Abstract
Patients treated for pain with controlled substances are at risk for adverse outcomes that include misuse, abuse, addiction, unintentional drug poisoning, and illegal diversion. Therapeutic success and compliance with medicolegal requirements necessitate risk mitigation strategies at treatment initiation and on an ongoing basis. Urine drug testing, checks of the state prescription-monitoring program, pill counts, and abuse-deterrent opioid formulations have a place in a comprehensive clinical pain management strategy. Rotation to a different opioid may be beneficial but requires caution. Risk management with controlled substance therapy is essential for reducing healthcare costs and improving patient outcomes.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Controlled substances
- Pain
- Pain management
- Opioid analgesics
- Therapeutic use
- Universal precautions
- Risk management
- Opioid-related disorder
- Adherence monitoring
- Abuse deterrence
- Urine drug testing
Introduction
Controlled substances, including opioid analgesics, have a legitimate, recognized place in chronic pain management but are associated with significant risks to patients and society stemming from misuse, abuse, diversion, addiction, and overdose deaths. The health and societal consequences of opioid misuse and abuse are severe. Prescription opioids contribute to more than 16,000 drug-poisoning deaths per year [1]. Approximately 4.5 million Americans are current nonmedical users of opioids [2]. By one estimate, the economic costs of nonmedical opioid use reach $53.4 billion a year in lost productivity, criminal justice costs, drug abuse treatment, and medical complications [3], and the personal damage done to individuals and families is incalculable.
Opioids, though clearly potentially harmful, do reduce pain and restore functionality for some patients who suffer from severe, chronic pain that is unresponsive to alternative pharmacologic or nonpharmacologic therapies. Long-term effectiveness data are sparse but indicate a subset of patients benefit from opioid analgesics [4], and that periodic monitoring using clinical tools to reduce opioid misuse and abuse can improve patient outcomes and reduce costs [5–7].
This chapter discusses risk mitigation tools to track the clinical effect and patient adherence to medical direction in the use of therapeutic opioids and other controlled substances for pain. Aside from opioids, commonly prescribed medications in pain management include agents to treat depression, anxiety, sleep, and other psychiatric and medical comorbidities that frequently co-occur with pain. Newer abuse-deterrent opioid formulations are discussed, and clinical strategies in opioid rotation are presented to maximize analgesia and minimize risk.
To aid clarity, this manuscript adheres to definitions of misuse and abuse reached by an expert panel as follows: Misuse is “use of a medication (for a medical purpose) other than as directed or indicated, whether willful or unintentional, and whether harm results or not [8].” Abuse is considered “any use of an illegal drug or the intentional self-administration of a medication for a nonmedical purpose such as altering one’s state of consciousness, for example, getting high [8].”
The Essentials of Risk Mitigation
An essential step for clinical and medicolegal reasons is to diligently document risk mitigation strategies in the patient record. Good documentation practices help ensure timely and appropriate medical attention to any issues that arise and demonstrate to regulatory and law-enforcement authorities that prescribing is for a legitimate medical purpose within the usual course of professional medical practice [9].
Managing risk first entails careful assessment and risk stratification. Patients may be screened for degree of risk and triaged to determine the intensity, frequency, and type of risk mitigation strategies to follow. A strategy devised by Gourlay et al. [10] stratifies patients into three treatment groups:
-
Group I contains patients without personal or family history of substance abuse and without major or untreated psychiatric or psychological disorder.
-
Patients in Group II do not display active addiction but are at risk due to history of treated substance abuse, significant family history of substance abuse, past or comorbid psychiatric or psychological disorder, or some combination; they should be comanaged with the help of a specialist in pain, substance abuse, mental health, or some combination as appropriate.
-
Patients in Group III are the most difficult to manage because of their active substance abuse or addiction or major untreated psychiatric or psychological disorder(s). Stringent follow-up or an opioid exit strategy should apply as appropriate. Recent data indicate recently released prisoners belong in this category [11].
Patients may be assessed using tools specifically formulated for opioid-treated patients, such as the Opioid Risk Tool (see Appendix C) [12] and the revised 24-item Screener and Opioid Assessment for Patients with Pain (SOAPP-R) (see Appendix D) [13]. These and additional available tools are not diagnostic of addiction nor are they intended to pinpoint whether a patient should be discharged from opioid therapy; rather, they assess the risk for aberrant drug-related behaviors by the patient, based on biological, social, and psychiatric risk factors, and are administered prior to beginning opioid therapy. Risk factors from the scientific literature include but are not limited to the following: [12–17]:
-
Nonfunctional status due to pain;
-
Exaggeration of pain;
-
Unclear etiology for pain;
-
Young age;
-
Smoking;
-
Poor social support;
-
Personal history of substance abuse;
-
Family history of substance abuse;
-
Psychological stress;
-
Psychological disease;
-
Focus on opioids;
-
Preadolescent sexual abuse.
Patients may not be honest when answering questions related to opioid abuse risk. Whether or not a formal tool is used, prescribers should be aware of risk factors and implement a clinical plan to assess patients based on them. Patients are monitored at a level in accordance with risk (Table 10.1) [18, 19]. However, patients may change risk categories over the course of treatment and require closer monitoring due to stress, increased pain, disease progression, social and familial difficulties, the onset or worsening of mental disease, and other factors. The toll chronic pain takes on family and social relationships, work, finances, and frequent struggles to obtain health insurance coverage significantly heighten stress and threaten adherence to the medication regimen. Tools are also available to assist with frequent reassessment and documentation to include the effects of opioid therapy on analgesia, daily activities, adverse effects, aberrant drug-related behaviors, cognition, and quality of life [20, 21].
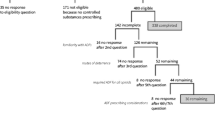
Types of medication misuse and abuse occur in patients and nonpatients, and motivations manifest along a spectrum (Fig. 10.1) [22]. Reasons for patient medication misuse or abuse vary widely and include the following [23]:
-
Misunderstanding between the patient and provider;
-
Unauthorized self medication of pain, mood, or sleep problems;
-
Desire to avoid symptoms of abstinence syndrome;
-
Desire for euphoria or other psychoactive reward;
-
Compulsive use due to addiction;
-
Illegal diversion for financial gain.
Spectrum of medication misuse in nonmedical users and pain patients. SUD substance-use disorder. From Kirsh and Passik [22]
Consider also that clinical manifestations of opioid-related substance abuse are more likely in a scenario of familial or social substance abuse. Talking about the issues with patients is critical. The physician can facilitate patient honesty by treating adherence to medical direction with opioid therapy as routine and by using an empathic rather than confrontational approach.
Although there is value in recognizing that patients do differ in their risk for medication misuse or abuse, clinicians should also meet a minimum threshold of risk mitigation for every patient who receives treatment with opioids or other controlled substances for pain. Subjective evaluation of patient adherence is best when used in combination with objective measures. Because aberrant drug-related behaviors such as escalating doses or requesting early refills may be difficult to interpret, and consensus is lacking as to which types and frequencies of behaviors demand clinical action, quantifiable measures increase clinician control. Clinicians should track the effect of the therapeutic regimen on the patient’s pain levels and functional, psychological, and social health throughout the course of therapy.
The discontinuation of opioid therapy may be necessary in some cases. Clinicians should have an exit strategy in place and be prepared to humanely taper patients and either treat or refer for treatment with alternatives to opioid therapy.
Clinical Monitoring Tools
Urine Toxicology
One of the most widely available, useful tools for monitoring adherence to the therapeutic regimen is the urine drug test (UDT) and one that is underutilized [24]. Results of a UDT are used to identify—within limitations—the presence of prescribed medications and the use of undisclosed, unauthorized prescription and illegal drugs. Compared with blood testing, it is less expensive, is less invasive, and has a longer window for detection of substances [25, 26]. In addition to ease of collection, turnaround time is quick and laboratories that provide the testing are accessible.
Urine toxicology is now an expected standard of practice in chronic pain management. As such, the UDT should be presented upfront to patients as a routine, consensual part of medical care, with a full explanation of why it is important.
Potential benefits of UDT include the following:
-
Establishing routine medical practice akin to testing glucose levels in diabetes;
-
Fostering communication between patient and clinician;
-
Helping guide treatment decisions;
-
Identifying early patients with potential substance-use disorders;
-
Increasing safety;
-
Allowing the clinicians to advocate on the patient’s behalf;
-
Discouraging drug misuse or recreational abuse;
-
Heightening the chance for therapeutic success through patient adherence to the treatment regimen.
Two steps in testing are required in most instances: qualitative/presumptive and quantitative/definitive testing [26, 27]. The qualitative immunoassay is radioactive or enzyme mediated and can help quickly establish whether a new patient has recently ingested illegal drugs or other opioid and prescription drugs. It detects certain drug classes but typically cannot isolate specific opioids. If results from the initial, presumptive test are inconsistent with medical direction, a follow-up test is necessary. This second step is a quantitative evaluation, usually via gas chromatography/mass spectrometry (GC/MS) technology or liquid chromatography dual mass spectrometry (LC/MS/MS). These tests are more specific than immunoassay and can detect actual molecular structures of specific drugs. Although immunoassay followed by definitive testing historically has been the standard, some laboratories have begun to offer definitive testing via LC/MS/MS that can identify more drugs than conventional immunoassays and that may be given as the initial test [27].
The temperature of the sample should be measured at the point of collection. Laboratories can test for specific gravity. Both measures guard against tampering with the sample [19, 26].
Testing in a clinical setting with its emphasis on scientific data collection to inform medical decisions is different from that performed in forensic or workplace settings. Laboratories for definitive testing should be carefully selected and informed of pain management goals. Cutoff points for the detection of drugs during definitive testing vary, and clinicians should discuss clinically relevant cutoff points with personnel at the laboratory that is to perform the testing. Discuss, also, with laboratory personnel the importance of the presence or absence of the prescribed drug, which is equal in importance to the presence of unauthorized substances for mitigating abuse or diversion.
Drugs to test include illicit drugs, commonly prescribed opioids (i.e., morphine, hydrocodone, hydromorphone, oxycodone, oxymorphone, fentanyl, and buprenorphine), benzodiazepines, barbiturates, carisoprodol, tramadol, selective serotonin reuptake inhibitors, serotonin–norepinephrine reuptake inhibitors, anxiolytics, sleep medications, and other substances as necessary [19].
Best practices regarding the frequency of UDT in pain management are evolving and may vary by state. Clinical guidelines suggest a baseline UDT for every patient to be prescribed opioids or other controlled substances long term (in general, >3 months) to be followed by periodic tests in alliance with the patient’s risk category or clinical signs of opioid misuse or abuse (Table 10.1) [18, 19, 28, 29]. A recent guideline from Peppin and colleagues recommends the possibility of periodic, random testing for every patient at every visit [19]. For patients at low risk, the same guideline recommends testing at least every 6 months and, if an immunoassay test is used, testing at least 1 time a year with GC/MS or LC/MS/MS. For moderate-to-high-risk patients, the recommendation is an immunoassay test every 3 months at minimum and definitive testing every 6 months. However, bear in mind, if a patient’s risk is quite high or if problematic behaviors or clinical signs need to be addressed, a test during every clinic visit may be more appropriate.
Risk category should guide, to some extent, how often a patient is tested. However, it is not possible to identify beyond doubt who is adherent to medical direction and who is not. Therefore, every patient prescribed controlled substances is presumed to be at some risk and is thus subject to risk mitigation measures in line with universal precautions, which is modeled on the infectious disease paradigm [10].
The clinician must appreciate certain limitations of the UDT, caused by variables such as individual patient and drug metabolism and test unreliability. False positives (when a drug is absent though the test indicates it is present) and false negatives (when a drug is actually present though the test result says it is not) are possible, though far more common with immunoassay testing than with LC/MS/MS quantitative laboratory testing [30].
Some common causes of inaccurate UDT results are listed below.
Cross-reactivity with certain foods, over-the-counter (OTC) medications, and prescribed drugs may cause false positives (Table 10.2) [26]. It is important to know all prescribed and OTC medications a patient is taking and to inform the laboratory that will perform the testing.
Windows of detection are limited to 2–3 days after exposure for most substances [31], meaning a patient who misunderstands dosing directions or who metabolizes opioids faster than is typical due to genetic factors may have a false result.
Laboratory error or test insensitivity could skew results, particularly with immunoassays, which may not be sensitive enough to detect opioids at therapeutic levels. Follow-up with the laboratory is advised to ensure the personnel are testing the correct substances with the most sensitive test available.
Drug metabolism, as mentioned, varies among patients due to genetic factors [32], and those who are quick metabolizers may falsely appear to have failed to consume a prescribed drug. Pharmacogenetic testing is now available to identify genetic biomarkers that may influence a patient’s response to medication, though it should be noted the clinical relevance of such biomarkers is still unclear with regard to supporting evidence [33].
Metabolites of prescribed drugs and manufacturing impurities may present as unexpected results [18, 34]. For example,
-
Codeine is metabolized to morphine;
-
Morphine is not metabolized to codeine, but small amounts of codeine may be a manufacturing by-product;
-
Codeine is partially metabolized to hydrocodone;
-
Hydrocodone is metabolized to hydromorphone;
-
Morphine can produce the minor metabolite hydromorphone;
-
Heroin is metabolized to 6-monoacetylmorphine (6-MAM) and morphine.
These limitations must be appreciated to help avoid errors in interpretation. One should understand, also, that the absence of a prescribed drug does not, in itself, prove hoarding or illegal diversion. Unexpected results should trigger a clinical discussion with the patient, which is then followed up in the medical record. Clinical decisions should only be made based on the most accurate test method, and all UDT results should be part of a broader risk mitigation strategy.
Prescription Drug-Monitoring Programs
Most states now operate electronic databases containing prescriber and patient data on dispensed prescriptions to enable healthcare, law-enforcement, and regulatory professionals to track clinically harmful or illegal activities involving controlled substances [35]. As of 2012, every state except Missouri either had a prescription drug-monitoring program (PDMP) or had plans to develop one, and systems were operational in 41 states [36]. A primary strength of state PDMPs is to identify quickly those who get opioids or other controlled substances from more than one medical source without authorization [36]. Newer systems offer real-time data and secure online access. The capabilities across states vary widely, however, and how effective the programs are in mitigating harm is still being assessed.
Some evidence indicates PDMPs do mitigate opioid-related harm in the general and treatment-seeking populations. Analysis of two data streams from the RADARS System showed reduced intentional exposures and substance-abuse treatment admissions involving opioids in states with PDMPs compared to states without [35]. The mechanism for the reduction is not completely clear. Another analysis found that states with proactive PDMPs, defined as those that generate unsolicited reports automatically, subsequently reported a reduced supply of prescribed opioids leading indirectly to less being available for misuse, abuse, and diversion [37]. Evidence pertaining to opioid-related mortality has, thus far, not shown a benefit from PDMPs, but additional research is necessary [38].
Discrepancies across state systems do limit the programs’ effectiveness. According to a report funded by the Pew Charitable Trusts [36], this lack of uniformity and other limitations likely contribute to physician reluctance to use the databases. Suggestions in the report for improvements include the following:
-
Increase the ability to share data across state lines;
-
Standardize the data fields and move toward real-time collection;
-
Collect data on all controlled substance schedules and some commonly abused drugs that are not scheduled;
-
Better integrate data into patients’ electronic health records (EHR);
-
Establish criteria for identifying questionable activity;
-
Generate automatic reports to guide prescribing decisions or investigations.
Overall, PDMPs appear to be beneficial and improving in quality, despite the need for further refining and better integration into daily practice. Most experts in the field of pain management and the Federation of State Medical Boards, on which many states base pain management guidelines, concur that PDMPs may help identify “doctor shopping” and provide information that may help make prescribing controlled substances safer for patients [25, 28]. In addition, some states are implementing requirements in regard to the timing and frequency of PDMP checks [39].
A prudent course is to check the state PDMP as follows:
-
For every new patient;
-
Periodically;
-
Whenever medications or dosages are changed;
-
When evidence of nonadherence to the therapeutic regimen occurs;
-
When aberrant drug-related behaviors are observed.
The clinicians may identify harmful patterns of multiple unauthorized prescriptions, potential for drug–drug interactions, and early indications of substance-use disorders in the patient. However, as with UDT, results should be interpreted with caution. Results from a PDMP check are not diagnostic of the disease of addiction, and alternative causes of observed discrepancies are possible. For instance, recent reports indicate that drug shortages and regulatory efforts aimed at reining in illegal diversion of prescription drugs have brought about circumstances in which patients have been forced to visit multiple pharmacies to get legitimately issued prescriptions filled [40].
Pill Counts
Pill (or patch) counts are often recommended, usually in concert with other adherence monitoring strategies [24, 28]. A prospective study of 500 consecutive patients receiving controlled substances documented a 50 % reduction in signs of opioid misuse and abuse associated with adherence monitoring that included pill counts together with UDT and periodic evaluation of the patient [6].
Typically, pill counts are an intensified monitoring measure for patients who are at high risk or who have exhibited a pattern of behaviors that might indicate opioid misuse or abuse, such as frequent early refills, lost medications, or inconsistent UDT results. Pills may be counted on a random basis during regularly scheduled clinic visits, or patients may be called and given a time frame to come to the office with their original pill bottle. These tighter controls typically accompany closer prescribing intervals (e.g., monthly or weekly). A failed test is a no-show or a quantity of medication that is inconsistent with prescribed and expected consumption levels.
Documentation of this practice in the medical record may help demonstrate appropriate medical practice if questions about a clinician’s prescribing practices should later arise with law-enforcement or regulatory authorities. Do note, however, that patients may circumvent the intent of pill counts through borrowing or purchasing medication so as to present the appropriate, expected quantity during the clinic visit. As with other objective risk mitigation measures, pill counts should be understood and implemented as part of an overall clinical strategy, not a single fix.
Abuse-Deterrent Formulations
The pharmaceutical industry is developing newer opioid formulations to maintain analgesia while reducing abuse liability. To date, the US Food and Drug Administration (FDA) has approved four products for labeling consistent with the agency’s draft guidance on the properties required for abuse-deterrent formulations (ADFs) [41]. The agents are as follows: reformulated oxycodone hydrochloride (HCL) extended-release (ER) tablets, oxycodone HCL/naloxone HCL ER tablets, morphine sulfate/naltrexone HCL ER capsules (which were voluntarily recalled because of stability concerns; relaunched in 2015), and hydrocodone bitartrate ER tablets (Table 10.3) [42–47]. All are indicated for the management of pain severe enough to require daily, around-the-clock, long-term opioid treatment and for which alternative treatment options are inadequate.
Additional agents formulated to deter abuse but without abuse-deterrent labeling include the following: hydromorphone HCL ER tablets (EXALGO™), oxycodone HCL/acetaminophen ER tablets (XARTEMIS™ XR), oxycodone HCL tablets (OXECTA™), oxymorphone HCL ER tablets (OPANA® ER), and tapentadol HCL ER tablets (NUCYNTA® ER) [48–52].
Newer formulations work by blocking the physical or chemical manipulations through which a formulation may be improperly accessed and ingested via an unintended route or method. Common methods and routes of opioid abuse include the following:
-
Crushing and swallowing;
-
Crushing and snorting;
-
Crushing and smoking;
-
Crushing and extracting for injection;
-
Swallowing intact;
-
Coingesting with alcohol or benzodiazepines.
The FDA classes the various properties of ADFs as follows [41]:
-
(1)
Physical or chemical barriers to tampering with or altering the opioid product. Physical barriers, such as housing viscous gel, resist chewing, grinding, crushing, or grating; chemical barriers block extraction of active ingredient through dissolving in liquids such as water or alcohol.
-
(2)
Agonist/antagonist combinations in which an agent such as naloxone or naltrexone is designed to remain inert during therapeutic use but is released so as to reverse the opioid effect if the formulation is altered.
-
(3)
Aversive agents such as capsaicin that produce an unpleasant effect if used nontherapeutically.
-
(4)
Delivery systems such as intramuscular depot injections or implants that are difficult to manipulate.
-
(5)
Prodrugs that are activated for analgesic purposes only by the gastrointestinal tract, thus frustrating injection or intranasal routes.
-
(6)
Combinations of the above methods.
Much research aims to deter abuse that is accomplished when long-acting opioid formulations are altered to access for immediate release (IR) an intended ER formulation. This principle of abuse potential associated with a drug is its abuse quotient (AQ), defined as the maximum serum concentration of the drug (Cmax) divided by the time required to reach that maximum level (Tmax) [53]. In general, tampering with ER formulations causes serum Cmax to increase and Tmax to decrease, as when a full dose of oxycodone ER is quickly released. Therefore, the larger the ratio, the greater the potential attractiveness of a drug to would-be abusers. The research focus on ER formulations is supported by the results that suggest that long-acting opioids, such as oxycodone ER, are more frequently abused than are IR, short-acting, and combination opioids once rates are normalized for the number of prescriptions written [54, 55].
People who misuse or abuse opioids may be patients or nonpatients. Patients who misuse opioids (i.e., any unauthorized use) may do so through error or for the medications’ psychoactive effects due to the disease of addiction, to escape physical pain, or to escape emotional or psychological pain. Most patients will misuse or abuse an opioid orally by swallowing whole or chewing. Nonpatients, who divert opioids from legitimate prescribing channels in order to get high or to satisfy a drug craving, may swallow pills whole or chew them; however, this population is probably more likely to crush pills for intranasal or intravenous administration and to have set patterns of abuse based on their drug(s) of choice (Fig. 10.2) [56]. The technology of abuse deterrence is aimed principally at populations that alter the medications in order to abuse them.
Preferred routes of administration by patients entering substance-abuse treatment facilities [Population of individuals seeking substance-abuse treatment who indicated past 30-days abuse of prescription opioids (N = 4807)]. From Budman et al. [56]
Populations vary in their abuse of opioids. Three broad categories with overlapping characteristics are as follows:
-
Novices, experimenters, occasional users, typically but not necessarily young people;
-
Nonaddicted, established users for whom prescription drug abuse is a recurrent activity;
-
More severely substance-use-disordered or addicted users.
It appears ADFs have potential for deterring substance abuse with prescription opioids. The reformulated oxycodone ER developed by Purdue Pharma demonstrated reduced abuse compared with the conventional formulation in the first 20 months post-approval in an epidemiological sample of individuals at high risk for prescription opioid abuse, particularly for methods that involve tampering [57]. However, the science is evolving, and the ultimate impact of ADFs on the societal problem with prescription drug abuse is still uncertain. Another study demonstrated changes in oxycodone and heroin use after introduction of reformulated oxycodone [58]. The reformulated oxycodone showed a 36 % decrease in abuse exposures in two years after introduction with a 59 % decrease with 80 mg tablets. There was concomitant 20 % increase in abuse exposure with the original formulation of oxycodone ER and a 21 % increase in heroin exposure. Dart et al. [59] showed a concomitant increase in heroin use and decrease in reformulated oxycodone use via the RADARS System and from poison centers and substance-abuse treatment centers. Similarly, Cicero et al. [60] showed that reformulated oxycodone was associated with a significant reduction of past-month abuse after its introduction (45.1 % [95 % CI, 41.2–49.1 %]), apparently owing to a migration to other opioids, particularly heroin. However, this reduction leveled off, such that 25–30 % of the sample persisted in endorsing past-month abuse from 2012 to 2014.
Abuse of ADFs could still occur, particularly by the most common route: oral ingestion [41, 56]. Nor is there evidence as of yet that ADFs have any effect upon reducing rates of addiction, which is a chronic brain disease characterized by compulsive drug seeking and use despite adverse consequences [61]. What the evidence does suggest is that clinicians should not feel falsely secure when prescribing ADFs, but should consider them one part of a comprehensive pain management strategy in combination with other components of risk management.
The higher cost of ADFs compared to available generics currently may reduce the willingness of private and public insurance payers to offer coverage for them. However, given the potential for mitigating a public health problem with opioid abuse and associated cost reductions, payers would do well to keep current with ADF development and consider the possible role of newer formulations in a universal precautions approach to opioid prescribing [62]. Additional areas for coverage consideration could be reimbursement for patient risk assessment, provider training on best prescribing practices, including opioid-sparing multimodal therapy, and addiction treatment [62].
Opioid Rotation to Prevent Abuse
If one medication appears to have attractiveness for abuse, rotation to another opioid may prove safer and more beneficial. Rapid-onset opioids, for example, may be too rewarding for patients who have vulnerabilities to substance abuse because of the speed with which they enter the bloodstream and brain (Table 10.1). In addition, patients whose health insurance changes or is insufficient to cover a current opioid medication may, of necessity, need to be rotated to a different medication in the same class.
Caution and individual consideration for every patient are necessary when rotating from one opioid to another. Equianalgesic conversion tables are meant to provide guidance but are insufficient to determine the equivalent doses of different opioids [63, 64]. A published paradigm recommends decreasing one opioid slowly while slowly titrating the new opioid to effect using the following three steps [65]:
-
(1)
Reduce the original opioid dose by 10–30 % while beginning the new opioid at the lowest available dose.
-
(2)
Reduce the original opioid dose by 10–25 % per week while increasing the dose of the new daily opioid dose by 10–20 % based upon clinical need and safety.
-
(3)
Provide sufficient IR opioid throughout the rotation to prevent withdrawal and keep pain levels down so the patient is not tempted to take too much medication.
In most instances, the complete switch can occur within 3 to 4 weeks. This process takes longer than most current opioid conversion practices suggest. Be sure to seek consultation with a more experienced prescriber of opioids when needed.
Rotation to methadone requires particular caution due to a long half-life (usually 8 to 59 h and up to 100 h) compared with the medication’s analgesic effect, which usually lasts only 4–8 h [66, 67]. This unusual pharmacokinetic/pharmacodynamic profile can contribute to an unpredictable accumulation of methadone and toxicity. For this reason, patients should be treated as opioid naïve regardless of previous opioid dose when starting methadone: Consider starting patients (whether or not they are opioid naïve) on 15 mg or less per day in divided doses (q8h) and increase total daily dose by no more than 25–50 % no more frequently than weekly [68]. Again, seek expert consultation when necessary.
Clinical Considerations
When a treatment goal is to reduce the potential rewarding effect of a medication in a patient perceived to be at risk for opioid abuse, any and all of the following factors may contribute to substance abuse and should be considered [18, 56]:
-
The drug (availability, cost, purity, mode of administration, speed of brain entry);
-
The user whether patient or nonpatient (genetics, metabolism of drug, psychiatric symptoms, risk-taking behavior);
-
The environment (social setting, community attitudes, availability of drug, employment, educational opportunities).
A patient perceived as being at risk for opioid abuse should be treated, when possible with nonopioid medications and nonpharmacological modalities, including cognitive behavioral therapy, physical rehabilitation, and other alternatives that encourage active participation by the patient. Combining therapies may help keep opioid doses low if an opioid is deemed necessary. For pain severe enough to warrant sustained, around-the-clock opioid analgesia, initiate using the lowest effective dose and titrate slowly. High-risk patients may require tight controls such as frequent clinic visits, smaller quantities per prescription, and medication choices with slower onset and slower entry into the brain and thus less chance of reward.
Conclusion
A number of risk management strategies are important for avoiding harm with controlled substances that are prescribed for pain, particularly opioid analgesics and comedications that also depress respiration. High-risk patients require more intense risk mitigation strategies; however, all patients who are prescribed controlled substances for pain should be monitored using universal precautions. A number of tools are available and include urine toxicology, prescription-monitoring databases, and pill counts to check for adherence to the therapeutic regimen. Opioid formulations designed to deter tampering and abuse have a place in current pain management strategies. Universal precautions may come to include ADFs with sufficient increased market availability, supporting post-marketing studies, and the willingness of insurance payers to extend coverage. A comprehensive strategy should incorporate a mix of objective and subjective monitoring measures to meet therapeutic goals and reduce adverse outcomes.
References
Chen LH, Hedegaard H, Warner M. Drug-poisoning deaths involving opioid analgesics: United States, 1999–2011. NCHS data brief, no 166. Hyattsville, MD: National Center for Health Statistics; 2014.
Substance Abuse and Mental Health Services Administration. Results from the 2011 National Survey on Drug Use and Health: Summary of National Findings, NSDUH Series H-44, HHS Publication No. (SMA) 12-4713. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2012.
Hansen RN, Oster G, Edelsberg J, Woody GE, Sullivan SD. Economic costs of nonmedical use of prescription opioids. Clin J Pain. 2011;27(3):194–202.
Noble M, Treadwell JR, Tregear SJ, et al. Long-term opioid management for chronic noncancer pain. Cochrane Database Syst Rev. 2010;20(1):CD006605.
Manchikanti L, Manchukonda R, Pampati V, et al. Does random urine drug testing reduce illicit drug use in chronic pain patients receiving opioids? Pain Phys. 2006;9(2):123–9.
Manchikanti L, Manchukonda R, Damron KS, Brandon D, McManus CD, Cash K. Does adherence monitoring reduce controlled substance abuse in chronic pain patients? Pain Phys. 2006;9(1):57–60.
McCarberg BH. Chronic pain: reducing costs through early implementation of adherence testing and recognition of opioid misuse. Postgrad Med. 2011;123(6):132–9.
Katz NP, Adams EH, Chilcoat H, et al. Challenges in the development of prescription opioid abuse-deterrent formulations. Clin J Pain. 2007;23(8):648–60.
Dispensing Controlled Substances for the Treatment of Pain, DEA Policy Statement, 71 Fed. Reg. 52716, 52717, 6 Sept 2006.
Gourlay DL, Heit HA, Almahrezi A. Universal precautions in pain medicine: a rational approach to the treatment of chronic pain. Pain Med. 2005;6(2):107–12.
Binswanger IA, Blatchford PJ, Mueller SR, Stern MF. Mortality after prison release: opioid overdose and other causes of death, risk factors, and time trends from 1999 to 2009. Ann Intern Med. 2013;159(9):592–600.
Webster LR, Webster RM. Predicting aberrant behaviors in opioid-treated patients: preliminary validation of the opioid risk tool. Pain Med. 2005;6(6):432–42.
Butler SF, Fernandez K, Benoit C, Budman SH, Jamison RN. Validation of the revised screener and opioid assessment for patients with pain (SOAPP-R). J Pain. 2008;9(4):360–72.
Friedman R, Li V, Mehrotra D. Treating pain patients at risk: evaluation of a screening tool in opioid-treated pain patients with and without addiction. Pain Med. 2003;4(2):182–5.
Alturi S, Sudarshan G. A screening tool to determine the risk of prescription opioid abuse among patients with chronic non-malignant pain. Pain Physician. 2002;5(4):447–8.
Savage SR. Assessment for addiction in pain-treatment settings. Clin J Pain. 2002;18:28–38.
Dunbar SA, Katz NP. Chronic opioid therapy for non-malignant pain in patients with a history of substance abuse: report of 20 cases. J Pain Symptom Manage. 1996;11(3):163–71.
Webster LR, Dove B. Avoiding opioid abuse while managing pain: a guide for practitioners. North Branch, MN: Sunrise River Press; 2007. p. 126.
Peppin JF, Passik SD, Couto JE, et al. Recommendations for urine drug monitoring as a component of opioid therapy in the treatment of chronic pain. Pain Med. 2012;13(7):886–96.
Passik SD, Kirsh KL, Whitcomb L, et al. Monitoring outcomes during long-term opioid therapy for noncancer pain: results with the pain assessment and documentation tool. J Opioid Manag. 2005;1(257–66):423.
Butler SF, Budman SH, Fernandez KC, et al. Development and validation of the current opioid misuse measure. Pain. 2007;130:144–56.
Kirsh KL, Passik SD. The interface between pain and drug abuse and the evolution of strategies to optimize pain management while minimizing drug abuse. Exp Clin Psychopharmacol. 2008;16(5):400–4.
Savage SR. Multidimensional nature of pain: implications for opioid therapy. In: The 2014 international conference on opioids, Boston, MA, 8–10 June 2014.
Kahan M, Mailis-Gagnon A, Tunks E. Canadian guideline for safe and effective use of opioids for chronic non-cancer pain: implications for pain physicians. Pain Res Manag. 2011;16(3):157–8.
Federation of State Medical Boards of the United States, Inc. Model policy on the use of opioid analgesics in the treatment of chronic pain. Washington, DC: Federation of State Medical Boards. 2013. Available at: http://www.fsmb.org/pdf/pain_policy_july2013.pdf. Accessed 22 Dec 2014.
Hammett-Stabler CA, Webster LR. A clinical guide to urine drug testing. Stamford: PharmaCom Group Ltd; 2008.
American Society of Addiction Medicine. Drug testing: a white paper of the American Society of Addiction Medicine (ASAM). Chevy Chase, MD; 2013.
Chou E, Fanciullo GJ, Fine PG, et al. American pain society-American academy of pain medicine opioids guidelines panel. clinical guidelines for the use of chronic opioid therapy in chronic non-cancer pain. J Pain. 2009;10(2):113–30.
Owen GT, Burton AW, Schade CM, Passik S. Urine drug testing: current recommendations and best practices. Pain Physician 2012;15(3 Suppl):ES119–33.
Manchikanti L, Malla Y, Wargo BW, Fellows B. Comparative evaluation of the accuracy of immunoassay with liquid chromatography tandem mass spectrometry (LC/MS/MS) of urine drug testing (UDT) opioids and illicit drugs in chronic pain patients. Pain Physician. 2011;14(2):175–87.
Caplan YH, Goldberger BA. Alternative specimens for workplace drug testing. J Anal Toxicol. 2001;25(5):396–9.
Trescot AM, Faynboym S. A review of the role of genetic testing in pain medicine. Pain Phys. 2014;17(5):425–45.
Kitzmiller JP, Groen DK, Phelps MA, Sadee W. Pharmacogenomic testing: relevance in medical practice: why drugs work in some patients but not in others. Cleve Clin J Med. 2011;78(4):243–57.
Gourlay D, Heit HA, Caplan YH. Urine drug testing in clinical practice: dispelling the myths and designing strategies. Stamford, CT: PharmaCom Group, Inc.; 2006.
Reifler LM, Droz D, Bailey JE. Do prescription monitoring programs impact state trends in opioid abuse/misuse? Pain Med. 2012;13(3):434–42.
Clark T, Eadie J, Kreiner P, Strickler G. Prescription drug monitoring programs: an assessment of the evidence for best practices. The Prescription Drug Monitoring Program Center of Excellence, Heller School for Social Policy and Management, Brandeis University. Prepared for The Pew Charitable Trusts, 20 Sept 2012.
Simeone R, Holland L. An evaluation of prescription drug monitoring programs. Simeone Associates, Inc. 2006. Available at: http://media.timesfreepress.com/docs/2008/03/Federal_prescription_monitoring_report.pdf. Accessed 5 Dec 2014.
Paulozzi LJ, Kilbourne EM, Desai HA. Prescription drug monitoring programs and death rates from drug overdose. Pain Med. 2011;12(5):747–54.
National Alliance for Model State Drug Laws. Compilation of state prescription monitoring program maps. Charlottesville, VA, Current as of June 2014. Available at: http://www.namsdl.org/library/593BC7A6-1372-636C-DD7A83E6A8F6F0BC/. Accessed 22 Dec 2014.
Anson P. Pain patients forced to go ‘cold turkey’ from hydrocodone. National Pain Report. November 7, 2014. Available at: http://americannewsreport.com/nationalpainreport/pain-patients-forced-to-go-cold-turkey-from-hydrocodone-8825107.html. Accessed 5 Dec 2014.
US Food and Drug Administration (FDA), Center for Drug Evaluation and Research (CDER). Draft guidance for industry: abuse-deterrent opioids—evaluation and labeling. Published January 2013. FDA website. Available at: http://www.fda.gov/downloads/drugs/guidancecomplianceregulatoryinformation/guidances/ucm334743.pdf. Accessed 1 Dec 2014.
U.S. Food and Drug Administration (FDA). FDA approves abuse-deterrent labeling for reformulated OxyContin (News Release). Silver Spring, MD, 16 Apr 2013.
U.S. Food and Drug Administration (FDA). FDA approves new extended-release oxycodone with abuse-deterrent properties (News Release). Silver Spring, MD, 23 July 2014.
U.S. Food and Drug Administration (FDA). FDA approves labeling with abuse-deterrent features for third extended-release opioid analgesic [News Release]. Silver Spring, MD, 17 Oct 2014.
King Pharmaceuticals, Inc. Statement on voluntary recall of Embeda extended-release capsules CII. Published March 16, 2011. Available at: http://www.pfizer.com/files/news/embeda_recall_031611.pdf. Accessed 9 Dec 2014.
EMBEDA™ safety information. New York, NY: Pfizer, Inc.; 2014.
U.S. Food and Drug Administration (FDA). FDA approves extended-release, single-entity hydrocodone product with abuse-deterrent properties (News Release). Silver Spring, MD, 20 Nov 2014.
EXALGO (package insert). Hazelwood, MO: Mallinckrodt Brand Pharmaceuticals, Inc.; 2014.
Morton T, Kostenbader K, Montgomery J, Devarakonda K, Barrett T, Webster L. Comparison of subjective effects of extended-release versus immediate-release oxycodone/acetaminophen tablets in healthy nondependent recreational users of prescription opioids: a randomized trial. Postgrad Med. 2014;126(4):20–32.
OXECTA (package insert). New York, NY: Pfizer Inc.; 2014.
U.S. Food and Drug Administration (FDA). FDA statement: original Opana ER relisting determination. Published May 10, 2013. http://www.fda.gov/Drugs/DrugSafety/ucm351357.htm. Accessed 9 Dec 2014.
Vosburg SK, Jones JD, Manubay JM, Ashworth JB, Shapiro DY, Comer SD. A comparison among tapentadol tamper-resistant formulations (TRF) and OxyContin® (non-TRF) in prescription opioid abusers. Addiction. 2013;108(6):1095–106.
Webster LR. The question of opioid euphoria. Drug Discovery and Development. Published July 30, 2009. Available at: http://www.dddmag.com/Article-The-Question-of-Opioid-Euphoria-073009.aspx. Accessed 1 Dec 2014.
Butler SF, Black RA, Cassidy TA, Dailey TM, Budman SH. Abuse risks and routes of administration of different prescription opioid compounds and formulations. Harm Reduct J. 2011;8(29):1–17.
Cicero TJ, Surratt H, Inciardi JA, Munoz A. Relationship between therapeutic use and abuse of opioid analgesics in rural, suburban, and urban locations in the United States. Pharmacoepidemiol Drug Saf. 2007;16(8):827–40.
Budman SH, Grimes Serrano JM, Butler SF. Can abuse deterrent formulations make a difference? Expectation and speculation. Harm Reduct J. 2009;6:8.
Butler SF, Cassidy TA, Chilcoat H, et al. Abuse rates and routes of administration of reformulated extended-release oxycodone: initial findings from a sentinel surveillance sample of individuals assessed for substance abuse treatment. J Pain. 2013;14(4):351–8.
Coplan PM, Kale H, Sandstrom L, Landau C, Chilcoat HD. Changes in oxycodone and heroin exposures in the national poison data system after introduction of extended-release oxycodone with abuse-deterrent characteristics. Pharmacoepidemiol Drug Saf. 2013;22(12):1274–82.
Dart RC, Severtson SG, Bucher-Bartelson B. Trends in opioid analgesic abuse and mortality in the United States. N Engl J Med. 2015;372(16):573–4.
Cicero et al. Abuse-deterrent formulations and the prescription opioid abuse epidemic in the United States: lessons learned from OxyContin. JAMA Psychiatry 2015;72(5):424–30.
American Society of Addiction Medicine. Public Policy Statement: Definition of Addiction. 2011. ASAM website. Available at: http://www.asam.org/for-the-public/definition-of-addiction. Accessed 1 Dec 2014.
Katz NP, Birnbaum H, Brennan MJ, et al. Prescription opioid abuse: challenges and opportunities for payers. Am J Manag Care. 2013;19(4):295–302.
Knotkova H, Fine PG, Portenoy RK. Opioid rotation: the science and the limitations of the equianalgesic dose table. J Pain Symptom Manage 2009;38(3):426–39 (Review).
Webster LR, Fine PG. Review and critique of opioid rotation practices and associated risks of toxicity. Pain Med. 2012;13(4):562–70.
Webster LR, Fine PG. Overdose deaths demand a new paradigm for opioid rotation. Pain Med. 2012;13(4):571–4.
U.S. Food and Drug Administration. Information for healthcare professionals: methadone hydrochloride. U.S. Department of Health and Human Services. Silver Spring, MD, 2006.
Eap CB. BuclinT, Baumann P. Interindividual variability of the clinical pharmacokinetics of methadone: implications for the treatment of opioid dependence. Clin Pharmacokinet. 2002;41(14):1153–93.
Webster LR. Methadone-related deaths. J Opioid Manage. 2005;1(4):211–7.
Acknowledgment
Beth Dove of Dove Medical Communications, LLC, in Salt Lake City, Utah, provided research and medical writing.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Webster, L.R. (2016). Risk Mitigation Strategies. In: Staats, P., Silverman, S. (eds) Controlled Substance Management in Chronic Pain. Springer, Cham. https://doi.org/10.1007/978-3-319-30964-4_10
Download citation
DOI: https://doi.org/10.1007/978-3-319-30964-4_10
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-30962-0
Online ISBN: 978-3-319-30964-4
eBook Packages: MedicineMedicine (R0)