Abstract
Intracranial dermoid cysts are rare congenital lesions resulting from the inclusion of ectodermal cells during the closure of the neural tube, which occurs between the third and fifth gestational week. They may be associated with dermal sinus tracts and other neural tube closure defects, although they are usually not present in the sellar region. The cyst wall is made of connective tissue, and they are filled with a heterogeneous mixture of fat, hair, dystrophic calcifications or teeth, and fatty products of sebaceous glands. The cyst growth results from the accumulation of these glandular secretions and epithelial desquamation. Dermoid cysts are intradural extra-axial lesions that tend to occur on the midline and particularly in the sellar/parasellar region. Exceptional extradural locations have also been reported, especially within the cavernous sinus. Common clinical symptoms include headaches, seizures, and suprasellar dermoid cysts which often present with visual disturbances. Dermoid cysts are also well-known to cause chemical meningitis when they rupture and spill their content in the subarachnoid cisterns. Hydrocephalus is a rare presentation, and is subsequent to the trapping of the ventricular system rather than aseptic meningitis.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Intracranial dermoid cysts are rare congenital lesions resulting from the inclusion of ectodermal cells during the closure of the neural tube, which occurs between the third and fifth gestational week. They may be associated with dermal sinus tracts and other neural tube closure defects, although they are usually not present in the sellar region. The cyst wall is made of connective tissue, and they are filled with a heterogeneous mixture of fat, hair, dystrophic calcifications or teeth, and fatty products of sebaceous glands. The cyst growth results from the accumulation of these glandular secretions and epithelial desquamation. Dermoid cysts are intradural extra-axial lesions that tend to occur on the midline and particularly in the sellar/parasellar region. Exceptional extradural locations have also been reported, especially within the cavernous sinus. Common clinical symptoms include headaches, seizures, and suprasellar dermoid cysts often present with visual disturbances. Dermoid cysts are also well-known to cause chemical meningitis when they rupture and spill their content in the subarachnoid cisterns. Hydrocephalus is a rare presentation, and is subsequent to the trapping of the ventricular system rather than aseptic meningitis.
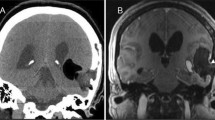
At imaging, a dermoid cyst appears as a well-circumscribed, fatty round mass with a peripheral capsule that may enhance or harbor calcifications. They are hypodense on CT, and possibly contain calcifications or teeth (Fig. 50.1). At MRI, dermoid cysts appear with characteristic fatty signal intensities on all sequences. Unlike lipomas, dermoid cysts are heterogeneous (Figs. 50.1 and 50.2) and have a capsule that may enhance (Fig. 50.2). The fatty content thus appears with T1- and T2-high signal intensities on spin-echo sequences, but demonstrate low GE T2 signal intensity. This point is crucial as it may mimic blood, like either a subacute parenchymal hematoma or a cavernoma. Therefore, T1WI with fat saturation is of precious help to confirm the fatty nature of the lesion and endorse the diagnosis of dermoid cyst when the lesion is heterogeneous (Figs. 50.1 and 50.4). Of course, in the absence of T1WI with fat saturation, one should consider that a simple nonenhanced CT scan easily demonstrates marked hypoattenuation in cases of fat and allows one to distinguish fatty from hemorrhagic lesions. Another clue to evoke the fatty origin of the signal is the presence of a chemical shift artifact that appears as a peripheral curvilinear hypointensity covering the lesion along the frequency-encoding direction (Fig. 50.3). In rare cases the fat floats on the rest of the liquid filling the cyst, giving a characteristic fat-fluid level, which we believe is pathognomonic of a dermoid cyst when observed in a well-defined intracranial lesion (Fig. 50.3). Finally, in cases of rupture in the subarachnoid space, the visualization of fatty T1-hyperintense droplets in the sulci or an anterior fat-fluid level in the ventricles is also highly suggestive of the diagnosis (Fig. 50.4).
Right parasellar dermoid cyst. (a) Sagittal T1WI depicts a hyperintense well-circumscribed right parasellar mass lesion that appears heterogeneous and nonenhancing on (b) axial CE T1WI. (c) Coronal T2WI nicely demonstrates that the lesion is composed of two distinct lobules, one being hyperintense (asterisk), the other isointense (star), a feature not present in lipoma. With decrease of both components signal intensities on (d) axial fat saturation T1WI, the fatty nature of the spontaneous T1 hyperintensity is confirmed. (e) Of note, fat content appears with low signal intensity on GE T2WI, as blood would. (f) Nonenhanced CT demonstrates marked hypoattenuation with no calcification
Huge dermoid cyst revealed by obstructive hydrocephalus. (a) Sagittal T1WI demonstrates a large, heterogeneous, hyperintense, well-circumscribed ovoid mass lesion with enlarged ventricles. Note a frontal focus of high signal intensity, known to be recent hemorrhage, along the external ventricle drainage. (b) Axial FLAIR image highlights heterogeneity of this parasellar lesion displacing internal temporal gyri and brainstem (star), leading to ventricular blockage at the level of the mesencephalon aqueduct (curved arrow), and subsequent hydrocephalus and transependymal resorption (asterisk). (c) Axial CE T1WI with fat saturation confirms the fatty nature of a significant part of the lesion and also shows mild enhancement of the cyst capsule (curved arrow)
Dermoid cyst of the left cavernous sinus. (a) Axial T2WI shows a round well-demarcated lesion within the left cavernous sinus, displacing the internal carotid artery medially. This axial slice reveals an obvious fluid-fluid level at mid-height of the lesion. On (b, c) Coronal T2WIs, the bottom part (b) appears with a homogeneous frankly hyperintense signal while the supernatant (c) appears less hyperintense, with a characteristic peripheral hypointense rim corresponding to a chemical shift artifact (arrows) along the frequency-encoding direction, as observed in the presence of fat. (d, e) Axial T1WIs without (d) and with (e) fat saturation confirm the fatty nature of the floating part of this cystic lesion. Such a fat-fluid level is a rare but very suggestive feature of dermoid cyst
Ruptured dermoid cyst with subarachnoid fatty droplets. (a) Coronal and (b) Sagittal T1WIs show a large ruptured right parasellar heterogeneous, hyperintense, well-demarcated mass and multiple foci of high signal intensity corresponding to lipid droplets scattered into the subarachnoid space and the left sylvian fissure (curved arrow), but also the left frontal horn, with a characteristic fat-fluid level (asterisk). (c) Coronal T2WI shows temporal/parasellar heterogeneous cyst covered by a hypointense rim consistent with a chemical shift artifact (arrow). (d) Coronal T1WI with fat saturation confirms the fatty component of this lesion by suppressing its spontaneous high signal intensity
Further Reading
Bonneville F, Cattin F, Marsot-Dupuch K et al (2006) T1 signal hyperintensity in the sellar region: spectrum of findings. Radiographics 26:93–113
Liu JK, Gottfried ON, Salzman KL et al (2008) Ruptured intracranial dermoid cysts: clinical, radiographic, and surgical features. Neurosurgery 62:377–384
Osborn AG, Preece MT (2006) Intracranial cysts: radiologic-pathologic correlation and imaging approach. Radiology 239:650–664
Author information
Authors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Bonneville, F. (2016). Dermoid Cyst. In: MRI of the Pituitary Gland. Springer, Cham. https://doi.org/10.1007/978-3-319-29043-0_50
Download citation
DOI: https://doi.org/10.1007/978-3-319-29043-0_50
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-29041-6
Online ISBN: 978-3-319-29043-0
eBook Packages: MedicineMedicine (R0)