclerostin and Wnt proteins (Fig. 1.2) [47, 48].
1.3.4 Endothelin-1
Production of endothelin-1 (ET-1) from PC cells has proven to induce a blastic metastasis promoting osteoblast differentiation and activity. ET-1 is a small vasoconstrictive peptide that plays a key role in vascular homeostasis. ET-1 promotes osteoblast function by binding to ET receptor subtype A (ETA). The activation of receptor ETA stimulates phosphate transport and is important for the initiation of bone matrix calcification. ET-1 also increases osteoblast proliferation and inhibits osteoclast formation and motility, and recently it has been suggested that these actions might be indirect and mediated through the Wnt/DKK-1 pathway, inhibiting DKK-1 [49–51]. ET-1 can also enhance the mitogenic effect of other growth factors, such as insulin-like growth factor 1 (IGF-1), platelet-derived growth factor (PDGF) and epidermal growth factor (EGF) [52]. Furthermore, ET-1 has been found to be elevated in androgen-resistant advanced PC. However, there are some doubts with regard to the pivotal role of ET-1 in osteoblastic lesions from PC, because a clinical trial with atrasentan, a selective ET receptor antagonist, produced a modest effect on metastatic PC [53].
1.3.5 Bone Morphogenetic Proteins
The expression of several BMPs has been detected in BMTs from PC. BMPs seem to have a crucial role in contributing to osteoblastic phenotype of BMT in PC. BMPs are members of TGF-beta family and are known to be involved in cancer cell migration. In PC tissues, the expression of BMP-7 was higher in metastatic bone than in normal tissue.
The BMPs are not only expressed by osteoblasts and stored in the bone matrix, but are also actively expressed from PC cells. The osteoblastic effects of BMPs are confirmed by the expression of noggin (an antagonist of BMPs) in PC cell lines. A recent study suggests that BMP-4 signalling inducing apoptosis and Smad-mediated gene expression can be repressed by IGF-1 by activating mTOR signalling in prostate epithelial cells (NRP-152), suggesting a crosstalk between BMP and IGF signalling. It has been recently demonstrated that BMP-7 secreted from bone stromal cells induces reversible senescence in prostate cancer stem-like cells (CSCs) by activating p38 mitogen-activated protein kinase and increasing expression of the cell cycle inhibitor, p21, and the metastasis suppressor gene, NDRG1 (N-myc downstream-regulated gene 1). This effect of BMP-7 depended on BMPR2 (BMP receptor 2), and BMPR2 expression correlated inversely with recurrence and BMT in PC patients. Importantly, this effect was reversible upon withdrawal of BMP-7 [54]. Recently, it has been shown that using CaP/bone stromal cell line coculture models, one possible mechanism underlying the castration resistance induced by BMTs involves BMP-6 induction by bone stroma-derived WNT5A. BMP-6, in turn, permits CaP cells to proliferate in the absence of androgens [55].
1.3.6 Wnt/DKK-1 Pathway
Canonical Wnt proteins bind at the cell surface at a co-receptor consisting of frizzled (FZD) and low-density lipoprotein receptor-related protein 5/6 (LRP5/LRP6). The activation of the canonical pathway signal results in the stabilisation and accumulation of beta-catenin, which upon translocation into the nucleus serves as co-factor for the T-cell factor family of transcription factors [56]. Canonical Wnt signalling directly controls multiple steps of osteoblast development, regulating the fate of mesenchymal precursors by determining the commitment to a chondroblastic or osteoblastic lineage [48, 57]. Furthermore, the Wnt, indirectly dependent on the activation of beta-catenin, suppresses osteoclast recruitment and activity via osteoprotegerin (OPG). In fact, OPG is a Wnt-responsive target gene and was found to be reduced in beta-catenin knock-out osteoblasts and upregulated in cells with hyperactive Wnt signalling [48, 57]. Interestingly, a reciprocal regulation of RANKL by Wnt was observed in osteoblasts where enhanced Wnt signalling led to increased RANKL expression and vice versa [58].
The canonical Wnt pathway is regulated by a large number of antagonists, including the DKK family and secreted frizzled-related proteins (SFRPs). DKK-1 is present in mature osteoblast/osteocytes, suggesting that the Wnt/DKK-1 balance might regulate bone homeostasis [59]. DDK-1 binds the Wnt co-receptors LRP5 and LRP6 and blocks canonical Wnt signalling [60]. In the presence of DKK-1, osteoblast differentiation is impaired and Wnt-mediated suppression of osteoclast differentiation via osteoprotegerin is blocked, resulting in a dysregulation of RANKL/osteoprotegerin expression with increased osteoclast activity [61].
Direct evidence that canonical Wnt signalling participates with Wnt antagonists in adult bone biology modulating bone remodelling is also of great interest in understanding bone metastasis development and the phenotype of the single metastasis The Wnt signal has recently been found to be expressed in PC and in multiple myeloma [62, 63]. Interestingly, in early stage of PC BMT, it has been supposed that an “osteolytic phase” driven by an overexpression of DKK-1 favours tumour establishment within the bone [47] and a molecular switch with suppression of DKK-1 signal mediates the transition to an osteoblastic phase of BMT [47]. Overexpression of DKK-1 in prostate C4-2B cells changes a mixed osteolytic–osteoblastic phenotype to an osteolytic phenotype. The equilibrium between Wnt and DKK-1 expression could dictate the phenotype of BMTs and may speculatively explain the heterogeneity of histological aspects of BMTs found in individual patients or the shift from osteoblastic to osteolytic aspects in the single metastasis. Other studies suggest that non-canonical Wnt signalling also stimulates osteoblast differentiation, through BMP-dependent and BMP-independent signalling pathways [64].
1.3.7 VEGF
Vascular endothelial growth factor, as in breast cancer BMT, has been shown to be upregulated in PC and is associated with clinical stage, Gleason score, progression and survival [65, 66]. It has been recently demonstrated that osteocytes are also critical mediators in the bone metastatic niche, not only through soluble factors and cell contact but also via tumour-generated pressure [67].
1.3.8 Role of Mineralised Bone Matrix Resorption in the Vicious Cycle of Lytic Metastasis
The mineralised bone tissue contributes actively to the development and overgrowth of the metastases themselves. Bone breakdown by osteoclasts releases a variety of growth factors previously stored in proactive form by osteoblasts during the bone formation phase and physiologically destined for bone remodelling modulation and bone response to bone inflammation or trauma healing [68]. It is well known that the bone matrix represents a mine of growth factors (such as pro-cytokines); chemotactic and adhesive factors for bone cells and cancer cells, such as TGFβ, PDGF, BMPs, FGFs, IGF-1 and IGF-2; and bone matrix proteins such as osteopontin, osteocalcin, osteonectin and bone sialoprotein [69]. Interestingly, many of these factors may also be expressed actively in breast cancer and PC.
The concentration of these molecules in the micro-environment of the bone remodelling site is a critical regulator of cellular proliferation, differentiation, extracellular matrix deposition and mineralisation, is responsible for the coupling between bone resorption and bone formation and serves as survival and growth factors for cancer cells. Furthermore, physical factor such as tumour-generated pressure acting on osteocytes and factors generated during osteoclast activity, such as low oxygen content, acid pH and high extracellular calcium concentration, are combined to sustain the favourable vicious cycle of tumour growth [67, 70].
1.3.9 TGFβ
Of the growth factors stored in the bone matrix, TGFβ is not the most abundant, but has been well-studied, particularly in cancer bone disease. TGFβ binds to a heterodimeric receptor and can activate either the canonical Smad signalling pathway or Smad-independent pathways [71]. TGFβ, of all the factors delivered from bone matrix, is the major stimulator of cancer cells to express PTHrP, which is expressed in many osteolytic cancer cell lines, and its expression is higher in BMTs than in non-skeletal metastases. As a consequence of the increased PTHrP expression via TGFβ, more osteoclasts reabsorb more of the bone matrix, expanding the lytic bone lesion and increasing locally the concentration of TGFβ and other growth factors. TGFβ, as discussed above, stimulates COX-2 expression in osteoblasts, in bone marrow cells and in breast cancer cells. COX-2 expression in breast cancer cells correlates with the secretion of IL-8 and IL-11, which may induce osteoclastogenesis either via RANKL or independently of RANKL respectively. TGFβ is also reported to act on the tumour cells to induce the production of VEGF and connective tissue growth factors (CTGF) [72]. Runx2 gene expression, regulating the expression of osteopontin and metalloproteases MMP-9 and MMP-13, which are involved in bone resorption and osteoclast recruitment, may be modulated by TGFβ both in cancer cells and in osteoblasts.
1.3.10 IGF-1
The insulin-like growth factors 1 and 2 are among the most abundant non-collagen proteins in mineralised bone. Both IGFs act in cancer and in metastases promoting angiogenesis and inducing cell proliferation and cancer invasion. IGF-1 released from bone by osteoclast bone resorption binds to the type I IGF receptor (IGF-IR) on cancer cell membrane and induces the transcription factor NF-kB, which in turn stimulates target gene transcription, stimulating cancer cell proliferation and chemotaxis and inhibiting apoptosis, leading to BMTs. IGFs promote osteoblasts to increase bone matrix apposition and decrease collagen degradation [73]. IGF-1 is upregulated in PC metastases to the bone and contributes to cancer cell proliferation and chemotaxis. In clinical studies, levels of IGF also correlate with cancer progression, as high levels of IGF-1 are associated with a Gleason score 7. The protein level of IGFs and IGF-binding proteins (IGFBPs), which serve as carrier proteins for IGFs, could be mediated by proteolysis of IGFBPs. Indeed, hydrolysing IGFBPs by urokinase-type plasminogen activator (uPA) increases IGF levels and stimulates osteoblast proliferation. The cleavage of IGFBP-3 by PSA also increases IGF-1 expression, rendering IGF-1 available to bind to its receptor and stimulate osteoblast proliferation [74].
Over expression of uPA has been shown in PC cells, and uPA seems to increase metastasis to the bone. uPA is associated with an aggressive disease phenotype, progression and metastasis to the bone and can be used as a factor in the prognosis and progression of PC [75]. The cleavage of IGFBP-3 by PSA also increases IGF-1 expression, rendering IGF-1 available to bind to its receptor and stimulate osteoblast proliferation. In PC biopsies of BMTs, IGF-IR is increased. Neutralising antibodies against human IGF-1 or mouse or human IGF-2 decreases the development of bone lesions in a prostate xenograft model. Currently, taking all data together, the complex role of IGFs in BMTs phatophysiology has not yet fully elucidated [76].
Finally, it is relevant that many bone matrix-derived factors, including TGFβ, PDGF and BMPs, have the ability to induce the epithelial–mesenchymal transition of cancer cells, which greatly enhances their malignant phenotype, and therefore implicates them in the activation of dormant tumour cells [77].
References
Crawford ED, Eisenberger MA, McLeod DG, Spaulding JT, Benson R, Dorr FA, Blumenstein BA, Davis MA, Goodman PJ (1989) A controlled trial of leuprolide with and without flutamide in prostatic carcinoma. N Engl J Med 321(7):419–424
Soloway MS, Hardeman SW, Hickey D, Raymond J, Todd B, Soloway S, Moinuddin M (1988) Stratification of patients with metastatic prostate cancer based on extent of disease on initial bone scan. Cancer 61(1):195–202
Vargas HA, Wassberg C, Fox JJ, Wibmer A, Goldman DA, Kuk D, Gonen M, Larson SM, Morris MJ, Scher HI, Hricak H (2014) Bone metastases in castration-resistant prostate cancer: associations between morphologic CT patterns, glycolytic activity, and androgen receptor expression on PET and overall survival. Radiology 271(1):220–229
Tait C, Moore D, Hodgson C, Brown M, Morris T, Growcott J, Malone M, Hughes A, Renehan A, Clarke NW, Dive C (2014) Quantification of skeletal metastases in castrate-resistant prostate cancer predicts progression-free and overall survival. BJU Int 114(6b):E70–E73
Pond GR, Sonpavde G, de Wit R, Eisenberger MA, Tannock IF, Armstrong AJ (2014) The prognostic importance of metastatic site in men with metastatic castration-resistant prostate cancer. Eur Urol 65(1):3–6
Ost P, Decaestecker K, Lambert B, Fonteyne V, Delrue L, Lumen N, Ameye F, De Meerleer G (2014) Prognostic factors influencing prostate cancer-specific survival in non-castrate patients with metastatic prostate cancer. Prostate 74(3):297–305
Wang CY, Wu GY, Shen MJ, Cui KW, Shen Y (2013) Comparison of distribution characteristics of metastatic bone lesions between breast and prostate carcinomas. Oncol Lett 5(1):391–397
Kakhki VR, Anvari K, Sadeghi R, Mahmoudian AS, Torabian-Kakhki M (2013) Pattern and distribution of bone metastases in common malignant tumors. Nucl Med Rev Cent East Eur 16(2):66–69
Conti G, La Torre G, Cicalese V, Micheletti G, Ludovico MG, Vestita GD, Cottonaro G, Introini C, Cecchi M (2008) Prostate cancer metastases to bone: observational study for the evaluation of clinical presentation, course and treatment patterns. Presentation of the METAURO protocol and of patient baseline features. Arch Ital Urol Androl 80(2):59–64
Goltzman D (1997) Mechanisms of the development of osteoblastic metastases. Cancer 80(8 Suppl):1581–1587
Clarke NW, McClure J, George NJ (1991) Morphometric evidence for bone resorption and replacement in prostate cancer. Br J Urol 68(1):74–80
Roudier MP, Morrissey C, True LD, Higano CS, Vessella RL, Ott SM (2008) Histopathological assessment of prostate cancer bone osteoblastic metastases. J Urol 180(3):1154–1160
Sone T, Tamada T, Jo Y, Miyoshi H, Fukunaga M (2004) Analysis of three-dimensional microarchitecture and degree of mineralization in bone metastases from prostate cancer using synchrotron microcomputed tomography. Bone 35(2):432–438
Jernberg E, Thysell E, Bovinder Ylitalo E, Rudolfsson S, Crnalic S, Widmark A, Bergh A, Wikström P (2013) Characterization of prostate cancer bone metastases according to expression levels of steroidogenic enzymes and androgen receptor splice variants. PLoS One 8(11):e77407. doi:10.1371/journal.pone.0077407
Larson SR, Zhang X, Dumpit R, Coleman I, Lakely B, Roudier M, Higano CS, True LD, Lange PH, Montgomery B, Corey E, Nelson PS, Vessella RL, Morrissey C (2013) Characterization of osteoblastic and osteolytic proteins in prostate cancer bone metastases. Prostate 73(9):932–940
Fang J, Xu Q (2015) Differences of osteoblastic bone metastases and osteolytic bone metastases in clinical features and molecular characteristics. Clin Transl Oncol 17(3):173–179
Martin TJ (2004) Paracrine regulation of osteoclast formation and activity: milestones in discovery. J Muscoloskelet Neuronal Interact 4:243–253
Ohshiba T, Miyaura C, Inada M et al (2003) Role of RANKL induced osteoclast formation and MMP dependent matrix degradation in bone destruction by breast cancer metastasis. Br J Cancer 88:1318–1326
Dallas SL, Prideaux M, Bonewald LF (2013) The osteocyte: an endocrine cell … more. Endocr Rev 34(5):658–690
Kitazawa S, Kitazawa R (2002) RANK ligand is a prerequisite for cancer associated osteolytic lesions. J Pathol 198:228–236
Strewler GI (2000) Mechanisms of disease: the physiology of parathyroid hormone related protein. N Engl J Med 342:177–185
Falzon M, Du P (2000) Enhanced growth of MCF-7 breast cancer cells overexpressing parathyroid hormone related peptide. Endocrinology 141:1882–1892
Vargas SJ, Gillespie MT, Powell GJ et al (1992) Localization of parathyroid hormone-related protein mRA expression in metastatic lesions by in situ hybridization. J Bone Miner Res 7:971–980
Kohno N, Kitazawa S, Fukase M et al (1994) The expression of parathyroid hormone related protein in human breast cancer with skeletal metastases. Surg Today 24:215–220
Arima Y, Matsueda S, Yano H et al (2005) Parathyroid hormone related protein as a common target molecule in specific immunotherapy for a wide variety of tumour types. Int J Oncol 27:981–988
Yao A, Harada A, Matsueda S et al (2005) New epitope peptides derived from parathyroid hormone related protein which have the capacity to induce prostate cancer reactive cytotoxic T-lymphocytes in HLA-A2* prostate cancer patients. Prostate 62:233–242
Karaptis AC, Goltzman D (2000) PTH PTHrP effects on the skeleton. Rev Endocr Metab Disord 1:331–341
Yamamoto I, Bringhurst FR, Potts JT et al (1988) Properties of parathyroid hormone receptors on circulating bovine lymphocytes. J Bone Miner Res 3:289–295
Atkinson MJ, Hesch RD, Cade C et al (1987) Parathyroid hormone stimulation of mitosis in rat thymic lymphocytes is independent of cyclic AMP. J Bone Miner Res 2:303–309
Wu X, Qian W, Ryan M et al (2005) Continuous PTH treatment causes bone loss through upregulated T cell localization to the bone surfaces. J Bone Miner Res 20(Suppl 1):S14
Graves DT, Jiang Y, Valente AJ (1999) The expression of monocyte chemoattractant protein 1 and other chemokines by osteoblasts. Front Biosci 4:571–580
Bendre M, Gaddy-Kurten D, Foote-Mon T et al (2006) Expression of interleukin 8 and not parathyroid hormone related protein by human breast cancer cells correlates with bone metastasis in vivo. Cancer Res 66:2250–2256
Bendre M, Montague D, Peery T et al (2003) Interleukin 8 stimulation of osteoclastogenesis and bone resorption is a mechanism for the increased osteolysis of metastatic bone disease. Bone 33:28–37
Guise TA, Chirgwin JM (2003) Transforming growth factor beta in osteolytic breast cancer bone metastases. Clin Orthop Relat Res 4155:532–538
Dovio A, Sartori ML, Masera RG et al (2004) Effects of physiological concentration of steroid hormones and interleukin 11 on basal and stimulated production of interleukin 8 by human osteoblast like cells with different functional profiles. Clin Exp Rheumatol 22:79–84
Founier P, Chirgwin JM, Guise T (2006) New insights into the role of T cells in the vicious cycle of bone metastases. Curr Opin Rheumatol 18(4):396–40410.1097/01.bor.0000231909.35043.da
Kostenuik PJ, Bolon B, Morony S et al (2004) Gene therapy with human recombinant osteoprotegerin reverses established osteopenia in ovariectomized mice. Bone 34(4):656–64
Whang PG, Schwarz EM, Gamradt SC et al (2005) The effects of RANK blockade and osteoclast depletion in a model of pure osteoblastic prostate cancer metastasis in bone. J Orthop Res 23:1475–1483
Miller R, Jones J, Tometsko M et al (2005) Antituomour efficacy of the RANK ligand inhibitor OPG-Fc in the MDA-231 breast cancer and PC3 prostate cancer experimental osteolytic metastases models. J Bone Miner Res 20(Suppl 1):S117
Yonou H, Kanomata N, Goya M et al (2003) Osteprotegerin/osteoclastogenesis inhibitory factor decreases human prostate cancer burden in human adult bone implanted into nonobese diabetic/sever combined immunodeficient mice. Cancer Res 63:2096–2102
Zhang J, Dai J, Qi Y et al (2001) Osteoprotegerin inhibits prostate cancer induced osteoclastogenesis and prevents prostate tumour growth in the bone. J Clin Invest 107:1235–1244
Wilson TJ, Nannuru KC, Futakuchi M, Sadanandam A, Singh RK (2008) Cathepsin G enhances mammary tumor-induced osteolysis by generating soluble receptor activator of nuclear factor-kappaB ligand. Cancer Res 68(14):5803–5811
Brown J, Corey E, Lee Z et al (2001) Osteoprotegerin and rank ligand expression in prostate cancer. Urology 57:611–616
Farrugia AN, Atkins GJ, To L et al (2003) Receptor activator of nuclear factor kappaB ligand expression by human myeloma cells mediates osteoclast formation in vitro and correlates with bone destruction in vivo. Cancer Res 63:5438–5445
Terpos E, Dimopoulos MA (2005) Myeloma bone disease: pathophysiology and management. Ann Oncol 16:1223–1231
Choi SJ, Oba Y, Gazitt Y et al (2001) Antisense inhibition of macrophage inflammatory protein 1 alpha blocks bone destruction in a model of myeloma bone disease. J Clin Invest 108:1833–1841
Hall CL, Keller ET (2006) The role of Wnts in bone metastases. Cancer Metastasis Rev 25:551–558
Hall CL, Kang S, Macdougald OA et al (2006) Role of Wnts in prostate cancer bone metastases. J Cell Biochem 97:661–672
Clines GA, Mohammad KS, Bao Y, Stephens OW, Suva LJ, Shaughnessy JD Jr, Fox JW, Chirgwin JM, Guise TA (2007) Dickkopf homolog 1 mediates endothelin-1-stimulated new bone formation. Mol Endocrinol 21(2):486–498
Chiao JW, Moonga BS, Yang YM, Kancherla R, Mittelman A, Wu-Wong JR, Ahmed T (2000) Endothelin-1 from prostate cancer cells is enhanced by bone contact which blocks osteoclastic bone resorption. Br J Cancer 83:360–365
Yin JJ, Mohammad KS, Kakonen SM, Harris S, Wu-Wong JR, Wessale JL, Padley RJ, Garrett IR, Chirgwin JM, Guise TA (2003) A causal role for endothelin-1 in the pathogenesis of osteoblastic bone metastases. Proc Natl Acad Sci U S A 100:10954–10959
Nelson JB, Chan-Tack K, Hedican SP, Magnuson SR, Opgenorth TJ, Bova GS, Simons JW (1996) Endothelin-1 production and decreased endothelin B receptor expression in advanced prostate cancer. Cancer Res 56:663–668
Russo A, Bronte G, Rizzo S, Fanale D, Di Gaudio F, Gebbia N, Bazan V (2010) Anti- endothelin drugs in solid tumors. Expert Opin Emerg Drugs 15:27–40
Kobayashi A, Okuda H, Xing F, Pandey PR, Watabe M, Hirota S, Pai SK, Liu W, Fukuda K, Chambers C, Wilber A, Watabe K (2011) Bone morphogenetic protein 7 in dormancy and metastasis of prostate cancer stem-like cells in bone. J Exp Med 208(13):2641–2655
Lee GT, Kang DI, Ha Y-S, Jung YS, Chung J, Min K, Kim TH, Moon KH, Chung JM, Lee DH, Kim W-J, Kim IY (2014) Prostate cancer bone metastases acquire resistance to androgen deprivation via WNT5A-mediated BMP-6 induction. Br J Cancer 110(6):1634–1644
Van de WM, Cavallo R, Dooijes D et al (1997) Armadillo coactivates transcription driven by the product of the Drosophila segment polarity gene dTCF. Cell 88:789–799
Day TF, Guo X, Garrett-Beal L et al (2005) Wnt/β-catenin signalling in mesenchymal progenitors controls osteoblast and chondrocyte differentiation during vertebrate skeletogenesis. Dev Cell 8:739–750
Glass DA, Bialek P, Ahn JD et al (2005) Canonical Wnt signalling in differentiated osteoblasts controls osteoclast differentiation. Dev Cell 8:751–764
Zhang Y, Wang Y, Li X et al (2004) The LRP 5 high-bone-mass G171V mutation disrupts LRP5 interaction with Mesd. Mol Cell Biol 24:4677–4684
Bafico A, Liu G, Yaniv A et al (2001) Novel mechanism of Wnt signalling inhibition mediated by Dikkopf 1 interaction with LRP6/Arrow. Nat Cell Biol 3:683–686
MacDonald BT, Joiner D, Oyserman S et al (2007) Bone mass is inversely proportional to DKK1 levels in mice. Bone 41:331–339
Pearse R (2006) Wnt antagonism in multiple myeloma: a potential cause of uncoupled bone remodelling. Clin Cancer Res 12(Suppl 20):6274S–6278S
Rosol TJ, Tannehill-Gregg SH, Corn S et al (2004) Animal models of bone metastasis. Cancer Treat Res 118:47–81
Dai J, Hall CL, Escara-Wilke J, Mizokami A, Keller JM, Keller ET (2008) Prostate cancer induces bone metastasis through Wnt-induced bone morphogenetic protein-dependent and independent mechanisms. Cancer Res 68:5785–5794
Rahim F, Hajizamani S, Mortaz E, Ahmadzadeh A, Shahjahani M, Shahrabi S, Saki N (2014) Molecular regulation of bone marrow metastasis in prostate and breast cancer. Bone Marrow Res 2014:405920
Roberts E, Cossigny DA, Quan GM (2013) The role of vascular endothelial growth factor in metastatic prostate cancer to the skeleton. Prostate Cancer 2013:418340
Sottnik JL, Dai J, Zhang H, Campbell B, Keller ET (2015) Tumor-induced pressure in the bone microenvironment causes osteocytes to promote the growth of prostate cancer bone metastases. Cancer Res 75(11):1–8
Monolagas SC, Jilka RL (1995) Bone marrow, cytokines and bone remodelling. N Engl J Med 332:305–311
Dallas SL, Rosser JL, Mundy GR et al (2002) Proteolysis of latent tranforming growth factor beta binding protein1 by osteoclasts. A cellular mechanism for release of TGF beta from bone matrix. J Biol Chem 277:21352–21360
Liao J, Schneider A, Datta NS, McCauley LK (2006) Extracellular calcium as a candidate mediator of prostate cancer skeletal metastasis. Cancer Res 66(18):9065–9073
Javelaud D, Alexaki VI, Dennler S, Mohammad KS, Guise TA, Mauviel A (2011) TGF-β/SMAD/GLI2 signaling axis in cancer progression and metastasis. Cancer Res 71(17):5606–5610
Wakefield LM, Hill CS (2013) Beyond TGFβ: roles of other TGFβ superfamily members in cancer. Nat Rev Cancer 13(5):328–341
Lee HL, Pienta KJ, Kim WJ, Cooper CR (2003) The effect of bone-associated growth factors and cytokines on the growth of prostate cancer cells derived from soft tissue versus bone metastases in vitro. Int J Oncol 22(4):921–926
Bogdanos J, Karamanolakis D, Tenta R, Tsintavis A, Milathianakis C, Mitsiades C, Koutsilieris M (2003) Endocrine/paracrine/autocrine survival factor activity of bone microenvironment participates in the development of androgen ablation and chemotherapy refractoriness of prostate cancer metastasis in skeleton. Endocr Relat Cancer 10(2):279–289
Wang N, Docherty FE, Brown HK, Reeves KJ, Fowles AC, Ottewell PD, Dear TN, Holen I, Croucher PI, Eaton CL (2014) Prostate cancer cells preferentially home to osteoblast-rich areas in the early stages of bone metastasis: evidence from in vivo models. J Bone Miner Res 29(12):2688–2696
Rubin J, Fan X, Rahnert J et al (2006) IGF1 secretion by prostate carcinoma cell does not alter tumor bone cell interactions in vitro or in vivo. Prostate 66:789–800
Morrison CD, Parvani JG, Schiemann WP (2013) The relevance of the TGF-β Paradox to EMT-MET programs. Cancer Lett 341(1):30–40
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Bertoldo, F. (2017). Biology and Pathophysiology of Bone Metastasis in Prostate Cancer. In: Bertoldo, F., Boccardo, F., Bombardieri, E., Evangelista, L., Valdagni, R. (eds) Bone Metastases from Prostate Cancer . Springer, Cham. https://doi.org/10.1007/978-3-319-42327-2_1
Download citation
DOI: https://doi.org/10.1007/978-3-319-42327-2_1
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-42326-5
Online ISBN: 978-3-319-42327-2
eBook Packages: MedicineMedicine (R0)