Abstract
Radioscapholunate (RSL) fusion is a partial wrist fusion for patients with localized arthritis of the wrist, such as those with Kienböck’s disease. An essential prerequisite is a well-preserved midcarpal joint, which can be confirmed on imaging, arthroscopy or intra-operatively. Cadaveric and clinical studies of RSL fusions demonstrate that excision of the distal scaphoid improves motion of a RSL fusion and has a better union rate. Other studies have also included excision of the triquetrum, demonstrating an increase in the radioulnar arc. There are a variety of fixation options, such as K-wires, staples, and plate fixation.
Long-term follow-up of our RSL fusions included three patients with Kienböck’s disease. Their outcomes were assessed using the visual analogue scale, Quick DASH, Mayo wrist score, measured ROM, and plain radiographs. All patients demonstrate good patient satisfaction, clinical outcomes, and preservation of the midcarpal articulation.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Avascular necrosis
- Distal scaphoid excision
- Fusion
- Kienböck’s disease
- Limited wrist fusion
- Long-term outcome
- Lunate
- Management
- Scaphoidectomy
- Surgical technique
- Radioscapholunate
- Wrist
Introduction
Radioscapholunate (RSL) fusion is a partial wrist fusion for localized disease with an intact midcarpal articulation. It is indicated for degenerative, inflammatory, post-traumatic, and Kienböck’s arthritis [1]. The midcarpal joint is preserved, which is responsible for the dart thrower’s motion, which is essential for daily use of a functional hand [2, 3].
Preoperative Assessment
Indications
If conservative modalities, such as modification of activities, analgesics, and use of a splint, have failed, su rgical management may be considered. It is essential to identify which joints are involved in the disease process. An absolute prerequisite for this procedure is a functional midcarpal articulation (Fig. 22.1), to achieve painless motion following the fusion [4]. In Kienböck’s disease, the RSL fusion can be performed where the cartilage deformities are limited to the proximal lunate and/or lunate facet. That is, cases with a Bain and Begg grade 1 or 2a (Fig. 22.2) [5].
Bain and Begg arthroscopic classification for Kienböck’s disease [1]. The grade is determined by the number of nonfunctional articular surfaces. The grading system assists the surgeon to determine the surgical treatment, based on the pathoanatomic findings. RSL fusion is indicated for grade 1 or 2a. Reproduced with permission Bain GI, Begg M. Arthroscopic assessment and classification of Kienböck’s disease. Tech Hand Up Extreme Surg. 2006, 10(1): 8–13
Imaging
Plain radiographs should be performed to determine the diagnosis and to assess the extent of the disease, including the status of the midcarpal joint. Computed tomography (CT) scan and magnetic reso nance imaging are also of value in determining the extent of the disease in the lunate, and the remainder of the carpus. Arthroscopy is the gold standard to determine the integrity of the articular surfaces. Intraoperative direct visualization of the articular cartilage can be the final decision as to whether or not to proceed with the limited fusion.
Fixation
There are many described methods of fixation for RSL fusion. These include K-wires, staples, plates, and screws [1, 6–9]. We used a set of principles when performing limited wrist fusions (Table 22.1) [1]. The insertion of K-wires allows for simple and accurate positioning to avoid impingement, however they do not offer compression. Non-locking plates have been associated with dorsal impingement, loss of fixation, and nonunion [8, 9]. We have used memory staples (Depuy International Ltd., Leeds, UK) as they are low profile and provide dynamic compress across the fusion site (Fig. 22.3a–c) [10]. Fixation devices with greater stability allow for earlier mobilization of the wrist.
(a) Cadaveric model of RSL fusion using memory staples. (b) Excision of the distal scaphoid increases flexion an d radial deviation. (c) Excision of the distal scaphoid and triquetrum increases extension and ulnar deviation. Reproduced with permission Bain GI, Sood A, Yeo CJ. RSL Fusion with excision of distal scaphoid and triquetrum: a cadaveric study. J Wrist Surg. 2014; 3(1): 37–41. Copyright © 2014, Rights Managed by Georg Theime Verlag KG Stuttgart, New York
Types of Fusion
Radioscapholunate Fusion
Surgical Technique
A dorsal approach via the third extensor compartment is used to expose the carpus. Some authors recommend excision of the posterior interosseous nerve, however we prefer to leave it intact to optimize proprioception . Using hand held curettes and rongeurs, the joint surfaces of the proximal scaphoid, lunate, and distal radius are thoroughly debrided. We avoid power instruments that may burn the bone. Using a closing fusion technique the radiocarpal fusion mass is stabilized (Fig. 22.4). That is, the full thickness of the articular surfaces are excised to allow the osseous structures to close [1]. To obtain a good long-term outcome, it is important to create a “stand-alone joint” which can potentially obtain a good long term outcome. Therefore the midcarpal joint surface of the scaphoid and lunate are perfectly aligned. We reduce the scapholunate interval, and stabilize it with 2 × 1.1 mm K-wires. Bone graft from the iliac crest is used to supplement the fusion mass.
(a) Open fusion techniq ue maintains height. (b) Closing fusion allows for bony apposition, stability, and increased union rate. Reproduced with permission from Bain GI, McGuire DT. Decision making for partial carpal fusions. J Wrist Surg. 2012, 1(2): 103–114. Copyright © 2012, Rights Managed by Georg Thieme Verlag KG Stuttgart, New York
The radiocarpal joint is then stabilized in 15° of extension, in order to achieve maximum extension and grip strength. The fusion site is stabilized using one of the methods described earlier (see Fig. 22.3a). Intraoper ative fluoroscopy is used to confirm the position of the fusion mass and the internal fixation.
A plaster slab is then applied and the patient encouraged to elevate the arm and mobilize the fingers. At 1 week, a full cast or removable splint is applied, depending upon patient factors and the f ixation. At 6 weeks the wrist is mobilized with graduated wrist strengthening and motion exercises.
Results
Variable rates of nonunion have been recorded between 0 and 25 % [4, 11, 12]. This is thought to be due to the scaphoid acting as a long lever and increasing pressure through the fusion mass [1].
The patients usually obtain good pain relief; however, there is a reduction in wrist range of motion. Normally the scaphoid flexes during wrist flexion and radial deviation. Thus, a fused radioscaphoid joint will mostly affect wrist movement in these two directions. The range of motion is 33–40 % of the normal wrist [12, 13], with a 40–50° flexion–extension (F-E) arc, and 21–28° radial–ulnar (R-U) arc [8, 14, 15].
A long-term study by Nagy and Büchler reported an undesirable high complication rate with RSL fusion. Five of their 15 patients (33 %) required a full wrist fusion at a mean of 8 years. Average range of motion was 18° flexion, 32° extension, 25° ulnar, and 3° radial deviation. More than half developed midcarpal arthritis and 27 % had a nonunion. Good results were reported for only seven (47 %) of their patients [8].
Shin and Jupiter reviewed a series of five patients with two angled 2.4 mm distal radius locking plates across the fusion mass to achieve complete union in all patients. Functional outcome was not reported [11].
RSL with Distal Scaphoid Excision
RSL fusion can be performed with excision of the distal scaphoid (see Fig. 22.3b), which can be used as bone graft. Clinical studies have reported that adding excision of the distal scaphoid improved motion [13], lowered the rate of nonunion [6] and midcarpal arthritis [16].
A cadaveric study by McCombe et al. demonstrated that excision of the distal scaphoid increased in the mean F-E arc from 60° to 122° and R-U deviation from 34° to 43° [13]. A similar study by Bain et al. reported that excision of the distal scaphoid reduced the long lever arm of the scaphoid and unlocked the midcarpal joint to increase wrist flexion and radial deviation (Table 22.2) [17].
Garcia-Elias et al. completed a review of 16 patients with RSL fusion and distal scaphoidectomy and reported improvement in pain, flexion, and radial deviation compared to previous studies with RSL fusions only. They reported no nonunions and a lower rate of midcarpal arthritis [12].
RSL with Distal Scaphoid and Triquetrum Excision
Excision of the triquet rum decreases the containment of the midcarpal joint, and therefore increases the joint motion (see Fig. 22.3c and Table 22.2) [17, 18]. The triquetrum is the best bone graft as the scaphoid is often sclerotic.
Cadaveric studies have been published on the effect of additional triquetrectomy to RSL fusion and distal scaphoid excision. Bain et al. reported that excision of the triquetrum will improve the R-U arc by a further 21 % compared to RSL and distal scaphoidectomy alone (Table 22.3) [17].
Berkhout et al. reported that the RSL fusion decreased the range of motion in all directions [14]. They reported excision of the scaphoid typically improves the F-E arc, while R-U deviation is most improved after excision of the triquetrum.
We have performed a minimum 10-year follow-up study of our RSL fusions, which include excision of the distal scaphoid and triquetrum in 24 patients. A mean follow-up of 14.7 years found these patients to have a strong trend toward a greater R-U arc than RSL fusion alone and RSL fusion with scaphoidectomy. There were no nonunions and radiological results showed preservation of the midcarpal joint. Pain scores progressively improved from pre-operation, to 2 years to 10 years following surgery. Patient satisfaction rate was 94 %.
Long-Term Follow-Up of RSL Fusion in Kienböck’s Disease
Of the 24 patients who had a RSL fusion, three patients had Kienböck’s disease. They were all either Bain and Begg grade 2a or 1. One patient underwent RSL fusion, while two had RSL fusion with distal scaphoidectomy.
Patient 1
Patient 1 is a 61-year-old female who had a RSL fusion with K-wires and staples to her nondominant wrist. Preoperatively, she had visual analogue scale (VAS) pain score of 4/10.
Six months post-operatively, plain radiographs demonstrated union of the fusion. At 18.4 years she was satisfied, with VAS pain score 0/10. Quick DASH score 6.8/100 and Mayo wrist score 85/100, which is graded as a good.
Patient 2
Patient 2 is a 55-year-old male who had a RSL fusion with excision of the distal scaphoid. Once the necrotic part of the lunate was excised, the remaining lunate was thought to be too small for staples, and was therefore stabilized with K-wires. The K-wires were removed at 15 weeks. By 7 months he had return to full-time work with restricted duties.
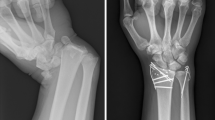
At 17.7 years he was satisfied with VAS score 0/10, Quick DASH 11.4/100, and Mayo Wrist score 65 was satisfactory. Plain radiographs demonstrated a solid fusion and preservation of the midcarpal joint (Fig. 22.5).
Patient 3
Patient 3 is a 72-year-old male who also had a RSL fusion with excision of his distal scaphoid on his dominant wrist, using staples. In view of the associated ulnar wrist pain symptoms, a matched hemi-resection of the distal ulna was also performed.
At 17.5 years follow-up he was satisfied with VAS pain score 1/10, Quick DASH 29.5/100 and Mayo wrist score 60. Plain radiographs confirmed union with preservation of the midcarpal articulation (Fig. 22.6a) and normal alignment (see Fig. 22.6b).
For the three Kienböck’s patients, the mean F-E arc was 46.6° and R-U deviation arc 20.8°. There were no nonunions or other complications and none of them required a full wrist fusion. The mean scaphocapitate and lunocapitate joint spaces measured 2.0 mm and 1.7 mm respectively, reflecting negligible progression to midcarpal arthritis.
Clearly this is a small cohort; however, with such a long follow-up these results are certainly pleasing. We attribute the good results to:
-
1.
Closely applied indications for surgery, in particular a well-preserved midcarpal joint.
-
2.
Following the principles of limited wrist fusion (see Table 22.1) [1].
-
3.
That a perfect reduction of the midcarpal joint is obtained.
-
4.
Good stability of the radiocarpal joint until union.
As the reader would note, we began performing the RSL fusion for Kienböck’s disease many years ago, in this very specific pati ent cohort. Since then newer methods of investigation have been introduced, such as gadolinium-enhanced MRI, which may further narrow the indication for this procedure.
Conclusion
RSL fusion is indicated for patients with localized arthritis of the wrist with an intact midcarpal articulation. This procedure can include excision of the distal scaphoid and triquetrum, which increases the motion and union rate. Long-term outcome studies have shown RSL fusion to be sustainable with good clinical and radiological outcomes in those patients in which the midcarpal joint is anatomically reduced and fusion mass well stabilized.
References
Bain GI, McGuire DT. Decision making for partial carpal fusions. J Wrist Surg. 2012;1(2):103–14.
Crisco JJ, Coburn JC, Moore DC, Akelman E, Weiss SP, Wolfe SW. In vivo radiocarpal kinematics and the dart thrower’s motion. J Bone Joint Surg Am. 2005;87:2729–40.
Wolfe SW, Crisco JJ, Orr CM, Marzke MW. The dart-throwing motion of the wrist: is it unique to humans? J Hand Surg Am. 2006;31:1429–37.
Bain GI, Ondimu P, Hallam P, Ashwood N. Radioscapholunate arthrodesis - a prospective study. Hand Surg. 2009;14(2–3):73–82.
Bain GI, Begg M. Arthroscopic assessment and classification of Kienböck’s disease. Tech Hand Upper Extrem Surg. 2006;10(1):8–13.
Mühldorfer-Fodor M, Ha HP, Hohendorff B, Löw S, Prommersberger KJ, Van Schoonhoven J. Results after radioscapholunate arthrodesis with or without resection of the distal scaphoid pole. J Hand Surg Am. 2012;37(11):2233–9.
Ishikawa H, Murasawa A, Nakazono K. Long-erm follow-up study of radiocarpal arthrodesis for the rheumatoid wrist. J Hand Surg Am. 2005;30:658–66.
Nagy L, Buchler U. Long-term results of radioscapholunate fusion following fractures of the distal radius. J Hand Surg Br. 1997;22(6):705–10.
Mulford JS, Ceulemans LJ, Nam D, Axelrod TS. Proximal row carpectomy vs four corner fusion for scapholunate (Slac) or scaphoid nonunion advanced collapse (Snac) wrists: a systematic review of outcomes. J Hand Surg Eur Vol. 2009;34:256–63.
Bain GI, Watts AC. The outcome of scaphoid excision and four-corner arthrodesis for advanced carpal collapse at a minimum of ten years. J Hand Surg Am. 2010;35(5):719–25.
Shin EK, Jupiter JB. Radioscapholunate arthrodesis for advanced degenerative radiocarpal osteoarthritis. Tech Hand Up Extrem Surg. 2007;11(3):180–3.
Garcia-Elias M, Lluch A, Ferreres A. Treatment of radiocarpal degenerative osteoarthritis by radioscapholunate arthrodesis and distal Scaphoidectomy. J Hand Surg Am. 2005;30:8–15.
McCombe D, Ireland DCR, McNab I. Distal scaphoid excision after radioscaphoid arthrodesis. J Hand Surg Am. 2001;26:877–82.
Berkhout MJ, Shaw MN, Berglund LJ, An KN, Berger RA, Ritt MJ. The effect of radioscapholunate fusion on wrist movement and the subsequent effects of distal scaphoidectomy and triquetrectomy. J Hand Surg Eur Vol. 2010;35(9):740–5.
Bach AW, Almquist EE, Newman DM. Proximal row fusion as a solution for radiocarpal arthritis. J Hand Surg Am. 1991;16(3):424–31.
Hug U, Guggenheim M, Kilgus M, Giovanoli P. Treatment of radiocarpal degenerative osteoarthritis by radioscapholunate arthrodesis: long-term follow-up. Chir Main. 2012;31(2):71–5.
Bain GI, Sood A, Yeo CJ. RSL fusion with excision of distal scaphoid and triquetrum: a cadaveric study. J Wrist Surg. 2014;3(1):37–41.
Bain GI, Sood A, Ashwood A, Turner PC, Fogg G. Effect of scaphoid and triquetrum excision on limited arthrodesis of the wrist: a laboratory study. J Hand Surg Eur Vol. 2009;34:614–7.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Ha, N.B., Phadnis, J., Bain, G.I. (2016). Radioscapholunate Fusion in Kienböck’s Disease. In: Lichtman, D., Bain, G. (eds) Kienböck’s Disease. Springer, Cham. https://doi.org/10.1007/978-3-319-34226-9_22
Download citation
DOI: https://doi.org/10.1007/978-3-319-34226-9_22
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-34224-5
Online ISBN: 978-3-319-34226-9
eBook Packages: MedicineMedicine (R0)