Abstract
The knowledge about the normal and abnormal vaginal microbiome has changed over the last years. Culturing techniques are not suitable any more for determination of a normal or abnormal vaginal microbiota. Non culture-based modern technologies revealed a complex and dynamic system mainly dominated by lactobacilli.
The normal and the abnormal vaginal microbiota are complex ecosystems of more than 200 bacterial species influenced by genes, ethnic background and environmental and behavioral factors. Several species of lactobacilli per individuum dominate the healthy vagina. They support a defense system together with antibacterial substances, cytokines, defensins and others against dysbiosis, infections and care for an normal pregnancy without preterm birth.
The numbers of Lactobacillus (L.) iners increase in the case of dysbiosis.
Bacterial vaginosis (BV) – associated bacteria (BVAB), Atopobium vaginae and Clostridiales and one or two of four Gardnerella vaginalis – strains develop in different mixtures and numbers polymicrobial biofilms on the vaginal epithelium, which are not dissolved by antibiotic therapies according to guidelines and, thus, provoke recurrences.
Aerobic vaginitis seems to be an immunological disorder of the vagina with influence on the microbiota, which is here dominated by aerobic bacteria (Streptococcus agalactiae, Escherichia coli). Their role in AV is unknown.
Vaginal or oral application of lactobacilli is obviously able to improve therapeutic results of BV and dysbiosis.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
6.1 A Historic Perpective
Albert Döderlein (1860–1941) was the first one to discover the importance of lactic acid producing bacteria in the vagina (Döderlein 1892). Krönig (1895), a co-worker of Döderlein, described lactobacilli as anaerobic and curved rods, which were later cultured by Curtis (1913) and named Mobiluncus curtisii (Spiegel and Roberts 1984). Finally, Stanley Thomas (1928) coined the term Lactobacillus acidophilus. In the 1980s Lauer, Helming and Kandler were able to distinguised several Lactobacillus species previously termed L. acidophilus by DNA-DNA hybridisation.
At the beginning of the last century first attempts were made to grade the vaginal microbiota. Manu af Heurlin (1914) characterised the vaginal microbiota of children, pregnant and not pregnant women and women of old age and tried to establish grades of healthines. Robert Schröder (1921) was the first one to define three bacteriologically different vaginal microbiota types termed “Reinheitsgrade” (grades of purity). Otto Jirovec (Jirovec et al. 1948) distinguished between six vaginal microbiota types (normal, abnormal, abnormal with many leucocytes, gonorrhea, trichomoniasis, candidosis).
In 1955 Herman Gardner and Charles Dukes (1955) described Haemophilus vaginalis, later renamed as Gardnerella vaginalis (Greenwood and Pickett 1980) as the main causative for bacterial vaginosis (BV), the most common disturbance of the vaginal microbiota and considered it as a sexually transmitted disease. Furthermore, they emphasised the importance of microscopy and defined “clue cells” as diagnostic marker.
By the end of the last century the hitherto valid definition of bacterial vaginosis was described as “a replacement of lactobacilli by characteristic groups of bacteria accompanied by changed properties of the vaginal fluid” (Mardh et al. 1984). With the advent of molecular and genetic technologies we had to reconsider our view and definition of a normal vaginal microbiota. New bacteria were discovered and the concepts of a bacterial biofilm and of vaginal microbiota types was introduced.
6.2 Normal Vaginal Microbiota
The outer and inner surfaces of a child born by vaginal delivery are primarily colonised by the vaginal microbiota of the mother. Futher colonisers are aquired from the skin and mouth microbiota of the mother. In the last years it became evident that mothermilk harbours a unique microbiota, mainly dominated by Lactobacilli, which is transfered to the suckling child (Martin et al. 2003). Before the menarche the vagina microbiota is a unsteady mix of skin and gut microbes, which may harbor some lactobacilli (Fettweis et al. 2012). The environmental conditions for lactobacilli become improved by estrogens and progesterone with the start and during the reproductive phase of women. Estrogens support the proliferation of the vaginal epithelium and the development of intraepithelial glycogen, while progesterone supports the cytolysis of epithelial cells, which release glycogen. Lactobacilli and other bacteria are able to metabolise this glycogen to glucose and maltose and further to lactic acid. This leads to a vaginal pH of 3.8–4.4 which is defined as normal.
Until now more than 120 lactobacillus species have been described (de Vos et al. 2012). Within the vaginas of women of reproductive age more than ten different species can be found. However, a single women is usually dominated by one or two species, of which the most frequent are L. crispatus, L. gasseri, L. jensenii and L. iners (Vasquez et al. 2002). Several of these lactobacilli are able to produce bacteriocines, biosurfactants and coaggregating molecules to inhibit the adhesion of pathogens (Reid 2001). Another property of lactobacilli found within the vagina is the ability to produce hydrogen peroxid (H2O2). Lactobacilli are by definition strict anaerobic bacteria. However, they are often found in niches enriched with oxygen. To detoxify the otherwise toxic oxygen, several but not all lactobacilli are able to produce H2O2. The presence of H2O2 producing lactobacilli is negatively associated with the formation of BV (Eschenbach et al. 1989).
6.2.1 The Normal Vaginal Microbiota: A Mixture of Many Bacteria in a Balance
Currently, the dogma, that a healthy vaginal microbiota is dominated by lactobacill is faltering as by genomic sequencing over 250 species of bacteria have been identified in the vagina (Li et al. 2012). Besides Lactobacilli many other bacteria can be found in the normal or abnormal vaginal microbiota, such as Actinomyces, Aerococcus, Allisonella, Alloscardovia, Anaerococcus, Arcanobacterium, Atopobium, Bacteroides, Balneimonas, Bifidobacterium, Blastococcus, Blautia, Bulleidia, Campylobacter, Citrobacter, Coriobacteriacea, Corynebacterium, Enterobacter, Escherichia, Facklamia, Faecalibacterium, Finegoldia, Gardnerella, Gemella, Haemophilus, Lachnospiracea, Massilia, Megasphera, Mobiluncus, Mollicutes, Moryella, Olsinella, Parvimonas, Peptinophilus, Peptostreptococcus, Prevotella, Porphyromonas, Proteobacteria, Providencia, Rhizobialis, Ruminococcaceae, Salmonella, Shigella, Shuttleworthia, Sneathia, Solobacterium, Staphylococcus, Streptococcus, Veillonella, Ureaplasma, and many lactobacilli species (Gajer et al. 2012).
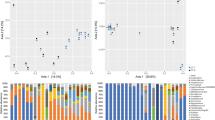
Within the human microbiome project, the vaginal microbiome project investigated the relationship between the vaginal microbiota and various physiological and infectious conditions (Fettweis et al. 2012). Various “vagitypes” have been identified of which many are dominated by a single bacterial taxon, others by a broad spectrum of different bacteria. Interestingly the ethnic background of women has an influence on the vaginal microbiota, as white/caucasian women are dominated by L. iners, asian women by L. crispatus and black and hispanic women by L. jenseni. However, a significant group of women harbored no lactobacilli in the vagina (Ravel et al. 2011, Hickley et al. 2012).
Jespers et al. (2012) identified in Antverpen/Belgium similarly three types of vaginal microbiota in healthy premenopausal women and in women at risk for BV of a STD clinic.
One group of women was dominated by L. crispatus, L. iners, L. jensenii and L. vaginalis with lower counts (<30 %) of L. gasseri and Atopobium vaginae. A second group harbored preferentially L. gasseri and L. vaginalis, but less L. jensenii, L. iners or L. crispatus. The third group was dominated by L. gasseri, A. vaginae and L. iners. Whithin the third group were mainly african and asian women. These flora types underly dynamic variations during the menstrual cycle and are influenced by external circumstances, for instance sexual behavior. But they seem to be in a rather stable balance, and a healthy vaginal system can obviously be strong enough to correct disturbences from outside, as Gajer et al. (2012) demonstrated in a longitudinal study. Women were grouped according to Ravel’s et al. (2011) “community state types” and vaginal swaps were taken for 16 successive weeks. Furthermore, menstruation, tampon use, vaginal, anal or oral sex, sex toys, digital penetration and lubricants were documented. It was evident, that the vaginal microbiota of several women became heavily disturbed by some of these actions, however other microbiotas showed no disturbences despite very frequent manipulations. Once again, black women were significantly different in their “community state types”.
The vaginal flora is influenced by the anal and the oral flora. Petricevic et al. (2012) found in around 80 % of 30 pregnant women and in 40 % of 30 postmenopausal women one or more Lactobacillus ssp. in the vagina and in the rectum, and they were in 80 % resp. 40 % of the same identity. These women were also in 50 % (pregnant) and in 30 % (postmenopausal) colonised by one or more Lactobacillus ssp. in their mouth. A healthy vaginal, balanced microbiota protects not only against ascending infections or HIV acquisition, but also against prematurity (Hoyme and Hübner 2010; Donders et al. 2011; Lamont et al. 2011; Martin 2012; Mendling et al. 2013).
On the other hand, too many vaginal lactobacilli (Cibley and Cibley 1991) or abnormal long lactobacilli (Horowitz et al. 1994) can cause vestibular pruritus, itching and dysuria. This “cytolytic vaginosis” or “lactobacillosis” can be misdiagnosed clinically as candidosis (Demirezen 2003).
6.2.2 Gene Polymorphisms and Vaginal Immunity
The vaginal microbiota is not only influenced by the ethnic background, but also by gene polymorphisms: the individual capacity to produce low or high levels of anti- or pro-microbial factors influences the composition of the vaginal microbiota. Polymorphisms in the interleukin-1 receptor antagonist gene or the Toll-like receptor (TLR) 4, which acts in the innate recognition of Gram-negative bacteria, influence the quantity of vaginal bacteria (Rodriguez et al. 1999) and can influence individual susceptibility to pregnancy complications (Genc and Onderdonk 2011). Such polymorphisms vary between different racial groups and may be associated with the different ecosystems between different populations (Linhares et al. 2010). Interestingly, periodontal disease and BV are influenced by gene polymprphisms and are both associated with preterm birth (Sanu and Lamont 2011).
The innate immune system of the vagina is represented by soluble factors like mannose-binding lectin (MBL), defensins, secretory leucocyte protease inhibitor, nitric oxid, and membrane-associated factors, the TLR (11 TLR have been identified) and phagocytes. Different TLR recognize lipoproteins and peptidoglucan in the surface of Gram-positive bacteria, the lipopolysaccharid of Gram-negative bacteria, flagellins, and others (Linhares et al. 2010; Mirmonsef et al. 2011). Vaginal cells release defensins with a non-specific antimicrobial activity. The production of special defensins is stimulated by estrogens and inhibited by progesterone. Bacterial vaginosis in pregnant women was associated with lower vaginal concentrations of defensin 3 (Mitchell et al. 2013). Women with MBL deficiency due to a polymorphism are more susceptible to recurrent Candida albicans vaginitis (Babula et al. 2003).
Toll-like receptor ligands and fatty acids, which are produced by many vaginal bacteria, have dramatic effects on the vaginal immune function: the anaerobes of BV produce bad smelling amines (putrescin, cadaverin and others), succinate, sialidases, and immunomodulatory substances such as lipopolysaccharides, lipoteichoid acids and peptidoglycans with many influences on cytokines and other immune responses (Mirmonsef et al. 2011).
6.3 Abnormal Vaginal Flora
A disturbed vaginal microbiota may be the cause for various diseases. However, within this chapter only two will be discussed, as only they are directly connected to a dysbiotic vaginal microbiota.
6.3.1 Bacterial Vaginosis (BV)
Gardner and Dukes (1955) named the vaginal disorder Haemophilus vaginalis vaginitis and described “clue cells”. It was later characterized as bacterial vaginosis and is defined by a replacement of lactobacilli with characteristic groups of bacteria accompanied by changed properties of the vaginal fluid (Weström et al. 1984).
The first diagnostic criteria for BV were published by Amsel et al. (1983): grey-white milky discharche, pH >4.5, bad “fishy” smell, especially if 10 % KOH solution is added, and at least 20 % “clue cells”. Later, Eschenbach et al. (1989) determined the lack of H2O2-producing lactobacilli, an overgrowth of G. vaginalis and anaerobic Gram – negative rods and anaerobic Gram – positive cocci as essential factors for the presence of BV. To improve the diagnostic analyis, Nugent et al. (1991) poposed a score (Nugent score): 0–3 = normal, 4–6 = intermediate, 7–10 = BV. It is solely based on Gram-staining criteria. However, it has been reported, that roughly 20 % of pregnant women in Germany have BV by definition, but not all suffered from symptoms (Mendling et al. 2013).
The development of BV was long associated with the presence of G. vaginalis. Currently, four different G. vaginalis strains have been described, of which only two produce the BV marker sialidase and only one predominated in women with BV (Jayaprakash et al. 2012). Hence, the existance of G. vaginalis in the vagina is no precondition of BV. In the last years it became evident, that no single strain alone is the cause of BV. Recently, BV associated bacteria (BVAB) 1, 2 and 3 have been described. Nearly all of these bacteria are unknown in clinical practice. Women, who harbor BVAB, especially G. vaginalis and Leptotrichia/Snethia or Megasphera in higher concentrations, develop significantly more BV (p = 0.001) (Marrazzo et al. 2012; Hillier et al. 2010). Additionally, Fredricks et al. (2005) demonstrated that the presence of L. iners is strongly associated with BV. L. iners, which belongs to the normal microbiota, but seems to be a “poisened apple in the basket”, because its presence is strongly connected with a shift of normal to abnormal microbiota. On the other hand, Women, who harbor L. crispatus are significantly less at risk to develop BV than others (p = 0.02).
BV is influenced by environmental and genetic factors. Thus, gene polymorphisms influence the occurrence of G. vaginalis and A. vaginae (Verstraelen et al. 2009). Furthermore, decreasing estrogen levels influence the number and diversity of vaginal lactobacilli and are in some women a risk factor for urogenital infections.
Sexual practices, especially receptive oral sex and digital vaginal penetration are significant risk factors for BV (which is perhaps an explanation for a higher risk of BV in lesbian women (Marrazzo et al. 2012)), and also cigarette smoking, black race, receptive anal sex before vaginal intercourse (Cherpes et al. 2008; Manhart et al. 2012). It should be kept in mind, that Gardner and Dukes (1955) could not cause BV by transferring cultivated G. vaginalis from a woman with BV to a healthy woman, but if they transferred the discharge of a woman with BV to a healthy vagina, this woman got BV. Hence, not single bacteria, albeit in high numbers, is important, but a critical mixture of BVAB together with special lactobacilli, and a lack of other lactobacilli seem to play a role in the development of BV (Lamont et al. 2011). Lamont et al. (2011) discussed, “that it is whether or not the strain/species of Lactobacillus produces H2O2 that dictates whether BV is present or absent. However, given that H2O2 – producing L. gasseri are found in BV patients, albeit at lower incidence, one might also argue that in vitro production of H2O2 is only a biomarker of a protective species of Lactobacillus, not an active factor in limiting the growth of vaginal anaerobes.”
6.3.2 Polymicrobial Bacterial Biofilms in BV and Sexual Transmission
A biofilm is defined as any group of microorganisms in which cells stick to each other on a surface. The first biofilm in gynecology was described in women with BV by Swidsinski et al. (2005). The epithelial cells of the vagina of healthy pre- or postmenopausal women or of children are free of bacteria. But BV is characterized by structured polymicrobial biofilms adherent to epithelial cells of the vagina. “Clue cells”, which Gardner and Dukes (1955) have seen microscopically on vaginal epithelial cells of the discharge, have their origin from this biofilm – coat on the vaginal wall. The biofilm consists in its majority of G. vaginalis (>50 % up to 90 %) and of A. vaginae (10–40 %), but also of lactobacilli and other bacteria. G. vaginalis formes in vitro significantly stronger biofilms, if Fusobacterium nucleatum or Prevotella bivia are added (Machado et al. 2013). No BV is equal in the composition of different bacteria and no biofilm of BV is equal.
It is unknown, whether the lactobacilli found in the biofilm are L. iners or other species. If treated with metronidazole, it does not get disrupted and, thus, seems to be the reason for the high recurrence rates of about 30 % after 3 months and 60 % after 6 months following therapy, respectively.
In addition to be present in the vagina, the BV-typical biofilm can be found on epithelial cells in the urine of females with BV and in the urine of their partners. Sometimes it may be found in cryopreserved donor semen, in the endometrium of non-pregnant women and in tissue of missed abortion/abortion (Swidsinski et al. 2013). If men were asked to void their urine after having pulled back the preputium, no biofilm was found, which confirms the observation that male circumcision reduces the risk for ulcerations, trichomoniasis and BV (Gray et al. 2009). Circumcision is associated with a significant change in the microbiota and with a significant decrease in putative anaerobic bacteria, especially Clostridiales and Prevotellaceae (Price et al. 2010). Women with treated BV have a higher risk for recurrence, if they have intercourse with the same partner without using condoms (Marrazzo et al. 2012; Guédou et al. 2013).
6.3.3 Aerobic Vaginitis (AV)
In 2002 Donders et al. (2002) characterised a new type of vaginitis. It is in contrast to BV dominated by aerobic bacteria, mainly Streptococcus agalactiae and Escherichia coli and named aerobic vaginitis (AV). The patients suffer from yellow-green discharge, the vagina is red by inflammation, the pH is 5.5–6.5, many toxic leucocytes, parabasal cells and a sparse coccoid flora without lactobacilli dominate the microscopic field. High levels of interleukin – 1 beta, – 6, – 8 and leukaemia inhibiting factor in contrast to BV. Severe cases resemble to desquamative inflammatory vaginitis, which is discussed to be an early form of Lichen ruber of the vagina. AV is a higher risk factor for preterm labour and preterm birth than BV (Donders et al. 2011). Some believe, that AV is primarily an immunologic disorder with secondary abnormal microbiota, or a dermatological disease in the vagina (Edwards 2010). Women with AV are at risk for low grade cervical squamous intraepithelial cell lesions (Jahic et al. 2013). About 5 % of women in reproductive age are suffering from AV, but some diagnosed it in a much higher frequence of 23 % (Fan et al. 2013). But partner treatment is without benefit for the woman with BV.
6.4 Prophylaxis and Therapy with Probiotics
Probiotics are microorganisms that provide a health benefit to the host. They act in the gastrointestinal tract and influence in various ways the immune system (Sherman et al. 2009). Although lactobacilli are in use for prophylaxis or treatment of vaginal discharge since decades, probiotic research devoleped rapidly over the last 30 years within the field of gynaecology (Spurbeck and Arvidson 2011; Reid 2012). One of the first clinical studies proposed the daily oral application of about 250 g Yoghurt containing L. acidophilus for 6 months to women with recurrent candida vulvovaginitis. The mean rate of recurrences in the control arm was 2.5 versus 0.38 in the yoghurt arm (p = 0.001) (Hilton et al. 1992). Since then, several species have been tested in various studies. L. rhamnosus Lcr 35 (Coudeyras et al.2008a, b) showed increased ability to metabolise glycogen to lactic acid and in vitro growth inhibition of G. vaginalis and C. albicans. The effect was higher after the manufactering process than compared to three other L. rhamnosus strains (Nivoliez et al. 2012). Lcr 35 adheres to cervicovaginal cells and is an antagonist of BVAB (Coudeyras et al. 2008a, b).
The strain L. rhamnosus GR-1 causes significant killing of E. coli in vitro and is able to cause bacterial death in BV biofilms in vitro (McMillan et al. 2011). The two strains L. rhamnosus GR-1 and L. reuteri RC-14 (formerly L. fermentum), which are traded in a vaginal tablet, inhibited in vitro the growth of C. albicans and upregulated inflammatory Interleukin levels in a human vaginal epithelial cell line (Martinez et al. 2009a, b). C. albicans lost it’s metabolic activity, showed increased expression of stress-related genes and lower expression of genes involved in fluconazole resistance (Köhler et al. 2012). Similar results were demonstrated by Sanchez et al. (2008) with a different strain, L. rhamnosus GG, which showed in a monolayer cell culture protection against damage by C. albicans, modulation of immune responses and immune conditioning of the mucosal surfaces (Schaller 2012). Probiotics, here administered as a daily probiotic drink for 6 months, can also enhance the clearance of human papillomavirus-related cervical lesions significantly against placebo (Verhoeven et al. 2013).
Clinical studies had been performed with different probiotics administered vaginally or orally. L. crispatus CTV-05 is one of the new probiotics in gynecology and well tolerated (Hemmerling et al. 2010). Vaginal intercourse (seminal fluid), and the presence of lactobacilli of the same species during vaginal administration inhibit the colonisation (Antonio et al. 2009). There seems to be a competition of one’s own and the foreign lactobacilli.
Oral administration of lactobacilli to influence the vaginal microbiota seems to be effective. The first to demonstrate this were Hilton et al. (1992) against Candida vaginitis and Shalev et al. (1996) against Candida and/or BV. Rectal lactobacilli with vaginal tropism can colonise the vagina and vice versa. Oral application of a mixture of 108 L. fermentum 57A, L. plantarum 57B and L. gasseri 57C daily for 60 days was able to colonise the rectum and the vagina between day 20 and 70 and decreased the vaginal pH, while the Nugent score improved (Strus et al. 2012). The oral administration of L. rhamnosus GR-1 and L. reuteri RC-14 for 30 days following treatment of BV with oral metronidazole improved the cure rate (Anukam et al. 2006). Furthermore, Bohbot and Cardot (2012) showed in a pilot study, that oral administration of L. rhamnosus Lcr35 is able to improve the Nugent score to normal values.
In addition to the improvement of BV symptoms the recurrences of vulvovaginal candidosis can be influenced by probiotics (Homayouni et al. 2014, Huang et al. 2013). Ehrström et al. (2010) showed improved treatment rates for women with BV and vulvovaginal candidosis by additional administration of L. gasseri LN40, L. fermentum LN99, L. casei subsp. rhamnosus LN113 and P. acidilactici LN23 for 5 days in vaginal capsules. Martinez et al. (2009a, b) improved the clinical treatment results of vulvovaginal candidosis with oral fluconazole, L. rhamnosus GR-1 and L. reuteri RC-14 similar to Kern et al. (2012).
Prebiotics, such as inulin, glycogen, or others, which support the metabolism of probiotics are sometimes added to probiotic tablets. However, within the field of gyneacolgy hitherto clinical studies to assess their superiority over probiotics are missing.
6.5 Summary and Conclusion
The normal and the abnormal vaginal microbiota is not yet fully understood. It is an ecosystem, which is influenced by genetic, ethnic, environmental and behavioral factors. More than 100 to 200 bacterial species, commensal, transient and endogenous, colonise the vagina and are influenced by the oral, rectal and penile microbiota. Cultural methods for the determination of normal or abnormal microbiota are insufficient and detect only a small, mostly aerobic, not representative and clinically unimportant spectrum. Lactobacilli mainly dominate the vaginal microbiota and are responsible, with other bacterial species, for the creation of a pH value between 3.8 and 4.5, which is considered as normal, at least in caucasian or asian women. Together with their antibacterial properties and immunological factors lactobacilli create a defense system against dysbiosis and infections within the vagina. This system is responsible for a healthy outer and inner genital tract, for a balanced restitution after intercourse and for a normal pregnancy and childbirth on time.
References
Abdo CL, Safdar N (2009) The role of Lactobacillus probiotics in the treatment or prevention of urogenital infections – a systematic review. J Chemother 21:243–252
Adams MR (1999) Safety of industrial lactic acid bacteria. J Biotechnol 68:171–178
af Heurlin M (1914) Bakteriologische Untersuchungen des Genitalsekretes. Karger, Berlin
Amsel R, Totten PA, Spiegel CA, Chen KCS, Eschenbach DA (1983) Non specific vaginitis. Diagnostic criteria and microbial and epidemiologic associations. Am J Med 74:14–22
Antonio MA, Meyn LA, Murray PJ, Busse B, Hillier SL (2009) Vaginal colonization by probiotic Lactobacillus crispatus CTV-05 is decreased by sexual activity and endogenous Lactobacilli. J Infect Dis 199:1506–1513
Anukam K, Osazuwa E, Ahonkhai I, Ngwu M, Osemene G, Bruce AW, Reid G (2006) Augmentation of antimicrobial metronidazole therapy of bacterial vaginosis with oral probiotic Lactobacillus rhamnosus GR-1 and Lactobacillus reuteri RC-14: randomized, double-blind, placebo-controlled trial. Microbes Infect 8:1450–1454
Babula O, Lazdana G, Kroica J, Ledger WJ, Witkin SS (2003) Relation between recurrent vulvovaginal candidiasis, vaginal concentrations of mannose-binding lectin, and mannose-binding lectin gene polymorphism in Latvian women. Clin Infect Dis 37:733–737
Barrons R, Tassone D (2008) Use of Lactobacillus probiotics for bacterial genitourinary infections in women: a review. Clin Ther 30:453–468
Barton PT, Gerber S, Skupsky DW, Witkin SS (2003) Interleukin-1 receptor antagonist gene polymorphism, vaginal interleukin-1 receptor antagonist concentrations, and vaginal Ureaplasma urealyticum colonization in pregnant women. Infect Immun 71:271–274
Bohbot JM, Cardot JM (2012) Vaginal impact of the oral administration of total freeze-dried culture of LCR-35 in healthy women. Infect Dis Obstet Gynecol 2012: 503648
Cherpes TL, Hillier SL, Meyn LA, Busch JL, Krohn MA (2008) A delicate balance: risk factors for acquisition of bacterial vaginosis include sexual activity, absence of hydrogen peroxide-producing lactobacilli, black race, and positive herpes simplex virus type 2 serology. Sex Transm Dis 35:78–83
Cibley LJ, Cibley LJ (1991) Cytolytic vaginosis. Am J Obstet Gynecol 165:1245–1249
Coudeyras S, Marchandin H, Fajon C, Forestier C (2008a) Taxonomic and strain – specific identification oft he probiotic strain Lactobacillus rhamnosus 35 within the Lactobacillus casei group. Appl Environ Microbiol 74:2679–2689
Coudeyras S, Jugie G, Vermerie M, Forestier C (2008b) Adhesion of human probiotic Lactobacillus rhamnosus to cervical and vaginal cells and interaction with vaginosis-associated pathogens. Infect Dis Obstet Gynecol. doi:10.1155/2008/549640
Curtis AH (1913) A motile curved anaerobic bacillus in uterine discharges. J Infect Dis 13:165–169
de Vos WM, Engstrand L, Drago L, Reid G, Schauber J, Hay R, Mendling W, Schaller M, Spiller R, Gahan CG, Rowland I (2012) Human microbiota in health and disease. Self Care 3(S1):1–68
Demirezen S (2003) Cytolytic vaginosis: examination of 2947 vaginal smears. Cent Eur J Public Health 11:23–24
Döderlein A (1892) Das Scheidensekret und seine Bedeutung für das Puerperalfieber. Besold, Leipzig
Donders GG, Vereecken A, Bosmans E, Dekeersmaecker A, Salambier G, Spitz B (2002) Definition of a type of abnormal vaginal flora that is distinct from bacterial vaginosis: aerobic vaginitis. BJOG 109:34–43
Donders G, Bellen G, Rezeberga D (2011) Aerobic vaginitis in pregnancy. BJOG 118:1163–1170
Edwards L (2010) Dermatologic causes of vaginitis: a clinical review. Dermatol Clin 28:727–735
Ehrström S, Daroczy K, Rylander E, Samuelsson C, Johannesson U, anzén B, Pahlson C (2010) Lactic acid bacteria colonization and clinical outcome after probiotic supplementation in conventionally treated bacterial vaginosis and vulvovaginal candidosis. Microbes Infect 12:691–699
Eschenbach DA, Davick PR, Williams BC, Klebanoff SJ, Young-Smith K, Critchlow CM, Holmes KK (1989) Prevalence of hydrogen peroxid-producing Lactobacillus species in normal women and women with bacterial vaginosis. J Clin Microbiol 27:251–256
Falsen E, Pascual C, Sjoden B, Ohlen M, Collins MD (1999) Phenotypic and phylogenetic characterization of a novel Lactobacillus species from human sources: description of Lactobacillus iners sp. nov. Int J Syst Bacteriol 49:217–221
Fan A, Yue Y, Geng N, Zhang H, Wang Y, Xue F (2013) Aerobic vaginitis and mixed infections: comparison of clinical and laboratory findings. Arch Gynecol Obstet 287:329–335
Fettweis JM, Serrano MG, Girerd PH, Jefferson PH, Buck GA (2012) A new era oft he vaginal microbiome: advances using next-generation sequencing. Chem Biodivers 9:965–976
Fredricks DM, Fiedler TL, Marazzo JM (2005) Molecular identification of bacteria associated with bacterial vaginosis. N Engl J Med 353:1899–1910
Gajer P, Brotman RM, Bai G, Sakamoto J, Schütte UME, Zhong X, Koenig SSK, Li F, Ma Z, Zhou X, Abdo Z, Forney LJ, Ravel J (2012) Temporal dynamics of the human vaginal microbiota. Sci Transl Med 4:132ra52. doi:10.1126/scitranslatmed.3003605
Gardner HL, Dukes CD (1955) Haemophilus vaginals vaginitis – a newly defined specific infection previously classified “non-specific” vaginitis. Am J Obstet Gynecol 69:962–976
Genc MR, Onderdonk A (2011) Endogenous bacterial flora in pregnant women and the influence of maternal genetic variation. BJOG 118:154–163
Gray RH, Kigozi G, Serwadda D, Makumbi F, Nalugoda F, Watya S, Moulton L, Chen MZ, Sewankambo NK, Kiwanuka N, Sempijja V, Lutalo T, Kagayi J, Wabwire-Mangen F, Ridzon R, Bacon M, Wawer MJ (2009) The effects of male circumcision on female partner’s genital tract symptoms and vaginal infections in a randomized trial in Rakai, Uganda. Am J Obstet Gynecol 200:42e1–42e7
Greenwood JR, Pickett MJ (1980) Transfer of Haemophilus vaginalis Gaedner and Dukes to a new genus, Gardnerella: G. vaginalis (Gardner and Dukes) comb. nov. Int J Syst Bacteriol 30:170–178
Guédou FA, van Damme L, Deese J, Crucitti T, Becker M, Mirembe F, Solomon S, Alary M (2013) Behavioural and medical predictors of bacterial vaginosis recurrence among female sex workers: longitudinal analysis from a randomized controlled trial. BMC Infect Dis 13:208. doi:10.1186/1471-2334-13-208
Hemmerling A, Harrison W, Schroeder A, Park J, Korn A, Shiboski S, Foster-Rosales A, Cohen CR (2010) Phase 2a study assessing colonization efficiency, safety, and acceptability of Lactobacillus crispatus CTV-05 in women with bacterial vaginosis. Sex Transm Dis 37:745–750
Hickley RJ, Zhou X, Pierson JD, Ravel J, Forney LJ (2012) Understanding vaginal microbiome complexity from an ecological perspective. Transl Res 160:267–282
Hillier SL, Meyn L, Macio I, Antonio M, Rabe L (2010) The back door reservoir for Lactobacilli and risk of BV (bacterial vaginosis) acquisition. Infect Dis Soc Obstet Gynecol. In: Proceedings of the 37th Annual Scientific Meeting, August 5, Santa Fe, New Mexico
Hilton E, Isenberg HD, Alperstein P, France K, Borenstein M (1992) Ingestion of yoghurt containing Lactobacillus acidophilus as prophylaxis for candidal vaginitis. Ann Intern Med 116:353–357
Homayouni A, Bastani P, Ziyadi S, Mohammad-Alizadeh-Charandabi S, Ghalibaf M, Mortazavian AM, Mehrabany EV (2014) Effects of probiotics on the recurrence of bacterial vaginosis: a review. J Low Genit Tract Dis 18; 79–86
Horowitz BJ, Mardh PA, Nagy E, Rank EL (1994) Vaginal lactobacillosis. Am J Obstet Gynecol 170:857–861
Hoyme UB, Hübner J (2010) Prevention of preterm birth is possible by vaginal pH screening, early diagnosis of bacterial vaginosis or abnormal vaginal flora and treatment. Gynecol Obstet Invest 70:286–290
Huang H, Song L, Zhao W (2013) Effects of probiotics for bacterial vaginosis in adult women: a meta-analysis of randomized clinical trials. Arch Gynecol Obstet 289: 1225–1234
Jahic M, Mulavdic M, Hadzimehmedovic A, Jahic E (2013) Association between aerobic vaginitis, bacterial vaginosis and squamous intraepithelial lesion of low grade. Med Arh 67:94–96
Jayaprakash TP, Schellenberg JJ, Hill JE (2012) Resolution and character-ization of distinct cpn60-based subgroups of gardnerella vaginalis in the vaginal microbiota. PLoS One 7(8):e43009. doi:10.1371/journal.pone.0043009
Jespers V, Menten J, Smet H, Poradosú S, Abdellati S, Verhelst R, Hardy L, Buvé A, Crucitti T (2012) Quantification of bacterial species of the vaginal microbiome in different groups of women, using nucleid acid amplification tests. BMC Microbiol 12:83
Jirovec O, Peter R, Malek J (1948) Neue Klassifikation der Vaginalbiocoenose auf sechs Grundbildern. Gynaecologia (Basel) 126:77
Kern AM, Bohbot JM, Cardot JM (2012) Traitement préventive de la candidose vulvovaginale récidivante par probiotique vaginal: résultats de l’étude observationelle Candiflore. Lett Gynécol 370:34–37
Köhler GA, Assefa S, Reid G (2012) Probiotic interference of Lactobacillus rhamnosus GR-1 and Lactobacillus reuteri RC-14 with the opportunistic fungal pathogen Candida albicans. Infect Dis Obstet Gynecol 2012:636474. doi:10.1155/2012/636474
Krönig B (1895) Über die Natur der Scheidenkeime, speciell über das Vorkommen anaerober Streptokokken im scheidensekret Schwangerer. Centrbl Gynäkol 16:409–412
Lamont RF, Sobel JD, Akins RA, Hassan SS, Chaiworapongsa T, Kusanovic JP, Romero R (2011) The vaginal microbiome: new information about the genital tract flora using molecular based techniques. BJOG 118:533–549
Li J, McCormick J, Bocking A, Reid G (2012) Importance of vaginal microbes in reproductive health. Reprod Sci 19:235–242
Linhares IM, Giraldo PC, Baracat EC (2010) New findings about vaginal bacterial flora. Rev Assoc Med Bras 56: doi 10.1590/S0104-4230210000300026
Machado A, Jefferson KK, Cerca N (2013) Interactions between Lactobacillus crispatus and bacterial vaginosis (BV)-associated bacterial species in initial attachment and biofilm formation. Int J Mol Sci 14:12004–12012
Manhart MC, Fiedler TK, Fredricks DN, Marrazzo J (2012) Behavioral predictors of colonization with Lactobacillus crispatus or Lactobacillus jensenii after treatment for bacterial vaginosis: a cohort study. Infect Dis Obstet Gynecol 2012:706540. doi:10.1155/1012/706540. Epub 2012 May 30
Marrazzo JM, Fiedler TL, Srinivasan S, Thomas KK, Liu C, Ko D, Xie H, Saracino M, Fredricks DN (2012) Extravaginal reservoirs of vaginal bacteria as risk factors for incident bacterial vaginosis. J Infect Dis 205:1580–1588
Martin DH (2012) The microbiota of the vagina and its influence on women’s health and disease. Am J Med Sci 343:2–9
Martin R, Langa S, Reviriego C, Jiminez E, Marin M, Xaus J, Fernandez L, Rodriguez J (2003) Human milk as a source of lactic acid bacteria for the infant gut. J Pediatr 143:754–758
Martinez RC, Seney SL, Summers KL, Nomizo A, de Martinis EC, Reid G (2009a) Effect of Lactobacillus rhamnosus GR-1 and Lactobacillus reuteri RC-14 on the ability of Candida albicans to infect cells and induce inflammation. Microbiol Immunol 53:487–495
Martinez RCR, Franceschini SA, Patta MC, Quintana SM, Candido RC, Ferrera JC, de Martinis ECP, Reid G (2009b) Improved treatment of vulvovaginal candidiasis with fluconazole plus probiotic Lactobacillus rhamnosus GR-1 and Lactobacillus reuteri RC-14. Lett Appl Microbiol 48:269–274
McMillan A, Dell M, Zellar MP, Cribby S, Martz S, Hong E, Abbas A, Dang T, Miller W, Reid G (2011) Disruption of urogenital biofilms by lactobacilli. Colloids Surf B Biointerfaces 86:58–64
Mendling W, Martius J, Hoyme UB (2013) S1 – guideline on bacterial vaginosis in gynecology and obstetrics. Geburtshilfe Frauenheilkd 73:1–4
Mirmonsef P, Gelbert D, Zariffard MR, Hamaker BR, Kaur A, Landay AL, Spear GT (2011) The effects of commensal bacteria on innate immune responses in the female genital tract. Am J Reprod Immunol 65:190–195
Mitchell C, Gottsch ML, Liu C, Fredricks DN, Nelson DB (2013) Association between vaginal bacteria and levels of vaginal defensins in pregnant women. Am J Obstet Gynecol 208:132.e1–132.e7
Nivoliez A, Camarez o, Paquet-Gachinat M, Bornes S (2012) Influence of manufacturing processes on in vitro properties of the probiotic strain Lactobacillus rhamnosus Lcr35. J Biotechnol 160:236–241
Nugent RP, Krohn MA, Hillier SL (1991) Reliability of diagnosing bacterial vaginosis is improved by a standardized method of gram stain interpretation. J Clin Pathol 29:297–300
Nürnberger L (1930) Die Erkrankungen der Scheide. In: Stoeckel (ed) Handbuch der Gynäkologie, revised 3rd edition of Handbuch der Gynäkologie by Veit J, vol 5. Bergmann, Munich
Petricevic L, Witt A (2008) The role of Lactobacillus casei rhamnosus Lcr35 in restoring the normal vaginal flora after antibiotic treatment of bacterial vaginosis. BJOG 115:1369–1374
Petricevic L, Unger FM, Viernstein Kiss H (2008) Randomized, double-blind, placebo-controlled study of oral lactobacilli to improve the vaginal flora of postmenopausal women. Eur J Obstet Gynecol Reprod Biol 141:54–57
Petricevic L, Domig KJ, Nierscher FJ, Krondorfer I, Janitschek C, Kneifel W, Kiss H (2012) Characterisation oft he oral, vaginal and rectal Lactobacillus flora in healthy pregnant and postmenopausal women. Eur J Obstet Gynecol Reprod Biol 160:93–99
Pirotta M, Gunn J, Chondros P, Grover S, O’Malley P, Hurley S, Garland S (2004) Effect of lactobacillus in preventing post-antibiotic vulvovaginal candidiasis: a randomised controlled trial. BMJ 329:458–51
Price LB, Liu CM, Johnson KE, Aziz M, Lau MK, Bowers J, Ravel J, Keim PS, Serwadda D, Wawer MJ, Gray RH (2010) The effects of circumcision on the penis microbiome. PLoS One 5:e8422
Ravel J, Gajer P, Abdo Z, Schneider GM, Koenig SSK, McCulle SL, Karlebach S, Gorle R, Russell J, Tacket CO, Brotman RM, Davis CC, Ault K, Peralta L, Forney LJ (2011) Vaginal microbiome of reproductive-age women. Proc Natl Acad Sci U S A 108(S1):4680–4687
Reid G (2001) Probiotic agents to protect the urogenital tract against infection. Am J Clin Nutr 73(Suppl):S437–S443
Reid G (2012) Probiotic and prebiotic applications for vaginal health. J AOAC Int 95:31–34
Rodriguez JM, Collins MD, Sjoden B, Falsen E (1999) Characterization of a novel Atopobium isolate from the human vagina: description of Atopobium vaginae sp. nov. Int J Syst Bacteriol 49:1573–1576
Sanchez D, Wagener J, Schaller M (2008) Impact of Lactobacillus species on localised Candida albicans infection and the mucosal innate immune response. Mycoses 51:434
Sanu O, Lamont RF (2011) Periodontal disease and bacterial vaginosis as genetic and environmental markers for the risk of spontaneous preterm labor and preterm birth. J Matern-Fetal Neonatal Med 24:1476–1485
Schaller M (2012) Lactobacilli in mucosal Candida albicans infections. In: de Vos WM, Engstrand L, Drago L, Reid G, Schauber J, Hay R, Mendling W, Schaller M, Spiller R, Gahan CG, Rowland I (eds) Human microbiota in health and disease. SelfCare 3(S1):S41–S45
Schröder R (1921) Zur Pathogenese und Klinik des vaginalen Fluors. Zbl Gynäkol 38:1350–1361
Senok AC, Verstraelen H, Temmerman M, Botta GA (2009) Probiotics for the treatment of bacterial vaginosis. Cochrane Database Syst Rev 7(4):CD006289
Shalev E, Battino S, Weiner E, Colodner R, Keness Y (1996) Ingestion of yogurt containing Lactobacillus acidophilus compared with pasteurized yogurt as prophylaxis for recurrent candidal vaginitis and bacterial vaginosis. Arch Fam Med 5:593–596
Sherman P, Ossa JC, Johnson-Henry K (2009) Unraveling mechanisms of action of probiotics. Nutr Clin Pract 24:10–14
Spiegel CA, Roberts M (1984) Mobiluncus gen. nov. Mobiluncus curtisii subsp. curtisii sp. nov., Mobiluncus curtisii subsp. holmesi subsp. nov., and Mobiluncus mulieris sp. nov., curved rods from the human vagina. Int Syst Bacteriol 34:177–184
Spurbeck RR, Arvidson CG (2011) Lactobacilli at the front line of defense against vaginally acquired infections. Future Microbiol 6:567–582
Strus M, Chmielarczyk A, Kochan P, Adamski P, Chelmicki Z, Chelmicki A, Palucha A, Heczko P (2012) Studies on the effect of probiotic Lactobacillus mixture given orally on vaginal and rectal colonization and on parameters of vaginal health in women with intermediate vaginal flora. Eur J Obstet Gynecol Reprod Biol 163:210–215
Swidsinski A, Mendling W, Loening-Baucke V, Ladhoff A, Swidsinski S, Hale LP, Lochs H (2005) Adherent biofilms in bacterial vaginosis. Obstet Gynecol 106:1013–1023
Swidsinski A, Mendling W, Loening-Baucke E, Swidsinki S, Dörfel Y, Scholze J, Lochs H, Verstraelen H (2008) An adherent Gardnerella vaginalis biofilm persists on the vaginal epithelium following standard therapy of bacterial vaginosis with oral metronidazole. Am J Obstet Gynecol 198:97e1–97e6
Swidsinski A, Dörffel Y, Loening-Baucke V, Mendling W, Schilling J, Patterson JL, Verstraelen H (2010) Dissimilarity in the occurrence of Bifidobacteriaceae in the vaginal and peranal microbiota in women with bacterial vaginosis. Anaerobe 16:478–482
Swidsinski A, Loening-Baucke V, Mendling W, Dörffel Y, Schilling J, Halwani Z, Jiang XF, Verstraelen H, Swidsinski S (2013) Infection through structured polymicrobial Gardnerella biofilms (StPM-GB). Histol Histopathol 29:567–597
Thies FL, König W, König B (2007) Rapid characterization of the normal and disturbed vaginal microbiota by application of 16S rRNA gene terminal RFLP fingerprinting. J Med Microbiol 56:755–761
Thomas S (1928) Döderlein’s bacillus: Lactobacillus acidophilus. J Infect Dis 43:218–227
Vasquez A, Jakobsson T, Ahrné S, Forsum U, Maey olin G (2002) Vaginal Lactobacillus flora of healthy Swedish women. J Clin Microbiol 40:2746–2749
Verhelst R, Verstraelen H, Claeys G, Verschraegen G, Delanghe J, van Simaey L, de Ganck C, Temmermann M, Vaneechoutte M (2004) Cloning of 16S rRNA genes amplified from normal and disturbed vaginal microflora suggests a strong association between Atopobium vaginae, Gardnerella vaginalis and bacterial vaginosis. BMC Microbiol 4:16
Verhoeven V, renard N, Makar A, van Royen P, Bogers JP, Lardon F, Peeters M, Baay M (2013) Probiotics enhance the clearance of human papillomavirus-related cervical lesions: a prospective controlled pilot study. Eur J Cancer Prev 22:46–51
Verstaelen H, Verhelst R, Nuytinck L, Roelens K, de Meester E, de Vos D, van Thielen M, Rossau R, Delva W, de Bakker E, Vaneechoutte M, Temmermann M (2009) Gene polymorphisms of Toll-like and related recognition receptors in relation to the vaginal carriage of G.vaginalis and A. vaginae. J Reprod Immunol 79:163–173
Verstraelen H, Swidsinski A (2013) The biofilm in bacterial vaginosis: implications for epidemiology, diagnosis and treatment. Curr Opin Infect Dis 26:86–89
Verstraelen H, Verhelst R, Claeys G, de Bakker E, Temmermann M, Vaneechoutte M (2009) Longitudinal analysis of the vaginal microflora in pregnancy suggests that L. crispatus promotes stability of the normal vaginal microflora and that L. gasseri and/or L. iners are more conducive to the occurrence of abnormal vaginal microflora. BMC Microbiol 9:116. doi:10.1186/1471-2180-9-116
Weström L (Working Group Co-ordinator), Evaldson G, Holmes KK, van der Meijden W, Rylander E, Fredriksson B (1984) Taxonomy of bacterial vaginosis; bacterial vaginosis – a definition. Symposium on bacterial vaginosis, Stockholm, Jan. 1984. In: Mardh PA, Taylor-Robinson D (eds) Bacterial vaginosis. Almquist & Wiksell, Stockholm, pp 259–260
Ya W, Reifer C, Miller LE (2010) Efficacy of vaginal probiotic capsules for recurrent bacterial vaginosis: a double-blind, randomized, placebo-controlled study. Am J Obstet Gynecol 203:120.e1–120.e6
Zhou X, Bent SJ, Schneider MG, Davis CC, Islam MR, Forney LJ (2004) Characterization of vaginal microbial communities in adult healthy women using cultivation-independent methods. Microbiology 150:2565–2573
Zhou X, Hansmann MA, Davis CC, Siuzuki H, Brown CJ, Schütte U, Pierson JD, Forney LJ (2010) The vaginal bacterial communities of Japanese women resemble those of women in other racial groups. FEMS Immunol Med Microbiol 58:169–181
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Mendling, W. (2016). Vaginal Microbiota. In: Schwiertz, A. (eds) Microbiota of the Human Body. Advances in Experimental Medicine and Biology, vol 902. Springer, Cham. https://doi.org/10.1007/978-3-319-31248-4_6
Download citation
DOI: https://doi.org/10.1007/978-3-319-31248-4_6
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-31246-0
Online ISBN: 978-3-319-31248-4
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)