Abstract
Over the course of the past several decades treatment of peripheral arterial disease (PAD) has changed in North America. Advent of new technology has led to a shift in the initial treatment of both intermittent claudication (IC) and critical limb ischemia (CLI) towards endovascular intervention—including percutaneous balloon angioplasty, stenting and atherectomy. Overall increase in interventions for PAD correlates with a surge in the number of endovascular procedures performed by interventional cardiologists, interventional radiologists and vascular surgeons. Changes in reimbursement patterns has led to a trend towards these procedures being performed in an outpatient or office setting. Although this has resulted in fewer cases being performed in the hospital potential cost saving has been offset by increased use of the more highly reimbursed atherectomy in the outpatient setting. With regard to recommendations on how to treat these patients the Society of Vascular Surgery (SVS) has recently published guidelines for the treatment of IC emphasizing the importance of initial conservative medical management. There continues to be significant equipoise in the treatment of CLI across North America leading to tremendous variability in the use of open surgery and endovascular therapy. Guidance for the future treatment of CLI is partially dependent upon the Best Endovascular versus Surgical Therapy in Patients with Critical Limb Ischemia (BEST-CLI) trial, a randomized, controlled trial currently accruing patients in North America.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Peripheral Arterial Disease
- Endovascular Intervention
- Critical Limb Ischemia
- Intermittent Claudication
- Endovascular Therapy
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Practice Patterns
Over the course of the last decade, the total number of lower extremity vascular interventions have nearly doubled, while amputation rates have diminished [1]. Endovascular therapy of PAD, to treat both IC and CLI, has become more common as first line treatment in North America [2–4]. An analysis of the Medicare database revealed that over a 10 year period (1996–2006), Medicare beneficiaries had a more than threefold increase in endovascular interventions for lower extremity PAD and an associated almost half-fold decrease in surgical bypass [1].
Increasing utilization of endovascular therapy in North America has led to increased costs. A charge analysis within the National (Nationwide) Inpatient Sample (NIS) from 1997 to 2007 demonstrated an increase in the average cost for endovascular intervention for both IC ($8670–$14,084) and CLI ($13,903–$23,196). The average cost per procedure for endovascular intervention was higher than for bypass in both IC ($13,903 vs $12,681; P = 0.02) and CLI ($23,196 vs $22,910; P = 0.04) cohorts [5, 6]. In addition, there has been a significant regional variation in spending on vascular care with regions most aggressively using endovascular therapy having highest costs but not necessarily lowest regional amputation rates [6].
In the past, endovascular procedures were mostly performed by interventional radiologists, while vascular surgeons performed open vascular surgery such as endarterectomy and bypass and interventional cardiologists focused on treating the heart. Over the course of the past two decades, this pattern has shifted to endovascular procedures being mostly performed by cardiologists, who expanded their practice to the periphery, and vascular surgeons, who acquired endovascular skills [1, 7]. Endovascular skills were learned by established vascular surgeons who sought out 1–3 month “mini-endovascular fellowships” while incorporation of endovascular training into the formal vascular fellowship made these procedures a mandatory part of vascular fellowship accreditation [8].
Analysis of specific provider endovascular practice patterns in the State Inpatient Databases for New Jersey (2003–2007) revealed that interventional cardiologists, in comparison with vascular surgeons, were more likely to treat patients with IC (80.7 % vs 60.7 %, P = 0.002) and less likely to treat patients with rest pain (6.2 % vs 16.0 %, P = 0.002) or tissue loss (13.1 % vs 23.3 %, P = .002). Stent use was similar. Cardiologists had higher hospital ($49,748 vs $42,158, P < 0.0001) and supply/equipment ($19,128 vs $12,737, P < 0.0001) charges. Finally, only 10.7 % of cardiologists, compared with 36.8 % of vascular surgeons (P < 0.05), were classified as high volume practitioners [9].
Ambulatory Practice
In 2008, the Centers of Medicare and Medicaid Services (CMS) changed the reimbursement rates for endovascular interventions to encourage more of these procedures to be performed in the outpatient setting to avoid higher costs associated with inpatient procedures. The focus was originally on the percutaneous treatment of venous disease, however it was expanded to the treatment of PAD. This has resulted in an increased volume of endovascular interventions in the outpatient, office based setting. Overall the shift from the inpatient to the outpatient facilities consisted of approximately 25 % of cases which resulted in a fivefold increase in outpatient treatment. This shift correlated with a concomitant increase in physician ownership of outpatient intervention rooms where these procedures were performed. The use of atherectomy, which has higher reimbursement than angioplasty, has also significantly increased in the outpatient setting from 7 to 125 procedures per 100,000 Medicare beneficiaries in 2003 and 2011, respectively. This change has occurred despite a lack of evidence supporting improved efficacy of this technique and was most likely due to increased reimbursement [10]. The expected savings from performing endovascular procedures in the inpatient setting may have been partially offset by the increased use of the more expensive atherectomy procedures [10].
An example of this phenomenon is highlighted by a physician practice in Michigan that documented a greater than twofold increase in treating patients in the outpatient setting from May 2006–April 2007 (period 1) to June 2007–May 2008 (period 2). There was a concomitant increase in office based endovascular cases from 1.5 % during period 1 to 31 % in period 2. This led to a fivefold increase in revenue to the group from these procedures. No deaths or amputations occurred as a result of procedures performed in the office. Total payment by Medicare, payment to the hospital and to the physicians were higher in all the cases [11].
Analysis of the New York State Inpatient Hospitalizations and Outpatient Surgeries Discharge Databases from 1998 through 2007 was used to assess changes in practice patterns. There was a threefold increase in endovascular revascularization procedures performed in an outpatient setting. Outpatient data analysis revealed a fivefold increase in vascular intervention for IC and CLI. The number of endovascular interventions doubled for IC and quadrupled for CLI. Notwithstanding, patient comorbidities treated in 2006 were substantially greater than those in the previous decade while cardiac and bleeding complications have significantly decreased [12].
Recommendations for Treating Intermittent Claudication
The SVS, the most prominent vascular society in North America, recently published consensus guidelines for the treatment of IC. A limited amount of level 1 evidence was cited to guide decisions [13]. Emphasis was placed on risk factor modifications including smoking cessation, medical therapies and increasing the use of exercise programs to improve both cardiovascular and functional status for patients with PAD. Screening for PAD with non-invasive studies was not recommended. For patients with a suspicion for IC, non-invasive studies using some combination of ankle brachial indices, toe pressures, pulse volume recordings and doppler studies were recommended upon initial evaluation. If initial non-invasive studies were normal then an exercise study was recommended. Additional imaging was only recommended if an intervention was planned.
The guidelines further suggested that initial treatment for symptomatic IC should consist of medical therapy and risk factor reduction. This includes smoking cessation, statin therapy, optimization of diabetes management, single agent antiplatelet therapy and medications such as cilostazol, pentoxyfylline, and ramipril, when not contraindicated. An exercise program was recommended at a minimum of three sessions per week for at least 12 weeks when possible. Revascularization for IC was thought to be appropriate for selected patients with disabling symptoms after a careful risk-benefit analysis. Invasive treatments for IC should provide a predictable functional improvement with a reasonable durability. The recommended minimum threshold of a >50 % likelihood of sustained efficacy for at least 2 years was suggested as the benchmark and anatomic patency was considered a prerequisite for sustained revascularization efficacy. Endovascular approaches were preferred for most candidates with aorto-iliac disease and for select patients with femoro-popliteal disease when anatomic durability was expected. Factors thought to limit endovascular durability included extensive calcification, small-caliber arteries, diffuse infrainguinal disease and poor runoff and, as such, supported the use surgical bypass which was also recommended to those who failed endovascular intervention. Common femoral artery disease was advised to be treated surgically and saphenous vein was suggested as preferred conduit for infrainguinal bypass grafting. Regular follow up in patients undergoing intervention was advised [13].
Critical Limb Ischemia: Unresolved Challenges
Patterns of treatment for CLI vary widely across North America and there is a paucity of good quality scientific evidence to guide clinical practice. The Bypass vs. Angioplasty in Severe Ischaemia of the Leg (BASIL) trial, the only randomized, controlled trial (RCT), in this space was a valiant attempt to create an evidence based standard of care but failed to do so due to numerous shortcomings including use of a suboptimal primary endpoint, lack of lesion standardization, adequate power and limitation of intervention in the endovascular arm to angioplasty alone.
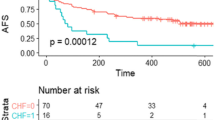
In October of 2013 the United States National Institutes of Health (NIH) funded the BEST-CLI trial. This prospective, multicenter, open label, superiority RCT initiated recruitment in the autumn of 2014 and aims to enroll 2100 patients at 140 sites in North America. This trial will compare treatment efficacy, functional outcomes and total cost in patients with CLI and infrainguinal PAD undergoing best open surgical or best endovascular revascularization. As such, BEST-CLI focuses on patients who are candidates for both infrainguinal bypass and endovascular therapy. It is designed as a pragmatic trial in that the definition of best therapy is left up to the individual investigator. All commercially available standard of care endovascular therapies are allowed, as are all surgical bypass techniques and types of conduit. At the risk of increasing heterogeneity, this feature will keep the trial relevant to clinical practice, over time. The BEST-CLI has a two-cohort design. The first cohort will evaluate outcomes in patients who have adequate single segment great saphenous vein (SSGSV) available for bypass, while the second cohort will include patients without adequate SSGSV. Since quality of conduit is paramount to infrainguinal bypass success Cohort 1 will compare bypass with best conduit to endovascular therapy. The question of how bypass with suboptimal conduit compares with endovascular therapy will be answered within Cohort 2. In each cohort, subjects will be randomized within four strata defined by two dichotomous factors based on clinical presentation (ischemic rest pain alone vs. tissue loss) and anatomical classification (presence or absence of significant tibial disease). The primary endpoint in the BEST-CLI is Major Adverse Limb Event (MALE)-free survival. Other endpoints include amputation-free survival, reintervention and amputation free survival, which incorporates MALE and minor reinterventions and freedom from hemodynamic failure, which evaluates the end result of enhanced limb perfusion. Lastly, BEST-CLI includes a robust health related quality of life and cost effectiveness analysis [14].
References
Goodney PP, Tarulli M, Faerber AE, Schanzer A, Zwolak RM. Fifteen-year trends in lower limb amputation, revascularization, and preventive measures among medicare patients. JAMA Surg. 2015;150(1):84–6.
Siracuse JJ, Giles KA, Pomposelli FB, Hamdan AD, Wyers MC, Chaikof EL, Nedeau AE, Schermerhorn ML. Results for primary bypass versus primary angioplasty/stent for intermittent claudication due to superficial femoral artery occlusive disease. J Vasc Surg. 2012;55(4):1001–7.
Siracuse JJ, Gill HL, Cassidy SP, Messina MD, Catz D, Egorova N, Parrack I, McKinsey JF. Endovascular treatment of lesions in the below-knee popliteal artery. J Vasc Surg. 2014;60(2):356–61.
Gallagher KA, Meltzer AJ, Ravin RA, Graham A, Shrikhande G, Connolly PH, Aiello F, Dayal R, McKinsey JF. Endovascular management as first therapy for chronic total occlusion of the lower extremity arteries: comparison of balloon angioplasty, stenting, and directional atherectomy. J Endovasc Ther. 2011;18(5):624–37.
Sachs T, Pomposelli F, Hamdan A, Wyers M, Schermerhorn M. Trends in the national outcomes and costs for claudication and limb threatening ischemia: angioplasty vs bypass graft. J Vasc Surg. 2011;54(4):1021–31.
Goodney PP, Travis LL, Brooke BS, DeMartino RR, Goodman DC, Fisher ES, Birkmeyer JD. Relationship between regional spending on vascular care and amputation rate. JAMA Surg. 2014;149(1):34–42.
Goodney PP, Beck AW, Nagle J, Welch HG, Zwolak RM. National trends in lower extremity bypass surgery, endovascular interventions, and major amputations. J Vasc Surg. 2009;50:54.
Assi R, Dardik A. Endovascular training of vascular surgeons in the USA. Ann Vasc Dis. 2012;5(4):423–7.
Vogel TR, Dombrovskiy VY, Carson JL, Haser PB, Graham AM. Lower extremity angioplasty: impact of practitioner specialty and volume on practice patterns and healthcare resource utilization. J Vasc Surg. 2009;50(6):1320–4.
Jones WS, Mi X, Qualls LG, Vemulapalli S, Peterson ED, Patel MR, Curtis LH. Trends in settings for peripheral vascular intervention and the effect of changes in the outpatient prospective payment system. J Am Coll Cardiol. 2015;65(9):920–7.
Jain KM, Munn J, Rummel M, Vaddineni S, Longton C. Future of vascular surgery is in the office. J Vasc Surg. 2010;51:509–13.
Egorova NN, Guillerme S, Gelijns A, Morrissey N, Dayal R, McKinsey JF, Nowygrod R. An analysis of the outcomes of a decade of experience with lower extremity revascularization including limb salvage, lengths of stay, and safety. J Vasc Surg. 2010;51(4):878–85. 885.
Society for Vascular Surgery Lower Extremity Guidelines Writing Group, Conte MS, Pomposelli FB, Clair DG, Geraghty PJ, McKinsey JF, Mills JL, Moneta GL, Murad MH, Powell RJ, Reed AB, Schanzer A, Sidawy AN, Society for Vascular Surgery. Society for vascular surgery practice guidelines for atherosclerotic occlusive disease of the lower extremities: management of asymptomatic disease and claudication. J Vasc Surg. 2015;61 Suppl 3:2S–41S.
Farber A, Rosenfield K, Menard M. The BEST-CLI trial: a multidisciplinary effort to assess which therapy is best for patients with critical limb ischemia. Tech Vasc Interv Radiol. 2014;17(3):221–4.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Siracuse, J.J., Farber, A. (2017). Vascular Surgery in North America: Current Perspectives in Peripheral Arterial Disease. In: Dardik, A. (eds) Vascular Surgery. Springer, Cham. https://doi.org/10.1007/978-3-319-33745-6_15
Download citation
DOI: https://doi.org/10.1007/978-3-319-33745-6_15
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-33743-2
Online ISBN: 978-3-319-33745-6
eBook Packages: MedicineMedicine (R0)