Abstract
The results of the lymphatic vessel transplantation have been objectified using different methods.
Volumes were measured before and after the surgery and compared to the contralateral limbs as far as possible following the method of Kuhnke. Hereby circumferences were measured in a distance of 4 cm, and the volumes of these disks with a height of 4 cm were added up to calculate the volume of the whole limb within the measured area.
With the help of independent investigators of the nuclear medicine and the radiology, function and patency of the grafts were examined.
Lymphoscintigraphies were performed before and after the surgery. The numeric lymphatic transport index was used to evaluate the findings. With this low-invasive method, repeated measurements were possible.
With the help of water-soluble contrast medium performing an indirect lymphography and later on using the sophisticated MRI lymphography, also long-term patency was proved in selected patients.
Quality of life assessment, specifically designed for patients with lymphedema and based on standard questionnaires, was developed and used for evaluation.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
4.1 Volume Measurement
Changes after any kind of edema treatment in extremities should be measured as exactly as possible. Measurements of circumferences at single points reflect the differences insufficiently.
Measurement of volumes is more accurate.
We used the method according to Kuhnke (1976) which is widespread in Germany. The volume is calculated from measuring the circumferences at a distance of 4 cm. The measuring can be simply performed just with the help of a tape measure.
Kuhnke described different ways of calculating (Kuhnke 1976, 1978).
The disk model is the most appropriate one. The volume of the disk with a height of 4 cm is calculated having measured the circumference.
Circumference and volume are connected according to the equation:
Since the height is 4, the equation is simplified:
The volumes of the disks are then added up and result in the volume of the extremity within the measured area (Fig. 4.1).
Different methods for calculating the volume have been described. They are comparable if used in the same way during the investigation.
The optoelectronic method calculates continuously the volume by measuring the diameter of the extremity in two directions, moving a frame over the extremity.
During the procedure of the water replacement method, the extremity is immersed into a tube filled with water, and the water which is driven out is measured.
These methods are basis of investigations from other groups.
4.2 Nuclear Medical Investigation
Another important way to follow the results of treatment is to assess the function of the lymphatic system.
In order to repeat the measurements, a low-invasive procedure is necessary.
For quantification different ways have been proposed. Determining and measuring regions of interest require a strict protocol to give reproducible results.
Therefore the Department of Nuclear Medicine at the LMU performed lymphoscintigraphies without determining regions of interest. It is stated that this is a low-invasive, versatile, simple technique, which may be suited well to assess lymphatic function.
Verbal description of lymphoscintigraphic findings alone however fails to evaluate the different findings.
Therefore visually five criteria were assessed and scored:
The lymphatic transport kinetics, K:
-
0, no delay
-
3, low-grade delay
-
5, extreme delay
-
9, missing transport
The distribution pattern, D:
-
0, normal distribution, i.e., nearly no background
-
3, partial diffuse (e.g., only in the surroundings of a knee)
-
5, diffuse distribution
-
9, transport stop
The time to appearance of lymph nodes, T:
-
Time in minutes to the first appearance of regional lymph nodes
-
9, no appearance
The assessment of lymph nodes, N:
-
0, clearly demonstrated
-
3, faint visualization
-
5, hardly recognizable
-
9, no visualization
The assessment of lymphatic vessels, V:
-
0, clearly demonstrated
-
3, faint visualization
-
5, hardly recognizable
-
9, no visualization
“The transport index (TI) is then calculated by the formula
The rational for this formula is that all criteria are considered as equivalent.
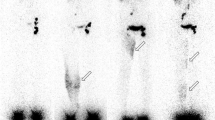
Score values range from 0 to 9 including all integer numbers. Thus, TI values range between 0 (normal) and 45 (pathological) (Fig. 4.2, Table 4.1).
Normalization of T (min) is performed by the factor 0.04, i.e., 200 min (maximal delay of lymph node appearance) yields the score value 8. No appearance is evaluated by 9.”
An interobserver study in 179 investigations was performed. A second observer reassessed the 179 limbs without knowledge of the results of the first observer. The mean difference for TI was rather small (2.61). The correlation was 0.96.
Using TI = 10 to discriminate between normal and pathologic lymph drainage in 122 investigation, 38 were found true positive, 75 true negative, 8 false positive, and only 1 false negative. Thus, sensitivity was 97.4 % and specificity 90.3%.
Although evaluation of lymphatic transport kinetics depends on the experience of the investigator, a good reproducibility was demonstrated (r = 0.96).
Therefore, that quantification of scintigraphic findings has proved very useful especially in follow-up studies. This method was used therefore to control the effect of reconstructive lymph vascular surgery in different studies (Kleinhans et al. 1985; Weiss et al. 2002, 2003).
All patients are investigated prior to surgery. At the lower extremity, the possibility of harvesting is clarified by lymphoscintigraphy, looking for a possible deficiency in lymphatic transport. At the edematous extremity, lymphoscintigraphy is performed in order to get an impression about the severity of the disturbance in lymphatic transport. Additionally it provides information about residual areas of less disturbed lymphatic outflow, and it serves as basic information for follow-up studies (Weiss et al. 2015a). About 1 year after surgery and for follow-up studies, lymphoscintigraphies are performed at the affected extremities. Figure 4.3 shows the example of a normal lymphoscintigraphy at the lower extremity. It was performed in order to check the possibility for harvesting a lymphatic graft.
In a recent study also the sequela of the harvest with respect of the lymphatic transport at the donor limb was investigated. In 19 consecutive patients 49 months after the harvest all values of the TI were close to the preoperative value and within the normal range. The results showed that microsurgical transfer of lymph vessel grafts is possible without compromising lymphatic drainage of the donor limb if safety precautions are taken into account ( Weiss et al. 2015b).
4.3 Indirect Lymphography
To prove the patency of lymphatic grafts by direct visualization is difficult.
Oily contrast medium was a long time used agent. However it harms the lymphatic vessels. In our experiments we found lymphatic anastomoses occluded after contact with the contrast medium. Furthermore, it would be necessary to sacrifice a lymphatic vessel in order to perform the injection.
Water-soluble contrast medium is another possibility to show lymphatic vessels. The contrast medium should be administered subepidermally at an average infusion rate of 0.12 ml/min with the aid of thin butterfly needles (size 20–25) and an infusion pump. Exact subepidermal positioning of the tip of the needle is of paramount importance to facilitate a “contrast depot” from which lymphatics fill (Partsch et al. 1988).
According to our experience, lymphatic vessels are shown normally in a distance of several centimeters. Occasionally however the dye finds its way to more distant located bigger vessels. In these cases also the grafts can be visualized.
The example in Fig. 4.4 shows a lymphatic graft above the clavicle 4 years after bypassing the axilla. Visualization was possible with the help of indirect lymphography using water-soluble contrast medium (Isovist®).
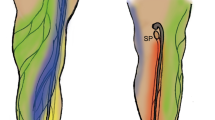
4.4 MRI Lymphangiography
Vascular surgery needs urgently a method to visualize the vessels. Advancements are necessary in order to visualize the tiny lymphatic vessels not only superficial beneath the skin like indocyanine green method or at short distances like the indirect lymphography. MR lymphangiography is a promising method to visualize the lymphatic without such restrictions. Contributions for further development have been made by the Institute for Clinical Research at the LMU. Since the method is elaborated, only in selected patients MRI lymphangiography has been used to prove patency and to clarify the lymphatic system preoperatively.
“MR-lymphangiography (MRL) with extracellular gadolinium derivatives has been shown by Lohrmann et al. (2006) to be a safe and feasible investigation for primary and secondary lymphedema, providing valuable anatomical information with high spatial and temporal resolution.
With MRL, the entire lower extremity can be examined in several steps. Fat-saturation techniques render image subtraction dispensable and allow for time-efficient acquisition (Lohrmann et al. 2007).
However, in plane resolution of MRL is limited at 1.5 Tesla (1,2,x1,2x1,1 mm3) following constraints associated with the field strength (Lohrmann et al. 2008), so that the depiction of typically delicate lymph vessels, with sub-millimeter diameters, may be difficult (Lohrmann et al. 2006).
The introduction of higher field strength at 3.0 Tesla and multichannel coils provide a higher signal gain, which can be invested in high spatial resolution and isotropy to generate 3D data sets with options for 3D postprocessing (Michaely et al. 2007).
Furthermore, parallel imaging techniques reduce acquisition time with negligible signal penalty (Schoenberg et al. 2005). This high-resolution depiction of lymph vessels may help to enhance the understanding of anatomical and morphological details and to identify potential donor vessels for lymph-vessel transplantation, information that is crucial in selected patients when physiotherapy is not effective enough (Baumeister et al. 1981).”
The introductory remarks by Notohamiprodjo et al. (2009) for a feasibility study regarding MR lymphangiography at 3.0 T describe the development of MR lymphangiography very well.
After injection of gadolinium, lymphatic vessels are visualized along the extremity. For lymph vascular surgery, it is important that also the main collectors which run above the fascia are visualized. Figure 4.5 shows an example of a normal MRI lymphography of the lower extremity.
Since the potential of MRL at 3.0 Tesla with parallel imaging techniques and ultrahigh spatial resolution was unknown, a prospective study was performed to establish an imaging protocol for contrast-enhanced MRL of the lower extremity to investigate the value of this technique to visualize peripheral lymphatic vessels and to describe the MR morphology of normal and abnormal lymphatic vessels in extremity lymphedema (Notohamiprodjo et al 2009).
This is of special interest for the investigation in primary lymphedema since the knowledge of the status of lymphatic vessels is crucial to clarify the possibility for lymphatic vessel transplantation.
Sixteen patients were examined with a highly resolved isotropic T1w-3D-GRE-(FLASH) sequence (TR 3.76 ms/TE 1.45 ms/FA 30°/voxel size 0.8 × 0.8 × 0.8 mm3) at 3 Tesla MRI after intracutaneous injection of gadolinium-diethylenetriamine-pentaacetic acid.
Two radiologists evaluated overall image quality, contrast between the lymphatic vessels and background tissue, venous contamination, visualized levels, and fat saturation homogeneity on 3D maximum intensity projections.
Overall image quality was good to excellent, and all examinations were diagnostic except one, where contrast medium was injected subcutaneously instead of intracutaneously.
Overall image quality was good to excellent in 12/16 cases. Depiction of lymphatic vessels was good to excellent in 15/16 cases. Venous contamination was always present, but diagnostically problematical in only one case.
Instant lymph drainage was observed in unaffected extremities, reaching the pelvic level after approximately 10 min.
Lymph drainage was considerably delayed in lymphedematous extremities. Ectatic lymphatic vessels, entrapment, and diffuse drainage of contrast medium correlated with impaired lymph drainage.
Based on these findings, MRL became a valuable tool for microsurgical treatment planning especially in primary lymphedemas and in patients with lymphatic fistulas and lymphoceles.
Also monitoring in selected cases with and without comparing to the functional findings in lymphoscintigraphy was successfully performed (Notohamiprodjo et al. 2012).
4.5 Quality of Life Assessment
In evidence-based medicine, studies are generally based on objectivity, and treatment outcomes are assessed by their effects. Particularly for chronic and malignant diseases, which impair patient’s everyday life, it is necessary to apply additional and new criteria to judge the outcomes. Outcomes of medical treatment assessed traditionally by parameters like “death rate” or “survival rate” are now evolving to not only “whether” or “for how long” there is a possibility of survival but “how is the life worth living” and “how harmful” is the situation which may be the most important points of view particularly from the patient’s perspective (Koller and Kussmann 1995).
To assess general health and whether lymphatic vessel transplantation was a successful treatment from the patient’s point of view, we developed a specially designed questionnaire (Springer 2011; Springer et al. 2012). We started with the standardized SF-12 quality of life instrument. This is a shortened form of the SF-36: It has been used for many years as an instrument to evaluate quality of life in different diseases (Jenkinson and Layte 1997).
The questions were then adapted to the main known complaint problems from patients with lymphedema.
We added two more questions to evaluate the possible burden caused by the amount of time that was needed for conservative therapy and the impairment of wearing compression garments.
In order to guarantee an objective observation, we first tested the questionnaire for comprehensibility and suitability. Six patients (three males and three females), who were undergoing treatment and were not included in our study, were asked to fill out the questionnaires. The questionnaires were also tested by six members of the staff (two female nurses, a male nurse, one doctor, and a medical student). Every participant rated the questionnaire as comprehensible and had no problems answering the questions.
We separated the questionnaire into two major sections with the first part assessing the period prior to the surgery and the second part after lymphatic vessel transplantation. Each section addressed three major themes: physiological conditions, psychological conditions, and burden of conservative therapy.
Each question had five possible answers ranging from 1 (least harming with highest quality of life) to 5 (most harming with lowest quality of life). By utilizing a numerical scoring system, comparisons were accomplished by simply adding the number of points in the different parts of the survey for analysis. Scores were averaged for upper and lower limbs for each theme, standard error determined, and values used for before and after operation comparisons. All pre- and postoperative measurements and comparisons were evaluated with Mann-Whitney rank sum test, and significance was determined by p ≤ 0.001 using SPSS.
4.5.1 Questions Regarding Physiological Conditions
This section includes four questions that assessed common problems for patients with lymphedema caused by the pressure of swollen tissue and skin: intensity of swelling, pain, paresthesias, and difficulty to work. The additional physiological question inquired about occurrence of skin infections and erysipelas.
4.5.2 Questions Regarding Psychological Conditions
This section contained four questions focusing on the social everyday and family life of the patients such as difficulties to get appropriate clothing, stigmatization, problems with the partner, and necessity to disclose the origin of the edema.
4.5.3 Questions Regarding Possible Burden of Conservative Therapy
This section consisted of two questions focusing on the burdens of conservative therapy including frequency of received manual lymph drainage and the impairment caused by wearing special compressive stockings.
References
Baumeister RGH, Seifert J, Hahn D (1981) Autotransplantation of Lymphatic Vessels. Lancet, Jan 17: 147
Jenkinson C, Layte R (1997) A shorter form health survey: can the SF-12 replicate results from the Sf-36 in longitudinal studies? J Public Health Med 19:179–209
Kleinhans E, Baumeister RG, Hahn D, Siuda S, Büll U, Moser E (1985) Evaluation of transport kinetics in lymphoscintigraphy: follow up study in patients with transplanted lymphatic vessels. Eur J Nucl Med 10:349–352
Koller M, Kussmann J (1995) Die Erfassung und Dokumentation der Lebensqualität nach Tumortherapie. Organspezifische Tumordokumentation. Springer, Berlin/Heidelberg
Kuhnke E (1976) Volumenbestimmung aus Umfangsmessungen. Folia Angiol 24:228–232
Kuhnke E (1978) Die Volumenbestimmung entrundeter Extremitäten aus Umfangsmessungen. Lymphologie 2:35–44
Lohrmann C, Foeldi E, Speck O, Langer M (2006) High-resolution MR lymphangiography in patients with primary and secondary lymphedema. AJR Am J Roentgenol 187:556–561
Lohrmann C, Foeldi E, Bartholoma JP, Langer M (2007) Magnetic resonance imaging of lymphatic vessels without image subtraction: a practicable imaging method for routine clinical practice? J Comput Assist Tomogr 31:303–308
Lohrmann C, Felmerer G, Foeldi E, Bartholoma JP, Langer M (2008) MR lymphangiography for the assessment of the lymphatic system in patients undergoing microsurgical reconstructions of lymphatic vessels. Microvasc Res 76:42–45
Michaely HJ, Kramer H, Attenberger U, Sourbron SP, Weckbach S, Reiser MF, Schoenberg SO (2007) Renal magnetic resonance angiography at 3.0 T: technical feasibility and clinical perspectives. Top Magn Reson Imaging 18:117–125
Notohamiprodjo M, Baumeister RGH, Jakobs TF, Bauner K, Boehm H, Horng A, Reiser MF, Glaser C, Herrmann KA (2009) MR-lymphangiography at 3.OT- a feasibility study. Eur Radiol 19:2771–2778
Notohamiprodjo M, Weiss M, Baumeister RGH, Sommer WH, Helck A, Crispin A, Reiser MF, Herrmann KA (2012) MR lymphangiography at 3.0.T: correlation with lymphoscintigraphy. Radiology 264:78–87
Partsch H, Stöberl C, Urbanek A, Wenzel-Hora BI (1988) Clinical use of indirect lymphography in different forms of leg edema. Lymphology 21:152–160
Springer S (2011) Veränderungen der Extremitätenvolumina und der Lebensqualität durch Lymphgefäßtransplantation bei Patienten mit Lymphödem. Inauguraldissertation LMU, München
Springer S, Koller R, Baumeister RGH, Frick A (2012) Changes in quality of life of patients with lymphedema after lymphatic vessel transplantation. Lymphology 44:65–71
Schoenberg SO, Rieger J, Weber CH, Michaely HJ, Waggershauser T, Ittrich C, Dietrich O, Reiser MF (2005) High-spatial-resolution MR angiography of renal arteries with integrated parallel acquisitions: comparison with digital subtraction angiography and US. Radiology 235:687–698
Weiss M, Baumeister RGH, Hahn K (2002) Post-therapeutic Lymphedema: scintigraphy before and after autologous lymph vessel transplantation 8 years of long-term follow-up Clin Nucl Med 27:788–792
Weiss M, Baumeister RGH, Hahn K (2003) Therapieplanung und Erfolgskontrolle der autologen Lymphgefäßtransplantation mittels nuklearmedizinischer Lymphabflussszintigraphie. Handchir Mikrochir Plast Chir 35:210–215
Weiss M, Baumeister RGH, Frick A, Wallmichrath J, Bartenstein P, Rominger A (2015a) Lymphedema of the upper limb evaluation of the functional outcome by dynamic imaging of lymph Kinetics after autologous lymph vessel transplantation. Clin Nucl Med 40:e117–e123
Weiss MF, Baumeister RGH, Zacherl MJ, Frick A, Bartenstein P, Rominger A (2015b) Microsurgical autologous lymph vessel transplantation: does harvesting lymphatic vessel grafts induce lymphatic transport disturbances in the donor limb? Handchir Mikrochir Plast Chir 47:359–364
Author information
Authors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Baumeister, R.G.H. (2017). Methods for Objectification of the Results. In: Reconstructive Lymph Vascular Surgery. Springer, Cham. https://doi.org/10.1007/978-3-319-31647-5_4
Download citation
DOI: https://doi.org/10.1007/978-3-319-31647-5_4
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-31645-1
Online ISBN: 978-3-319-31647-5
eBook Packages: MedicineMedicine (R0)