Abstract
Present day, the neurovascular preservation is accomplished by the surgeon’s expertise and knowledge of the anatomy, as well as by the improvements of visualization, instrumentation, and magnification provided by novel robotic systems. In this chapter, we discuss fundamental aspects of the neurovascular anatomy, define landmarks and principles for a NS radical prostatectomy, and also review some of the new technological developments designed to help surgeons to perform these critical steps and achieve an early return of the erectile function.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Radical prostatectomy
- Potency
- Technical innovations
- Athermal nerve spare
- Minimal countertraction
- Retrograde nerve spare
- Dehydrated human amnion chorion membrane
- Immunofluorescence
- Penile rehabilitation
Introduction
With radical prostatectomy (RP) delivering better survival results, preservation of erectile function has become an increasing priority among patients who choose surgery as the first line of treatment. To date, the ideal outcome cannot be limited to oncologic freedom since contemporary patients, due to their young age, are motivated to preserve their sexual function and urinary continence.
Before the discovery of the neurovascular bundles (NVBs) by Walsh and Donker [1], the cause of erectile dysfunction following RP was not completely understood. Since the introduction of the anatomic nerve-sparing (NS) technique, the injury to the cavernous nerve intraoperatively may be preventable. An adequate surgical technique that minimizes the damage to the NVBs plays a key role in preservation and functional recovery.
Present day, the neurovascular preservation is accomplished by the surgeon’s expertise and knowledge of the anatomy, as well as by the improvements of visualization, instrumentation, and magnification provided by novel robotic systems. In this chapter, we discuss fundamental aspects of the neurovascular anatomy, define landmarks and principles for a NS radical prostatectomy, and also review some of the new technological developments designed to help surgeons to perform these critical steps and achieve an early return of the erectile function.
Anatomy of Neurovascular Bundles
The pelvic splenic nerves arise from the anterior sacral roots, with most branches originating from S4 and smaller contribution of S2 and S3. These parasympathetic fibers converge with sympathetic fibers from the hypogastric nerve to form the pelvis plexus.
The inferior extension of the pelvic plexus unites with several vessels to form the neurovascular bundle (NVB) of Walsh. This tubular structure runs along the dorsolateral aspect of the prostate gland enclosed in fascial sheets and intimately associates with the capsular vessels of the prostate.
Many anatomic studies have suggested that in addition to the NVB, multiples accessory channels exist that ramify in the prostatic and Denonvillier’s fascia and which supply neural stimulation of the penis. These accessory fibers, which form an apical plexus on the posterolateral aspect of the prostatic apex and urethra, could potentially act as a neural pathway for the urethral sphincter [2] (Fig. 6.1).
Prostatic Vasculature as a Landmark for Nerve-Sparing RARP
There is a lack of clear macroscopic landmarks to identify the NVB during a radical prostatectomy . We have identified intraoperative elements of the prostate vasculature as anatomical reference points, key to display natural separation planes between the prostate and the neurovascular bundle. This allows us to perform the nerve sparing in a more standardized and consistent manner. A landmark artery (LA) was identified running on the lateral border of the prostate corresponding to either a prostatic or capsular artery.
The arterial supply to the prostate originates from the internal iliac (or hypogastric) artery [3, 4]. The prostatic artery (PA) is a branch of the vesicoprostatic trunk and reaches the prostate on its anterolateral aspect at the base [5]. From there, it can continue distally down to the perineum or give origin to a network of capsular arteries (CAs) running along the lateral border of the prostate [6]. During their course alongside the prostate, these elements of the prostatic vasculature (PV), especially the CAs, are related intimately with the capsular nerve (CNs) and provide a scaffold to the nerves at their course along the prostate [7]. Therefore, the PV may provide a macroscopic landmark for identifying and preserving the CNs at the time of surgery.
After opening sharply the levator fascia over the prostate, the presence of a distinctive PA could be found posterior laterally between the midprostate and the base. The artery enters the prostate on the anterolateral aspect, and it is easily recognized by its large size and tortuosity (Fig. 6.2). Delicately developing a plane of dissection between the PA and the prostate results in a natural detachment of the NVB from the prostate. For a complete NS, the correct plane of dissection is recognized by the presence of pearly areolar tissue and is gently developed posteriorly following the prostatic contour until the previously created posterior plane is reached.
Left: The prostatic artery (PA) can be recognized after opening the levator fascia on the base of the prostate. It has a large diameter and a tortuous configuration, which makes it easy to be recognized intraoperatively. It continues alongside the prostate occupying the medial aspect of the neurovascular bundle (NVB). Right: Complete left nerve sparing; the prostate has been detached from the NVB. Note how the pointed PA follows the course of the NVB and enters the perineum behind the urethra
Another common finding is the absence of a distinctive PA and the presence of multiple CAs. These arteries are found on the lateral aspect of the prostate, forming a mesh throughout the thickness of the NVB. The most superficial of these CAs can be recognized after opening the levator fascia over the prostate. It is located over the medial border of the NVB fat, close to the point where the fat ends over the prostate (Fig. 6.3).
Left: Capsular arteries (CAs) can be recognized after opening the levator fascia. They are found more distally than the prostatic artery (PA), at the level of the midprostate. CAs are thin, harder to identify, and do not have a tortuous configuration like the PA. They usually end in small twigs at the apex and do not perforate into the perineum. Right: A plane of dissection has been developed between the landmark CA and the prostate. Notice that as the dissection gets deeper, additional CAs are found along the medial aspect of the neurovascular bundle (NVB; arrow). The right plane of dissection for a complete nerve sparing is to stay on the medial aspect of the CAs, through the pearly areolar tissue between the prostate and the NVB (asterisk)
Nerve-sparing approach can be classified as either medial or lateral to the landmark artery. Fine tailoring on the medial border of the landmark artery can consistently result in a complete nerve sparing, whereas performing the nerve sparing on its lateral border results in several degrees of incomplete partial nerve sparing (Table 6.1).
Anatomic Grading of Nerve Sparing During RARP
The goal of NS during RP is to preserve the greatest possible amount of nerve tissue without compromising surgical margins. In this context, a very elegant manipulation is necessary to achieve the precise amount of nerve preservation needed for an individual patient. Schatloff et al. [8] described a standardized NS grading system based on intraoperative visual cues. The NS was graded by the surgeon intraoperatively before specimen extraction independently for either side as follows: 1 = no NS; 2 = <50 NS; 3 = 50 % NS; 4 = 75 % NS; 5 = 95 % NS. The technique consisted of sharp opening the levator fascia and identification of the LA with its course in retrograde manner up to the pedicle. This way, we were able to show a significant correlation between a higher NSS and a decreased area of residual nerve tissue on prostatectomy specimens (Fig. 6.4).
A cross-section of the neurovascular bundle, represented as a histology slide (left) and a didactic diagram (right), demonstrates our graded approach to nerve sparing (NS). Several degrees of partial NS can be obtained when paying careful attention to the anatomic cues that are discussed. LA landmark artery
In our recently updated series of 2036 patients, the potency outcomes suggested that our subjective NS system predicted potency recovery and indicated that even minor nerve trauma significantly prolonged EF recovery. By Kaplan–Meier analysis, recovery of potency is more rapid in higher NS grades (grade 2 vs. grade 3, log-rank p = 0.032; grade 3 vs. grade 4, log-rank p < 0.001; grade 4 vs. grade 5, log-rank p < 0.001) (Fig. 6.5).
Key Principles of Neurovascular Preservation
The goal of nerve sparing during RARP is to preserve the greatest possible amount of nerve tissue without compromising surgical margins. A very meticulous approach is necessary to achieve the precise amount of nerve preservation needed for an individual patient. In our institution, we established our approach to avoid an excessive traction, use of thermal energy, or direct damage during dissection (Fig. 6.6).
Retrograde Versus Antegrade Nerve Sparing During RARP
Techniques to preserve the neurovascular bundles (NVBs) have become an important part of modern RP. Increasing evidence suggests that the grades of NS are related to the recovery of potency [9–11]. Approaches for the preservation of NVBs can be performed from the prostate base to the apex (antegrade) or from the apex to the base (retrograde). The supposed benefit of the retrograde NS approach over the antegrade NS approach is the earlier identification and release of the NVB from the prostate before ligating the prostatic pedicle, thus avoiding a misplaced clip on the pedicle. The theoretical benefit of earlier release of the NVB with the pedicle intact is to attenuate neuropraxia [12–14]. Although there is evidence supporting that NS does not affect the positive surgical margin (PSM) rates, the effect of antegrade or retrograde dissection of the NVBs on PSM rates is still unknown [15, 16].
Our group first published comparative results of NS antegrade and retrograde approach demonstrating superiority of the latter one to cause less traction [17]. Based on the data of literature in open retropubic RP and laparoscopic procedure, we suggested athermal retrograde release of the NVBs during RARP.
Antegrade approach: With upward traction of the vasa and seminal vesicles, the prostatic pedicle is identified and athermally controlled close to the base to decrease the risk of severing the NVB. The prostate is then retracted, and the lateral pelvic fascia is exposed. Entering the triangular space between Denonvillier’s fascia, the lateral pelvic fascia, and the prostate, the NVB is exposed. Reflecting the lateral pelvic fascia off the prostate, dissection is performed in the interfascial plane, outside the prostatic fascia.
Retrograde approach: After the seminal vesicles have been dissected and the posterior plane is widely developed, the prostate is then rotated and the levator fascia over the prostate is opened sharply to expose the NVB from above. An interfascial plane between the prostate and the NVB is created at the level of the midprostate and is further developed until the previously created posterior plane is reached (Fig. 6.7). The plane is then continued in a retrograde direction toward the base of the prostate to completely detach the NVB from the prostatic pedicle. The plane is then continued toward the apex by detaching the prostate from the NVB.
The computer matched two groups of patients with complete bilateral NS, with no difference between groups, antegrade NS (n = 172) and retrograde NS (n = 172). Potency rates were evaluated during similar time frames using the SHIM questionnaire. The potency rate was significantly higher in the retrograde NS group than in the antegrade NS group at 3, 6, and 9 months after RARP, without compromising margins status (Fig. 6.8).
Athermal Versus Thermal Dissection of the NVB
The difference between thermal and athermal dissection of the neurovascular bundles (NVB) has been documented extensively [18]. In a 2008 prospective study, Ahlering et al. [19] compared 38 patients receiving cautery nerve sparing with 50 receiving cautery-free cavernous nerve preservation. Selecting only patients <65 years of age who were preoperatively potent, the authors reported significant advantages in favor of athermal dissection 24 months after the procedures. In 2010, Samadi et al. [20] compared 590 patients who received an antegrade cautery nerve-sparing procedure using the bipolar device with two other groups of patients who underwent athermal dissection using clips and a “curtain” technique. In this study, including preoperatively potent patients, according to the SHIM questionnaire, with a mean age of 59 years old, the authors showed a statistically significant advantage only in favor of the athermal technique at 3 months follow-up. Any difference disappeared after 6 or 12 months postoperatively.
Considering the data coming from the clinical series reviewed, the mean potency rates at 3, 6, and 12 months were 44 %, 50 %, and 66 % (62–75 %), respectively, in the four series using monopolar or bipolar dissection and 52 %, 78 % (70–86 %), and 81 % (62–90 %), respectively, in the four studies using the athermal dissection. Interestingly, available data with longer follow-up showed a 24-month mean potency rate as high as 82 % (69–94 %) in patients who received cautery nerve sparing.
Nerve-Sparing Technique with Minimal Countertraction
It is well documented that subtle technical variation affects potency preservation during robot-assisted laparoscopic radical prostatectomy (RARP) . Most prostatectomy studies focus on achieving the optimal anatomic nerve-sparing dissection plane. However, these sections focus on how the assistant/surgeon neurovascular bundle (NVB) countertraction can impact the sexual function outcomes. Several authors have been able to correlate the effect of countertraction and erectile dysfunction (ED) after RARP. Mulhall et al. [21] identified NVB countertraction as a source of postprostatectomy neurogenic injury. Kaul et al. [22] asserted that endopelvic fascia sparing and delayed DVC ligation reduced NVB traction without mention of assistant or surgeon-specific technique as it relates to NVB tension.
Technique: With an aim of nerve sparing with minimal countertraction (NS-MC) , Kowalczyk et al. [13] modified their technique to avoid assistant/surgeon lateral countertraction to dissect the prostate away from the NVB instead of the NVB away from the prostate. Additionally, they decreased robotic scissors excursion with blunt dissection during intrafascial nerve sparing to attenuate tension on the NVB. NS-MC was associated with significantly higher sexual function scores at 5 months after RARP compared to NS countertraction (median: 20 vs 10; p < 0.001), been this difference more accentuated for bilateral intrafascial nerve sparing in preoperatively potent men.
New Developments in Minimally Invasive Dissection and Protection NVB During RARP
Human Amniotic Membrane Allograft Nerve Wrap Around the Prostatic Neurovascular Bundle
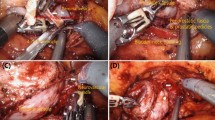
Clinical use of growth factors and anti-inflammatory substances for prostatic NVB regeneration is novel, and human amnion membrane allograft (dHACM) is a source of implantable neurotrophic factors and cytokines [23, 24]. Since 2014, we implemented a local application of this allograft for preoperatively potent men. The bilateral, retrograde, athermal NS RARP was performed in each patient (Fig. 6.9a), with bladder neck reconstruction, an anterior suspension stitch, and posterior reconstruction (Rocco stitch). There were 58 patients in this series, who were preoperatively continent (American Urological Association Symptom Score <10) and potent (Sexual Health Inventory for Men [SHIM] score >19) and underwent bilateral dHACM placement (AmnioFix; MiMedx Group, Marietta, GA, USA) at a cost of $900 per patient. The dHACM allograft was cut into two longitudinal pieces and placed over each NVB as a nerve wrap. The wrap was placed circumferentially around the NVB after extirpative RARP, postanastomosis (Fig. 6.9b).
This group was computer matched with a similar group of patients who did not receive allograft placement. Postoperative outcomes were analyzed between both groups, including time to return to continence, biochemical recurrence, and potency. Potency at 8 weeks returned in 65.5 % of the patients in the dHACM group and 51.7 % of the patients in the no-dHACM group. The mean time to potency was significantly shorter in the graft group (1.34 months) than in the nongraft group (3.39 months; p = 0.007) (Fig. 6.10). SHIM scores were also higher for the dHACM group than for the no-dHACM group (mean score 16.2 vs. 9.1). In conclusion, our short-term results are encouraging for patients undergoing full NS RARP and dHACM placement.
Instant Toggling of Endoscope During RARP
With the introduction of the da Vinci Xi robotic surgical system some of its new applications have been built to try to achieve a more precise sparing procedure. For instance, the laparoscope has a digital end-mounted camera for improved vision. The scope can be placed into any of the robotic arms and has autofocus. The new endoscope is used to see deep inside the body, is far easier to setup and delivers sharp, high-definition 3D images.
We implemented this advanced imaging for clear visualization of the neurovascular bundle to initiate its dissection. The use of maneuver to rotate the 3D camera with 30° lens angles up to 180° can facilitate a more direct view to identify a route of NVB in order to start releasing its dissection from posterior surface (Fig. 6.11a). It is essential to fully dissect the posterior plane up to the apex and laterally to the bundles. Once this is accomplished, early release of NVB can then be performed. At the level of the apex and midportion of the prostate, the avascular plane between the neurovascular bundle and prostatic fascia is developed with caution. Then, the monopolar scissors are used to create the window to separate the prostate from the bundle. By rotating the camera back, it is feasible to maintain an interfacial approach to dissect the anterior and lateral surface of the prostate preserving neurovascular bundle (Fig. 6.11b). Stepwise procedure includes gentle dissection with sweeping motions of scissors, clear identification of the landmark artery, and gentle dissection with preservation of the neurovascular bundle toward the plane of dissection initiated from the posterior surface before. The retrograde direction facilitates a more anatomical-based plane of dissection toward the prostatic pedicle. The path of the bundle is now delineated and focus can now turn to controlling the prostatic vascular pedicle.
Ultimately, this approach may provide the surgeon with guidance for exact placement of a first hem-o-lock clip to pedicle above the level of the released NVB. This technique allows complete NVB preservation without the use of any thermal energy, significant trauma, or inadvertent damage. Kumar et al. presented results of our first 20 patients using the instant toggling of endoscope during RARP. The mean time for NS was 12.3 min versus 18.1 min in standard procedure (p < 0.005). There were no intraoperative/postoperative complications.
The Application of Immunofluorescence as a Novel Optical Imaging Tool to Better Visualize Landmark Artery
Since 2010, a near-infrared fluorescence (NIRF) camera was integrated into the da Vinci Si and the Xi systems, creating a combination of technically and minimally invasive advantages that have been embraced by several experienced surgeons (Fig. 6.12). Commonly used as a contrast agent the Indocyanine Green (ICG) is a vital fluorescent dye characterized by excellent tolerability, few side effects, and low toxicity and allergic reactions. As a result of these characteristics, ICG have been utilized in several fields, in particular to assess microvascular circulation and organ vascularization.
Intraoperatively we injected intravenously 0.75 ml of ICG before pedicle ligation and NVB dissection. The time to target vasculature of prostate was 20–40 s. The technique allowed us to identify the landmark artery in 17/20 (85 %) patients (Fig. 6.13). In three patients we were unable to visualize the landmark artery due to large veins overlapping the view.
Penile Rehabilitation After Radical Prostatectomy
Despite the advantages of this new surgical approach, a significant proportion of patients might experience erectile dysfunction, with different degrees of severity.
PDE5 Inhibitors
Since Mulhall et al. [25] first reported the results of penile rehabilitation using sildenafil in 2005, clinical studies have reported that PDE5 inhibitors have protective effects on smooth muscle and endothelial cells, nerve-modulating effects, and inducing effects on corpus cavernosum oxygenation. When sildenafil was administered daily to 76 patients with normal erectile function who had undergone bilateral nerve-sparing radical prostatectomy 48 weeks earlier, the recovery rate of erectile function was 24 % in the 50 mg dose group, 33 % in the 100 mg dose group, and 5 % in the placebo group. Additionally, when sildenafil was administered to 40 male patients who had undergone bilateral nerve-sparing radical prostatectomies, and a biopsy was conducted before and 6 months after the surgery to compare the effect of sildenafil, no loss of the smooth muscle was seen in the 50 mg dose group, and increased smooth muscle tissue was seen in the 100 mg dose group [26]. Based on these results, we advise our patients to start penile rehabilitative treatment with PDE5 inhibitors soon after surgery.
Intracavernous Injection of Pro-erectile Compound
Intracavernous injection (ICI) of alprostadil represents a valid alternative for patients not responding to PDE5 inhibitors. Claro et al. [27] reported that when intracavernosal injection was conducted on patients who had normal sexual function before curative surgery, but who had postoperative erectile dysfunction, 40 % of the patients showed a good result, and 94.6 % showed erection sufficient to have sexual intercourse. The main disadvantage of ICI relies in the limited compliance to the treatment due to the secondary effects. Penile pain remains the major cause to abandon treatment [28].
Vacuum Constriction Devices
A previous clinical study on the treatment of erectile dysfunction following radical prostatectomy reported that when a vacuum constriction device (VCD) was used for 9 months after the surgery, 80 % of the patients were able to have sex using the device, but only 29 % of the control group members were able to have sex. Another study showed a decrease in penis length by 2 cm in patients who started to use the device 6 months after surgery compared with patients who used the device 1 month after surgery [29]. No large-scale, randomized, controlled study has been reported due to insufficient patient numbers, although we recommend this to our patients in order to prevent penis dystrophy. Chapter 9 discussed penile rehabilitation in more detail.
Published Results
In a multi-institutional prospective analysis of 8000 consecutive cases of robotic-assisted laparoscopic radical prostatectomy according to D’Amico risk criteria [30], the potency rate at 12 months follow-up was 88.4, 79.0, and 60 % in low, intermediate, and high-risk groups, respectively; however, there were no statistically significant differences. Moreover, the overall potency rate ranged from 32.7 to 96.6 %, and similarly, RRP had greater variation (32.7–81.3 %), whereas LRP (64.6 %) and RARP (69–96.6 %) achieved the greater rates. Ninety-four of the 300 patients received a bilateral NVB preservation during RARP, potency was achieved in 87.2 % of the cases.
Our group has also reported our outcomes after RARP. In terms of potency, Patel et al. [31] achieved a 96.6 % of 404 patients, over a follow-up period of 18 months.
Recently, Ficarra et al. [18] summarized results of systematic review and meta-analysis reporting potency rates after RARP when compared with retropubic radical prostatectomy (RRP) and laparoscopic radical prostatectomy (LRP) (Figs. 6.14 and 6.15). Although the initial RARP series showed 12-month potency rates ranging from 70 to 80 %, a lack of comparative studies did not permit any definitive conclusion about the superiority of this technique. Cumulative analyses showed better 12-month potency rates after RARP in comparison with RRP (odds ratio [OR]: 2.84; 95 % confidence interval [CI]: 1.46–5.43; p = 0.002) (Fig. 6.14). Only a nonstatistically significant trend in favor of RARP was reported after comparison with LRP (OR: 1.89; p = 0.21) (Fig. 6.15). This update, for the first time, demonstrated a significant advantage in favor of RARP in comparison with RRP in terms of 12-mo potency rates.
Conclusion
Nerve-sparing (NS) procedures RARP have demonstrated improved postoperative functional outcomes. We have demonstrated our technique of nerve sparing: athermal, early retrograde release, minimization of tension with identification of landmark artery. We have shown the role of our subjective NS regression model in predicting the recovery time of postoperative erectile function after RARP.
The surgeon’s experience and volume are the key determinants in NS RARP. The ICG and NIRF technology during NS RARP has the potential to identify LA accurately and improve the quality of NS. Use of instant toggling of endoscope using Xi da-Vinci robotic surgical system can improve quality of NS in challenging cases of RARP. The dHACM allograft can hasten early return of continence and potency in patients following RARP. However, further multi-institutional long-term randomized controlled trials are required to validate these new findings.
References
Walsh PC, Donker PJ. Impotence following radical prostatectomy: insight into etiology and prevention. J Urol. 1982;128:492–7.
Tewari A, Peabody JO, Fisher M, et al. An operatives and anatomic study to help in nerve sparing during laparoscopic and robotic radical prostatectomy. Eur Urol. 2003;44:444–54.
Flocks RH. The arterial distribution within the prostate gland: its role in transurethral prostatic resection. J Urol. 1937;37:524–48.
Clegg EJ. The arterial supply of the human prostate and semnal vesicles. J Anat. 1955;89:209–16.
Bilhim T, Pisco JM, Furtado A, et al. Prostatic arterial supply: demonstration by multirow detector angio CT and catheter angiography. Eur Radiol. 2011;21:1119–26.
Clegg EJ. The vascular arrangements within the human prostate gland. Br J Urol. 1956;28:428–35.
Lepor H, Gregerman M, Crosby R, Mostofi FK, Walsh PC. Precise localization of the autonomic nerves from the pelvic plexus to the corpora cavernosa: a detailed anatomical study of the adult male pelvis. J Urol. 1985;133:207–12.
Schatloff O, Chauhan S, Sivaraman A, Kameh D, Palmer K, Patel VR. Anatomic grading of nerve sparing during robot-assisted radical prostatectomy. Eur Urol. 2012;61:796–802.
Levinson AW, Pavlovich CP, Ward NT, Link RE, Mettee LZ, Su LM. Association of surgeon subjective characterization of nerve sparing quality with potency following laparoscopic radical prostatectomy. J Urol. 2008;179:1510–4.
Dubbelman YD, Dohle GR, Schroder FH. Sexual function before and after radical retropubic prostatectomy: a systematic review of prognostic indicators for a successful outcome. Eur Urol. 2006;50:711–20.
van der Poel HG, de Blok W. Role of extent of fascia preservation and erectile function after robot-assisted laparoscopic prostatectomy. Urology. 2009;73:816–21.
Coughlin G, Dangle PP, Palmer KJ, Samevedi S, Patel VR. Athermal early retrograde release of the neurovascular bundle during nervesparing robotic-assisted laparoscopic radical prostatectomy. J Robot Surg. 2009;3:13–7.
Kowalczyk KJ, Huang AC, Hevelone ND, et al. Stepwise approach for nerve sparing without counterattraction during robot-assisted radical prostatectomy: technique and outcomes. Eur Urol. 2011;60:536–47.
Alemozaffar M, Duclos A, Hevelone ND, et al. Technical refinement and learning curve for attenuating neurapraxia during robotic assisted radical prostatectomy to improve sexual function. Eur Urol. 2012;61:1222–8.
Ward JF, Zincke H, Bergstralh EJ, Slezak JM, Myers RP, Blute ML. The impact of surgical approach (nerve bundle preservation versus wide local excision) on surgical margins and biochemical recurrence following radical prostatectomy. J Urol. 2004;172:1328–32.
Palisaar RJ, Noldus J, Graefen M, Erbersdobler A, Haese A, Huland H. Influence of nerve-sparing (NS) procedure during radical prostatectomy (RP) on margin status and biochemical failure. Eur Urol. 2005;47:176–84.
Ko YH, Coelho RF, Sivaraman A, Schatloff O, Chauhan S, Abdul-Muhsin HM, et al. Retrograde versus antegrade nerve sparing during robotassisted radical prostatectomy: which is better for achieving early functional recovery? Eur Urol. 2013;63:169–77.
Ficarra V, Novara G, Ahlering T, et al. Systematic review and meta-analysis of studies reporting potency rates after robot-assisted radical prostatectomy. Eur Urol. 2012;61:418–30.
Ahlering TE, Rodriguez E, Skarecky DW. Overcoming obstacles: nerve-sparing issues in radical prostatectomy. J Endourol. 2008;22:745–50.
Samadi DB, Muntner P, Nabizada-Pace F, Brajtbord JS, Carlucci J, Lavery HJ. Improvements in robot-assisted prostatectomy: the effect of surgeon experience and technical changes on oncologic and functional outcomes. J Endourol. 2010;24:1105–10.
Mulhall JP, Slovick R, Hotaling J, et al. Erectile dysfunction after radical prostatectomy: hemodynamic profiles and their correlation with the recovery of erectile function. J Urol. 2002;167:1371–5.
Kaul S, Savera A, Badani K, Fumo M, Bhandari A, Menon M. Functional outcomes and oncological efficacy of Vattikuti Institute prostatectomy with veil of aphrodite nerve sparing: an analysis of 154 consecutive patients. BJU Int. 2006;97:467–72.
Liang H, Liang P, Xu Y, Wu J, Liang T, Xu X. DHAM-BMSC matrix promotes axonal regeneration and functional recovery after spinal cord injury in adult rats. J Neurotrauma. 2009;26:1745–57.
Quinlan DM, Nelson RJ, Partin AW, Mostwin JL, Walsh PC. The rat as a model for the study of penile erection. J Urol. 1989;141:656–61.
Mulhall J, Land S, Parker M, Waters WB, Flanigan RC. The use of an erectogenic pharmacotherapy regimen following radical prostatectomy improves recovery of spontaneous erectile function. J Sex Med. 2005;2:532–40.
Schwartz EJ, Wong P, Graydon RJ. Sildenafil preserves intracorporeal smooth muscle after radical retropubic prostatectomy. J Urol. 2004;171:771–4.
Claro J de A, de Aboim JE, Maríngolo M, Andrade E, Aguiar W, Nogueira M, et al. Intracavernous injection in the treatment of erectile dysfunction after radical prostatectomy: an observational study. Sao Paulo Med J. 2001;119:135–7.
Lakin MM, Montague DK, et al. Intracavernous injection therapy: analysis of results and complications. J Urol. 1990;143:1138–41.
Köhler TS, Pedro R, Hendlin K, Utz W, Ugarte R, Reddy P, et al. A pilot study on the early use of the vacuum erection device after radical retropubic prostatectomy. BJU Int. 2007;100:858–62.
Ou YC, Yang CK, Wang J, Hung SW, Cheng CL, Tewari AK, et al. The trifecta outcome in 300 consecutive cases of robotic-assisted laparoscopic radical prostatectomy according to D’Amico risk criteria. Eur J Surg Oncol. 2013;39:107–13.
Patel VR, Coelho RF, Chauhan S, et al. Continence, potency and oncological outcomes after robotic-assisted radical prostatectomy: early trifecta results of a high-volume surgeon. BJU Int. 2010;106(5):696–702.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Ogaya-Pinies, G., Mouraviev, V., Ganapathi, H., Patel, V. (2016). Technical Innovations to Optimize Early Return of Erectile Function. In: Razdan, S. (eds) Urinary Continence and Sexual Function After Robotic Radical Prostatectomy. Springer, Cham. https://doi.org/10.1007/978-3-319-39448-0_6
Download citation
DOI: https://doi.org/10.1007/978-3-319-39448-0_6
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-39446-6
Online ISBN: 978-3-319-39448-0
eBook Packages: MedicineMedicine (R0)