Abstract
Stenotrophomonas maltophilia is an emerging opportunistic pathogen with an environmental origin. One of the most cumbersome characteristics of S. maltophilia is its natural low susceptibility to different antimicrobial agents that are currently in use in the clinical practice. Because of that, this species is considered as a prototype of intrinsically resistant microorganism. Part of its capability to resist the action of antimicrobials resides in a number of chromosomally encoded efflux pumps. Notably, overexpression of some of these efflux pumps can confer clinically relevant resistance to quinolones. This is likely the reason why, in contrast to other pathogens, no S. maltophilia-resistant isolates have been found presenting mutations in the genes encoding bacterial topoisomerases. Along this chapter, we describe different efflux pumps that have been so far reported in S. maltophilia as well as the mechanisms that allow their regulation. The clinical relevance these efflux pumps may have for the success of S. maltophilia in producing infections in patients is also discussed. Finally, we focus on the function that efflux pumps may have in the adaptation of S. maltophilia to nonclinical ecosystems, such as rhizosphere, where antimicrobial selective pressure is likely low.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Stenotrophomonas maltophilia is an opportunistic pathogen with an environmental origin, which is considered to be a prototype of a bacterium intrinsically resistant to antimicrobial agents [1, 2]. Before the wide use of antimicrobial agents, most opportunistic pathogens were species belonging to the commensal microbiota capable of colonizing previously debilitated patients. Whereas commensals are still responsible for a large fraction of nosocomial infections, bacteria with an environmental origin, such as Pseudomonas aeruginosa, Acinetobacter baumannii, or S. maltophilia, also constitute a problem in habitats, such as hospitals hosting immunosuppressed patients [3], patients with a basal disease or needing care after a surgery, and generally speaking, debilitated patients. This situation, in which the host response to infection is too weak to avoid a disease, allows different organisms to colonize a human host that otherwise will not be infected. In the presence of immune system deficiency, the most important line of defense consists of the use of antimicrobials, and, in this context of high antimicrobial load, only antimicrobial-resistant organisms are able to produce an infection, despite their reduced virulence. One of these types of microorganisms is S. maltophilia, which is not highly virulent but is an increased cause of infections in hospitals and in people suffering from cystic fibrosis [4]. The reason behind is likely its low susceptibility to antimicrobial agents currently in clinical use. Indeed, one of the risk factors for being infected by S. maltophilia is a previous treatment of a patient with antimicrobial drugs.
Reasons for the reduced susceptibility to different antimicrobials are multifaceted. S. maltophilia, as other Gram-negative non-fermenting bacteria, presents a reduced membrane permeability, which precludes the fast and easy entrance of antimicrobial agents. In addition, the chromosome of S. maltophilia contains several genes coding for proteins that contribute to its resistance to several drugs. Among them, it is important to highlight two β-lactamases (including a metalloenzyme) that are capable of inactivating penicillins, cephalosporins, and/or carbapenems [5, 6]; two aminoglycoside-modifying enzyme genes, aph(3′)-IIc encoding an aminoglycoside phosphotransferase [7] and aac(6′)-Iz coding for an N-aminoglycoside acetyltransferase [8, 9], which can inactivate most aminoglycosides; one quinolone-resistantce protein (SmQnr) [10–12]; and several efflux pumps, belonging to different families of transporters [13], which altogether constitute one of the most important mechanisms of antimicrobial resistance in S. maltophilia [1].
Since S. maltophilia is not a producer of antibiotics used in clinics for treating human infections, such as β-lactams or aminoglycosides, it is intriguing to know the reasons why this bacterial species presents such a wide range of antimicrobial resistance determinants. Two possibilities (not necessarily mutually exclusive another) may explain this situation: (i) given that S. maltophilia colonizes the rhizosphere, it can encounter there a dense bacterial population (including antibiotic producers) and needs to present elements for avoiding the inhibitory activity of competitors; (ii) as proposed for different antimicrobial resistance determinants, their function in nature, an environment where the antimicrobial load is not high, is likely not to provide resistance to the inhibitory action of antimicrobials [14–17]. As described below, this can be the situation of the SmeDEF efflux pump which seems to be involved in the colonization of the roots of the plants [18]. In the current chapter, we discuss the relevance of S. maltophilia efflux pumps for the acquisition of resistance to clinically relevant antimicrobial drugs, as well as the role these efflux pumps may have in other bacterial processes.
2 Characterization of Efflux Pumps in S. maltophilia
The efflux pump of S. maltophilia, SmeDEF, was described in 2000 [19]. Later on, in 2002, the efflux pump SmeABC was also described [20], and in 2008 the sequencing of complete genome of S. maltophilia K279a strain [13] allowed the identification of genes encoding several multidrug transporters belonging to three different superfamilies of transporters: the chromosome of S. maltophilia contains genes coding for eight multidrug resistance (MDR) efflux pumps belonging to resistance-nodulation-cell division (RND) superfamily, three efflux pumps belonging to the major facilitator superfamily (MFS), and two ATP-binding cassette (ABC) superfamily pumps [13]. After their first identification, different studies aimed to characterize them in detail, in particular their role in antimicrobial resistance, but also their involvement in resistance to biocides as well as their role in other cellular processes, including the colonization of plant hosts and the response to stress.
2.1 RND Efflux Pumps
The structure of S. maltophilia RND efflux pumps is the same as for other members of the superfamily. These efflux pumps form a tripartite complex composed of three proteins: an inner membrane protein, an RND transporter that binds and translocates substrates, an outer membrane protein (OMP), and a membrane fusion protein (MFP), which links the outer and inner membrane proteins in the periplasmic space. In general, the genes encoding the three efflux pump proteins are located in the same operon, with some exceptions in which the operon does not contain the OMP (Fig. 15.1). In other Gram-negative bacteria, when the OMP is not encoded in the same operon, the substrates can be extruded to the periplasmic space and leave the bacteria through an OMP encoded elsewhere on the chromosome, which is recruited to form a tripartite pump. For instance, the P. aeruginosa MexXY efflux pump can accommodate OprM [21, 22], whose gene is located in the operon encoding MexAB-OprM [23]. Usually, located upstream and divergently transcribed from the efflux pump operon are gene(s) encoding for a transcriptional regulator protein [24] or a two-component regulatory system [20]. Expression of these efflux pumps is tightly downregulated by such regulators, and high expression levels can be achieved either in the presence of an inducer or upon mutations of the regulators.
RND operons in S. maltophilia. Operons containing RND genes and the genes for their local regulators are represented. The same figure is used for genes codifying for proteins with the same function, as detailed in the figure. RND genes are smeB, smeE, smeH, smeJ, smeN, smeP, smeW, and smeZ. Adjacent membrane fusion protein (MFP) genes and outer membrane protein (OMP) genes are shown. Genes encoding local regulatory proteins, as well as their DNA regulatory regions (Reg. Region) containing promoters and operator regions, are shown. Asterisks (*) indicate operons whose role in antimicrobial resistance has not been proven yet
Six of the eight RND efflux pumps identified in the S. maltophilia chromosomal sequence have been functionally characterized, SmeABC, SmeDEF, SmeIJK, SmeOP, SmeVWX, and SmeYZ (Table 15.1), while the putative role of SmeGH and SmeMN in antimicrobial resistance remains unknown. Among them, SmeDEF, SmeIJK, SmeOP, and SmeYZ, as well as the ABC efflux pump MacABCsm (see below), have shown to have a role in intrinsic resistance to different compounds (Table 15.1). The overexpression of SmeABC provides resistance to ß-lactams, aminoglycosides, and quinolones, although only the deletion of the OMP of the system, SmeC, has an effect in the susceptibility to several antimicrobial drugs [20]. This may suggest that the observed effect is not due to the efflux pump itself but of another efflux pump that can make use of SmeC for its activity in extruding antibiotics. SmeDEF has an important role in susceptibility to chloramphenicol, tetracycline, quinolones, and cotrimoxazole, as well as to biocides such as triclosan [28, 35–38]. When overexpressed, the efflux pump SmeVWX is mainly involved in acquired resistance to chloramphenicol and quinolones [28, 29]. The efflux pump SmeOP confers low susceptibility to aminoglycosides, nalidixic acid, doxycycline, and macrolides, as well as to some nonantibiotic compounds, such as carbonyl cyanide n-chlorophenylhydrazone (CCCP), crystal violet, sodium dodecyl sulfate, and tetrachlorosalicylanilide. However its overexpression only alters the susceptibility to toxic compounds not used in therapy such as CCCP and tetrachlorosalicylanilide [27]. Other two efflux pumps, SmeIJK and SmeYZ, provide levofloxacin resistance when they are overexpressed [26]. Nevertheless, their substrate profile is different. While efflux pump SmeIJK overexpression affects susceptibility to aminoglycosides, ciprofloxacin, and tetracycline, SmeYZ overproduction only changes aminoglycosides’ susceptibility [13].
The overexpression or the inactivation of efflux pumps affects antimicrobial susceptibility in different ways. The fact that the deletion of OMPs, such as SmeC and TolCsm, alters the susceptibility to antimicrobial agents, together with the absence of OMP-encoding genes in the operons encoding some efflux pumps such as SmeIJK, SmeOP, and SmeYZ, suggests that such OMPs are not efflux pump specific and several pumps could use the same OMP. Actually, the deletion of smeC, encoded in the smeABC operon, affects susceptibility to several antimicrobials, whereas the deletion of the gene encoding the actual inner membrane efflux pump smeB does not have any relevant effect on antimicrobial susceptibility [20]. In a similar way, the tolCsm gene encodes an OMP and is located upstream smeOP in another operon, smeRo-pcm-tolC, which suggests that it might form part of the SmeOP efflux pump [27, 39]. Nevertheless the deletion of tolCsm increases the susceptibility to several compounds, without showing any correlation with the phenotype observed in a mutant lacking smeOP [39].
It has been recently shown that the use of antibodies targeting efflux pumps might increase S. maltophilia susceptibility to antimicrobials [40]. These OMPs that are shared by different efflux pumps might be good targets for such antibodies since their inactivation will potentially inhibit simultaneously the action of different efflux pumps.
2.2 MFS Efflux Pumps
The study of efflux pumps belonging to the other families already found in S. maltophilia, namely, MFS and ABC, has received less attention than in the case of RND pumps. Four MFS efflux pumps have been so far identified in the genome of this bacterial species [13, 41]. One of these, EmrCABsm, is encoded in an operon of four genes that encodes the three efflux pump components and the transcriptional regulator of the expression of the pump emrRsm (MarR type) transcribed in the same direction. The deletion of emrRsm causes the overexpression of the efflux pump, which reduces S. maltophilia susceptibility to nalidixic acid and CCCP [31]. This indicates that emrRsm encodes a repressor of emrCABsm. The second MFS-type efflux pump (Smlt0032) has been identified only by bioinformatics analysis, and information on its role in antimicrobial resistance remains to be confirmed [13]. The third MFS-type efflux pump, MfsA, has been associated with methyl viologen resistance. Its regulator, SoxR, is a sensor of superoxide-generating agents [41]. However, whether or not this efflux pump has a role in the resistance of S. maltophilia against REDOX compounds remains to be established. SmtcrA is another MFS efflux pump, which is associated to tetracycline resistance. It is localized near another antimicrobial resistance gene, Smqnr. Previous work shows that both genes seem to be regulated by the same regulator SmQnrR [32], although a more recent study indicated that the effect of SmQnrR on Smqnr regulation is strain specific and that this repressor regulates SmtcrA expression in the two S. maltophilia strains studied so far [42].
2.3 ABC Efflux Pumps
Two ABC efflux pumps, SmrA and MacABCsm, are present in S. maltophilia [33, 34]. The activity of the MacABCsm efflux pump is associated with reduced susceptibility to aminoglycosides, macrolides, and polymyxins. Interestingly, a mutant presenting the deletion of the OMP, macCsm, has a different phenotype than mutants lacking macAB. These data suggest that the MacABCsm efflux pump can use an alternative, still-unidentified, OMP [34], as it was reported for some of the RND-type efflux pumps (see above). The second ABC efflux pump, SmrA, has been studied only in the heterologous host E. coli, in which it provides resistance to fluoroquinolones, tetracycline, doxorubicin, and multiple dyes. Whether or not this efflux pump is involved in resistance to these compounds in S. maltophilia remains to be established [33].
3 Regulation of the Expression of S. maltophilia Efflux Pumps
Expression of efflux pumps is in general tightly controlled by both local and general regulators. A possible reason why they are expressed at low levels unless an effector is present is that their expression can entail fitness costs. This cost can be due to the waste of energy required for the synthesis and activity of these macromolecular complexes and also because efflux pumps may extrude molecules that are important for microbial physiology such as quorum-sensing signals or virulence determinants among other compounds [43–45]. As shown in Table 15.1, hypothetical regulators, belonging to different structural families, have been identified for five RND efflux pumps. Most studies are based on the in vitro inactivation of the regulator. In two cases [42], the efflux pumps smeDEF and smeVWX, mutations inactivating their regulators, SmeT (TetR type) and SmeRv (LysR type) that lead to the overexpression of SmeDEF and SmeVWX, respectively [28, 46], were characterized both in vitro and in vivo [28, 38, 47–52]. Another TetR-type protein (SmeRo) regulates the efflux pump SmeOP [27]. In the case of SmeABC, a two-component system seems to be responsible of its regulation [20], a situation also observed for the efflux pump SmeYZ [13].
The molecular and structural basis of the regulation of smeDEF has been studied in detail. Expression of this efflux pump is downregulated by the transcriptional repressor SmeT, which is encoded upstream of smeDEF, in its complementary DNA strand [46]. In addition to repressing smeDEF transcription, SmeT also downregulates smeT transcription [46]. Crystal structure and biochemical analyses have shown that, like other members of the TetR family of transcriptional repressors, SmeT behaves as a dimer. A pair of dimers binds to a pseudopalindromic 28 bp region that overlaps both smeT and smeD promoters [53]. Binding of SmeT to this operator region precludes the transcription of smeT and smeDEF, likely by steric hindrance impeding RNA polymerase binding to DNA (Fig. 15.2). It is to be noticed that while most studied clinical isolates overexpressing SmeDEF present mutations in smeT, one smeDEF-overexpressing clinical isolate did not present relevant changes neither in smeT nor in its operator sequence [47]. This result strongly suggests that other proteins besides SmeT may participate in the regulation of smeDEF expression.
Transcriptional repression of smeDEF by SmeT. Representation of a pair of dimers of the transcriptional repressor SmeT (yellow spheres) bound to its DNA operator region (green double helix). The binding of the protein impedes the smeDEF pump transcription since the smeD promoter overlaps with the repressor’s operator, making impossible the RNA polymerase-DNA initiation complex. A bar indicating the order and position of the smeT and smeDEF genes (yellow and pink, respectively), as well as their promoters (psmeT and psmeDEF), is included
High-level expression of SmeDEF can be achieved by mutating SmeT or by releasing its binding from its operator in the presence of a SmeT effector. It has been shown that, while antibiotics that are good substrates of the efflux pumps are not effectors of SmeT, other compounds such as biocides or flavonoids present in plant exudates can be accommodated by the SmeT binding pocket (Fig. 15.3), releasing the regulator from its operator and, consequently, allowing the induction of SmeDEF expression [18, 37, 54]. The fact that flavonoids, and not antibiotics, are good SmeT effectors suggests that the original function of SmeDEF is not necessarily the extrusion of antibiotics (see below).
Crystal structure of the SmeT-triclosan complex. Shown is a cartoon representation of a dimer of the transcriptional regulator SmeT (one monomer in pale yellow and the second one in orange) accommodating two molecules of the biocide triclosan (blue and light blue sticks). The residues responsible for the key interactions protein-biocide (His-67, Met-113, Phe-133, and His-167) are represented as red spheres
4 Clinical Relevance of S. maltophilia Efflux Pumps
Most works on the substrate range and regulation of S. maltophilia efflux pumps have been performed in vitro. From these studies, we can state which efflux pumps are involved in intrinsic S. maltophilia resistance to antimicrobial agents (Table 15.1) and predict which ones may contribute to the acquired resistance upon their overexpression. Nevertheless there are few detailed epidemiological analyses describing mutants overexpressing these efflux pumps in clinical isolates. These studies are hampered because, in contrast to the situation in other Gram-negative bacteria in which efflux can be inferred by determining the minimal inhibitory concentrations (MICs) of the antimicrobials of choice in the presence and in the absence of the efflux pump inhibitor phenylalanine-arginine-ß-naphthylamide, this compound does not inhibit the activity of S. maltophilia efflux pumps [55]. Despite this situation, functional and molecular assays have shown that overexpression of SmeDEF is common among clinical S. maltophilia isolates [47, 48, 56]. In addition, clinical isolates overexpressing SmeVWX have been also found, some of them presenting the same mutation in smeRv, which encodes the transcriptional regulator of this efflux pump that has been described for in vitro selected smeVWX overexpressing mutants [38, 50–52]. These data support the idea that in vitro evolution studies may help in predicting mutations appearing in vivo during the treatment of patients [57–60]. This could help in improving therapeutic regiments in order to avoid the emergence of antimicrobial resistance, particularly MDR, because selection by a single antimicrobial of mutants that overexpress an efflux pump will render resistance to all the antimicrobials that are substrates of such an efflux pump.
One aspect in which S. maltophilia efflux pumps’ activity is particularly cumbersome concerns acquired resistance to quinolones. Quinolones are synthetic antimicrobials with a broad spectrum of activity. They were discovered in the 1960s while studying chloroquine for malaria treatment [61]. Afterward, it was proven that a fluoride group added to the central ring of the molecule increases the efficiency of the antimicrobial, creating the fluoroquinolones. Since there are no quinolone producers in nature, it was expected that resistance to this family of drugs would appear just through mutations in the genes encoding for their targets, the bacterial topoisomerases [62]. In fact, mutations in these genes, especially in the quinolone resistance-determining regions (QRDRs), are the main cause of high-level quinolone resistance in all studied microorganisms.
The exception to this rule is S. maltophilia. Different works have shown that, in sharp contrast with what happens for other bacterial species, such mutations are not found in quinolone-resistant S. maltophilia strains, neither in mutants selected in vitro nor in clinical isolates [28, 63–65]. The reason behind this situation is likely that, whereas usually overexpression of efflux pumps confers low-level resistance to quinolones in all bacterial pathogens so far studied, the overexpression of efflux pumps may confer the clinically relevant resistance in the case of S. maltophilia. Indeed, it has been shown that the overexpression of SmeDEF correlates with the quinolone resistance of in vitro selected mutants [28] and several clinical isolates overexpress this system [38, 47, 52, 56, 66]. Further, even when this efflux pump is inactivated, quinolone-resistant mutants do not present changes in the QRDR of the topoisomerases, but resistance is caused by the overexpression of yet another different efflux pump, SmeVWX [28]. It is important to notice that SmeVWX-overexpressing clinical strains presenting the same mutations in its regulator as the in vitro selected mutants have been reported [28, 52].
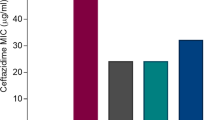
One intriguing finding is that although SmeDEF overexpression is found more frequently in both the in vitro obtained mutants and the clinical isolates, SmeVWX overexpression leads to higher quinolone MICs in S. maltophilia [28, 52]. It is possible that, once a clinically relevant resistance is achieved, the only factor affecting the selection of one mutation over another consists of a fitness cost associated with the acquisition of each of such mutations [59, 60, 67, 68]. In this regard, it has been described that SmeDEF overexpression impairs S. maltophilia fitness and virulence [66]. Whether or not the effect of SmeVWX overexpression in S. maltophilia is similar (or eventually more drastic) remains to be established.
While efflux pumps seem to be major players in the acquisition of quinolone resistance by S. maltophilia, this bacterial species also contains in its genome a gene encoding a quinolone resistance protein SmQnr, which also might contribute to this resistance [11, 12]. Although the in vitro studies show that the SmQnr overexpression increases MICs of quinolones [11, 12], the SmQnr overexpression has not been found as the cause of resistance neither in in vitro selected quinolone-resistant mutants nor in clinical isolates. A reason for such situation is that in contrast to the overexpression of S. maltophilia efflux pumps, the SmQnr overexpression renders only a low-level quinolone resistance [28, 52]. We can then conclude that the overexpression of either SmeDEF or SmeVWX is the only known mechanism of quinolone resistance in S. maltophilia, which is present after the in vitro selection of quinolone-resistant mutants, and has been described in clinical isolates of this bacterial species [28, 52, 69].
5 S. maltophilia Efflux Pumps: More Than Antimicrobial Resistance Determinants
Even though the majority of studies related to efflux pumps explore their role in antimicrobial resistance, it is known that functions of MDR pumps are very diverse [14]. It has been shown that, besides antibiotics, efflux pumps can extrude a huge variety of compounds like heavy metals [70], organic solvents [71], dyes [72], detergents [25], bile salts [73], biocides [36], quorum-sensing signals [43–45], or plant-produced compounds [74–77]. However, little is known about functions that S. maltophilia efflux pumps have in dealing with the behavior of this microorganism in its natural habitat.
Some recent works begin to address this issue; SmeDEF, for example, is involved in the colonization of plant roots by S. maltophilia [28]. Plant-produced flavonoids can bind to SmeT, derepressing smeDEF expression. They are bona fide effectors regulating smeDEF expression, since they specifically induce this pump and not other S. maltophilia efflux pumps. Consistent with these findings, the deletion of smeE impairs S. maltophilia colonization of plant roots. These results show that one original function of SmeDEF is the colonization of plant roots, and only in clinical settings the quinolone resistance is manifested as a function of this efflux pump, being a good example of exaptation, an evolutionary process in which a change of function is achieved by an environmental shift, not by a genetic change [17, 78].
Not only has SmeDEF a role in the interaction of S. maltophilia with plants, but SmeVWX might also be somehow related. The diffusible signal factor (DSF) is a quorum-sensing molecule of fatty acid nature that was first detected in Xanthomonas campestris [79]. This molecule is also present in S. maltophilia and is involved in the regulation of the expression of numerous genes directly or indirectly involved in plant growth promotion and biocontrol, including antimicrobial resistance genes such as SmeW [80]. When the gene encoding the DSF synthase, rpfF, is deleted, the smeW expression is downregulated, indicating that SmeW is an efflux pump that may also be somehow involved in colonization of plants by S. maltophilia, although further studies are needed to address this hypothesis. DSF also regulates chaperone biosynthetic genes and therefore the stress resistance [80], establishing an indirect link between SmeVWX efflux pump and stress response.
SmeIJK operon contains two RND-type transporters (SmeJ and SmeK) and is constitutively expressed in the absence of antimicrobial pressure, indicating that antimicrobial resistance is not likely the main function of this pump. A recent study showed a direct relationship among the SmeIJK efflux pump, the cell envelope integrity, and the envelope stress response mediated by the sigma factor RpoE [81]. When smeIJK is deleted, S. maltophilia is more susceptible to hyposmolarity and to membrane-damaging agents (MDAs) such as sodium dodecyl sulfate or Triton X-100. In addition, the loss of SmeIJK activates the rpoE regulon. This regulon can also be activated in the presence of MDAs, and this activation further upregulates SmeIJK expression. In the presence of antimicrobials that are known substrates of SmeIJK efflux pump, smeIJK expression is not increased, further confirming the main function of SmeIJK to be a part of the S. maltophilia envelope stress responses via RpoE [81]. Another pump with a known function in S. maltophilia envelope stress responses is the ABC-type efflux pump, MacABCsm [34]. This pump is also constitutively expressed, and besides envelope stress responses, it also has a role in oxidative tolerance and biofilm formation.
S. maltophilia is an opportunistic pathogen with increasing relevance in nosocomial infections [4]; however, its natural habitats are water and soil, where this microorganism can colonize all parts of plants, including the whole endosphere [82]. As stated previously, little is known about the role of efflux pumps of S. maltophilia in the natural environment, but with this natural origin, it is predicted that the majority of efflux pumps should display different functions in these habitats. The interest in knowing the original functions of efflux pumps is increasing, so it is expected that, in the next years, more natural functions for these antimicrobial resistance determinants will be deciphered.
References
Sánchez MB, Hernández A, Martínez JL (2009) Stenotrophomonas maltophilia drug resistance. Future Microbiol 4:655–660. doi:10.2217/fmb.09.45
Sánchez MB (2015) Antibiotic resistance in the opportunistic pathogen Stenotrophomonas maltophilia. Front Microbiol 6:658. doi:10.3389/fmicb.2015.00658
Quinn JP (1998) Clinical problems posed by multiresistant nonfermenting Gram-negative pathogens. Clin Infect Dis 27(Suppl 1):S117–S124. doi:10.1086/514912
Brooke JS (2012) Stenotrophomonas maltophilia: an emerging global opportunistic pathogen. Clin Microbiol Rev 25:2–41. doi:10.1128/CMR.00019-11
Walsh TR, Macgowan AP, Bennett, P.M. (1997). Sequence analysis and enzyme kinetics of the L2 serine β-lactamase from Stenotrophomonas maltophilia. Antimicrob Agents Chemother 41:1460–1464.
Avison MB, Higgins CS, Ford PJ, von Heldreich CJ, Walsh TR, Bennett PM (2002) Differential regulation of L1 and L2 β-lactamase expression in Stenotrophomonas maltophilia. J Antimicrob Chemother 49:387–389. doi:10.1093/jac/49.2.387
Okazaki A, Avison MB (2007) Aph(3′)-IIc, an aminoglycoside resistance determinant from Stenotrophomonas maltophilia. Antimicrob Agents Chemother 51:359–360. doi:10.1128/AAC.00795-06
Lambert T, Ploy MC, Denis F, Courvalin P (1999) Characterization of the chromosomal aac(6′)-Iz gene of Stenotrophomonas maltophilia. Antimicrob Agents Chemother 43:2366–2371
Li X-Z, Zhang L, McKay GA, Poole K (2003) Role of the acetyltransferase AAC(6′)-Iz modifying enzyme in aminoglycoside resistance in Stenotrophomonas maltophilia. J Antimicrob Chemother 51:803–811. doi:10.1093/jac/dkg148
Sánchez MB, Hernández A, Rodríguez-Martínez JM, Martínez-Martínez L, Martínez JL (2008) Predictive analysis of transmissible quinolone resistance indicates Stenotrophomonas maltophilia as a potential source of a novel family of Qnr determinants. BMC Microbiol 8:148. doi:10.1186/1471-2180-8-148
Shimizu K, Kikuchi K, Sasaki T, Takahashi N, Ohtsuka M, Ono Y, Hiramatsu K (2008) Smqnr, a new chromosome-carried quinolone resistance gene in Stenotrophomonas maltophilia. Antimicrob Agents Chemother 52:3823–3825. doi:10.1128/AAC.00026-08
Sánchez MB, Martínez JL (2010) SmQnr contributes to intrinsic resistance to quinolones in Stenotrophomonas maltophilia. Antimicrob Agents Chemother 54:580–581. doi:10.1128/AAC.00496-09
Crossman LC, Gould VC, Dow JM, Vernikos GS, Okazaki A, Sebaihia M, Saunders D, Arrowsmith C et al (2008) The complete genome, comparative and functional analysis of Stenotrophomonas maltophilia reveals an organism heavily shielded by drug resistance determinants. Genome Biol 9:R74. doi:10.1186/gb-2008-9-4-r74
Martínez JL, Sánchez MB, Martínez-Solano L, Hernández A, Garmendia L, Fajardo A, Alvarez-Ortega C (2009) Functional role of bacterial multidrug efflux pumps in microbial natural ecosystems. FEMS Microbiol Rev 33:430–449. doi:10.1111/j.1574-6976.2008.00157.x
Martínez JL, Fajardo A, Garmendia L, Hernández A, Linares JF, Martinez-Solano L, Sánchez MB (2009) A global view of antibiotic resistance. FEMS Microbiol Rev 33:44–65. doi:10.1111/j.1574-6976.2008.00142.x
Fajardo A, Linares JF, Martinez JL (2009) Towards an ecological approach to antibiotics and antibiotic resistance genes. Clin Microbiol Infect 15(Suppl 1):14–16. doi:10.1111/j.1469-0691.2008.02688.x
Baquero F, Alvarez-Ortega C, Martínez JL (2009) Ecology and evolution of antibiotic resistance. Environ Microbiol Rep 1:469–476. doi:10.1111/j.1758-2229.2009.00053.x
García-León G, Hernández A, Hernando-Amado S, Alavi P, Berg G, Martínez JL (2014) A function of SmeDEF, the major quinolone resistance determinant of Stenotrophomonas maltophilia, is the colonization of the roots of the plants. Appl Environ Microbiol 80:4559–4565. doi:10.1128/AEM.01058-14
Alonso A, Martínez JL (2000) Cloning and characterization of SmeDEF, a novel multidrug efflux pump from Stenotrophomonas maltophilia. Antimicrob Agents Chemother 44:3079–3086. doi:10.1128/AAC.44.11.3079-3086.2000
Li X-Z, Zhang L, Poole K (2002) SmeC, an outer membrane multidrug efflux protein of Stenotrophomonas maltophilia. Antimicrob Agents Chemother 46:333–343. doi:10.1128/AAC.46.2.333-343.2002
Mine T, Morita Y, Kataoka A, Mizushima T, Tsuchiya T (1999) Expression in Escherichia coli of a new multidrug efflux pump, MexXY, from Pseudomonas aeruginosa. Antimicrob Agents Chemother 43:415–417
Masuda N, Sakagawa E, Ohya S, Gotoh N, Tsujimoto H, Nishino T (2000) Contribution of the MexX-MexY-OprM efflux system to intrinsic resistance in Pseudomonas aeruginosa. Antimicrob Agents Chemother 44:2242–2246. doi:10.1128/AAC.44.9.2242-2246.2000
Gotoh N, Tsujimoto H, Poole K, Yamagishi J, Nishino T (1995) The outer membrane protein OprM of Pseudomonas aeruginosa is encoded by oprK of the mexA-mexB-oprK multidrug resistance operon. Antimicrob Agents Chemother 39:2567–2569. doi:10.1128/AAC.39.11.2567
Grkovic S, Brown MH, Skurray RA (2002) Regulation of bacterial drug export systems. Microbiol Mol Biol Rev 66:671–701. doi:10.1128/MMBR.66.4.671-701.2002
Zhang L, Li X-Z, Poole K (2001) SmeDEF multidrug efflux pump contributes to intrinsic multidrug resistance in Stenotrophomonas maltophilia. Antimicrob Agents Chemother 45:3497–3503. doi:10.1128/AAC.45.12.3497-3503.2001
Gould VC, Okazaki A, Avison MB (2013) Coordinate hyperproduction of SmeZ and SmeJK efflux pumps extends drug resistance in Stenotrophomonas maltophilia. Antimicrob Agents Chemother 57:655–657. doi:10.1128/AAC.01020-12
Lin CW, Huang YW, Hu RM, Yang TC (2014) SmeOP-TolCsm efflux pump contributes to the multidrug resistance of Stenotrophomonas maltophilia. Antimicrob Agents Chemother 58:2405–2408. doi:10.1128/AAC.01974-13
García-León G, Salgado F, Oliveros JC, Sánchez MB, Martínez JL (2014) Interplay between intrinsic and acquired resistance to quinolones in Stenotrophomonas maltophilia. Environ Microbiol 16:1282–1296. doi:10.1111/1462-2920.12408
Chen CH, Huang CC, Chung TC, Hu RM, Huang YW, Yang TC (2011) Contribution of resistance-nodulation-division efflux pump operon smeU1-V-W-U2-X to multidrug resistance of Stenotrophomonas maltophilia. Antimicrob Agents Chemother 55:5826–5833. doi:10.1128/AAC.00317-11
Lin YT, Huang YW, Chen SJ, Chang CW, Yang TC (2015) SmeYZ efflux pump of Stenotrophomonas maltophilia contributes to drug resistance, virulence-related characteristics, and virulence to mice. Antimicrob Agents Chemother 59:4067–4073. doi:10.1128/aac.00372-15
Huang YW, Hu RM, Chu FY, Lin HR, Yang TC (2013) Characterization of a major facilitator superfamily (MFS) tripartite efflux pump EmrCABsm from Stenotrophomonas maltophilia. J Antimicrob Chemother 68:2498–2505. doi:10.1093/jac/dkt250
Chang YC, Tsai MJ, Huang YW, Chung TC, Yang TC (2011) SmQnrR, a DeoR-type transcriptional regulator, negatively regulates the expression of Smqnr and SmtcrA in Stenotrophomonas maltophilia. J Antimicrob Chemother 66:1024–1028. doi:10.1093/jac/dkr049
Al-Hamad A, Upton M, Burnie J (2009) Molecular cloning and characterization of SmrA, a novel ABC multidrug efflux pump from Stenotrophomonas maltophilia. J Antimicrob Chemother 64:731–734. doi:10.1093/jac/dkp271
Lin YT, Huang YW, Liou RS, Chang YC, Yang TC (2014) MacABCsm, an ABC-type tripartite efflux pump of Stenotrophomonas maltophilia involved in drug resistance, oxidative and envelope stress tolerances and biofilm formation. J Antimicrob Chemother 69:3221–3226. doi:10.1093/jac/dku317
Sánchez MB, Martínez JL (2015) The efflux pump SmeDEF contributes to trimethoprim-sulfamethoxazole resistance in Stenotrophomonas maltophilia. Antimicrob Agents Chemother 59:4347–4348. doi:10.1128/AAC.00714-15
Sánchez P, Moreno E, Martínez JL (2005) The biocide triclosan selects Stenotrophomonas maltophilia mutants that overproduce the SmeDEF multidrug efflux pump. Antimicrob Agents Chemother 49:781–782. doi:10.1128/AAC.49.2.781-782.2005
Hernández A, Ruiz FM, Romero A, Martínez JL (2011) The binding of triclosan to SmeT, the repressor of the multidrug efflux pump SmeDEF, induces antibiotic resistance in Stenotrophomonas maltophilia. PLoS Pathog 7:e1002103. doi:10.1371/journal.ppat.1002103
Alonso A, Martínez JL (2001) Expression of multidrug efflux pump SmeDEF by clinical isolates of Stenotrophomonas maltophilia. Antimicrob Agents Chemother 45:1879–1881. doi:10.1128/AAC.45.6.1879-1881.2001
Huang YW, Hu RM, Yang TC (2013) Role of the pcm-tolCsm operon in the multidrug resistance of Stenotrophomonas maltophilia. J Antimicrob Chemother 68:1987–1993. doi:10.1093/jac/dkt148
Al-Hamad A, Burnie J, Upton M (2011) Enhancement of antibiotic susceptibility of Stenotrophomonas maltophilia using a polyclonal antibody developed against an ABC multidrug efflux pump. Can J Microbiol 57:820–828. doi:10.1139/w11-076
Srijaruskul K, Charoenlap N, Namchaiw P, Chattrakarn S, Giengkam S, Mongkolsuk S, Vattanaviboon P (2015) Regulation by SoxR of mfsA, which encodes a major facilitator protein involved in paraquat resistance in Stenotrophomonas maltophilia. PLoS One 10:e0123699. doi:10.1371/journal.pone.0123699
Sánchez MB, Martínez JL (2015) Regulation of Smqnr expression by SmqnrR is strain-specific in Stenotrophomonas maltophilia. J Antimicrob Chemother 70:2913–2914. doi:10.1093/jac/dkv196
Evans K, Passador L, Srikumar R, Tsang E, Nezezon J, Poole K (1998) Influence of the MexAB-OprM multidrug efflux system on quorum sensing in Pseudomonas aeruginosa. J Bacteriol 180:5443–5447
Köhler T, van Delden C, Curty LK, Hamzehpour MM, Pechère JC (2001) Overexpression of the MexEF-OprN multidrug efflux system affects cell-to-cell signaling in Pseudomonas aeruginosa. J Bacteriol 183:5213–5222. doi:10.1128/JB.183.18.5213-5222.2001
Olivares J, Alvarez-Ortega C, Linares JF, Rojo F, Köhler T, Martínez JL (2012) Overproduction of the multidrug efflux pump MexEF-OprN does not impair Pseudomonas aeruginosa fitness in competition tests, but produces specific changes in bacterial regulatory networks. Environ Microbiol 14:1968–1981. doi:10.1111/j.1462-2920.2012.02727.x
Sánchez P, Alonso A, Martínez JL (2002) Cloning and characterization of SmeT, a repressor of the Stenotrophomonas maltophilia multidrug efflux pump SmeDEF. Antimicrob Agents Chemother 46:3386–3393. doi:10.1128/AAC.46.11.3386-3393.2002
Sánchez P, Alonso A, Martínez JL (2004) Regulatory regions of smeDEF in Stenotrophomonas maltophilia strains expressing different amounts of the multidrug efflux pump SmeDEF. Antimicrob Agents Chemother 48:2274–2276. doi:10.1128/AAC.48.6.2274-2276.2004
Chang LL, Chen HF, Chang CY, Lee TM, Wu WJ (2004) Contribution of integrons, and SmeABC and SmeDEF efflux pumps to multidrug resistance in clinical isolates of Stenotrophomonas maltophilia. J Antimicrob Chemother 53:518–521. doi:10.1093/jac/dkh094
Gould IM (2010) Coping with antibiotic resistance: the impending crisis. Int J Antimicrob Agents 36(Suppl 3):S1–S2. doi:10.1016/S0924-8579(10)00497-8
Cho HH, Sung JY, Kwon KC, Koo SH (2012) Expression of Sme efflux pumps and multilocus sequence typing in clinical isolates of Stenotrophomonas maltophilia. Ann Lab Med 32:38–43. doi:10.3343/alm.2012.32.1.38
Liaw SJ, Lee YL, Hsueh PR (2010) Multidrug resistance in clinical isolates of Stenotrophomonas maltophilia: roles of integrons, efflux pumps, phosphoglucomutase (SpgM), and melanin and biofilm formation. Int J Antimicrob Agents 35:126–130. doi:10.1016/j.ijantimicag.2009.09.015
García-León G, Ruiz de Alegria Puig C, Garcia de la Fuente C, Martínez-Martínez L, Martínez JL, Sánchez MB (2015) High-level quinolone resistance is associated with the overexpression of smeVWX in Stenotrophomonas maltophilia clinical isolates. Clin Microbiol Infect 21:464–467. doi:10.1016/j.cmi.2015.01.007
Hernández A, Mate MJ, Sánchez-Diaz PC, Romero A, Rojo F, Martínez JL (2009) Structural and functional analysis of SmeT, the repressor of the Stenotrophomonas maltophilia multidrug efflux pump SmeDEF. J Biol Chem 284:14428–14438. doi:10.1074/jbc.M809221200
Sánchez MB, Decorosi F, Viti C, Oggioni MR, Martinez JL, Hernández A (2015) Predictive studies suggest that the risk for the selection of antibiotic resistance by biocides is likely low in Stenotrophomonas maltophilia. PLoS One 10:e0132816. doi:10.1371/journal.pone.0132816
Sánchez P, Le U, Martínez JL (2003) The efflux pump inhibitor Phe-Arg-β-naphthylamide does not abolish the activity of the Stenotrophomonas maltophilia SmeDEF multidrug efflux pump. J Antimicrob Chemother 51:1042–1045. doi:10.1093/jac/dkg181
Gould VC, Avison MB (2006) SmeDEF-mediated antimicrobial drug resistance in Stenotrophomonas maltophilia clinical isolates having defined phylogenetic relationships. J Antimicrob Chemother 57:1070–1076. doi:10.1093/jac/dkl106
Barlow M, Hall BG (2002) Predicting evolutionary potential: in vitro evolution accurately reproduces natural evolution of the TEM β-lactamase. Genetics 160:823–832
Hall BG (2004) Predicting the evolution of antibiotic resistance genes. Nat Rev Microbiol 2:430–435. doi:10.1038/nrmicro888
Martínez JL, Baquero F, Andersson DI (2007) Predicting antibiotic resistance. Nat Rev Microbiol 5:958–965. doi:10.1038/nrmicro1796
Martínez JL, Baquero F, Andersson DI (2011) Beyond serial passages: new methods for predicting the emergence of resistance to novel antibiotics. Curr Opin Pharmacol 11:439–445. doi:10.1016/j.coph.2011.07.005
Deitz WH, Bailey JH, Froelich EJ (1963) In vitro antibacterial properties of nalidixic acid, a new drug active against Gram-negative organisms. Antimicrob Agents Chemother (Bethesda) 161:583–587
Hernández A, Sánchez MB, Martínez JL (2011) Quinolone resistance: much more than predicted. Front Microbiol 2:22. doi:10.3389/fmicb.2011.00022
Ribera A, Domenech-Sanchez A, Ruiz J, Benedi VJ, Jimenez de Anta MT, Vila J (2002) Mutations in gyrA and parC QRDRs are not relevant for quinolone resistance in epidemiological unrelated Stenotrophomonas maltophilia clinical isolates. Microb Drug Resist 8:245–251. doi:10.1089/10766290260469499
Valdezate S, Vindel A, Echeita A, Baquero F, Cantó R (2002) Topoisomerase II and IV quinolone resistance-determining regions in Stenotrophomonas maltophilia clinical isolates with different levels of quinolone susceptibility. Antimicrob Agents Chemother 46:665–671. doi:10.1128/AAC.46.3.665-671.2002
Valdezate S, Vindel A, Saez-Nieto JA, Baquero F, Cantó R (2005) Preservation of topoisomerase genetic sequences during in vivo and in vitro development of high-level resistance to ciprofloxacin in isogenic Stenotrophomonas maltophilia strains. J Antimicrob Chemother 56:220–223. doi:10.1093/jac/dki182
Alonso A, Morales G, Escalante R, Campanario E, Sastre L, Martínez JL (2004) Overexpression of the multidrug efflux pump SmeDEF impairs Stenotrophomonas maltophilia physiology. J Antimicrob Chemother 53:432–434. doi:10.1093/jac/dkh074
Andersson DI, Hughes D (2011) Persistence of antibiotic resistance in bacterial populations. FEMS Microbiol Rev 35:901–911. doi:10.1111/j.1574-6976.2011.00289.x
Martínez JL, Coque TM, Baquero F (2015) What is a resistance gene? Ranking risk in resistomes. Nat Rev Microbiol 13:116–123. doi:10.1038/nrmicro3399
Pak TR, Altman DR, Attie O, Sebra R, Hamula CL, Lewis M, Deikus G, Newman LC et al (2015) Whole-genome sequencing identifies emergence of a quinolone resistance mutation in a case of Stenotrophomonas maltophilia bacteremia. Antimicrob Agents Chemother 59:7117–7120. doi:10.1128/AAC.01723-15
Nies DH (2003) Efflux-mediated heavy metal resistance in prokaryotes. FEMS Microbiol Rev 27:313–339. doi:10.1016/S0168-6445(03)00048-2
Ramos JL, Duque E, Gallegos MT, Godoy P, Ramos-Gonzalez MI, Rojas A, Teran W, Segura A (2002) Mechanisms of solvent tolerance in Gram-negative bacteria. Annu Rev Microbiol 56:743–768. doi:10.1146/annurev.micro.56.012302.161038
DeMarco CE, Cushing LA, Frempong-Manso E, Seo SM, Jaravaza TA, Kaatz GW (2007) Efflux-related resistance to norfloxacin, dyes, and biocides in bloodstream isolates of Staphylococcus aureus. Antimicrob Agents Chemother 51:3235–3239. doi:10.1128/AAC.00430-07
Buckley AM, Webber MA, Cooles S, Randall LP, La Ragione RM, Woodward MJ, Piddock LJ (2006) The AcrAB-TolC efflux system of Salmonella enterica serovar Typhimurium plays a role in pathogenesis. Cell Microbiol 8:847–856. doi:10.1111/j.1462-5822.2005.00671.x
Palumbo JD, Kado CI, Phillips DA (1998) An isoflavonoid-inducible efflux pump in Agrobacterium tumefaciens is involved in competitive colonization of roots. J Bacteriol 180:3107–3113
Burse A, Weingart H, Ullrich MS (2004) NorM, an Erwinia amylovora multidrug efflux pump involved in in vitro competition with other epiphytic bacteria. Appl Environ Microbiol 70:693–703. doi:10.1128/AEM.70.2.693-703.2004
Dixon RA (2001) Natural products and plant disease resistance. Nature 411:843–847. doi:10.1038/35081178
Espinosa-Urgel M, Kolter R, Ramos JL (2002) Root colonization by Pseudomonas putida: love at first sight. Microbiology 148:341–343. doi:10.1099/00221287-148-2-341
Gould SJ, Vrba S (1982) Exaptation: a missing term in the science of form. Paleobiology 8:4–15
Barber CE, Tang JL, Feng JX, Pan MQ, Wilson TJ, Slater H, Dow JM, Williams P et al (1997) A novel regulatory system required for pathogenicity of Xanthomonas campestris is mediated by a small diffusible signal molecule. Mol Microbiol 24:555–566. doi:10.1046/j.1365-2958.1997.3721736.x
Alavi P, Muller H, Cardinale M, Zachow C, Sanchez MB, Martinez JL, Berg G (2013) The DSF quorum sensing system controls the positive influence of Stenotrophomonas maltophilia on plants. PLoS One 8:e67103. doi:10.1371/journal.pone.0067103
Huang YW, Liou RS, Lin YT, Huang HH, Yang TC (2014) A linkage between SmeIJK efflux pump, cell envelope integrity, and σE-mediated envelope stress response in Stenotrophomonas maltophilia. PLoS One 9:e111784. doi:10.1371/journal.pone.0111784
Zhu B, Liu H, Tian WX, Fan XY, Li B, Zhou XP, Jin GL, Xie GL (2012) Genome sequence of Stenotrophomonas maltophilia RR-10, isolated as an endophyte from rice root. J Bacteriol 194:1280–1281. doi:10.1128/JB.06702-11
Acknowledgments
Work in the authors’ laboratory is supported by grants from the Spanish Ministry of Economy and Competitiveness (BIO2014-54507-R), from the Madrid Autonomous Community (S2010/BMD2414 (PROMPT)), from the Instituto de Salud Carlos III (Spanish Network for Research on Infectious Diseases (REIPI RD12/0015)), and from the European Union (HEALTH-F3-2011-282004 (EVOTAR)).
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Sánchez, M.B., García-León, G., Hernández, A., Martínez, J.L. (2016). Antimicrobial Drug Efflux Pumps in Stenotrophomonas maltophilia . In: Li, XZ., Elkins, C., Zgurskaya, H. (eds) Efflux-Mediated Antimicrobial Resistance in Bacteria. Adis, Cham. https://doi.org/10.1007/978-3-319-39658-3_15
Download citation
DOI: https://doi.org/10.1007/978-3-319-39658-3_15
Published:
Publisher Name: Adis, Cham
Print ISBN: 978-3-319-39656-9
Online ISBN: 978-3-319-39658-3
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)