Abstract
Mechanical ventilation (MV) has saved countless lives. Since MV was introduced, it is the primary therapy for respiratory failure and a fundamental treatment in intensive care units. Whether MV is used during a surgical procedure or to treat respiratory failure, it is generally a time-limited therapy that, when withdrawn, has no untoward sequelae. However, there are a number of patients who become dependent on MV. These patients, often referred to as “failure to wean” (FTW), present a significant physiologic and economic burden to the healthcare system.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Spinal Cord Injury
- Phrenic Nerve
- Functional Electrical Stimulation
- Spinal Cord Injury Patient
- Diaphragm Muscle
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Introduction
Mechanical ventilation (MV) has saved countless lives. Since MV was introduced, it is the primary therapy for respiratory failure and a fundamental treatment in intensive care units. Whether MV is used during a surgical procedure or to treat respiratory failure, it is generally a time-limited therapy that, when withdrawn, has no untoward sequelae. However, there are a number of patients who become dependent on MV. These patients, often referred to as “failure to wean” (FTW), present a significant physiologic and economic burden to the healthcare system.
FTW patients arise from those who required “prolonged” MV (PMV), defined as greater than 96 h of MV. Patients on PMV or FTW have longer hospital days (median 17 days vs. 6), higher comorbidities, poor functional outcomes, and increase cost [1]. Damuth reviewed worldwide data of PMV patients with 124 studies ultimately included in results. This report showed a 1-year mortality of 58 % in ICU patients. Only 50 % of patients were ever liberated from mechanical ventilation [2]. Additional reports have mortality ranging from 20 to 50 %. The 1-year functional outcomes in PMV patients demonstrate only 9 % being able to perform activities of daily living independently. Conversely, 65 % were completely dependent on others. PMV incur substantially greater hospital costs than patients who are able to wean, with 1-year survival costs averaging $306,000.00 US dollars. The number of patients requiring PMV is growing 5.5 % annually, 4.4 % higher than the total hospital admission growth rate. It is estimated that by the year 2020, there will be 605,000 patients requiring PMV with hospital costs of $64 billion.
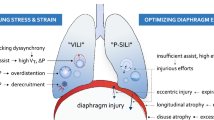
Multiple medical conditions, such as heart failure, severe respiratory disease, critical illness neuropathy, and respiratory muscle weakness, can lead to PMV. In addition to medical etiologies, MV has its own deleterious effects. Positive pressure MV leads to inactivity of the diaphragm muscle, causing atrophy and weakness. Because the diaphragm is the primary inspiratory muscle, ventilator-induced diaphragm dysfunction (VIDD) is widely recognized as a major contributing factor to FTW [3]. For this chapter, it will be important to remember the diaphragm is innervated by the phrenic nerve, composed of nerve roots from cervical level 3 to 5.
High level spinal cord injury (SCI) is another condition that lends itself to PMV. Approximately 4 % of the 12,000 SCI patients per year in the USA require chronic long-term MV. Respiratory complications are the leading cause of death in SCI, with pneumonia being the leading cause of death in those on MV. Patients with the same level of injury who require MV have significantly shorter life spans. Chronic long-term MV is associated with increased anxiety for both patient and caregiver. It alters speech patterns, decreases sense of smell, adds bulk and weight to wheelchairs, and impedes mobility, and noise and tubing attract unwanted attention [3]. The presence of a tracheostomy increases secretions and may cause tracheal malacia and tracheal erosion.
Surgical Intervention with Diaphragm Pacing
Diaphragm pacing (DP) was developed to provide natural negative pressure ventilation in SCI patients on PMV. DP involves laparoscopically placed electrodes at the motor point of each hemidiaphragm where stimulation provides maximal contraction of the diaphragm. Essentially, DP electrically stimulates intact lower motor units in the spinal column replacing the upper motor neuron signal. It has been shown to decrease, delay, or replace MV.
Surgical implantation of DP begins with patients receiving deep vein thrombosis prophylaxis through sequential compression devices and appropriate warming apparatuses. General anesthesia is administered without neuromuscular blocking agents. Short-acting agents such as propofol for amnesia and remifentanil for pain along with inhalation agents are the preferred anesthetic management for patients undergoing DP [4]. Standard four-port laparoscopy begins with generous amounts of preemptive local anesthetic being placed into the incisions to decrease pain and intraoperative spasms. The abdomen is insufflated, and the falciform ligament is divided allowing easier access of the implant instruments to the diaphragm. Then a 12-mm epigastric port is placed for the implant instrument and to provide an unimpeded exit for the pacing electrodes.
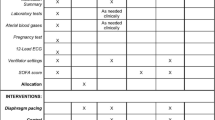
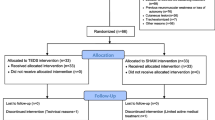
The next step of DP surgery is mapping of the diaphragm. This process identifies the motor point. The tip of a laparoscopic dissector is touched against the diaphragm muscle (Fig. 12.1 a, b). A twitch stimulus is delivered from a clinical station to the instrument, and both qualitative and quantitative data are obtained. Quantitatively, changes in abdominal pressure are measured through tubing that is attached to one of the surgical ports and connected to the clinical station. A greater change in pressure indicates closer proximity to the motor point of the phrenic nerve and a larger diaphragm muscle contraction. Qualitatively, visual observation of the diaphragm is made during stimulation.
(a) The laparoscopic dissector is placed against the right diaphragm, an electrical burst from the clinical station externally will allow contraction if the phrenic nerve is intact, and subsequent mapping will show ideal location for implantation; (b) the diaphragm has a diffuse but weak contraction which will improve with diaphragm conditioning
The area of electrode placement is chosen based on location of larger contraction with strong preference for the posterior diaphragm to facilitate posterior lung lobe ventilation that will decrease atelectasis. Two electrodes are then implanted into the right and left diaphragm muscle. Placement of two electrodes in each diaphragm provides redundancy and synergy for maximal muscle recruitment. The electrodes are implanted using an implant instrument (Fig. 12.2 a, b). The electrode is threaded through the instrument to the tip of the needle. The needle at the end of the instrument is skived into the muscle, and the polypropylene barb on the end of the electrode releases upon withdrawal of the needle. The four electrodes and an anode are then tunneled subcutaneously to an appropriate exit site. A chest x-ray is taken at the end of the case to assess for the presence of a capnothorax that may result from carbon dioxide tracking from the abdominal cavity into the pleural space from the diaphragm. Small capnothoraxes resolve spontaneously where a larger one may need to be aspirated [5].
(a) The implant instrument houses the diaphragm pacing electrode which is a double helix of 14 stainless steel wires that are Teflon coated. The needle of the implant instrument enters the diaphragm muscle and a polypropylene barb allows the electrode to be fixated. (b) Two electrodes in the left diaphragm
The implanted intramuscular electrodes are connected to a four-channel external pulse generator (EPG) (Fig. 12.3). This stimulator provides capacitively coupled charge-balanced biphasic stimulation to each subcutaneous electrode. The EPG is programmed with patient-specific parameters of pulse amplitude, pulse duration, inspiratory time, pulse rate, and respiratory rate by a clinician. DP users simply connect and turn the device on and/or off. The maximal settings for patient safety are 25 mA for amplitude, 200 for pulse width, and 20 for Hz. Patients should never exceed these parameters [5]. The goal for patient settings is to use the highest settings within the safety parameters that do not cause any patient discomfort.
Once implanted, the device can be utilized immediately to begin diaphragm conditioning. Each patient should have a customized conditioning program that entails initiation of DP use which gradually increases over time. Patients often begin with 30 min of DP use several times daily and increase usage every 3–5 days [3, 5]. DP conditioning will convert the atrophied muscle fibers from fast-fatigable type 2B muscle fibers to slow-twitch type 1.
Results of Diaphragm Pacing
The initial FDA multicenter clinical trial of DP in SCI dependent on tracheostomy MV showed 100 % of implanted patients were able to breathe for four consecutive hours with DP alone. Over 50 % of patients utilized DP for over 24 h of continuous use. The patients ranged in age from 18 years to 74 years (36 years old average). There were 37 males with the majority of injuries resulting from motor vehicle accidents followed by sports injuries. Patients were on PMV from 3 months to 27 years prior to DP implant with the average time of injury to implant being 5.6 years. This trial reports no pneumonia deaths.
Another study done with DP in SCI but focused on SCI patients who had a permanent internal cardiac pacemaker was completed in 2010. The study included 20 SCI patients who had both cardiac pacemaker and DP. This study also showed all patients were able to achieve tidal volumes to meet their basic metabolic needs with 71 % able to replace MV with DP full time. The internal cardiac pacemakers were interrogated at the time of DP implant with DP being set at maximal stimulation settings and the cardiac pacemakers being set at their most sensitive. No device interactions were noted [6].
DP has been implanted successfully in pediatric patients. A report of six pediatric SCI patients ranging in age 3–17 years (average age 9 years old) with an average weight of 32.6 kg was successfully implanted with no technical difficulties. Unique to the pediatric population is growth that may require DP reprogramming and scoliosis, which may need to be addressed prior to implantation and/or may affect ventilator weaning. Pediatric patients experienced the same success with being liberated from MV as their adult counterparts [7].
More recent and exciting data on DP in the SCI population was published in 2014 [8]. This study focused on early implantation of DP. Their analysis included 29 patients, 22 of whom were implanted and 7 patients had denervated “dead diaphragms” at surgery. The average time frame of injury to implant was 3–112 days with a median of 33 days. Seventeen percent of patients were weaned completely off MV in an average of 13.1 days. A subset of patients implanted within 11 days of injury weaned off MV in 5.7 days. Some patients (36 %) implanted early after injury had recovery of respiration and were able to wean off of DP. This study highlighted the potential of electrical stimulation from DP and neuroplasticity of the spinal cord allowing recovery of phrenic nerve function. Also noteworthy was the fact that early identification of those patients with “dead diaphragms” will save significant amounts of time, frustration, and money on futile ventilator weaning and also allow early consideration of the growing use of nerve transfer techniques to allow recovery.
Recent uses of DP expanded from SCI to diaphragm dysfunction. DD can be either unilateral or bilateral with varying degrees of symptomatology ranging from asymptomatic to respiratory failure requiring mechanical ventilation. Onders reported the use of DP in a group of 21 patients. The study identified six patients with non-stimulable diaphragms at surgery. Of note, preoperative testing, which included radiographic exams, phrenic nerve conduction studies, and pulmonary testing, showed no statistical difference between the two groups. Ten of the implanted patients had false-negative phrenic nerve conduction studies with no measurable muscle action potentials. The average duration of symptoms for those implanted was 41 months compared to 22 months in the non-stimulable group. Four patients were on tracheostomy mechanical ventilation. Diaphragm dysfunction was a result of phrenic nerve injury from thoracic surgery, shoulder surgery, idiopathic and one spinal muscle atrophy (SMA), one Charcot-Marie-Tooth disease, and one diaphragm flutter (belly dancer syndrome). Sixty-two percent had clinically relevant improvements in respiration. All four mechanically ventilated patients were weaned off tracheostomy mechanical ventilation and ultimately decannulated and weaned off DP with electrodes removed. Two people decreased noninvasive ventilation use; two were weaned off oxygen therapy and two had resolution of paradoxical motion of the diaphragms and three additional patients having improved diaphragms on chest x-ray. Using an adapted cable, the implanted DP electrodes were used to assess diaphragm electromyographic activity that not only allowed for identification of abnormalities such as central apneas but also provided an avenue for monitoring of diaphragm recovery [9].
Conclusion
Prolonged mechanical ventilation is a significant and growing healthcare predicament. DP has been successfully used in SCI to replace or decrease mechanical ventilation. Early implantation of DP has substantial benefits and no known drawbacks. The more recent utilization of DP in DD is a foundation for DP to be used in critical care units. Duplication of the success of DP in weaning patients from tracheostomy mechanical ventilation would change the paradigm of therapy in intensive care units.
References
Criner G. Long-term ventilator dependent patients: new facilities and new models of care. The American perspective. Port Rev Pneumol. 2012;18:214–6.
Damuth E, Mitchell J, Bartock B, Roberts B, Treciak S. Long-term survival of critically ill patients treated with prolonged mechanical ventilation: a systematic review and met-analysis. Lancet Resp Med. 2015;3:544–53.
Elmo M, Kaplan C, Onders R. Diaphragm pacing: helping patients breathe. AANLCP J Nurse Life Care Plann. 2012;12:600–11.
Onders RP, Carlin AM, Elmo MJ, Sivashankaran S, Katirji B, Schilz R. Amyotrophic lateral sclerosis: the Midwestern surgical experience with diaphragm pacing stimulation system shows that general anesthesia can be safely performed. Am J Surg. 2009;197:386–90.
Onders RP, Elmo M, Khansarinia S, Bowman B, Yee J, Road J, Bass B, Dunkin B, Ingvarsson PE, Oddsdottir M. Complete worldwide experience in laparoscopic diaphragm pacing: results and differences in spinal cord injured patients and amyotrophic lateral sclerosis patients. Surg Endosc. 2009;23:1433–40.
Onders RP, Khansarinia S, Weiser T, Chin C, Hungness E, Soper N, DeHoyos A, Cole T, Ducko C. Multi-center analysis of diaphragm pacing in tetraplegic with cardiac pacemakers: positive implications for ventilator weaning in intensive care units. Surgery. 2010;148:893–7.
Onders RP, Ponsky TA, Elmo MJ, Lidsky K, Barksdale E. First reported experience with intramuscular diaphragm pacing in replacing positive pressure mechanical ventilators in children. J Pediatr Surg. 2011;46:72–6.
Posluszny JA, Onders R, Kerwin AJ, Weinstein MS, Stein DM, Knight J, Lottenberg L, Cheatham ML, Khansarinia S, Dayal S, Byeno PM. Multicenter review of diaphragm pacing in spinal cord injury: successful not only in weaning from ventilators but also in bridging to independent respiration. J Trauma Acute Care Surg. 2014;76:303–10.
Onders R, Elmo MJ, Kaplan C, Katirji B, Schilz R. Extended use of diaphragm pacing in patients with unilateral of bilateral diaphragm dysfunction: a New therapeutic option. Surgery. 2014;156:772–86.
Conflict of Interest Disclosure
Dr. Raymond Onders, University Hospitals of Cleveland, and Case Western Reserve University School of Medicine have intellectual property rights involved with the diaphragm pacing system and equity in Synapse Biomedical who manufactures the device.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Onders, R.P. (2017). Recovery of Diaphragm Function Through Functional Electrical Stimulation: Diaphragm Pacing. In: Elkwood, A., Kaufman, M., Schneider, L. (eds) Rehabilitative Surgery. Springer, Cham. https://doi.org/10.1007/978-3-319-41406-5_12
Download citation
DOI: https://doi.org/10.1007/978-3-319-41406-5_12
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-41404-1
Online ISBN: 978-3-319-41406-5
eBook Packages: MedicineMedicine (R0)