Abstract
Radiation therapy is a key component of combined modality therapy for Hodgkin’s lymphoma. In an effort to improve the therapeutic ratio and prevent late effects, radiation fields designed to encompass entire lymph node regions have recently been replaced with conformal methods of target volume delineation, known as involved-site radiation therapy (ISRT) and involved-node radiation therapy (INRT). Due to an increased risk of marginal misses with these new approaches, FDG-PET has become a critical aspect of modern radiation therapy planning, given its ability to identify areas of disease overlooked on CT. However, there are many challenges inherent to using PET for radiation planning. The current standard is a qualitative visual method, whereby PET/CT images are fused to the planning CT and the radiation oncologist contours target volumes using information from both image sets. Although not always possible, this method is best applied with input from an experienced radiologist or nuclear medicine physician given the complex nature of PET imaging and high rates of false positives. Due to a significant degree of inter- and intra-observer variability with this method, an effort has been made to explore the use of automated segmentation methods, which vary from simple standardized uptake value (SUV) cutoffs to more complex algorithms that incorporate signal-to-background ratios and sophisticated edge detection methodologies. This chapter covers the role of PET/CT in radiation planning for HL including automated and semiautomated contouring methods and the common pitfalls and artifacts in PET that are relevant when applied to radiation planning.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Standardize Uptake Value
- Plan Target Volume
- Brown Adipose Tissue
- Clinical Target Volume
- Gross Tumor Volume
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
5.1 History of Radiation Therapy in Hodgkin’s Lymphoma
Only seven years after Wilhelm Conrad Röntgen discovered X-rays in 1895, the first documented case of Hodgkin’s lymphoma (HL) was treated with radiotherapy [40]. William Allen Pusey, a professor of dermatology at the University of Illinois, had been using X-rays to treat a variety of dermatologic conditions. A 4-year-old boy with enlarged cervical lymph nodes “the size of a fist” was referred to Dr. Pusey and after irradiation the mass remarkably diminished to the size of an almond. In an era when there were no successful cancer therapies, 40 years before the introduction of chemotherapy, Dr. Pusey and colleagues marveled at this seemingly magical response. Radiation was offered to subsequent patients with HL over the next few years, and although a response to therapy was almost always demonstrated, the treatment was palliative. Primitive treatment machines were only capable of delivering low energy X-rays and the disease inevitably recurred.
In the early 1920s, kilovoltage equipment was developed. This allowed higher doses of radiation therapy to penetrate deeper into tissue with more skin-sparing effects. René Gilbert, a Swiss radiologist, was the first to report durable responses in treating patients with HL using kV X-rays with larger treatment fields that also included lymph node regions that were not obviously involved with disease. A number of patients treated in this way had a remarkable long-term survival [15], and by the 1950s, Vera Peters at the Ontario Institute of Radiotherapy had studied enough patients to report that early-stage HL can be cured with fractionated radiation therapy using large fields [39]. By the 1970s it had been established that the standard of care for early-stage HL was RT with fields aimed at all of the clinically relevant lymph node regions of the body [25]. Around this time, outcomes for advanced disease were further improved with the introduction of multi-agent chemotherapy regimens [11]. Radiation remains one of the most effective modalities for the treatment of HL as lymphomas and lymphatic tissue in general are highly radiosensitive. It is well known that the sensitivity of cells to radiation is proportional to the degree of proliferative activity and inversely proportional to the degree of differentiation. In other words, undifferentiated cells with high mitotic capability, such as the cells within malignant nodes in HL, are more likely to be radiosensitive. Of course, other factors play a role, including the oxygen concentration (hypoxic tumors are less sensitive to radiation) and inherent cellular response to DNA damage.
Over the last 40 years, radiation delivery techniques have continued to improve. This allowed for a more uniform dose distribution and better-targeted therapy. Advances were seen in other disciplines as well – more effective and less toxic multi-agent chemotherapy agents were developed, there were vast improvements in radiographic imaging, we obtained a better understanding of prognostic factors, and after rigorous study we made strides toward tailoring therapy based on stage and risk classification. In the modern era, early-stage HL is commonly treated with combined chemotherapy and radiation. Advanced disease is generally treated with more intensive chemotherapy regimens, while RT is reserved for bulky masses or areas of residual disease after chemotherapy. Today with combined modality treatment, HL has one of the highest cure rates of all malignancies with long-term survival over 80 %.
Unfortunately these high cure rates have come with a price. The majority of HL patients are children or young adults and late effects of treatment can be devastating and has an impact on survival. Two of the most significant late effects include development of secondary malignancy and cardiovascular disease [1, 3, 6]. It is felt that the risk of developing a radiation-induced secondary malignancy is related to both dose and field size. In a retrospective study of patients treated for HL, death caused by heart disease was exceeded only by death caused by HL and other neoplasms. Mediastinal irradiation increases the risk of subsequent death from heart disease, and this risk increases with total dose delivered to the mediastinum, minimal cardiac blocking, and young age at treatment [21].
Radiation continues to have an important role in ensuring locoregional control and improving overall outcome in the combined modality treatment approach for HL, but efforts have been made to minimize treatment judiciously in order to lower the impact of late effects on morbidity and mortality. One of the most dramatic ways in which we have scaled back treatment has been the reduction in radiation field size as we move away from elective nodal irradiation with involved field radiation to more targeted conformal approaches with involved-node and involved-site radiotherapy. Central to this paradigm shift have been improvements in radiation delivery techniques, including the incorporation of FDG-PET/CT into the design of radiation treatment fields.
Although multiple radiopharmaceuticals exist, 18F-FDG is the most widely available and widely used radiopharmaceutical in oncology including in HL. Therefore 18F-FDG will be the focus of this text. PET/CT has proven its value in staging for HL as well as in evaluating treatment response and has been increasingly used as an imaging method for the planning of radiation therapy for lymphomas.
5.2 Evolution of Radiation Treatment Fields
Historically lymphoma was managed with extended fields that encompassed all of the lymph node regions in the body, given the possibility of microscopic extension of disease outside the areas of palpable disease as well as reports of distant recurrences after local radiotherapy alone. These traditional extended fields are illustrated in Fig. 5.1. A mantle field includes the lymph node regions above the diaphragm and the inverted-Y field includes the lymph node regions in the abdomen and pelvis. When an inverted-Y field was combined with mantle field radiation, the combination was referred to as total nodal irradiation. At the time, single-modality radiation was preferred over the mechlorethamine, vincristine (Oncovin), procarbazine, and prednisone (MOPP) regimen of chemotherapy given its high rates of sterility and secondary leukemia, and chemotherapy was reserved for cases of disease refractory to RT. Radiation was delivered with linear accelerators using two-dimensional planning. 2-D planning makes use of an X-ray simulator and a two-dimensional treatment planning system used for calculation of dose distribution after the radiation oncologist defines treatment fields based on bony anatomy.
In the 1980s, computerized tomography (CT) revolutionized the imaging of tumors. CT scans were not only helpful for the radiation oncologist because they allowed for a better understanding of the tumor and normal tissue in 3-dimensions, but by the 1990s, CTs also became a critical component of treatment planning and a routine part of cancer management. An additional advantage of CT scan for radiation planning is that Hounsfield units (metrics to quantify tissue radiodensity) are correlated with electron density of tissue at each voxel relative to the electron density of water. Due to this correlation it became possible to use information from the CT to calculate radiation absorption and scattering in tissue. In the modern era of 3-D planning, the radiation oncologist contours the volume of tissue to be irradiated as well as normal structures. Dose parameters can then be calculated for any region that is contoured on the planning software. In this process of contouring, the radiation oncologist utilizes all available information regarding the patient’s anatomy, including diagnostic CT, MRI, PET, ultrasound, physical exam, as well as reports from any endoscopic procedures or operations. Using the treatment planning software, it is possible to fuse other imaging modalities to the planning CT such that information from both PET and MRI can be seamlessly incorporated into target volume delineation on the planning CT. In this way, the PET is directly incorporated into the process of radiation treatment planning.
In the 1990s and early 2000s, it was recognized that when chemotherapy was added to radiation therapy, the extended field could be replaced with a smaller field known as the “involved field,” which remained the standard of care until recently [49]. Involved field radiation encompasses not only the involved lymph nodes but also the other lymph nodes within the same lymph node region defined by the Ann Arbor classification for HL staging. All of the field borders were based on bony landmarks such that they could be planned on 2-D simulation units.
A review of relapses in patients treated with chemotherapy alone showed that most recurrences occur in the initially involved lymph nodes [42]. With continued advances in radiation technology and imaging, including 3-D planning and the introduction of FDG-PET scans, it became possible to further minimize treatment fields to only include the initially involved nodal volume in an effort to minimize radiation dose to normal tissues. This concept was introduced in 2006 by the EORTC-GELA in the form of involved nodal radiation therapy (INRT) [18].
Unlike the involved field, which included adjacent uninvolved lymph nodes, INRT limited treatment to only the pre and post-chemotherapy involved lymph node remnant(s) plus a relatively small margin for setup error of 1 cm [18]. The shift from involved field to involved-node radiation techniques mirrored the larger shift within the field of radiation oncology from 2D planning based on bony landmarks and more conformal radiation delivery with 3D treatment planning using CT scans. For the first time, ICRU (International Commission on Radiation Units and Measurements) terms were formally incorporated into the management of HL. These terms include the gross tumor volume (GTV), clinical target volume (CTV), and planning target volume (PTV). GTV refers to the position and extent of gross tumor, i.e., what can be seen, palpated, or imaged. The CTV contains the GTV plus a margin for sub-clinical disease spread. This is often the most difficult volume to contour because this area cannot be fully imaged and it is difficult to accurately define. The PTV includes the CTV plus a margin to account for setup uncertainty. The PTV is the volume to which an isodose line is prescribed. In order to successfully implement INRT, patients must have pre- and post-chemotherapy contrast-enhanced CT scans in the treatment position, and whenever possible the pretreatment CT is performed in conjunction with a PET/CT, also in the treatment position. A major advantage of incorporating the PET/ CT into RT planning for INRT is that it can identify previously undetected lymph nodes that are likely to contain disease. As initially involved lymph nodes are usually either no longer visible or of normal size, a CTV is contoured that is the initial location and extent of disease prior to chemotherapy. Per the EORTC-GELA INRT guidelines, a 1 cm isotropic margin around the CTV was recommended as the PTV in most situations to account for internal organ motion and setup error [17]. Examples of IFRT and INRT treatment fields are also shown in Fig. 5.2.
Axillary radiation fields with (a) IFRT and (b) INRT displayed on digitally reconstructed radiographs. The volume contoured in green encompasses the pre-chemotherapy GTV. This volume represents the CTV in INRT treatment planning. In IFRT, the axillary field includes ipsilateral infraclavicular and supraclavicular lymph node regions with the superior extent of the field at C5–C6 interspace
Because INRT requires precisely fused pre- and post-chemotherapy images (including PET/CT) in the treatment position, the International Lymphoma Radiation Oncology Group (ILROG) introduced the concept of Involved Site Radiation Therapy (ISRT) in 2013 [44]. One of the differences between ISRT and INRT is related to the quality and accuracy (i.e., patient positioning) of the pre-chemotherapy imaging. ISRT incorporates the opportunity to create larger CTV volumes associated with uncertainties related to less than optimal pretreatment imaging (e.g., the pretreatment PET/CT is not obtained in the treatment position). Per the ISRT guidelines, it is recommended that when contouring the CTV, one takes into account the quality and accuracy of imaging, volume changes since imaging, any potential disease spread, potential subclinical involvement, and adjacent normal tissue. There remains a great deal of subjectivity to this process and quantitative imaging, such as PET/CT can be an invaluable tool in order to minimize this inter-observer variability. The approach to ISRT planning is shown in Fig. 5.3.
Involved-site radiation therapy (ISRT). (a) Pre-chemotherapy GTV based on PET/CT. (b) Pre-chemotherapy GTV on post-chemotherapy planning CT. (c) Clinical target volume encompassing the extent of initial disease, created by modifying the pre-chemotherapy GTV on post-chemotherapy planning CT. (d) Digitally reconstructed radiograph of AP field
Both INRT and ISRT would not be possible without the many advances in the field of radiation therapy over the past two decades including computer-assisted 3D planning and treatment delivery. More precise delivery of radiation is now possible with maximum coverage of target volumes and more normal tissue sparing due to the development of intensity-modulated radiotherapy (IMRT) and 3D conformal RT. Technical advances with dynamic multi-leaf collimators, image-guided radiation therapy, and improvements in patient immobilization and positioning all facilitate the delivery of highly complex, multi-field, conformal treatment plans. In order to take full advantage of the recent and dramatic advances in radiation treatment delivery methods and successfully implement INRT/ISRT, the most accurate and precise target delineation is required. In the pre-PET era, the definitions of tumor volumes and treatment volumes were based primarily on structural imaging with contrast CT, physical exam findings, and clinical judgment. The clinical target volume represents the microscopic extent of disease. Although there is no way to image the CTV directly, it is formed with a margin applied to the GTV that was contoured on the pretreatment planning CT and in most cases fused to the pretreatment PET/CT adjusting for changes in the position of normal tissues. Microscopic disease may be missed if the imaging fails to precisely define the extent of tumor. Additionally, further reduction in field size necessitates increased precision, and thus, the value of PET/CT for the planning of ISRT has dramatically increased. Although there is no data to suggest that incorporating PET/CT into volumes leads to improvement in disease related outcomes, it is viewed as an invaluable resource and the incorporation of PET/CT into RT treatment planning has become a central component of modern HL therapy with INRT and ISRT.
5.3 Impact of PET on Target Volume Delineation in Hodgkin’s Lymphoma
As discussed in Chap. 1, there is a higher accuracy in HL staging with FDG-PET scan, compared to CT alone. Furthermore, studies in lymphoma as well as other malignancies have shown that the estimate of tumor extent is more accurate when functional and structural images are combined (see Chapter 4). Functional imaging with PET can influence RT planning for HL in a number of ways. PET can reveal areas of disease that are not well visualized by other imaging modalities. These areas represent additional areas of disease adjacent to the primary tumor volume or unsuspected lymph nodes (LN) or extranodal sites (ENS) involved with disease. Moreover, upon PET/CT incorporation, equivocally involved LN or ENS on CT or MRI, benign reactive lymphadenopathy or brown fat tissue will be less likely included in the radiation field. As discussed in Chap. 2, PET is also useful in evaluating residual masses after chemotherapy and can aid in the final decision regarding radiation dose in HL since higher doses are required for macroscopic compared to microscopic disease.
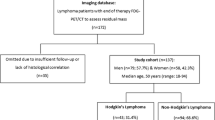
As mentioned above, there have yet to be randomized prospective studies to demonstrate an improvement in clinical outcome combining both imaging techniques for RT planning compared to CT alone, since FDG-PET has been widely adopted together with CT into routine standard practice. However, the impact of FDG-PET in radiation planning for HL has been addressed in a number of studies, which are summarized in Table 5.1. The proportion of HL cases in which there are changes in target volume with the incorporation of PET into RT planning in these studies ranges from 17 to 70 %. In general, FDG-PET is more likely to increase rather than decrease treatment field size, and significant changes in the radiation field tend to occur with the incorporation of FDG-avid lymph nodes that would not have been included with CT planning alone. This is critical in the application of INRT and ISRT where the potential for a marginal miss is enhanced. Reasons for the difference in reported changes may be due to the different methods for defining the RT field, different inclusion criteria (e.g., age) and the fields that were evaluated (e.g., supradiaphragmatic disease only vs. supra- and infradiaphragmatic fields).
In 2004 Lee et al. reported one of the earliest studies addressing the feasibility and impact of incorporating PET into RT treatment fields in lymphoma [30]. Seventeen PET scans from patients with thoracic lymphoma (both HL and NHL) were registered to CT. Comparisons were made between GTV on PET compared to GTV on CT in regard to total volume, as well as lateral and inferior extension of the volume. Of note, the authors did not include both CT and PET information in delineating GTV, as is often done in modern treatment planning. Of the patients who had disease visible on both imaging techniques, the median total CT volume was larger than the total PET volume. In drawing lateral blocks, there were differences >3.0 cm in 40 % of cases. In only three cases the GTV based on PET was smaller than the GTV based on CT. Furthermore, the inferior CT extent of disease was in general lower to that of PET. Although contouring with PET led to significant differences in GTV extent compared to CT alone, the treatment fields were only minimally impacted since conformal treatment methods were not used. The authors conclude that incorporating PET into treatment planning is feasible and the influence of PET in thoracic lymphoma radiation fields appears to be modest.
The subsequent studies examining the impact of PET/CT in RT field design using IFRT or INRT including areas outside of the mediastinum did not agree with this conclusion. Hutchings et al. retrospectively evaluated the treatment plans for 30 adult patients with early-stage HL who underwent PET/CT prior to chemotherapy with adriamycin, bleomycin, vinblastine, dacarbazine (ABVD) [23]. They each received IFRT as defined by the Nordic guidelines after chemotherapy. The radiation oncologists were blinded on the PET result; therefore only CT was used in the treatment field delineation. According to the Nordic guidelines, the radiation field according to IFRT modality encompasses only the tissue volume that had contained the anatomical extent of detectable HL masses prior to chemotherapy, with an additional margin of at least 3 cm while sparing the remaining Ann Arbor lymph node region uninvolved by disease. In this study, the patients received 30.6 Gy in 1.8 Gy daily fractions with a boost of 5.4 Gy to areas of residual disease after chemotherapy. After completion of the RT course, the delineation of treatment fields was repeated on the planning CT scan including information from staging PET CT images. The study was aimed at assessing the contribution of PET/CT to a CT-defined radiation volume; a radiologist and a nuclear medicine expert delineated the radiation field in CT and PET, respectively. When a focus was defined as PET positive, the actual delineation of the target volume was performed using the corresponding CT images for the precise anatomical definition and target volumes defined based on the Nordic IFRT guidelines. In 10 of the 30 patients (approximate 33 %), the delineation of the CTV would have been changed by PET/CT. Seven patients had sites of PET involvement that were outside of the irradiated volume; hence the final irradiated volume would have increased. In these patients, the volume receiving a minimum of 90 % of the prescribed dose was increased by 8–87 % (median 17 %). In two patients, PET CT would have decreased the irradiated volume, and the volume receiving a minimum of 90 % of the prescribed dose was decreased by 18 % and 30 %. One patient had evidence of FDG uptake in the spleen that had not been visible on CT and was upstaged from stage IIB to stage IIIBS. Given that the majority of patients had an increase in treatment field size, it was recommended that FDG-PET should be used to reduce the amount of tissue receiving radiation therapy and would be warranted in RT planning for smaller fields such as INRT. It is noteworthy that of the 30 patients who received IFRT based on CT only in this study, 29 are in complete remission at the time of publication after a median follow-up of 24 months. One patient relapsed within the irradiated field after 2.8 years in a site that was positive on both CT and PET.
Robertson et al. performed a similar study in the pediatric HL population [41]. A nuclear medicine physician experienced in pediatric PET imaging interpreted the staging PET/CT. IFRT was delivered with a CTV created that covered that particular anatomic region as defined by the Ann Arbor staging system. The methods were slightly different in that all relevant lymph node sites and extranodal sites were systematically evaluated in 30 patients and analyzed separately by both CT and FDG-PET. Criteria for anatomic and functional imaging were defined by the current Children’s Oncology Group (COG) protocol guidelines. The CT criteria were based on lymph node size depending on anatomical location. The PET criteria, on the other hand, remained rather subjective with “the level of tumor uptake assessed subjectively by visual inspection and semi-quantitatively by determination of SUV.” The authors found an overall 14 % discordant rate between PET and CT results with more disagreement in nodal vs. extranodal sites. When the studies disagreed for a particular anatomic location, it was more common for the PET to be positive with a negative CT than vice versa. Thirty-two new sites were added and 15 sites were excluded from the IFRT fields, which altered the final treatment volumes in an impressive 21 of 30 (70 %) of patients. The most commonly added sites were the contralateral neck, para-aortic nodes, and spleen. The most commonly excluded sites were pleura, pericardia, and lung nodules. The authors concluded that PET was particularly helpful in detecting disease in relatively small lymph nodes in the neck and axilla that were below CT size criteria and was also superior in revealing disease in areas that are difficult to visualize on CT such as in the abdomen near the head of the pancreas. Patients in this study were treated to 21 Gy in either 1.5 or 1.8 Gy fractions. Four of the 30 (13 %) had relapsed at some point during or after treatment. There were no recurrences in sites excluded from RT based on PET with the exception of an axillary recurrence in a node that was not considered FDG avid nor positive on CT and therefore was not included in the treatment field. In retrospect, however, the site was reinterpreted as hypermetabolic at time of initial staging highlighting the importance of identifying initially involved lymph nodes for RT field delineation. The other three recurrences were within RT treatment fields in areas that were positive on CT and PET.
Paulino et al. also examined the impact of PET/CT on IFRT field design for pediatric HL. This was the largest cohort with 53 patients studied [38]. On CT scan, any node was considered involved with lymphoma if the transverse diameter was >1.5 cm above the diaphragm and >1 cm below the diaphragm (except mesenteric nodes where >1.5 cm was the cutoff). Staging PET CT was also performed where the level of tumor uptake was assessed subjectively by “visual inspection by a nuclear medicine physician and semi-quantitatively by determination of SUV” per COG guidelines. IFRT was delivered (21 Gy in 14 fractions) to all sites of initial disease plus the entire nodal region. IFRT fields were drawn with and without PET CT information and compared. According to the study design, in cases where there was a discrepancy between CT and PET/CT staging, sites of disease were confirmed by either biopsy (n = 4) or by response to chemotherapy (n = 19) prior to administering RT. On retrospective review, 19 of 53 patients (35.8 %) had discordance in at least 1 site between CT and PET/CT findings, which led to a change in radiotherapy field in 9 (17 %). Upon PET/CT staging, the fields increased in size in 8 patients and decreased in 1, with a similar pattern reported in Hutchings et al. and Robertson et al. The most notable change in the RT field was the inclusion of the spleen in 4 cases. Twenty-five nodal sites and disease regions were examined, the specificity, sensitivity, and positive predictive value of PET being 99.5 %, 96.3 %, and 97.9 %, respectively, similar to that reported in previously published reports [13]. The author’s conclusion was similar to that of Hutchings et al. that upon inclusion of PET/CT for IFRT planning, the size of radiation fields likely increases, a concept in sharp contrast to the ongoing paradigm shift toward decreasing treatment intensity (and therefore field size) to minimize late effects.
The relationship between PET/CT-aided RT planning and size of radiation fields was also addressed by Girinsky et al. [16]. Thirty patients with early-stage HL who were treated with INRT according to the EORTC-GELA guidelines were included in the study. All tumor masses but one were FDG-avid prior to chemotherapy. FDG helped localize undetected lymph nodes on CT scan in 36 % of the patients and the metabolic information from pre-chemotherapy PET/CT significantly modified the final irradiation volumes – the average volume incorporating PET was 313 cm3 (95 % CI: 230–397) compared to 291 cm3 by CT (95 % CI: 212–370) (p = 0.0007). In this study, the only recurrence after a median of 2 years was in an unirradiated area in a patient with stage II disease treated with ABVD.
Terezakis et al. report similar results in the examination of patients with HL, NHL, and plasma cell neoplasms [46]. They found that with the incorporation of PET in the definition of IFRT fields, treatment volume had increased in 15 sites (47 %) by a median of 11 % and treatment volume was reduced in 8 sites (25 %) by a median of 20 %.
Despite the limitations of these studies, including the retrospective nature of the analysis, lack of statistical validation due to small sample size, and mainly descriptive methods applicable to this type of data, each provides valuable insight into the role of PET/CT in treatment planning for HL. With the exception of Lee et al., which examined less modern treatment and imaging techniques, these studies concordantly conclude that FDG-PET significantly changes the final treatment volumes in IFRT and INRT fields. Moreover, the incorporation of PET is recommended for modern conformal fields such as INRT and ISRT, as is the current treatment paradigm.
5.4 Methods for Incorporating FDG-PET in RT Planning
After co-registration of the pretreatment PET/CT to the posttreatment planning CT, the target volume should be delineated as described above. Ideally, only the tumor-dependent FDG uptake should be included in the radiation field, while the unspecific FDG uptake by inflammatory tissue should not be taken into account. Prior to the introduction of PET/CT, the definition of an involved lymph node in HL was variable. The dimensional criteria, with a threshold of 1–1.5 cm in the longest transverse diameter as suggestive of lymphoma harbinger, were generally accepted [7]. There are many objections to this definition including a technical limitation related to the fact that cross-sectional lymph node dimension may vary in different spatial directions on CT scan, lymph node architecture can be modified by tumor invasion, and, most importantly, lymph nodes can contain disease without a significant increase in size. An additional layer of complexity is added due to inter-observer variability with CT scanning.
The EORTC-GELA guidelines on how to incorporate PET CT into treatment planning for INRT are summarized below [17].
-
Both planning CT and PET/CT images in the treatment position must be obtained prior to chemotherapy and planning CT images only after chemotherapy. All images should be contrast-enhanced.
-
Pre-chemotherapy PET/CT should be carefully analyzed to identify any lymph nodes that may have been overlooked on CT. An example of an FDG-avid lymph node overlooked on CT is shown in Fig. 5.4.
-
Comparison of pre- and post-chemo images, both for morphologic asymmetry on CT and functional asymmetry on PET/CT, can be an indicator of disease involvement (e.g., involved lymph nodes may decrease in size or disappear entirely).
With the movement from extended field to involved field and more recently to involved-node or involved-site radiotherapy, there has been a strong desire to generate more specific guidelines on target volume delineation including how to interpret imaging results from the PET/CT scan, particularly given the degree of inter-observer variability. As it stands, no consensus has emerged.
5.4.1 Automated and Semi-automated Methods of Target Volume Definition
All of the studies and guidelines mentioned thus far have focused around using a primarily qualitative visual assessment of FDG-PET to aid in target delineation. This inherently subjective method requires input from an experienced radiologist and/or nuclear medicine physician and is prone to inter- and intra-observer variability. Contouring the tumor with the aid of PET is particularly prone to variability as one can easily make the GTV appear larger or smaller on the PET scan by adjusting the threshold levels in the planning or image viewing software. Despite these limitations, the visual interpretation method reflects the current level of practice.
One challenge with PET imaging in particular is the issue of edge detection. The appearance of the lesion edge on PET can by influenced by a number of factors related to the size and shape of the lesion. One way to address this problem is to fuse the PET with cross-sectional anatomy on CT scan as is often done in clinical practice. The edges that are not well defined on PET may be better defined on CT. However, in areas of disease that are imbedded within an area of similar Hounsfield units (e.g., tumor next to atelectatic lung), this is not very helpful. Visual contouring is the most common method of defining edges in 3-dimensional space, but this again invites inter-observer variability and creates potential pitfalls with quality assurance.
Much controversy surrounds the value of PET in tumor volume delineation or the delineation of the pre-chemo GTV, which if performed in an automated or semiautomated way would require both a cutoff value and edge detection methodologies. Those who do not believe that PET should be used to delineate tumor volumes base their argument on the fact that PET and CT are conceptually different imaging modalities [16]. Additionally, CT scan can provide an instantaneous image, particularly when breath-hold techniques are utilized, and inherent in its nature, a PET scan produces an image over time and as a result cannot be controlled for motion (e.g., mediastinal mass motion during the breathing cycle). Spatial resolution is also different between the two and image windowing can dramatically change the size of a tumor mass on FDG-PET. Regardless, PET remains an invaluable tool for target delineation given the metabolic information it provides that complements the anatomic information from CT scan [20].
Because PET is critical to implementing INRT and ISRT, some authors have suggested that a threshold-based target volume could be determined in order to facilitate reproducibility from patient to patient and from physician to physician [29]. PET is a quantitative imaging technique; therefore mathematical models and imaging processing methods have been proposed to aid in contouring a PET volume using an automatic or semiautomatic methodology. All methods have advantages and disadvantages, and none have proven to be clearly superior to the others. However, it must always be remembered that in their current state, automated methods have a shared inherent weakness in that they cannot differentiate between FDG uptake due to malignancy compared to other benign conditions, which some would argue is the most challenging aspect of target delineation with PET in radiation planning for lymphoma. A few of the most common automated and semiautomated methods of target volume delineation will be described below.
5.4.2 SUV
PET was ultimately developed as a quantitative tool. Although many methods have been developed [19], the SUV, despite its limitations, is the most widely used method for quantifying FDG-PET studies. In fact, most automatic or semiautomatic contouring methods involve SUV in some way. The SUV represents the FDG uptake within a tissue measured over a certain interval after FDG administration and normalized to the injected dose and to a factor that takes into account the distribution of FDG throughout the body (such as body weight) [28]. The determination of max SUV in a given lesion is a very common and reliable way to differentiate between benign and malignant conditions. However, one must always keep in mind that SUV should not be taken out of context, and absolute SUV measurements can be unreliable since it is a value that is affected by many factors. Technical factors such as errors in calibration between the PET scanner and dose calibrator [14], biologic factors such as patient comfort [2], and physical factors such as various image reconstruction parameters and region of interest (ROI) definitions [4] all play a role in SUV determination (see Chapter 4). It is also important to remember that a PET scan is not a sophisticated cancer map; it is simply a measure of glucose uptake in tissue. There are many other reasons why tissues take up glucose – e.g., physiologic reasons, inflammation, etc. which will be explained in more detail later in the chapter and more extensively in the Chap. 6 of this book.
5.4.3 Thresholding
The simplest method of using PET for target volume delineation is to use SUV itself. For example, in NSCLC, an SUV value ≥ 2.5 is considered abnormal and highly suspicious for tumor [22]. Although this approach may be reasonable for lung tumors, the appropriate SUV value cutoff is less clear for other malignancies such as head and neck cancer, esophageal cancer, and lymphoma. Furthermore, it is well known that benign conditions can lead to SUV >2.5 and small lesions and edges of moving lesions may falsely lower the SUV to <2.5 due to what is known as the partial volume effect.
Using an absolute threshold or cutoff value with SUV is not only helpful in determining which lesions represent disease, it is also a straightforward way to perform auto-segmentation (i.e., auto-contouring) [50]. In fact, one of the most common methods of contouring a tumor based on FDG-PET is using a fixed threshold method. For example, with a threshold cutoff value of 2.5, any voxel with an SUV of 2.5 or higher would be included the target volume.
In a similar way, a percent threshold for SUVmax or SUVpeak can be used instead of an absolute threshold value. In this method, the volume defined as tumor represents a fixed percentage relative to the tumor SUVmax. Most reports use the value of 40–50 %; however with these thresholds, this technique may underestimate the size of the GTV, particularly when the primary tumor is large with inhomogeneous FDG uptake, as is often the case with lymphoma. On the other hand, using lower thresholds may overestimate the tumor volume and include areas that do not represent disease. A recent retrospective analysis of pediatric and young adult patients with HL demonstrated that applying SUVmax thresholds from 15 to 40 % led to significant variations on INRT treatment volumes and the optimum starting threshold may be somewhere between 15 and 20 %, with the caveat that this low threshold will often include areas of physiologic uptake that must be carefully excluded by the trained eye with input from a nuclear medicine physician [47].
5.4.4 Other Automated Segmentation Methods
More complex algorithms have been described in the literature for metabolic tumor volume (MTV) assessment, based on a tumor contouring approach, using a predefined cutoff value of the measured activity inside the tumor compared to the surrounding background: the tumor to background (T/B) ratio [10]. The advantage of this method is that it is independent of tracer uptake in tumor, which can be quite heterogeneous in HL. The main disadvantage is that it relies on quantifying background uptake, which is fraught with challenges similar to SUV calculation with inherent technical and statistical errors. In order to address the issue with edge detection, numerous publications have reported the successful use of complex algorithms and adaptive thresholding methods [12].
Although there have been many approaches to auto-segmentation described in the literature, each approach has limitations that preclude its implementation as standard of care. Most experts agree that automated or semiautomated methods should be aimed at reducing variability rather than replacing human operation, but we do not know the ideal way to use PET for target volume delineation. Given that the qualitative visual method (with knowledge of quantitative parameters such as SUV) is still the primary method of incorporating PET into RT planning, there is a need for a multidisciplinary assessment of patients upfront before chemotherapy in order to have an accurate assessment of regions involved with disease for the application of smaller radiation treatment fields.
5.4.5 PET Imaging Protocols
Although most information on PET scan results can be gathered with visual assessment in daily practice, the quantitative readings could in theory give some advantages, by providing information on a continuous variable such as the intensity of FDG uptake by the tumor. Quantitative metrics for FDG uptake measurement is critical in response assessment, staging, and RT planning. Imaging protocols are designed to make results reproducible between patients. As such, they are often rigorous and must be consistently applied in order to generate the most meaningful information. Some PET scanners are located within radiation oncology departments and other institutions rely on PET scans obtained in the nuclear medicine department. Regardless of the location of the PET scanner, the quality control is still important [33, 35]. In 2008, shortly after INRT was introduced in Europe, the International Atomic Energy Agency published guidelines summarizing two consensus meetings regarding the role of PET in radiation treatment planning. These guidelines clearly state that when PET scans are to be used for radiation planning, all of the tools used for patient immobilization should be available including customized molds and face masks. All images should be obtained on a flat tabletop (similar to the radiation treatment table). Furthermore, laser beams should be installed for patient alignment and the gantry aperture must permit a range of patient positions, including arms up and arms akimbo [24]. Of course, this represents the ideal situation. Often, stand-alone pretreatment PET/CT images are all we have available, in which case a great deal of caution must be used when transferring the PET or PET/CT into the RT planning software workstation and the PET imaging should be checked for correct normalization and SUV quantification.
As previously described, RT planning after chemotherapy is based on the pre-chemo extent of disease unless disease progression has occurred. Ideally, the radiation oncologist should see the patient at diagnosis and obtain CT and PET/CT in the treatment position to allow for ease of contouring at the time of treatment. The treatment position in lymphoma varies depending on clinical factors including areas of disease involvement as well as patient age and normal tissue exposure. For the most part, arms will either be raised or akimbo with neck extended in cases that require irradiation of cervical nodes or Waldeyer’s ring. This includes imaging with immobilization devices where appropriate. If the radiation oncology facility is not equipped with a PET/CT scanner or if pre-chemo imaging in the treatment position is not available, then co-registration must take place.
Fusing the pretreatment PET/CT directly to the posttreatment, CT has the advantage of providing physiologic data with precise topographic localization and is preferred over side-by-side imaging. Metwally et al. assessed the inter-observer variability in CTV definitions when pretreatment PET/CTs were either co-registered to posttreatment planning CTs or evaluated with side-by-side imaging. The authors found that registration of the PET/CT and planning CT images resulted in significantly greater consistency of tumor volume definition [34].
5.4.6 Concept of Dose Escalation
In an attempt to better understand the biological significance of FDG-avid areas of tumor in HL, Girinsky et al. measured the degree of shrinkage in the FDG-avid volume of tumor compared to non-FDG-avid volume after treatment with chemotherapy [16]. The hypothesis was that FDG-avid areas of disease may demonstrate less response to chemotherapy and would therefore benefit from receiving higher doses of radiation therapy (also known as dose escalation or dose painting). However, responses after chemotherapy were similar for both FDG-avid and non-FDG-avid lesions (67 and 68 % decrease in size, respectively). In addition, on average 25 % of the volume of disease at baseline was FDG avid (range 0–54 %), suggesting that about 75 % of the tumor mass would not have been visualized if the PET had been performed alone. The authors conclude that dose escalation based on FDG avidity is not a reasonable treatment strategy in HL. Although this study does not support the use of dose escalation based on FDG avidity, there may be other imaging biomarkers that hold promise in determining which patients and which lesions are more likely to recur and would therefore benefit from more aggressive local therapy.
5.5 FDG-PET: Pitfalls and Artifacts Relevant to RT Planning
Although PET has high sensitivity in HL, there can be a number of false positives [31], particularly when interpreted by radiologists or nuclear medicine physicians who lack experience in the pediatric lymphoma population [27]. Multiple noncancerous conditions can mimic lymphoma such as thermogenic brown fat (also known as brown adipose tissue (BAT)), strained muscle, infections, transforming germinal centers in normal lymphatic tissue, thymic hyperplasia, and general inflammatory conditions such as granulomatous diseases (e.g. sarcoidosis) (see Chapter 6).
5.5.1 Organ Motion
One must keep in mind that PET images are acquired over a relatively long period of time (more than 20’) and therefore lesions that are subject to motion related to the breathing cycle may appear larger than their actual size. This also has an impact on partial volume effect, where the tumor SUV is underestimated. We do not typically use respiratory gating during PET/CT acquisition but this could be considered moving forward if PET if PET alone were to be used for target volume delineation.
5.5.2 Brown Adipose Tissue
BAT as opposed to white adipose tissue (WAT) is capable of generating heat in response to cold exposure or food ingestion as a consequence of its unique ability to uncouple oxidative phosphorylation in mitochondria. Hence, heat is generated rather than ATP during metabolism. The metabolism of glucose during this process is via the anaerobic pathway and a greater amount of glucose is required in order to provide the ATP for fatty acid oxidation. For this reason BAT is a potential source of false positives in PET scans. Brown fat is more common in children and females, is characteristically not associated with a radiographic or clinical abnormality, and typically has a curvilinear distribution in the neck and supraclavicular areas. This highlights the importance of contouring with FDG-PET co-registered with a CT scan to provide superior anatomic localization of all PET abnormalities. This abnormal uptake is also present in adipose tissue in other parts of the body, specifically in the mediastinum and perinephric fat. The incidence of FDG-avid adipose tissue has been estimated to be between 2 and 6 % depending on the series and can be easily misinterpreted as additional areas of pathologic lymphadenopathy [8]. Measurement of SUV is not always helpful in differentiating between malignant and benign etiology. In one series, the SUV associated with BAT was reported as high as 20 [51]. An example of FDG uptake due to brown adipose tissue is shown in Fig. 5.5.
5.5.3 Thymic FDG Uptake
It is generally accepted that some degree of thymic FDG uptake can be expected until puberty, at which point the thymus undergoes fatty infiltration and involutes. In these prepubescent patients, the rate of mild FDG uptake associated with a normal thymus has been estimated to be about 50 % [37]. Some studies have shown that physiologic uptake can be seen in older patients as well [36]. Another cause of thymic uptake is thymic hyperplasia. This phenomenon is associated with chemotherapy, particularly in children with lymphoma, but can also be seen in adults [5]. A critical evaluation of the thymus may be necessary in radiation planning given that it is not uncommon for the thymus to be involved with mediastinal HL, more commonly in the nodular sclerosis subtype [48]. The recognition of physiologic uptake from involvement with HL is particularly important in the era of more conformal radiation techniques. In equivocal cases, other imaging modalities such as MRI can be useful to differentiate benign thymic uptake from malignancy.
5.5.4 Physiologic FDG Uptake
We must keep in mind that FDG uptake also occurs in nonmalignant tissue other than brown fat and the thymus [9, 43]. FDG accumulation is actually most notable in the brain and heart due to the presence of glycolytic metabolism. Because FDG is excreted through the urinary system, FDG activity will be present in the kidney’s intrarenal collecting system, the ureters, and the bladder. Less intense radiotracer activity is present in the liver, spleen, and bone marrow. Variable physiologic uptake can occur in the digestive tract as well. It is not uncommon for focal uptake to occur at the GE junction. Uptake in the digestive system could easily be assumed to represent subdiaphragmatic lymphadenopathy without correlation to anatomic cross-sectional imaging on CT. In patients who have fasted (which is required for PET scanning), it is not uncommon for the stomach, normal colon, and small intestine to also display FDG uptake. In the bowel, the uptake is typically isolated rather than diffuse and its linear configuration allows the correct identification as uptake limited to the normal bowel. Other areas that can also lead to FDG uptake include the skeletal muscle, thyroid, and bone marrow.
5.5.5 Benign Pathologic Causes of FDG Uptake
Benign pathologic FDG uptake can occur in lymph nodes, posing problems in using PET/CT for RT planning in HL. One must be aware that active granulomatous disease such as sarcoidosis and tuberculosis can also cause uptake in lymph nodes [32]. Healing bone and degenerative joints and other sites of infection or inflammation can all cause an increase in FDG that may mimic malignancy [45].
References
Aleman BMP, van den Belt-Dusebout AW, Klokman WJ, et al. Long-term cause-specific mortality of patients treated for Hodgkin’s disease. J Clin Oncol. 2003;21:3431–9. doi:10.1200/JCO.2003.07.131.
Alkhawaldeh K, Alavi A. Quantitative assessment of FDG uptake in brown fat using standardized uptake value and dual-time-point scanning. Clin Nucl Med. 2008;33:663–7. doi:10.1097/RLU.0b013e318184b3de.
Bhatia S, Robison LL, Oberlin O, et al. Breast cancer and other second neoplasms after childhood Hodgkin’s disease. N Engl J Med. 1996;334:745–51. doi:10.1056/NEJM199603213341201.
Boellaard R, Krak NC, Hoekstra OS, Lammertsma AA. Effects of noise, image resolution, and ROI definition on the accuracy of standard uptake values: a simulation study. J Nucl Med. 2004;45:1519–27.
Brink I, Reinhardt MJ, Hoegerle S, et al. Increased metabolic activity in the thymus gland studied with 18 F-FDG PET: age dependency and frequency after chemotherapy. J Nucl Med. 2001;42:591–5.
Brinker H. A re-analysis of available dose-response and time-dose data in Hodgkin’s disease. Radiother Oncol. 1994;30:227.
Cheson BD, Pfistner B, Juweid ME, et al. Revised response criteria for malignant lymphoma. J Clin Oncol. 2007;25:579–86. doi:10.1200/JCO.2006.09.2403.
Cohade C, Osman M, Pannu HK, Wahl RL. Uptake in supraclavicular area fat (“USA-fat”): description on 18F-FDG PET/CT. J Nucl Med. 2003;44:170–6.
Cook GJR, Fogelman I, Maisey MN. Normal physiological and benign pathological variants of 18-fluoro-2-deoxyglucose positron-emission tomography scanning: potential for error in interpretation. Semin Nucl Med. 1996;26:308–14. doi:10.1016/S0001-2998(96)80006-7.
Daisne J-F, Sibomana M, Bol A, et al. Tri-dimensional automatic segmentation of PET volumes based on measured source-to-background ratios: influence of reconstruction algorithms. Radiother Oncol. 2003;69:247–50. doi:10.1016/S0167-8140(03)00270-6.
Devita VT. Combination chemotherapy in the treatment of advanced Hodgkin’s disease. Ann Intern Med. 1970;73:881. doi:10.7326/0003-4819-73-6-881.
Drever L, Wilson R, McEwan A, et al. Comparison of three image segmentation techniques for target volume delineation in positron emission tomography. J Appl Clin Med Phys. 2007;8:93–109.
Freudenberg LS, Antoch G, Schütt P, et al. FDG-PET/CT in re-staging of patients with lymphoma. Eur J Nucl Med Mol Imaging. 2004;31:325–9. doi:10.1007/s00259-003-1375-y.
Geworski L, Knoop BO, de Wit M, et al. Multicenter comparison of calibration and cross calibration of PET scanners. J Nucl Med. 2002;43:635–9.
Gilbert R. Radiotherapy in Hodgkin’s disease (malignant granulomatosis). Am J Roentgenol. 1939;41:198–241.
Girinsky T, Ghalibafian M, Bonniaud G, et al. Is FDG-PET scan in patients with early stage Hodgkin lymphoma of any value in the implementation of the involved-node radiotherapy concept and dose painting? Radiother Oncol. 2007;85:178–86. doi:10.1016/j.radonc.2007.07.003.
Girinsky T, Specht L, Ghalibafian M, et al. The conundrum of Hodgkin lymphoma nodes: to be or not to be included in the involved node radiation fields. The EORTC-GELA lymphoma group guidelines. Radiother Oncol. 2008;88:202–10. doi:10.1016/j.radonc.2008.05.012.
Girinsky T, van der Maazen R, Specht L, et al. Involved-node radiotherapy (INRT) in patients with early Hodgkin lymphoma: concepts and guidelines. Radiother Oncol. 2006;79:270–7. doi:10.1016/j.radonc.2006.05.015.
Graham M, Peterson L, Hayward R. Comparison of simplified quantitative analyses of FDG uptake. Nucl Med Biol. 2000;27:647–55. doi:10.1016/S0969-8051(00)00143-8.
Gregoire V. Is there any future in radiotherapy planning without the use of PET: unraveling the myth…. Radiother Oncol. 2004;73:261–3. doi:10.1016/j.radonc.2004.10.005.
Hancock SL, Hoppe RT, Horning SJ, Rosenberg SA. Intercurrent death after Hodgkin disease therapy in radiotherapy and adjuvant MOPP trials. Ann Intern Med. 1988;109:183–9.
Hong R, Halama J, Bova D, et al. Correlation of PET standard uptake value and CT window-level thresholds for target delineation in CT-based radiation treatment planning. Int J Radiat Oncol Biol Phys. 2007;67:720–6. doi:10.1016/j.ijrobp.2006.09.039.
Hutchings M, Loft A, Hansen M, et al. Clinical impact of FDG-PET/CT in the planning of radiotherapy for early-stage Hodgkin lymphoma. Eur J Haematol. 2007;78:206–12. doi:10.1111/j.1600-0609.2006.00802.x.
International Atomic Energy Agency (IAEA). IAEA-TECDOC-1603: the role of PET/CT in radiation treatment planning for cancer patient treatment. 2008.
Kaplan HS. The radical radiotherapy of regionally localized Hodgkin’s disease. Radiology. 1962;78:553–61. doi:10.1148/78.4.553.
Kaplan S. The treatment of Hodgkin’s disease. Med Clin North Am. 1966;50:1591–610.
Kaste SC, Howard SC, McCarville EB, et al. 18 F-FDG-avid sites mimicking active disease in pediatric Hodgkin’s. Pediatr Radiol. 2005;35:141–54. doi:10.1007/s00247-004-1340-3.
Kim CK, Gupta NC. Dependency of standardized uptake values of fluorine-18 fluorodeoxyglucose on body size: comparison of body surface area correction and lean body mass correction. Nucl Med Commun. 1996;17:890–4.
Krasin MJ, Hudson MM, Kaste SC. Positron emission tomography in pediatric radiation oncology: integration in the treatment-planning process. Pediatr Radiol. 2004;34:214–21. doi:10.1007/s00247-003-1113-4.
Lee YK, Cook G, Flower MA, et al. Addition of 18F-FDG-PET scans to radiotherapy planning of thoracic lymphoma. Radiother Oncol. 2004;73:277–83. doi:10.1016/j.radonc.2004.07.029.
Levine JM, Weiner M, Kelly KM. Routine use of PET scans after completion of therapy in pediatric Hodgkin disease results in a high false positive rate. J Pediatr Hematol Oncol. 2006;28:711–4. doi:10.1097/01.mph.0000243648.66734.eb.
Lewis PJ, Salama A. Uptake of fluorine-18-fluorodeoxyglucose in sarcoidosis. J Nucl Med. 1994;35:1647–9.
Lucignani G, Jereczek-Fossa BA, Orecchia R. The role of molecular imaging in precision radiation therapy for target definition, treatment planning optimisation and quality control. Eur J Nucl Med Mol Imaging. 2004;31:1059–63. doi:10.1007/s00259-004-1517-x.
Metwally H, Courbon F, David I, et al. Coregistration of prechemotherapy PET-CT for planning pediatric Hodgkin’s disease radiotherapy significantly diminishes interobserver variability of clinical target volume definition. Int J Radiat Oncol Biol Phys. 2011;80:793–9. doi:10.1016/j.ijrobp.2010.02.024.
Mutic S, Dempsey JF, Bosch WR, et al. Multimodality image registration quality assurance for conformal three-dimensional treatment planning. Int J Radiat Oncol. 2001;51:255–60. doi:10.1016/S0360-3016(01)01659-5.
Nakahara T, Fujii H, Ide M, et al. FDG uptake in the morphologically normal thymus: comparison of FDG positron emission tomography and CT. Br J Radiol. 2001;74:821–4. doi:10.1259/bjr.74.885.740821.
Patel PM, Alibazoglu H, Ali A, et al. Normal thymic uptake of FDG on PET imaging. Clin Nucl Med. 1996;21:772–5.
Paulino AC, Margolin J, Dreyer Z, et al. Impact of PET-CT on involved field radiotherapy design for pediatric Hodgkin lymphoma. Pediatr Blood Cancer. 2012;58(6):860–4. doi:10.1002/pbc.23273.
Peters M. A study of survivals in Hodgkin’s disease treated radiologically. Am J Roentgenol Radium Ther. 1950;63:299–311.
Pusey WA. Cases of sarcoma and of Hodgkin’s disease treated by exposures to x-rays—a preliminary report. JAMA J Am Med Assoc. 1902;XXXVIII:166. doi:10.1001/jama.1902.62480030024001h.
Robertson VL, Anderson CS, Keller FG, et al. Role of FDG-PET in the definition of involved-field radiation therapy and management for pediatric Hodgkin’s lymphoma. Int J Radiat Oncol Biol Phys. 2011;80:324–32. doi:10.1016/j.ijrobp.2010.02.002.
Shahidi M, Kamangari N, Ashley S, et al. Site of relapse after chemotherapy alone for stage I and II Hodgkin’s disease. Radiother Oncol. 2006;78:1–5. doi:10.1016/j.radonc.2005.10.018.
Shreve PD, Anzai Y, Wahl RL. Pitfalls in oncologic diagnosis with FDG PET imaging: physiologic and benign variants. Radiographics. 1999;19:61–77. doi:10.1148/radiographics.19.1.g99ja0761, quiz 150–1.
Specht L, Yahalom J, Illidge T, et al. Modern radiation therapy for Hodgkin lymphoma: field and dose guidelines from the international lymphoma radiation oncology group (ILROG). Int J Radiat Oncol Biol Phys. 2014;89:854–62. doi:10.1016/j.ijrobp.2013.05.005.
Strauss LG. Fluorine-18 deoxyglucose and false-positive results: a major problem in the diagnostics of oncological patients. Eur J Nucl Med. 1996;23:1409–15.
Terezakis SA, Hunt MA, Kowalski A, et al. [18F]FDG-positron emission tomography coregistration with computed tomography scans for radiation treatment planning of lymphoma and hematologic malignancies. Int J Radiat Oncol Biol Phys. 2011;81:615–22. doi:10.1016/j.ijrobp.2010.06.044.
Walker AJ, Chirindel A, Hobbs RF, et al. Use of standardized uptake value thresholding for target volume delineation in pediatric Hodgkin lymphoma. Pract Radiat Oncol. 2015;5:219–27. doi:10.1016/j.prro.2014.12.004.
Wernecke K, Vassallo P, Rutsch F, et al. Thymic involvement in Hodgkin disease: CT and sonographic findings. Radiology. 1991;181:375–83. doi:10.1148/radiology.181.2.1924775.
Yahalom J, Mauch P. The involved field is back: issues in delineating the radiation field in Hodgkin’s disease. Ann Oncol. 2002;13 Suppl 1:79–83. doi:10.1093/annonc/mdf616.
Yaremko B, Riauka T, Robinson D, et al. Thresholding in PET images of static and moving targets. Phys Med Biol. 2005;50:5969–82. doi:10.1088/0031-9155/50/24/014.
Yeung HWD, Grewal RK, Gonen M, et al. Patterns of (18)F-FDG uptake in adipose tissue and muscle: a potential source of false-positives for PET. J Nucl Med. 2003;44:1789–96.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Walker, A.J., Terezakis, S.A. (2016). PET/CT in RT Planning. In: Gallamini, A. (eds) PET Scan in Hodgkin Lymphoma. Springer, Cham. https://doi.org/10.1007/978-3-319-31797-7_5
Download citation
DOI: https://doi.org/10.1007/978-3-319-31797-7_5
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-31795-3
Online ISBN: 978-3-319-31797-7
eBook Packages: MedicineMedicine (R0)