Abstract
Accurate baseline staging of Hodgkin lymphoma (HL) is crucial for prognostication and guides important treatment decisions. This remains true in the era of highly effective combined modality treatments and intensive multi-agent chemotherapy regimens that lead to cure in the vast majority of HL patients irrespective of disease stage [1, 2]. In the early 1970s the Committee on Hodgkin’s Disease Staging Classification convened in Ann Arbor, Michigan, and this resulted in the first staging classification for HL which was named after the city [3]. The Ann Arbor staging classification became the widely accepted classification for disease staging in HL and enabled comparison of studies by different investigators. The main clinical purpose of the Ann Arbor Classification was to accurately identify patients with limited-stage HL who could be treated with a curative intent with radiotherapy alone. Accurate staging was pursued through rigorous procedures, which included both a clinical and a pathological staging workup. Clinical stage was determined from physical examination, symptom assessment, lymphangiograms, and radiograms, some of which are still elements in modern HL staging. Pathological stage was derived from the results of invasive staging procedures including diagnostic laparotomy and iliac crest bone marrow biopsy (BMB). The risk of serious complications and discomfort related to invasive procedures were tolerated at that time as no good alternatives for evaluation of deep lymph node regions and organs were available. The introduction of computed tomography (CT) enabled noninvasive assessment of deep lymph node regions/organs and changed the staging of HL fundamentally. The committee convened to discuss the evaluation and staging of patients with Hodgkin’s disease met in the Cotswolds (UK) and the report generated by the committee recommended CT of the thorax and abdomen in the routine staging workup of HL. Invasive staging procedures with the exception of iliac crest bone marrow biopsy were no longer considered necessary (Cotswold modifications of the Ann Arbor Classification) [4].
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Positron Emission Tomography
- Hodgkin Lymphoma
- Bone Marrow Involvement
- Positron Emission Tomography Tracer
- Hodgkin Lymphoma Patient
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1.1 Historical Background
Accurate baseline staging of Hodgkin lymphoma (HL) is crucial for prognostication and guides important treatment decisions. This remains true in the era of highly effective combined modality treatments and intensive multi-agent chemotherapy regimens that lead to cure in the vast majority of HL patients irrespective of disease stage [1, 2]. In the early 1970s the Committee on Hodgkin’s Disease Staging Classification convened in Ann Arbor, Michigan, and this resulted in the first staging classification for HL which was named after the city [3]. The Ann Arbor staging classification became the widely accepted classification for disease staging in HL and enabled comparison of studies by different investigators. The main clinical purpose of the Ann Arbor Classification was to accurately identify patients with limited-stage HL who could be treated with a curative intent with radiotherapy alone. Accurate staging was pursued through rigorous procedures, which included both a clinical and a pathological staging workup. Clinical stage was determined from physical examination, symptom assessment, lymphangiograms, and radiograms, some of which are still elements in modern HL staging. Pathological stage was derived from the results of invasive staging procedures including diagnostic laparotomy and iliac crest bone marrow biopsy (BMB). The risk of serious complications and discomfort related to invasive procedures were tolerated at that time as no good alternatives for evaluation of deep lymph node regions and organs were available. The introduction of computed tomography (CT) enabled noninvasive assessment of deep lymph node regions/organs and changed the staging of HL fundamentally. The committee convened to discuss the evaluation and staging of patients with Hodgkin’s disease met in the Cotswolds (UK) and the report generated by the committee recommended CT of the thorax and abdomen in the routine staging workup of HL. Invasive staging procedures with the exception of iliac crest bone marrow biopsy were no longer considered necessary (Cotswold modifications of the Ann Arbor Classification) [4].
1.2 The Introduction of Functional Imaging
The introduction of functional imaging was another shift in paradigm and defined the current era of modern HL staging. From a CT-based disease staging relying on the size of lymph nodes and morphological abnormalities in organs, functional imaging now provides information on local metabolic activity. This is a major advantage, since knowledge of local metabolism can facilitate discrimination between active HL and nonmalignant morphological abnormalities as well as visualize HL lesions in areas without clear morphological abnormalities. The first functional imaging method to enhance the accuracy of HL staging was the whole-body 67gallium scintigraphy, but this procedure is laborious and the image quality often rather poor. After the introduction of positron emission tomography (PET), gallium scans quickly disappeared from the management of HL. The most common PET tracer is the radioactive glucose analogue 18F-flurodeoxyglucose (FDG). This tracer is widely studied in HL and FDG-PET is the only type of functional imaging that has been implemented in the routine management of the disease. FDG-PET (in the following referred to as PET) provides a whole-body map of glucose metabolism and HL lesions were found to be universally PET positive (except for very small lesions below the spatial resolution of PET) [5]. An important limitation of stand-alone PET is the inability to locate the exact anatomical area of increased glucose metabolism. This was overcome with the introduction of integrated PET/CT scanner, which made it possible to perform both PET and CT in a single procedure, using CT for attenuation correction of PET data, and to demonstrate the anatomical localization of areas with increased glucose metabolism seen on PET. In this way, modern imaging enables clinically relevant functional and anatomical information to be obtained together. CT and PET can be viewed separately, side-by-side and “fused” with the PET scan overlaid on the CT in color. Today, PET studies are almost exclusively performed with integrated PET/CT machines (Fig. 1.1).
1.3 Early Studies of Staging PET
PET is more sensitive and specific than CT because abnormal FDG uptake may be observed in normal-sized nodes and also seen without changes in organ architecture, e.g., in the liver, spleen, and bones. Over the past 20 years, a number of studies have demonstrated the increased sensitivity of PET relative to conventional imaging.
In their study published in 1998, Bangerter et al. scanned 44 HL patients as a part of their initial staging workup. PET and conventional staging were concordant in 128 (96 %) of 133 diseased lymph node regions. Six patients changed stage as a result of PET, five being upstaged and one downstaged, leading to a change of treatment strategy in all six patients. This study was the first to demonstrate on a reasonably high number of patients that PET is largely concordant with CT for staging of HL and that the additional value of the method has an impact on the management of the patients [6].
Partridge et al. retrospectively investigated the impact of 44 pretreatment scans on the management of HL patients. PET found almost twice as many positive sites than CT (159 vs. 84) and 21 patients would have had their staging changed as a result of PET (18 upstaging and three downstaging. According to PET, treatment strategy should have been changed in 11 patients, in 10 cases to a more intensive therapy. 12 patients had a total of 19 extranodal disease sites. PEt alone detected 15 of these sites, four sites were seen on both CT and PET, and PET missed no sites seen on CT. This study suggested a very high sensitivity for detection of organ involvement [7].
Jerusalem et al. undertook the first thorough study of region-by-region accuracy in HL. They scanned 33 patients before initial treatment or before treatment of relapse and evaluated the impact on nodal staging. Overall concordant results were seen in 22 patients, but in two patients both methods indicated lesions that were not shown by the other method. In six patients, PET showed involvement of more regions than conventional methods. The sensitivities of PET for detecting involved lymph node regions were 95 % in peripheral regions, 96 % in thoracic regions, and 78 % in abdominal/pelvic regions. The corresponding sensitivities for conventional staging procedures were 80 %, 81 %, and 86 %. Although the impact on staging was clear, PET staging would only have had impact on treatment strategy in one patient [8]. Weihrauch et al. applied a quite similar approach. In 22 patients they identified 72 involved lymph node regions. In 48 lesions in 22 patients, both CT and PET were positive. 20 lesions in 11 patients were positive on PET but not detected by CT or other conventional staging methods. Sensitivity of PET and CT was 88 % and 74 %, respectively, and out of 22 patients, four were upstaged due to PET findings [9].
The general impression from these early studies was that:
-
1.
PET seemed to have a relatively high sensitivity for nodal staging.
-
2.
PET was clearly more sensitive than CT in detecting extranodal disease, both in the bone marrow and in other organs (Fig. 1.2).
-
3.
PET had a consistent, large influence on the staging, with a potential impact on treatment strategy in a substantial number of patients.
More recent studies have confirmed these findings: Cerci and colleagues enrolled 210 newly diagnosed HL patients in a prospective study aiming to evaluate the cost-effectiveness of PET in HL staging. They found sensitivity for initial staging of PET was higher than that of CT in initial staging (97.9 % vs. 87.3 %). The incorporation of PET in the staging procedure upstaged disease in 50 (24 %) patients and downstaged disease in 17 (8 %) patients, with a resultant changes in treatment in 32 (15 %) patients [10].
But the high sensitivity of stand-alone PET came at the expensive of a relatively large number of false positive results, in part due to well-known pitfalls including FDG uptake in reactive lymph nodes due to inflammation/infection (Figs. 1.3 and 1.4), brown fat uptake (Fig. 1.5), physiological bowel uptake, uptake due to thymic rebound, etc. After the introduction of PET/CT, such false positive findings became much less common, resulting in a high specificity despite the high sensitivity.
An example of false positive PET results. Hodgkin lymphoma patient scanned 2 months after completion of treatment. PET/CT early during chemotherapy had shown a complete metabolic response. A biopsy was taken from the PET-positive mediastinal lymph nodes, and the histology showed a sarcomatoid reaction, with no signs of malignant disease
1.4 PET/CT Staging
The first study of PET/CT was a prospective comparison of PET, CT, and PET/CT in 99 newly diagnosed HL patients. The results of PET and PET/CT were not disclosed to the treating physicians, and furthermore, the reviewers of PET, CT, and PET/CT were blinded to the results the other imaging modalities. In nodal regions, the sensitivity of PET and PET/CT was higher than that of CT (92 % and 92 % vs. 83 %). PET had more false positive nodal sites than CT and PET/CT (1.6 % vs 0.7 % and 0.5 %). For evaluation of organs, PET and PET/CT had high sensitivities (86 % and 73 %) while CT detected only 37 % of involved organs. PET would have upstaged 19 % of patients and downstaged 5 % of patients, leading to a different treatment strategy in 9 % of patients [11]. An analysis of the same group of patients revealed that FDG avidity varied between different subtypes of classical HL and that the FDG uptake in nodular lymphocyte-predominant (NLP) HL was significantly lower than in classical HL [12].
Bednaruk-Młyński and colleagues compared the results of staging CT and PET/CT in 96 HL patients. Also in this study, the radiologists and nuclear medicine physicians were blinded to results of the other modality and to the clinical course of the patients. The number of patients with stage I, II, III, and IV disease based on CT versus PET/CT was 5 vs. 7, 49 vs. 37, 28 vs. 22, and 14 vs. 30, respectively. PET/CT changed the stage in 33 (34 %) patients; 28 % were upstaged and 6 % downstaged. Upstaging was mainly caused by detection of new extranodal involvements (47 sites in 26 patients): the bone marrow (10 patients), spleen (5 patients), and lung (2 patients). Downstaging resulted from the absence of FDG uptake in enlarged nodes (<15 mm) in the abdomen and pelvis. PET/CT led to a treatment modification in 20 (21 %) of the patients, with 16 patients allocated to more intensive treatment and 4 to less intensive treatment [13].
A different approach was taken by El-Galaly et al. who performed a historical comparison of staging patterns in Danish HL patients before and after the introduction of staging PET/CT. Their analysis covered two large cohorts of patients with classical HL staged without PET/CT (n = 324) and with PET/CT (n = 406). In PET/CT-staged patients, stage I disease was less frequent (16 % vs. 27 %) while stage IV disease was more frequent (17 % vs. 10 %). Imaging-detected skeletal involvement was recognized more often in PET/CT-staged patients (17 % vs. 2 %), and the presence of focal skeletal PET/CT lesions was associated with higher risk of progression [14].
NLP HL has more characteristics in common with indolent lymphomas, and as mentioned above this subtype has lower FDG avidity than classical Hodgkin lymphoma [12], but still the sensitivity of PET/CT staging seems to be high. In a study of 35 patients with this rare histological subtype, Grellier et al. found that PET/CT resulted in stage migration in 34 % of the patients, with detection of disease in the bone or bone marrow in 20 % of the patients. The identification of advanced disease in NLP HL is particularly important for management, since localized NLP HL is often treated with local radiotherapy alone and thus without systemic therapy [15].
Figures 1.6 and 1.7 show PET/CT images of HL patients with stage II and stage III, respectively.
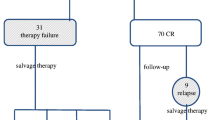
1.5 Stage Migration and Overtreatment
Hodgkin lymphoma can be cured in the vast majority of cases but cure comes the price of serious treatment-related late effects, including second cancers and cardiopulmonary disease [16]. While optimizing cure is always a goal of clinical cancer research, in first-line Hodgkin lymphoma treatment, there is a stronger call for reduction of the treatment intensity in order to avoid unnecessary overtreatment in some patients without losing efficacy for others [17]. As discussed, PET/CT results in considerable upward stage migration and allocation of 10–20 % of patients to a more advanced treatment group. If PET/CT is incorporated into routine and the existing treatment paradigms are kept unchanged, this will result in even more overtreatment (Fig. 1.8). The introduction of more sensitive staging methods also calls for relevant therapeutic modifications, so the more refined imaging is used to individualize therapy rather than to aggravate the overtreatment problem. Such treatment modifications as a consequence of PET/CT have indeed already taken place: The shift from involved-field radiotherapy to involved-node radiotherapy resulted in a dramatic reduction of radiation fields to HL patients, and this change was a direct result of the more accuracy baseline imaging by PET/CT [18].
Upward stage migration as a consequence of PET/CT. This young lady was diagnosed with classical Hodgkin lymphoma and stage IIA disease according to CT performed before referral. Staging PET/CT showed a clearly PET-positive lesion in the spleen. There was no corresponding abnormality on CT and biopsy was not feasible. The original treatment plan was changed from a brief course of chemotherapy followed by local irradiation to the neck and upper mediastinum to 6 cycles of combination chemotherapy. During her treatment, she developed pneumonitis as a result of bleomycin treatment, and she needed high-dose prednisone treatment for several months. With the patient well and in continued remission more than 5 years after treatment, it is still not clear if PET/CT saved her from undertreatment or resulted in overtreatment
1.6 Is Contrast-Enhanced CT Necessary in the PET/CT Era?
The CT part of a PET/CT scan may be performed with contrast enhancement (ceCT) at full radiation dose to obtain a high-quality CT examination or without contrast using a lower radiation dose. Low-dose CT is used to correct for the attenuation of radioactivity within the patient and to localize abnormalities seen on PET, with less radiation than a full diagnostic examination. Whichever protocol is used, CT must be acquired during shallow breathing or end of expiration to avoid misregistration and artifacts [19]. A number of studies have compared PET/CT with and without ceCT, and although ceCT may identify additional findings and improve detection of abdominal and pelvic disease, this rarely has an impact on management [20–22]. The use of contrast may result in small errors in the measurement of FDG uptake due to an effect on attenuation correction; this may cause errors in comparison of uptake between tumor and reference sites by causing FDG uptake to be overestimated in the mediastinum and liver by 10–15 %. Although these errors are unlikely to be clinically important for staging purposes, they may be important for response assessment during and after treatment [23, 24]. In practice, many patients have already undergone a ceCT as part of the diagnostic workup and before referral to PET/CT. If performed, it is recommended that ceCT be performed during a single visit in combination with PET/CT.
1.7 The Need for Bone Marrow Biopsy
The Cotswold modifications to the Ann Arbor classification discouraged all invasive staging procedures with exception of bone marrow biopsy in selected patients [4]. While stand-alone CT is insufficient for evaluation of HL infiltration in the bone marrow, PET/CT detects areas of pathological skeletal FDG uptake suggestive of bone marrow involvement (BMI) in 10–20 % of the patients. PET-detected BMI is usually seen as areas of focally increased FDG uptake and often without accompanying morphological changes on CT [25–28] (Fig. 1.9). The fact that these lesions are seen in up to one-fifth of the patients has changed the old perception of bone marrow involvement being rare in HL. Most studies relying on bone marrow biopsy for detection of BMI only report frequencies of around 5–8 % for BMI in HL [29, 30]. The use of iliac crest bone marrow biopsy as a surrogate for the whole bone marrow compartment has been challenged by frequent finding of focal FDG lesions in the bone marrow in patients undergoing PET/CT staging. In addition, one-sided bone marrow involvement has been reported in nearly half of the HL patients undergoing bilateral bone marrow biopsies [31]. Directed biopsies and/or additional imaging with scintigraphy and MRI has supported the presence of HL in areas of otherwise unexplained focal FDG uptake in the bone marrow [21, 27]. Furthermore, there seems to be complete agreement between FDG uptake in the site of the bone marrow biopsy and results of bone marrow biopsy [32]. In conclusion, PET/CT has much higher sensitivity for bone marrow involvement than conventional bone marrow biopsy [33]. The few patients with BMI initially not detected by PET/CT but only by routine bone marrow biopsy almost exclusively present with advanced-stage disease based on the PET/CT findings, and therefore the added diagnostic information from bone marrow biopsies very rarely leads to changes in clinical management [25, 26]. The presence of diffuse FDG uptake throughout the whole axial skeleton without simultaneous focal lesions is a common finding in patients with newly diagnosed HL (Fig. 1.10). Despite FDG uptake at the sites of bone marrow biopsies, patients with this kind of diffuse FDG uptake in the bone marrow usually (but not always) present with negative bone marrow biopsies [25, 28, 34, 35]. Other findings suggest that inflammatory response may explain the diffuse FDG uptake in the bone marrow of HL patients since anemia and increased leukocyte count are associated with the presence of a diffuse FDG uptake [5, 17, 25, 36] Finally, a study has shown that there is a high degree of concordance in the reporting of PET/CT-ascertained bone marrow involvement [36]. The Lugano classification acknowledges the insignificant contribution of routine bone marrow biopsy to the baseline staging of HL by recommending against its use in PET/CT-staged HL patients [19, 37]. Thus, the last reminiscence of the pathological staging included in the original Ann Arbor classification has finally been eliminated.
1.8 Newer PET Tracers
Like other cancers, HL is characterized by deregulated cell cycle progression and most anticancer drugs are designed to inhibit cell proliferation. So a tracer enabling imaging of cell proliferation could be useful for both initial characterization and treatment monitoring of the disease. FDG uptake is somewhat correlated with cell proliferation, but this correlation is weakened by a number of factors, including FDG uptake in nonmalignant lesions [38, 39]. The nucleoside [11C]thymidine was the first PET tracer to specifically address cell proliferation. Early studies showed that [11C]thymidine could determine both disease extent and early response to chemotherapy in aggressive non-Hodgkin lymphoma (NHL) patients [40, 41]. However, the short 20 min half-life of 11C along with rapid in vivo metabolism has limited the clinical application of [11C]thymidine. The thymidine analogue 3′-deoxy-3′-[18F]fluorothymidine (FLT) offers a more suitable half-life of 110 min (same as FDG) and is stable in vivo [42]. More recent studies have shown that FLT-PET can sensitively identify lymphoma sites [43]. FLT uptake is highly correlated with proliferation rate and may thus be able to distinguish between high- and low-grade lymphomas [44, 45]. And furthermore, recent studies have showed a potential of FLT for imaging early response to treatment in lymphoma [46–49]. Amino acid metabolism of cancer cells is influenced by catabolic processes favoring tumor growth [50]. It has been shown that increased uptake of amino acids reflects the increased transport and protein synthesis of malignant tissue [51, 52]. This is the background for PET imaging of amino acid metabolism with the labeled amino acids l-[methyl-11C]methionine (MET) and O-2-[18F]fluoroethyl)-l-tyrosine (FET) [53]. Nuutinen et al. studied 32 lymphoma patients and found MET-PET highly sensitive for the detection of disease sites although there was no correlation between MET uptake and patient outcome [54]. While these results are encouraging, it should be noted that no studies have shown the usefulness or cost-effectiveness of amino acid or nucleoside tracers in large patient cohorts. Furthermore, high physiological tracer uptake in the abdomen limits the usefulness of these tracers for imaging of abdominal and pelvic lymphomas.
1.9 International Guidelines and the Lugano Classification
In recent years, several national and regional guidelines have included PET/CT in the recommended HL staging workup [55]. Recently, a revision of the international recommendations for staging and response assessment of lymphoma was published (the Lugano classification) [37]. These recommendations are accompanied by internationally accepted guidelines for the use of imaging in lymphoma [19]. Both the imaging recommendations and the staging guidelines recommend PET/CT for routine staging and response assessment of HL, and in patients with PET/CT staging, routine BMB is discouraged, based on the data presented above. The Lugano classification has abandoned the use of B symptoms (fever, night sweats, weight loss) as signs of disseminated disease in NHL, since these constitutional symptoms do not confer an unfavorable outcome according to the different NHL prognostic indices [56–58]. However, since the presence of one or more B symptoms is a prognostic factor in HL which still plays a role in treatment allocation, HL patients continue to be categorized into stages I–IV (primarily according to PET/CT) and with the suffix A or B (with or without B symptoms). In the imaging recommendations it is acknowledged that a 4-point staging classification is a rather crude representation of the modern, advanced imaging methods. Modern CT and PET methodology allows for advanced quantification of both anatomical and metabolic image information, and it is encouraged to explore the value of such quantitative measures in the near future. In a few years, the disease stage may very well be expressed as a precise volume and a metabolic intensity rather than as a number on a four-step scale.
References
Engert A, Diehl V, Franklin J, Lohri A, Dorken B, Ludwig WD, et al. Escalated-dose BEACOPP in the treatment of patients with advanced-stage Hodgkin’s lymphoma: 10 years of follow-up of the GHSG HD9 study. J Clin Oncol. 2009;27(27):4548–54.
Engert A, Plutschow A, Eich HT, Lohri A, Dorken B, Borchmann P, et al. Reduced treatment intensity in patients with early-stage Hodgkin’s lymphoma. N Engl J Med. 2010;363(7):640–52.
Carbone PP, Kaplan HS, Musshoff K, Smithers DW, Tubiana M. Report of the Committee on Hodgkin’s Disease Staging Classification. Cancer Res. 1971;31(11):1860–1.
Lister TA, Crowther D, Sutcliffe SB, Glatstein E, Canellos GP, Young RC, et al. Report of a committee convened to discuss the evaluation and staging of patients with Hodgkin’s disease: Cotswolds meeting. J Clin Oncol. 1989;7(11):1630–6.
Weiler-Sagie M, Bushelev O, Epelbaum R, Dann EJ, Haim N, Avivi I, et al. (18)F-FDG avidity in lymphoma readdressed: a study of 766 patients. J Nucl Med. 2010;51(1):25–30.
Bangerter M, Moog F, Buchmann I, Kotzerke J, Griesshammer M, Hafner M, et al. Whole-body 2-[18F]-fluoro-2-deoxy-D-glucose positron emission tomography (FDG-PET) for accurate staging of Hodgkin’s disease. Ann Oncol. 1998;9(10):1117–22.
Partridge S, Timothy A, O’Doherty MJ, Hain SF, Rankin S, Mikhaeel G. 2-Fluorine-18-fluoro-2-deoxy-D glucose positron emission tomography in the pretreatment staging of Hodgkin’s disease: influence on patient management in a single institution. Ann Oncol. 2000;11(10):1273–9.
Jerusalem G, Beguin Y, Fassotte MF, Najjar F, Paulus P, Rigo P, et al. Whole-body positron emission tomography using 18F-fluorodeoxyglucose compared to standard procedures for staging patients with Hodgkin’s disease. Haematologica. 2001;86(3):266–73.
Weihrauch MR, Re D, Bischoff S, Dietlein M, Scheidhauer K, Krug B, et al. Whole-body positron emission tomography using 18F-fluorodeoxyglucose for initial staging of patients with Hodgkin’s disease. Ann Hematol. 2002;81(1):20–5.
Cerci JJ, Trindade E, Buccheri V, Fanti S, Coutinho AMN, Zanoni L, et al. Consistency of FDG-PET accuracy and cost-effectiveness in initial staging of patients with Hodgkin lymphoma across jurisdictions. Clin Lymphoma Myeloma Leuk. 2011;11(4):314–20.
Hutchings M, Loft A, Hansen M, Pedersen LM, Berthelsen AK, Keiding S, et al. Position emission tomography with or without computed tomography in the primary staging of Hodgkin’s lymphoma. Haematologica. 2006;91(4):482–9.
Hutchings M, Loft A, Hansen M, Ralfkiaer E, Specht L. Different histopathological subtypes of Hodgkin lymphoma show significantly different levels of FDG uptake. Hematol Oncol. 2006;24(3):146–50.
Bednaruk-Młyński E, Pieńkowska J, Skórzak A, Małkowski B, Kulikowski W, Subocz E, et al. Comparison of positron emission tomography/computed tomography with classical contrast-enhanced computed tomography in the initial staging of Hodgkin lymphoma. Leuk Lymphoma. 2014;56(2):377–82.
El Galaly TC, Hutchings M, Mylam KJ, Brown Pde N, Bukh A, Johnsen HE, et al. Impact of 18F-fluorodeoxyglucose positron emission tomography/computed tomography staging in newly diagnosed classical Hodgkin lymphoma: fewer cases with stage I disease and more with skeletal involvement. Leuk Lymphoma. 2014;55(10):2349–55.
Grellier J, Vercellino L, Leblanc T, Merlet P, Thieblemont C, Weinmann P, et al. Performance of FDG PET/CT at initial diagnosis in a rare lymphoma: nodular lymphocyte-predominant Hodgkin lymphoma. Eur J Nucl Med Mol Imaging. 2014;41(11):2023–30.
Aleman BM, van den Belt-Dusebout AW, Klokman WJ, Van’t Veer MB, Bartelink H, van Leeuwen FE. Long-term cause-specific mortality of patients treated for Hodgkin’s disease. J Clin Oncol. 2003;21(18):3431–9.
Hutchings M. How does PET/CT help in selecting therapy for patients with Hodgkin lymphoma? ASH Educ Program Book. 2012;2012(1):322–7.
Girinsky T, van der Maazen R, Specht L, Aleman B, Poortmans P, Lievens Y, et al. Involved-node radiotherapy (INRT) in patients with early Hodgkin lymphoma: concepts and guidelines. Radiother Oncol. 2006;79(3):270–7.
Barrington SF, Mikhaeel NG, Kostakoglu L, Meignan M, Hutchings M, Mueller SP, et al. Role of imaging in the staging and response assessment of lymphoma: consensus of the International Conference on Malignant Lymphomas Imaging Working Group. J Clin Oncol. 2014;32(27):3048–58.
Chiaravalloti A, Danieli R, Caracciolo CR, Travascio L, Cantonetti M, Gallamini A, et al. Initial staging of Hodgkin’s disease: role of contrast-enhanced 18F FDG PET/CT. Medicine. 2014;93(8), e50.
Schaefer NG, Hany TF, Taverna C, Seifert B, Stumpe KDM, von Schulthess GK, et al. Non-Hodgkin lymphoma and Hodgkin disease: coregistered FDG PET and CT at staging and restaging – do we need contrast-enhanced CT? Radiology. 2004;232(3):823–9.
Chalaye J, Luciani A, Enache C, Beaussart P, Lhermite C, Evangelista E, et al. Clinical impact of contrast-enhanced computed tomography combined with low-dose 18F-fluorodeoxyglucose positron emission tomography/computed tomography on routine lymphoma patient management. Leuk Lymphoma. 2014;55(12):2887–92.
Vriens D, Visser E, de Geus-Oei L-F, Oyen W. Methodological considerations in quantification of oncological FDG PET studies. Eur J Nucl Med Mol Imaging. 2010;37(7):1408–25.
Berthelsen AK, Holm S, Loft A, Klausen TL, Andersen F, Højgaard L. PET/CT with intravenous contrast can be used for PET attenuation correction in cancer patients. Eur J Nucl Med Mol Imaging. 2005;32(10):1167–75.
El Galaly TC, d’Amore F, Mylam KJ, Nully Brown P, Bøgsted M, Bukh A, et al. Routine bone marrow biopsy has little or no therapeutic consequence for positron emission tomography/computed tomography-staged treatment-naive patients with Hodgkin lymphoma. J Clin Oncol. 2012;30(36):4508–14.
Weiler-Sagie M, Kagna O, Dann E, Ben Barak A, Israel O. Characterizing bone marrow involvement in Hodgkin’s lymphoma by FDG-PET/CT. Eur J Nucl Med Mol Imaging. 2014;41(6):1133–40.
Purz S, Mauz-Körholz C, Körholz D, Hasenclever D, Krausse A, Sorge I, et al. [18F]fluorodeoxyglucose positron emission tomography for detection of bone marrow involvement in children and adolescents with Hodgkin’s lymphoma. J Clin Oncol. 2011;29(26):3523–8.
Chen-Liang TH, Martin-Santos T, Jerez A, Senent L, Orero MT, Remigia MJ, et al. The role of bone marrow biopsy and FDG-PET/CT in identifying bone marrow infiltration in the initial diagnosis of high grade non-Hodgkin B-cell lymphoma and Hodgkin lymphoma. accuracy in a multicenter series of 372 patients. Am J Hematol. 2015;90(8):686–90.
Howell SJ, Grey M, Chang J, Morgenstern GR, Cowan RA, Deakin DP, et al. The value of bone marrow examination in the staging of Hodgkin’s lymphoma: a review of 955 cases seen in a regional cancer centre. Br J Haematol. 2002;119(2):408–11.
Levis A, Pietrasanta D, Godio L, Vitolo U, Ciravegna G, Di Vito F, et al. A large-scale study of bone marrow involvement in patients with Hodgkin’s lymphoma. Clin Lymphoma. 2004;5(1):50–5.
BRUNNING RD, BLOOMFIELD CD, McKENNA RW, PETERSON L. Bilateral trephine bone marrow biopsies in lymphoma and other neoplastic diseases. Ann Intern Med. 1975;82(3):365–6.
Adams H, Kwee T, Fijnheer R, Dubois S, Nievelstein R, de Klerk J. Bone marrow FDG-PET/CT in Hodgkin lymphoma revisited: do imaging and pathology match? Ann Nucl Med. 2015;29(2):132–7.
Adams HJA, Kwee TC, de Keizer B, Fijnheer R, de Klerk JMH, Littooij AS, et al. Systematic review and meta-analysis on the diagnostic performance of FDG-PET/CT in detecting bone marrow involvement in newly diagnosed Hodgkin lymphoma: is bone marrow biopsy still necessary? Ann Oncol. 2014;25(5):921–7.
Adams HJA, Kwee TC, Fijnheer R, Dubois SV, Nievelstein RAJ, de Klerk JMH. Diffusely increased bone marrow FDG uptake in recently untreated lymphoma: incidence and relevance. Eur J Haematol. 2015;95(1):83–9.
Chiang SB, Rebenstock A, Guan L, Alavi A, Zhuang H. Diffuse bone marrow involvement of Hodgkin lymphoma mimics hematopoietic cytokine-mediated FDG uptake on FDG PET imaging. Clin Nucl Med. 2003;28(8):674–6.
Zwarthoud C, Ouvier M, Borra A, Bergesio F, Chauvie S, Biggi A, et al. Patterns of PET/CT-assessed bone-marrow involvement in newly diagnosed Hodgkin lymphoma; a detailed review of 150 ABVD treated patients. Leuk Lymphoma. 2015;56:1233. Ref Type: Abstract.
Cheson BD, Fisher RI, Barrington SF, Cavalli F, Schwartz LH, Zucca E, et al. Recommendations for initial evaluation, staging, and response assessment of Hodgkin and Non-Hodgkin lymphoma: the Lugano classification. J Clin Oncol. 2014;32(27):3059–68.
Buck AK, Halter G, Schirrmeister H, Kotzerke J, Wurziger I, Glatting G, et al. Imaging proliferation in lung tumors with PET: 18F-FLT versus 18F-FDG. J Nucl Med. 2003;44(9):1426–31.
Sandherr M, von Schilling C, Link T, Stock K, von Bubnoff N, Peschel C, et al. Pitfalls in imaging Hodgkin’s disease with computed tomography and positron emission tomography using fluorine-18-fluorodeoxyglucose. Ann Oncol. 2001;12(5):719–22.
Martiat P, Ferrant A, Labar D, Cogneau M, Bol A, Michel C, et al. In vivo measurement of carbon-11 thymidine uptake in non-Hodgkin’s lymphoma using positron emission tomography. J Nucl Med. 1988;29(10):1633–7.
Shields AF, Mankoff DA, Link JM, Graham MM, Eary JF, Kozawa SM, et al. Carbon-11-thymidine and FDG to measure therapy response. J Nucl Med. 1998;39(10):1757–62.
Shields AF, Grierson JR, Dohmen BM, Machulla HJ, Stayanoff JC, Lawhorn-Crews JM, et al. Imaging proliferation in vivo with [F-18]FLT and positron emission tomography. Nat Med. 1998;4(11):1334–6.
Buchmann I, Neumaier B, Schreckenberger M, Reske S. [18F]3′-deoxy-3′-fluorothymidine-PET in NHL patients: whole-body biodistribution and imaging of lymphoma manifestations--a pilot study. Cancer Biother Radiopharm. 2004;19(4):436–42.
Buck AK, Bommer M, Stilgenbauer S, Juweid M, Glatting G, Schirrmeister H, et al. Molecular imaging of proliferation in malignant lymphoma. Cancer Res. 2006;66(22):11055–61.
Kasper B, Egerer G, Gronkowski M, Haufe S, Lehnert T, Eisenhut M, et al. Functional diagnosis of residual lymphomas after radiochemotherapy with positron emission tomography comparing FDG- and FLT-PET. Leuk Lymphoma. 2007;48(4):746–53.
Buck AK, Kratochwil C, Glatting G, Juweid M, Bommer M, Tepsic D, et al. Early assessment of therapy response in malignant lymphoma with the thymidine analogue [18F]FLT. Eur J Nucl Med Mol Imaging. 2007;34(11):1775–82.
Herrmann K, Buck AK, Schuster T, Rudelius M, Wester HJ, Graf N, et al. A pilot study to evaluate 3′-deoxy-3′-18F-fluorothymidine PET for initial and early response imaging in mantle cell lymphoma. J Nucl Med. 2011;52(12):1898–902.
Herrmann K, Buck AK, Schuster T, Junger A, Wieder H, Graf N, et al. Predictive value of initial 18F-FLT uptake in patients with aggressive non-Hodgkin lymphoma receiving R-CHOP treatment. J Nucl Med. 2011;52(5):690–6.
Graf N, Herrmann K, den Hollander J, Fend F, Schuster T, Wester HJ, et al. Imaging proliferation to monitor early response of lymphoma to cytotoxic treatment. Mol Imaging Biol. 2008;10(6):349–55.
Hoffman RM. Altered methionine metabolism, DNA methylation and oncogene expression in carcinogenesis. A review and synthesis. Biochim Biophys Acta. 1984;738(1-2):49–87.
Stern PH, Wallace CD, Hoffman RM. Altered methionine metabolism occurs in all members of a set of diverse human tumor cell lines. J Cell Physiol. 1984;119(1):29–34.
Wheatley DN. On the problem of linear incorporation of amino acids into cell protein. Experientia. 1982;38(7):818–20.
Leskinen-Kallio S, Ruotsalainen U, Nagren K, Teras M, Joensuu H. Uptake of carbon-11-methionine and fluorodeoxyglucose in non-Hodgkin’s lymphoma: a PET study. J Nucl Med. 1991;32(6):1211–8.
Nuutinen J, Leskinen S, Lindholm P, Soderstrom KO, Nagren K, Huhtala S, et al. Use of carbon-11 methionine positron emission tomography to assess malignancy grade and predict survival in patients with lymphomas. Eur J Nucl Med. 1998;25(7):729–35.
Eichenauer DA, Engert A, André M, Federico M, Illidge T, Hutchings M, et al. Hodgkin’s lymphoma: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2014;25 suppl 3:iii70–5.
A predictive model for aggressive non-Hodgkin’s lymphoma. The International Non-Hodgkin’s Lymphoma Prognostic Factors Project. N Engl J Med. 1993;329(14):987–94.
Solal-Celigny P, Roy P, Colombat P, White J, Armitage JO, Arranz-Saez R, et al. Follicular lymphoma international prognostic index. Blood. 2004;104(5):1258–65.
Hoster E, Dreyling M, Klapper W, Gisselbrecht C, van Hoof A, Kluin-Nelemans HC, et al. A new prognostic index (MIPI) for patients with advanced-stage mantle cell lymphoma. Blood. 2008;111(2):558–65.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Hutchings, M., Loft, A., El-Galaly, T.C. (2016). PET/CT for HL Staging. In: Gallamini, A. (eds) PET Scan in Hodgkin Lymphoma. Springer, Cham. https://doi.org/10.1007/978-3-319-31797-7_1
Download citation
DOI: https://doi.org/10.1007/978-3-319-31797-7_1
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-31795-3
Online ISBN: 978-3-319-31797-7
eBook Packages: MedicineMedicine (R0)