Abstract
Depressive disorders are among the most prevalent psychiatric illnesses in the general population. In cancer patients, the prevalence of depression is dramatically increased. In addition to the psychosocial impact of a negative diagnosis, recent evidence suggests that cancer-induced depression (CID) is mediated by biological processes. This oncodynamic effect of cancer on the development of depression is poorly understood, leading to ineffective treatment of CID with drugs that are developed for depressive disorders in the general population. This chapter begins by outlining the clinical profile of major depressive disorder (MDD). We then provide a discussion of the most prominent neurobiological hypotheses of depression, including the monoamine hypothesis, the role of neurotrophins, physiological stress, inflammation, and glutamatergic signalling. The efficacy of current antidepressants is then discussed for depression in the general population and in cancer patients. This leads to a discussion of the biological basis of CID, including the effects of physiological stress, inflammation, and glutamatergic signalling. We conclude that more research is needed to determine oncodynamic events in the development of CID. Development of validated animal models is the first step in delineating contributing biological mechanisms, which will ultimately lead to more targeted drug development and improved efficacy.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Depression
- Cancer
- Antidepressants
- Prefrontal cortex
- Hippocampus
- Inflammatory cytokines
- Stress
- BDNF
- Glutamate
- NMDA antagonist
Introduction
The psychosocial impact of a cancer diagnosis undoubtedly contributes to co-morbid depression in cancer patients. While depression in the general population occurs with a lifetime prevalence of ~8–12 % [4], it can reach as high as 57 % in breast cancer patients and can be a staggering 95 % in high grade glioma [77]. In addition to the psychosocial contribution, recent preclinical and clinical evidence suggests the involvement of biological mechanisms in cancer-induced depression (CID). This biological underpinning, and the development of the capacity to investigate it at the basic level, has a potentially profound impact on the quality of life of cancer patients. Currently, treatment for CID is limited to therapies developed for non-cancer-related major depressive disorder (MDD) despite lack of convincing evidence for the efficacy of these treatments in cancer patients [73]. A more effective strategy for treating CID begins with the investigation of the oncodynamic effect of cancer on depression at the most basic level. A better understanding of this interaction would provide the framework for developing new pharmacotherapy aimed at novel targets. This chapter will discuss what is currently known about the oncodynamic effect of cancer on depression by first reviewing depression at the clinical and etiological level, then examining cancer signalling events that are likely to contribute to CID.
Depression
The term melancholia (ancient Greek for “black bile”) was first used by Hippocrates around 400 B.C. to describe a disease state of persistent fear and despair [101]. According to the humoral theory, this disease state arose from excess black bile—one of the four bodily liquids, or humors. In the early nineteenth century, a “clinico-anatomical” view of disease asserted that symptoms of illnesses could be correlated with anatomical lesions [10]. During the second half of the nineteenth century, this conceptual shift led to greater focus on the brain in an effort to better understand melancholia. Today, insight from preclinical, biochemical, genetic, post-mortem, and neuroimaging studies have led to a greater understanding and classification of mood disorders. In addition to developing cognitive behavioural therapy (CBT), the last several decades have seen a proliferation of psychotropic drugs, which target specific biological pathways, enter the market. In the case of antidepressants, while the efficacy and tolerance have generally improved, low clinical response rates underscore the importance of continued progress in understanding the neurobiology of depression.
Diagnosis and Classification of Depression
Mood disorders are characterized by persistent periods of intensely reduced or elevated mood that interfere with normal functioning. The subcategory of mood disorders that is defined by reduced mood is termed depressive disorders. According to the current fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) of the American Psychiatric Association (APA), the common feature of this subcategory is the presence of sad, empty, or irritable mood [5]. This can be accompanied by various somatic and cognitive changes that impede day-to-day functioning. Differences between depressive disorders depend on duration and timing of symptoms, as well as presumed aetiology.
In the case of (MDD; commonly called major depression, clinical depression, or simply depression), changes in affect, cognition, and neurovegetative function occur in discrete episodes with inter-episodic remission [5]. Episodes must persist for at least 2 weeks, although typically last considerably longer, and at least one episode is required to make a diagnosis of MDD. If the mood disturbances persist for 2 or more years without periods of remission, a diagnosis of persistent depressive disorder (or dysthymia) is given. The depressive episodes required to make a diagnosis of MDD or dysthymia are characterized by the presence of five (or more) of nine symptoms, summarized in Table 1.1. In addition, at least one of the symptoms must be either (1) depressed mood or (2) anhedonia (loss of interest or pleasure).
Neurobiology of Depression
There are several neurochemical and neuroanatomical correlates of depression, which have led to multiple etiological hypotheses. In reviewing these hypotheses, it is worth noting that no single model can sufficiently account for all aspects and variations of depression. Rather than a unified hypothesis of depression, it is likely that the true aetiology of a complex and heterogeneous mental disorder such as depression incorporates components from all current theories.
The Monoamine Hypothesis of Affective Disorders
Monoamine neurotransmitters are a class of neurotransmitters derived from aromatic amino acids, and most notably include serotonin, norepinephrine, and dopamine. In the 1950s, the role of monoamines in mood disorders became apparent through a series of inadvertent discoveries, which eventually culminated in the monoamine hypothesis of affective disorders [101]. In 1955, some patients being treated with the antihypertensive agent reserpine were found to become depressed after treatment [48, 95]. It was later shown that reserpine depletes vesicular storage of brain serotonin, which in turn reduces the available serotonin for synaptic transmission [48, 101, 135]. Conversely, the antimycobacterial agent iproniazid was shown to improve mood in tubercular patients with depression [22, 48]. Iproniazid inhibits monoamine oxidase (MAO), the enzyme that degrades free monoamines in the presynaptic nerve terminal. By inhibiting MAO, iproniazid enhances central serotonin and norepinephrine transmission. This discovery prompted the development of other monoamine oxidase inhibitors (MAOIs). Further support for the monoamine hypothesis came when imipramine, a drug initially developed as an anxiolytic for agitated patients with psychosis, was shown to have antidepressant effects [48, 69]. Imipramine, now classified as a tricyclic antidepressant (TCA), acts by blocking monoamine reuptake transporters, thereby increasing the level of serotonin and norepinephrine in the synapse. Together, MOAIs and TCAs constitute first generation antidepressants. In the late 1980s, momentum for the monoamine hypothesis prompted a second generation of antidepressants to enter development. These drugs aimed to increase receptor specificity and, therefore, decrease adverse side effects and increase tolerability. This second generation of antidepressants includes selective serotonin reuptake inhibitors (SSRIs), which are currently the most prescribed class of antidepressants, as well as serotonin–norepinephrine reuptake inhibitors (SNRIs). Although current antidepressants that target monoamine transmission are clinically efficacious for some patients, their delayed antidepressant effect has proven to be problematic for the monoamine hypothesis. SSRIs increase monoamine transmission within hours of administration and begin to cause side effects within hours or days [48, 68]. However, enhanced mood requires weeks of chronic treatment. Additionally, monoamine depletion studies have found that acute reduction of monoamines can decrease mood in patients with a personal or family history of depression but not in healthy controls [68, 104, 123]. Rather than a direct effect of monoamine neurotransmission on mood state, it is now thought that antidepressants induce secondary transcriptional and translational changes that ultimately lead to synaptogenesis and neurogenesis [68, 101, 113]. For example, the transcription factor CREB (cAMP response element binding protein) is downstream of serotonin receptors and regulates expression of brain-derived neurotrophic factor (BDNF). Clinical studies report decreased levels of CREB in the cortex of depressed patients, and experimentally increased CREB activity in the hippocampus of rodents has been reported to induce antidepressant-like effects on behavioural tests [12, 101]. Additionally, CREB levels in the hippocampus are increased following chronic administration of antidepressants, such as the SSRI fluoxetine [12, 106]. These neuroplastic changes require several weeks and are necessary to achieve behavioural changes, which is consistent with the delayed response to antidepressants. Although the monoamine hypothesis has been the most clinically relevant theory of depression, leading to the development of first and second generation antidepressants, the delayed clinical response to increased monoamines suggests that monoamine deficiency is not a primary abnormality in the aetiology of depression.
Neurotrophins, BDNF, and the Anatomy of Depression
In the brain, the monoamines serotonin and norepinephrine are largely released by the raphe nuclei and the locus coeruleus, respectively. These brainstem structures project to regions in the cerebral cortex and limbic system that regulate emotion, reward, attention, and executive function. Specifically, neuroimaging and volumetric post-mortem studies have identified reduced neural activity and dendritic atrophy in the hippocampus and the prefrontal cortex (PFC) [25, 60, 102, 134]. Although functional imagining studies have produced limited overlap in the brain regions identified in depression, meta-analytic results suggest that the regions with the most consistently reduced neural activity include the PFC, insula, cerebellum, and the parahippocampal gyrus (PHG; the major inflow tract to the hippocampus) [32, 45]. More consistent results have been provided through structural neuroimaging studies. These results were summarized in a meta-analysis, which revealed consistent volume reductions in frontal regions (anterior cingulate, orbitofrontal, and PFC), as well as in the hippocampus and dorsal striatum [45, 63]. Moreover, volume reductions have been shown to be attenuated with antidepressant treatment [134].
The precise mechanism of region-specific volume reductions in depression has not been established. However, the role of BDNF has attracted interest in recent years. Stress-induced downregulation in hippocampal BDNF expression has been well documented in preclinical studies [26]. Conversely, chronic treatment with antidepressants has been shown to upregulate hippocampal and PFC BDNF expression [87]. Post-mortem studies on humans support preclinical results, showing decreased levels of hippocampal BDNF in untreated subjects compared to subjects treated with antidepressant at the time of death [16, 26, 58, 87]. These correlation studies have prompted investigation into a more causal role of BDNF regulation in depression. To investigate the possibility of a causal association, a single-nucleotide polymorphism (SNP) in BDNF was developed, which substitutes methionine for valine at amino acid 66 (Val66Met), leading to improper storage of BDNF in neurons [30, 68]. Consequently, less BDNF is secreted from the nerve terminals. When implemented into a biological system, knock-in mice with this polymorphism exhibited increased anxiety-related behaviours when exposed to stressors [17, 68]. Antidepressants have also been shown to increase other growth factors in the hippocampus, such as vascular endothelial growth factor (VEGF), likely through the activation of transcriptional regulators such as CREB [68, 143]. However, a direct neuroprotective role of growth factors such as BDNF has not been straightforward to establish due to region-specificity. For example, in the ventral tegmental area (VTA; most notably involved in reward response and drug addiction) and the nucleus accumbens (NAc; also involved in reward processing), infusion of BDNF causes increased depressive-like behaviours in mice [67].
Stress and Cytokines
There is a strong evidence in the literature that dysregulation of the hypothalamic–pituitary–adrenal axis (HPA) is an important factor in the biological aetiology of depression. In response to perceived stress by the cortical regions, the hypothalamus releases corticotropin-releasing hormone (CRH). CRH then stimulates the anterior pituitary gland to release adrenocorticotropic hormone (ACTH), which in turn stimulates the adrenal cortex to release cortisol, a glucocorticoid. In a negative feedback mechanism, excess cortisol inhibits the hypothalamus and anterior pituitary, halting further production of cortisol. Although the first depressive episode usually involves a stressful psychosocial “trigger”, later episodes of depression become increasingly “endogenous” as the illness progresses [45]. Even in the absence of exogenous triggers, increased plasma, urine, and cerebrospinal fluid (CSF) cortisol levels have been well documented in a subset of patients with depression [57, 85, 110, 111]. Chronic exposure to elevated levels of glucocorticoids can have a deleterious impact on brain structures involved in cognition and emotional functions [82]. In fact, hypercortisolaemia has been shown to cause structural remodelling in the hippocampus, amygdala, and PFC [90]. In the hippocampus, certain types of acute stress have been demonstrated to suppress neurogenesis in the dentate gyrus, leading to atrophy—an effect that has also been observed in patients with Cushing’s syndrome, which is primarily characterized by increased ACTH release from the pituitary gland and hypercortisolaemia [139]. This stress-induced atrophy has been postulated to be the underlying mechanism of the volumetric reductions observed in the hippocampus and PFC of patients with depression. Further support for the role of chronic stress in depression has come from preclinical studies. The most successful and widely used murine models of depression have, in fact, relied on the clinical observations of stress as a risk factor in depression [103]. Chronic mild stress, chronic unpredictable stress, social defeat paradigms, as well as direct chronic administration of corticosterone have all provided some measure of construct validity in modelling depression by causing anhedonia in the sucrose preference test [39, 103, 114, 146, 147]. These paradigms have also demonstrated face validity by modelling demonstrable symptoms of depression (e.g. decreased investigative and locomotor activity), and predictive validity through the reversal of depressive-like behaviours following chronic antidepressant treatment [103, 146]. It is important to note, however, that true construct validity cannot be achieved in models of depression, as this would require re-creating the disease aetiology, which remains largely unknown. At the molecular level, there is evidence that hypercortisolaemia is associated with modulation of the serotonergic system. The serotonin receptor subtype 5-HT1A has been strongly implicated in depression and anxiety, with reduced receptor numbers and affinity reported in some patients [126]. Recently, preclinical and clinical evidence has suggested a causal role of stress-induced hypercortisolaemia on reduced 5-HT1A receptor downregulation [72, 80].
“Sickness behaviour” constitutes a set of clinically recognized behaviours that human and animal subjects exhibit at the onset of infectious disease [44]. These behaviours, which are due to activation of the inflammatory response, share many characteristics with depression, such as anhedonia and cognitive impairment [45]. Cytokines are the molecular mediators of inflammatory responses. Pro-inflammatory cytokines such as interleukin 1 (IL-1), IL-6, and tumour necrosis factor alpha (TNF-α) have been found to be elevated in the plasma and CSF of patients with depression [151]. In rodents, direct injection of low doses of IL-1 has also been shown to induce “sickness behaviour” [28, 68]. In humans, depressive symptoms have been reported as a common side effect of treatment with interferon alpha (IFN-α), a pro-inflammatory agent, occurring in approximately 30–50 % of patients [52]. Conversely, evidence suggests that anti-inflammatory treatment such as non-steroidal anti-inflammatory drugs (NSAIDs) can be effective adjuvant drugs, particularly for treatment-resistant depression [65]. Despite strong evidence for a possible role of inflammation in the aetiology of depression, the neurobiological mechanism involved remains unknown. Further investigations should focus on the effect of neuroimmunological mediators (i.e. microglia) on surrounding glia and neurons [68].
Glutamate
Glutamate is the anionic form of the amino acid glutamic acid. In the nervous system, glutamate is the most abundant neurotransmitter [92] and plays a key role in cognitive processes that are dependent on synaptic plasticity, such as learning and memory [89]. Peripherally, glutamate is released as a response to induced inflammation and activation of peripheral nociceptive fibres [19, 109]. Additionally, direct injection of glutamate has been shown to increase sensitivity to thermal and mechanical stimuli in murine models [11, 54].
Ketamine is a widely used general anaesthetic, and is pharmacologically classified as an antagonist to N-Methyl-D-aspartate receptors (NMDAR), a type of ionotropic glutamate receptors. In recent years, ketamine has become the focus of accumulating reports assessing its antidepressant effects in both humans and animal models [97, 153]. In 2000, Berman and colleagues carried out the first clinical study that reported on ketamine’s rapid antidepressant properties. The antidepressant effects of ketamine were robust for the patients involved in the randomized trial [9] and were then replicated in a larger study involving 18 treatment-resistant patients [153]. Since then, glutamate signalling has become well established as a factor in the neurostructural changes in depression [29, 125], with extensive preclinical [8, 38, 39, 75] and clinical evidence [53, 152] to support the validity of glutamate modulation for treating depression.
In 2010, interested in the potential for new depression therapeutics, Li and colleagues carried out a study on rats that began to elucidate a possible antidepressant mechanism for ketamine. They found that administration of ketamine rapidly activated the mammalian target of rapamycin (mTOR) pathway, leading to increased synaptogenesis in the PFC [74]. Additionally, blocking mTOR signalling effectively blocked ketamine’s ability to induce synaptogenesis. It is now suggested that antagonism of NMDA receptors by ketamine causes an increased concentration of extracellular glutamate, resulting in fast excitation of neurons through increased activity of α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid (AMPA) receptors, another type of ionotropic glutamate receptors [27]. This fast excitation causes an influx of calcium ions through voltage-gated calcium channels, which in turn stimulates the release of BDNF. BDNF subsequently stimulates tropomyosin-related kinase B (TrkB) and downstream signalling pathways including PI3 K-Akt and MAPK. These pathways stimulate mTOR, a serine-threonine protein kinase, which in turn regulates genes that increase the density of synaptic proteins, ultimately leading to synaptogenesis and antidepressant behavioural responses [27]. Although ketamine is also known to interact with other signalling systems, including the dopamine D2 receptors, opioid receptors, and sigma (σ) receptors [66, 119], there is considerable evidence to suggest that the primary antidepressant response of ketamine is mediated by the NMDA receptor. For example, other NMDA antagonists, including MK-801 and CPPene, have also shown effectiveness in inducing anti-depressive effects in animal models [7, 84]. Moreover, the behavioural antidepressant effects of ketamine in animal models of depression have been shown to act independently of σ receptors [119]. In addition to ketamine, the antidepressant action of tianeptine, a clinically used TCA, has recently been attributed to glutamatergic regulation, possibly through the modulation of both AMPAR and NMDAR [91].
Clinically, concentrations of glutamate are elevated in the serum or plasma of patients with MDD [3, 61, 88, 94]. At the brain level, studies using magnetic resonance spectroscopy (MRS) reveal a decreased unresolved glutamate/glutamine signal (Glx) and glutamate alone signal (Glu) in brain regions that are relevant to depression, such as the PFC and anterior cingulate cortex [6, 46].
Antidepressants
Treatment for MDD has improved significantly since the serendipitous discovery of MAOIs and the formation of the monoamine hypothesis of depression in the 1950s. However, with the underlying aetiology of the illness still unclear, efforts to create increasingly targeted therapy has been relatively stagnant. Monotherapy with first and second generation antidepressants often fails to alleviate symptoms, and it may take multiple attempts with different antidepressants and adjunct therapy to achieve clinical efficacy. Treating depression becomes even more difficult when it presents as comorbidity, in part due to a lack of understanding of the relationship between the primary disease and depression. Few studies have examined depression in cancer patients at the basic level, and thus treatment options for CID are limited to those therapies developed for use in non-cancer-related MDD. In this section, we will consider the clinical efficacy of antidepressants in MDD as well as CID.
Antidepressants in Major Depressive Disorder
The Sequenced Treatment Alternatives to Relieve Depression (STAR*D) trial was the largest effort to date on the efficacy of antidepressants. It was commissioned by the National Institute of Mental Health (NIMH) and completed in 2006 [124]. In 2008, data from the trial became available. The study recruited 4041 adult patients (1127 dropped out; 2876 were analyzable) with MDD from primary care and psychiatric settings [50, 124]. As the primary outcome measure for remission, STAR*D used the Hamilton Depression Rating Scale (HAM-D) to measure the severity of depression. The HAM-D is a commonly used 52-item questionnaire that rates severity of depression on a 17-point scale, with scores of 0–7 considered normal [42]. In level 1 treatment, patients received citalopram monotherapy, one of the most prescribed SSRIs, and remission rates were approximately 28 % based on HAM-D scores [51]. In levels 2, 3, and 4 of the trial, patients who did not achieve remission in the previous level were either switched to a different antidepressant or received an augmentation to citalopram treatment. Switches to new antidepressants consisted of other SSRIs, SNRIs, TCAs, or other agents that act on monoamine transmission. In the case of treatment augmentation, a wide range of agents were used, including anxiolytics, lithium, and thyroid hormone T3 [51]. In each level of the trial, the treatment-resistant patients from the previous level were randomized to the new treatment regimens. Remission rates in levels 2, 3, and 4 of the trial were all below 30 %. With only a third of MDD patients responding to initial monotherapy, systematic reviews of randomized control trials (RCTs) have sought to better define the role of antidepressants in the clinical setting. In 2009, Cipriani et al. showed that of the commonly prescribed second generation antidepressants, escitalopram and sertraline were the most efficacious and best tolerated, leading to fewer discontinuations [18]. In another meta-analysis, Fournier et al. investigated antidepressant efficacy relative to initial symptom severity [33]. They concluded that patients with severe MDD benefit substantially from antidepressant treatment, whereas benefit is minimal in mild or moderate MDD. In addition to pharmacological modulation, CBT has been shown to be beneficial for patients with depression, even in the case of severe MDD [24, 49]. In some cases of severe MDD that is not responsive to antidepressants, electroconvulsive therapy (ECT) may be used. ECT has been extensively shown to be effective in achieving remission in treatment-resistant patients [93]. However, due to the requirement of anaesthetic, ECT is rarely used as a first line of treatment. More recently, repetitive transcranial magnetic stimulation (rTMS) has also been shown to provide some benefit as adjunct therapy in treatment-resistant patients [93].
Antidepressants in Cancer-Induced Depression
In stark contrast to the large-scale and high-quality RCTs available for primary MDD, few studies have investigated antidepressant efficacy and alternative or adjunct therapies in cancer patients. This is surprising considering the high prevalence of depression comorbidity in cancer, a clinical observation that spans decades [13, 31, 35, 62, 78, 144]. Difficulties in studying and treating CID are found at the preclinical and clinical levels. At the preclinical level, the lack of validated animal models for CID has restricted inquiry into the possible biological mechanisms involved. Cancer patients with comorbid depression are, therefore, limited to antidepressant treatment developed for non-cancer patients. Clinically, depression is underdiagnosed and undertreated in cancer patients, largely owing to the psychosocial complication of what might be considered “appropriate sadness” in terminally ill patients compared to treatable psychiatric disease [13, 78, 137]. In addition, factors such as cancer type, cancer stage, and demographic convolute an already complex mental disorder. Thus, in the absence of more precisely tailored treatment, antidepressants (particularly SSRIs) remain the first line of treatment in the oncologic setting.
Although few studies have examined the efficacy of antidepressants in CID, a handful of systematic reviews have compiled such studies in an attempt to draw clinical conclusions. In 2006, 2007, and 2011, three groups examined the literature for antidepressant efficacy in cancer. The first review focused on SSRIs and found that four of the five studies reported positive results, and one study using fluoxetine showed no difference in incidence of depression compared to placebo [145]. The second review, which had overlapping studies with the first, also examined the efficacy of mianserin (a tetracyclic antidepressant; TeCA) in two included studies [120]. In this review, three placebo-controlled trials (including the two mianserin studies) showed positive results. Of the remaining four studies, the two placebo-controlled trials did not detect a difference between treatment and placebo, while the two trials comparing active treatments found temporal improvement of depressive scores but no group differences. The third review in 2011 updated the previous results with one additional study, which did not detect a difference between placebo and paroxetine or desipramine [105]. Underscoring the lack of high-quality studies on the topic, a 2013 Cochrane review found no eligible RCTs, controlled trials, cohort studies or case-control studies investigating antidepressant efficacy in patients with primary brain tumours [122]. Studies under consideration were excluded for a wide range of issues, such as reporting on usual clinical care rather than systematically evaluating specific treatments. Most recently, another systematic review has investigated antidepressant efficacy in breast cancer specifically [15]. This review identified two eligible studies with mixed results, both of which have been included in other systematic reviews [105, 120, 145]. Concerns raised in this review included small sample sizes, and therefore a significant risk of bias. Overall, these systematic reviews highlight the inadequacy of currently available literature on the question of antidepressant efficacy in cancer patients. From these studies, broad clinical conclusions cannot be drawn, which points to a need for larger and better designed clinical trials as well as a capacity to study CID at the basic level.
In addition to pharmacotherapy, psychological interventions such as CBT, supportive psychotherapy, and group psychotherapy may be efficacious for cancer patients either as primary treatment or in combination with antidepressants [2, 73, 79]. However, in clinical trials of antidepressants, physiological interventions, including regular hospice care, may be a confounding variable that can mask antidepressant effect [79]. Therefore, intervention models under investigation need to be well designed and appropriately analyzed to control for such confounds.
Cancer-Induced Depression
Strong clinical and preclinical evidence exists in the literature to support a causal role of cancer on depression. In the introduction to this chapter, the prevalence of depression in the oncologic setting was discussed in comparison to depression in the general population. While the staggeringly high prevalence of depression in cancer patients suggests a strong correlation, the impact of psychosocial factors makes it difficult to establish causation or biological mechanisms. However, early clinical studies reveal that psychological changes relating to depression may in fact precede the diagnosis of cancer [40, 55, 112]. More recently, a breast cancer study, which included 428 women, reported that over 25 % of women with breast cancer exhibited symptoms of depression prior to being informed of their cancer diagnosis [142]. Using data from the World Mental Health Survey Initiative, another study performed a retrospective analysis on the mental health of cancer patients, which included 19 countries and more than 52,000 patients [107]. The study found that depression symptoms appear predictive of a later cancer diagnosis. By demonstrating an increased prevalence of depression in patients who have cancer but are unaware of their diagnosis, these clinical findings effectively eliminate the confounding psychosocial effect of a cancer diagnosis, and suggest a possible causal role of cancer on mental health at the biological level. In addition to clinical support, this oncodynamic impact of cancer on depression is supported through common biological systems between cancer and depression; namely, inflammation, physiological stress, and glutamatergic dysregulation. In order to investigate the possible causal role of these systems in the induction of depression by cancer cells, validated CID animal models need to be established. In 2009, Pyter et al. reported that peripheral mammary tumours induce behavioural changes such as anhedonia in rats and increase plasma biomarkers such as cytokines and corticosterone [115]. Similarly, in 2011 Lamkin et al. were able to replicate these findings using ovarian cancer in mice [71]. To investigate possible neurological correlates in CID, Yang et al. recently showed that tumour-bearing mice had reduced proliferating and progenitor neurons in the dentate gyrus of the hippocampus when compared to control animals [149]. Although these studies have provided compelling insight into the association between cancer and depression, more rigorous validation of CID models is needed. Behavioural and relevant neuroanatomical comparisons to existing validated models of depression would yield more convincing animal models. In addition, reversal trials using antidepressants on the positive control depressive models would further establish the validity of the behavioural tests used prior to evaluating the CID models. Properly validated CID models would be an essential tool in manipulating inflammatory, stress, and glutamatergic systems in the investigation of the causal oncodynamic effect of cancer on depressive symptoms. To date, only correlative associations have been established between cancer and depression, although a causal relationship has been postulated based on the clinical studies discussed in earlier in this chapter. Expanding on what is currently known about the common biological systems that are involved in cancer and depression, we can discuss the most plausible oncodynamic mechanisms of CID. These proposed mechanisms of CID are summarized in Fig. 1.1.
Schematic summarizing proposed oncodynamic mechanisms of CID. Glioma cells in the brain release large amounts of glutamate (Glu), which directly cause excitotoxicity of neurons by hyperexcitation of NMDARs. This causes a decrease in neurogenesis and synaptogenesis in brain regions such as the hippocampus (HIP) and PFC, which leads to depressive symptoms. Peripheral cancer cells also release large amounts of glutamate. Substance P (SP) released by cancer cells impairs the blood–brain barrier (BBB), causing increased permeability, which may allow peripherally secreted glutamate to enter the brain. Alternatively, peripherally secreted glutamate may act on the spinal cord through signal transduction pathways that project to brain regions involved in depression. Peripheral cancer cells also secrete cytokines, which may be a causal factor in vegetative depressive symptoms. Tumour burden has also been shown to influence the hypothalamic–pituitary–adrenal (HPA) axis, which leads to chronic physiological stress and depressive symptoms
Oncodynamic Effect Through Inflammation
A well-established characteristic of most cancer cells is their ability to exploit the host’s immune system at multiple stages of tumour development and metastasis [1, 20, 21, 34, 41, 43]. Specifically, cancer cells recruit an array of cytokine-producing leukocytes, such as tumour-associated macrophages (TAMs) [20, 100]. Cancer cells themselves are also capable of expressing various cytokines, such as TNF-α and Il-6, that attract more leukocytes [20]. In doing so, cancer cells employ the same mechanisms that are normally activated to repair tissue in response to tissue damage [70]. For example, in order to repair normal tissue damage, the extracellular matrix (ECM) that binds cells together must be broken down in order to allow for the recruitment of new cells to the site of injury. Platelets aggregating at the site of injury release platelet derived growth factor (PDGF), which in turn stimulates fibroblasts to secrete matrix metalloproteinases (MMPs). These enzymes break down the ECM of damaged cells and allow the arrival of new cells [70]. Cancer cells that secrete PDGF can exploit this mechanism by recruiting MMP-secreting fibroblasts to break down the ECM of healthy epithelial cells and by replacing them with multiplying cancer cells [70, 76].
As previously discussed in this chapter, depression is strongly associated with pro-inflammatory mediators in clinical and preclinical studies. The ability of cancer cells to directly secrete pro-inflammatory mediators highlights one possible oncodynamic pathway of CID. We can further postulate on the specific downstream effect of this oncodynamic event through closer investigation of inflammatory consequences in depression. Clinical studies investigating the cytokine profile of cancer patients have shown that IL-6, which is directly secreted by cancer cells [127], is elevated in the plasma of cancer patients who also exhibit depressive symptoms, compared to cancer patients who do not exhibit depressive symptoms [56, 99, 138]. In another study, the increased plasma concentration of IL-6 in ovarian cancer patients was associated with the vegetative symptoms of depression (such as fatigue and weight loss), but not with affective symptoms or overall depression [83]. Similar effects on vegetative, but not affective, depression symptoms have been observed with IFN-α therapy-induced inflammation [14, 70, 98]. Taken together, these results suggest that cancer cell-secreted IL-6 (and possibly other inflammatory mediators) induces an oncodynamic effect on depression, which specifically exacerbates vegetative symptoms.
Oncodynamic Effect Through Physiological Stress
Physiological stress through activation of the sympathetic nervous system is an adaptive response to environmental stressors. As previously discussed, dysregulation of this response is strongly implicated in the aetiology of depression. Undoubtedly, the psychosocial impact of a cancer diagnosis is one source of this dysregulation. The induction of chronic physiological stress in cancer patients is supported by the clinical observation of increased plasma cortisol in advanced cancer patients [81, 128]. Additionally, plasma levels of cortisol are higher with increased tumour burden, metastasis, and pervasiveness of the cancer [116, 129, 141]. This suggests a direct impact of cancer cells on physiological stress, in addition to the psychosocial contribution. However, the mechanism of cancer-induced activation of the stress response has not been investigated, with the notable exception of adrenal tumours that autonomously produce and secrete cortisol [36]. Other studies have investigated general HPA activation in cancer patients, but not the mechanism of activation, and often in the context of investigating depressive symptoms [83, 138]. Although clinical studies suggest a direct oncodynamic effect of cancer on the dysregulation of the physiological stress response (and ultimately depression), a discussion on the biological mechanisms is lacking in the literature.
Oncodynamic Effect Through Glutamatergic Signalling
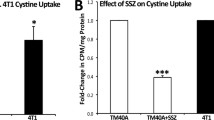
As early as the 1980s, results from clinical investigations have demonstrated elevated plasma levels of glutamate in cancer patients [108, 118]. More recently, the mechanism of glutamate release by cancer cells as well downstream consequences of this release have garnered attention in the literature. Initial studies focused on glioma cell lines and found that glutamate secretion into the extracellular environment involved the glutamate/cystine antiporter system x −c [59]. This excess glutamate secretion causes excitotoxicity and death of surrounding neurons through over-activation of NMDARs [131, 150]. The same mechanism of glutamate secretion through system x −c was later characterized in multiple cancer cell lines, including metastatic breast and prostate cancers, through in vitro and in vivo studies [130–133, 140].
Earlier in this chapter, the emerging role of glutamatergic signalling in the aetiology of depression was discussed. Excess glutamate secretion by cancer cells provides a biologically plausible cause of glutamate dysregulation in depression. This connection is particularly convincing in the case of gliomas, which secrete very high amounts of glutamate and which are also associated with a very high incidence of depression, as previously discussed. Neuronal hyperactivation due to glioma-secreted glutamate would interfere with neuroplastic and synaptoplastic events in the mPFC and the hippocampus, ultimately leading to depression. In peripheral cancers, the effect of glutamate on depression may not be as direct. Because of glutamate’s key role in many neuronal signalling events, glutamate distribution and extracellular fluid (ECF) concentrations in the brain are tightly controlled. The vast majority of glutamate in the brain is stored in astrocytes, while glutamate in the ECF is maintained at very low concentrations relative to plasma levels in the periphery [47, 86, 136]. The blood-brain-barrier (BBB) is a crucial structure in the maintenance of this concentration difference between plasma and brain ECF glutamate. Excitatory amino acid transporters (EAATs) on the abluminal (brain-facing) membrane of the BBB transport glutamate from the ECF to the peripherally circulating blood. The luminal (blood-facing) membrane lacks EAATs, thus preventing the entrance of glutamate from the blood into the brain under normal physiological conditions. However, recent evidence has suggested that pathological conditions disrupt the BBB, leading to increased permeability. Substance P (SP) is a pro-inflammatory neuropeptide that has been implicated in nociception [23], depression [64, 96, 148], and is expressed in breast cancer cells [117]. It was recently shown that breast cancer cell-secreted SP is involved in the transmigration of cancer cells across the BBB [121]. To do this, SP activates an inflammatory response in the endothelial cells that comprise the BBB, which ultimately increases their permeability. Therefore, under pathological conditions such as metastatic disease, tight regulation of brain glutamate may be impaired by breaches in the BBB. This represents one possible mechanism through which glutamate secreted by peripheral tumours can affect brain physiology and induce depression.
An alternative oncodynamic mechanism would be analogous to pain transmission. Glutamate released by peripheral cancer cells causes pain in a model of bone metastasis, which is attenuated using an antagonist of system x −c [140]. In this paradigm, glutamate does not need to cross the BBB in order to transmit a pain signal. Nociceptive fibres are activated peripherally and the signal is transmitted through the ascending pathway to cortical regions that perceive pain [37]. Similarly, it is plausible that peripheral glutamate activates CNS pathways indirectly through signal transmission, culminating in brain alterations consistent with depression. Therefore, although a mechanism has not been investigated in the literature, preclinical and clinical evidence suggests that cancer-secreted glutamate imparts an oncodynamic effect on the development of CID. In this section, two biologically plausible mechanisms for this oncodynamic effect have been suggested.
Conclusion
Depression in cancer patients is a highly prevalent comorbidity, which affects quality of life and survivorship. Although psychosocial factors contribute to depression in the cancer setting, the clinical evidence reviewed in this chapter suggests a more causal role of cancer on the induction of depression. Through careful consideration of the overlapping biological mechanisms involved in depression aetiology and cancer physiology, we can postulate on the initial oncodynamic signalling event(s) that lead to the induction of depression. However, a robustly validated preclinical model of CID is lacking in the literature. Therefore, the capacity to investigate the oncodynamic mechanism of CID through manipulation of a valid model has yet to be established. Future direction in this field of research should focus on developing the capacity to investigate the mechanism(s) of CID, while being attentive to advancements in the understanding of depression aetiology.
References
Aggarwal BB, Shishodia S, Sandur SK, et al. Inflammation and cancer: how hot is the link? Biochem Pharmacol. 2006;72:1605–21.
Akechi T. Psychotherapy for depression among patients with advanced cancer. Jpn J Clin Oncol. 2012;42:1113–9.
Altamura CA, Mauri MC, Ferrara A, et al. Plasma and platelet excitatory amino acids in psychiatric disorders. Am J Psychiatry. 1993;150:1731–3.
Andrade L, Caraveo-Anduaga JJ, Berglund P, et al. The epidemiology of major depressive episodes: results from the international consortium of psychiatric epidemiology (ICPE) surveys. Int J Methods psychiatr Res. 2003;12:3–21.
Association AP. Diagnostic and statistical manual of mental disorders. 5th ed. Arlington: American Psychiatric Publishing; 2013.
Auer DP, Putz B, Kraft E, et al. Reduced glutamate in the anterior cingulate cortex in depression: an in vivo proton magnetic resonance spectroscopy study. Biol Psychiatry. 2000;47:305–13.
Autry AE, Adachi M, Nosyreva E, et al. NMDA receptor blockade at rest triggers rapid behavioural antidepressant responses. Nature. 2011;475:91–5.
Banasr M, Chowdhury GM, Terwilliger R, et al. Glial pathology in an animal model of depression: reversal of stress-induced cellular, metabolic and behavioral deficits by the glutamate-modulating drug riluzole. Mol Psychiatry. 2010;15:501–11.
Berman RM, Cappiello A, Anand A, et al. Antidepressant effects of ketamine in depressed patients. Biol Psychiatry. 2000;47:351–4.
Berrios GE. Melancholia and depression during the 19th century: a conceptual history. Br J Psychiatry: (the journal of mental science). 1988;153:298–304.
Bhave G, Karim F, Carlton SM, et al. Peripheral group I metabotropic glutamate receptors modulate nociception in mice. Nat Neurosci. 2001;4:417–23.
Blendy JA. The role of CREB in depression and antidepressant treatment. Biol Psychiatry. 2006;59:1144–50.
Caplette-Gingras A, Savard J. Depression in women with metastatic breast cancer: a review of the literature. Palliat Suppor Care. 2008;6:377–87.
Capuron L, Gumnick JF, Musselman DL, et al. Neurobehavioral effects of interferon-alpha in cancer patients: phenomenology and paroxetine responsiveness of symptom dimensions. Neuropsychopharmacol (official publication of the American College of Neuropsychopharmacology). 2002;26:643–52.
Carvalho AF, Hyphantis T, Sales PM, et al. Major depressive disorder in breast cancer: a critical systematic review of pharmacological and psychotherapeutic clinical trials. Cancer Treat Rev. 2014;40:349–55.
Chen B, Dowlatshahi D, Macqueen GM, et al. Increased hippocampal BDNF immunoreactivity in subjects treated with antidepressant medication. Biol Psychiatry. 2001;50:260–5.
Chen ZY, Jing D, Bath KG, et al. Genetic variant BDNF (Val66Met) polymorphism alters anxiety-related behavior. Science. 2006;314:140–3.
Cipriani A, Furukawa TA, Salanti G, et al. Comparative efficacy and acceptability of 12 new-generation antidepressants: a multiple-treatments meta-analysis. Lancet. 2009;373:746–58.
Conn PJ, Pin JP. Pharmacology and functions of metabotropic glutamate receptors. Annu Rev Pharmacol Toxicol. 1997;37:205–37.
Coussens LM, Werb Z. Inflammation and cancer. Nature. 2002;420:860–7.
Coussens LM, Zitvogel L, Palucka AK. Neutralizing tumor-promoting chronic inflammation: a magic bullet? Science. 2013;339:286–91.
Crane GE. The psychiatric side-effects of iproniazid. Am J Psychiatry. 1956;112:494–501.
De Felipe C, Herrero JF, O’brien JA et al. Altered nociception, analgesia and aggression in mice lacking the receptor for substance P. Nature. 1998;392:394–397.
Driessen E, Hollon SD. Cognitive behavioral therapy for mood disorders: efficacy, moderators and mediators. Psychiatric Clin North Am. 2010;33:537–55.
Duman RS, Aghajanian GK. Synaptic dysfunction in depression: potential therapeutic targets. Science. 2012;338:68–72.
Duman RS, Monteggia LM. A neurotrophic model for stress-related mood disorders. Biol Psychiatry. 2006;59:1116–27.
Duman RS, Voleti B. Signaling pathways underlying the pathophysiology and treatment of depression: novel mechanisms for rapid-acting agents. Trends Neurosci. 2012;35:47–56.
Dunn AJ, Swiergiel AH, De Beaurepaire R. Cytokines as mediators of depression: what can we learn from animal studies? Neurosci Biobehav Rev. 2005;29:891–909.
Duric V, Banasr M, Stockmeier CA, et al. Altered expression of synapse and glutamate related genes in post-mortem hippocampus of depressed subjects. Int J Neuropsychopharmacol [official scientific journal of the Collegium Internationale Neuropsychopharmacologicum (CINP)]. 2013;16:69–82.
Egan MF, Kojima M, Callicott JH, et al. The BDNF val66met polymorphism affects activity-dependent secretion of BDNF and human memory and hippocampal function. Cell. 2003;112:257–69.
Endicott J. Measurement of depression in patients with cancer. Cancer. 1984;53:2243–9.
Fitzgerald PB, Laird AR, Maller J, et al. A meta-analytic study of changes in brain activation in depression. Hum Brain Mapp. 2008;29:683–95.
Fournier JC, Derubeis RJ, Hollon SD, et al. Antidepressant drug effects and depression severity: a patient-level meta-analysis. JAMA: (the journal of the American Medical Association). 2010;303:47–53.
Franklin RA, Liao W, Sarkar A, et al. The cellular and molecular origin of tumor-associated macrophages. Science. 2014;344:921–5.
Fras I, Litin EM, Pearson JS. Comparison of psychiatric symptoms in carcinoma of the pancreas with those in some other intra-abdominal neoplasms. Am J Psychiatry. 1967;123:1553–62.
Goh G, Scholl UI, Healy JM, et al. Recurrent activating mutation in PRKACA in cortisol-producing adrenal tumors. Nat Genet. 2014;46:613–7.
Gordon-Williams RM, Dickenson AH. Central neuronal mechanisms in cancer-induced bone pain. Curr Opin Support Palliat Care. 2007;1:6–10.
Gourley SL, Espitia JW, Sanacora G, et al. Antidepressant-like properties of oral riluzole and utility of incentive disengagement models of depression in mice. Psychopharmacology. 2012;219:805–14.
Gourley SL, Taylor JR. Recapitulation and reversal of a persistent depression-like syndrome in rodents. In: Crawley N, et al, editors. Current protocols in neuroscience/ editorial board, Jacqueline Chapter 9: Unit 9 32. 2009.
Green AI, Austin CP. Psychopathology of pancreatic cancer. A psychobiologic probe. Psychosomatics. 1993;34:208–21.
Grivennikov SI, Greten FR, Karin M. Immunity, inflammation, and cancer. Cell. 2010;140:883–99.
Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62.
Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011;144:646–74.
Hart BL. Biological basis of the behavior of sick animals. Neurosci Biobehav Rev. 1988;12:123–37.
Hasler G. Pathophysiology of depression: do we have any solid evidence of interest to clinicians? World Psychiatry: [official journal of the World Psychiatric Association (WPA)]. 2010;9:155–61.
Hasler G, Van Der Veen JW, Tumonis T, et al. Reduced prefrontal glutamate/glutamine and gamma-aminobutyric acid levels in major depression determined using proton magnetic resonance spectroscopy. Arch Gen Psychiatry. 2007;64:193–200.
Hawkins RA. The blood-brain barrier and glutamate. Am J Clin Nutr. 2009;90:867S–74S.
Hirschfeld RM. History and evolution of the monoamine hypothesis of depression. J Clin Psychiatry. 2000;61(6):4–6.
Hoifodt RS, Strom C, Kolstrup N, et al. Effectiveness of cognitive behavioural therapy in primary health care: a review. Fam Pract. 2011;28:489–504.
Howland RH. Sequenced treatment alternatives to relieve depression (STAR*D). Part 1: study design. J Psychosoc Nurs Ment Health Serv. 2008;46:21–4.
Howland RH. Sequenced treatment alternatives to relieve depression (STAR*D). Part 2: Study outcomes. J Psychosoc Nurs Ment Health Serv. 2008;46:21–4.
Hoyo-Becerra C, Schlaak JF, Hermann DM. Insights from interferon-alpha-related depression for the pathogenesis of depression associated with inflammation. Brain Behav Immun. 2014;42:222–231.
Ibrahim L, Diazgranados N, Franco-Chaves J, et al. Course of improvement in depressive symptoms to a single intravenous infusion of ketamine vs add-on riluzole: results from a 4-week, double-blind, placebo-controlled study. Neuropsychopharmacology: (official publication of the American College of Neuropsychopharmacology). 2012;37:1526–33.
Jackson DL, Graff CB, Richardson JD, et al. Glutamate participates in the peripheral modulation of thermal hyperalgesia in rats. Eur J Pharmacol. 1995;284:321–5.
Jacobsson L, Ottosson JO. Initial mental disorders in carcinoma of pancreas and stomach. Acta Psychiatr Scand Suppl. 1971;221:120–7.
Jehn CF, Kuehnhardt D, Bartholomae A, et al. Biomarkers of depression in cancer patients. Cancer. 2006;107:2723–9.
Juruena MF, Cleare AJ. Pariante CM (2004), The hypothalamic pituitary adrenal axis, glucocorticoid receptor function and relevance to depression. Revista brasileira de psiquiatria. 1999;26:189–201.
Karege F, Vaudan G, Schwald M, et al. Neurotrophin levels in postmortem brains of suicide victims and the effects of antemortem diagnosis and psychotropic drugs. Brain Res Mol Brain Res. 2005;136:29–37.
Kato S, Negishi K, Mawatari K, et al. A mechanism for glutamate toxicity in the C6 glioma cells involving inhibition of cystine uptake leading to glutathione depletion. Neuroscience. 1992;48:903–14.
Kempton MJ, Salvador Z, Munafo MR, et al. Structural neuroimaging studies in major depressive disorder. Meta-analysis and comparison with bipolar disorder. Arch Gen Psychiatry. 2011;68:675–90.
Kim JS, Schmid-Burgk W, Claus D, et al. Increased serum glutamate in depressed patients. Archiv fur Psychiatrie und Nervenkrankheiten. 1982;232:299–304.
Koenig R, Levin SM, Brennan MJ. The emotional status of cancer patients as measured by a psychological test. J Chronic Dis. 1967;20:923–30.
Koolschijn PC, Van Haren NE, Lensvelt-Mulders GJ, et al. Brain volume abnormalities in major depressive disorder: a meta-analysis of magnetic resonance imaging studies. Hum Brain Mapp. 2009;30:3719–35.
Kormos V, Gaszner B. Role of neuropeptides in anxiety, stress, and depression: from animals to humans. Neuropeptides. 2013;47:401–19.
Kornstein SG, Schneider RK. Clinical features of treatment-resistant depression. J Clin Psychiatry. 2001;62(16):18–25.
Kortekaas R, Maguire RP, Van Waarde A, et al. Despite irreversible binding, PET tracer [11C]-SA5845 is suitable for imaging of drug competition at sigma receptors-the cases of ketamine and haloperidol. Neurochem Int. 2008;53:45–50.
Krishnan V, Han MH, Graham DL, et al. Molecular adaptations underlying susceptibility and resistance to social defeat in brain reward regions. Cell. 2007;131:391–404.
Krishnan V, Nestler EJ. The molecular neurobiology of depression. Nature. 2008;455:894–902.
Kuhn R. The treatment of depressive states with G 22355 (imipramine hydrochloride). Am J Psychiatry. 1958;115:459–64.
Lamkin DM. Inflammatory processes and depressive-like behavior in a syngeneic model of ovarian cancer. Iowa City: University of Iowa; 2010.
Lamkin DM, Lutgendorf SK, Lubaroff D, et al. Cancer induces inflammation and depressive-like behavior in the mouse: modulation by social housing. Brain Behav Immun. 2011;25:555–64.
Lanzenberger R, Wadsak W, Spindelegger C, et al. Cortisol plasma levels in social anxiety disorder patients correlate with serotonin-1A receptor binding in limbic brain regions. Int J Neuropsychopharmacol/[official scientific journal of the Collegium Internationale Neuropsychopharmacologicum (CINP)]. 2010;13:1129–43.
Li M, Fitzgerald P, Rodin G. Evidence-based treatment of depression in patients with cancer. J Clin Oncol: (official journal of the American Society of Clinical Oncology). 2012;30:1187–96.
Li N, Lee B, Liu RJ, et al. mTOR-dependent synapse formation underlies the rapid antidepressant effects of NMDA antagonists. Science. 2010;329:959–64.
Li N, Liu RJ, Dwyer JM, et al. Glutamate N-methyl-D-aspartate receptor antagonists rapidly reverse behavioral and synaptic deficits caused by chronic stress exposure. Biol Psychiatry. 2011;69:754–61.
Link CJ Jr, Kohn E, Reed E. The relationship between borderline ovarian tumors and epithelial ovarian carcinoma: epidemiologic, pathologic, and molecular aspects. Gynecol Oncol. 1996;60:347–54.
Litofsky NS, Farace E, Anderson F, Jr. et al. Depression in patients with high-grade glioma: results of the Glioma Outcomes Project. Neurosurgery. 2004;54:358–366; discussion 366–357.
Lloyd-Williams M. Difficulties in diagnosing and treating depression in the terminally ill cancer patient. Postgrad Med J. 2000;76:555–8.
Lloyd-Williams M, Payne S, Reeve J, et al. Antidepressant medication in patients with advanced cancer–an observational study. QJM: (monthly journal of the Association of Physicians). 2013;106:995–1001.
Lopez JF, Chalmers DT, Little KY, et al. A.E. Bennett Research Award. Regulation of serotonin1A, glucocorticoid, and mineralocorticoid receptor in rat and human hippocampus: implications for the neurobiology of depression. Biol Psychiatry. 1998;43:547–73.
Lundstrom S, Furst CJ. Symptoms in advanced cancer: relationship to endogenous cortisol levels. Palliat Med. 2003;17:503–8.
Lupien SJ, Mcewen BS, Gunnar MR, et al. Effects of stress throughout the lifespan on the brain, behaviour and cognition. Nat Rev Neurosci. 2009;10:434–45.
Lutgendorf SK, Weinrib AZ, Penedo F, et al. Interleukin-6, cortisol, and depressive symptoms in ovarian cancer patients. J Clin Oncol: (official journal of the American Society of Clinical Oncology). 2008;26:4820–7.
Maeng S, Zarate CA Jr, Du J, et al. Cellular mechanisms underlying the antidepressant effects of ketamine: role of alpha-amino-3-hydroxy-5-methylisoxazole-4-propionic acid receptors. Biol Psychiatry. 2008;63:349–52.
Mahar I, Bambico FR, Mechawar N, et al. Stress, serotonin, and hippocampal neurogenesis in relation to depression and antidepressant effects. Neurosci Biobehav Rev. 2014;38:173–92.
Mann GE, Yudilevich DL, Sobrevia L. Regulation of amino acid and glucose transporters in endothelial and smooth muscle cells. Physiol Rev. 2003;83:183–252.
Martinowich K, Manji H, Lu B. New insights into BDNF function in depression and anxiety. Nat Neurosci. 2007;10:1089–93.
Mauri MC, Ferrara A, Boscati L, et al. Plasma and platelet amino acid concentrations in patients affected by major depression and under fluvoxamine treatment. Neuropsychobiology. 1998;37:124–9.
Mcentee WJ, Crook TH. Glutamate: its role in learning, memory, and the aging brain. Psychopharmacology. 1993;111:391–401.
Mcewen BS. Physiology and neurobiology of stress and adaptation: central role of the brain. Physiol Rev. 2007;87:873–904.
Mcewen BS, Chattarji S, Diamond DM, et al. The neurobiological properties of tianeptine (Stablon): from monoamine hypothesis to glutamatergic modulation. Mol Psychiatry. 2010;15:237–49.
Meldrum BS. Glutamate as a neurotransmitter in the brain: review of physiology and pathology. J Nutr. 2000;130:1007s–15s.
Micallef-Trigona B. Comparing the effects of repetitive transcranial magnetic stimulation and electroconvulsive therapy in the treatment of depression: a systematic review and meta-analysis. Depression Res Treat. 2014;2014:135049.
Mitani H, Shirayama Y, Yamada T, et al. Correlation between plasma levels of glutamate, alanine and serine with severity of depression. Prog Neuropsychopharmacol Biol Psychiatry. 2006;30:1155–8.
Muller JC, Pryor WW, Gibbons JE, et al. Depression and anxiety occurring during Rauwolfia therapy. J Am Med Assoc. 1955;159:836–9.
Munoz M, Covenas R. Involvement of substance P and the NK-1 receptor in human pathology. Amino Acids. 2014;46:1727–50.
Murrough JW. Ketamine as a novel antidepressant: from synapse to behavior. Clin Pharmacol Ther. 2012;91:303–9.
Musselman DL, Lawson DH, Gumnick JF, et al. Paroxetine for the prevention of depression induced by high-dose interferon alfa. New Eng J Med. 2001;344:961–6.
Musselman DL, Miller AH, Porter MR, et al. Higher than normal plasma interleukin-6 concentrations in cancer patients with depression: preliminary findings. Am J Psychiatry. 2001;158:1252–7.
Nashed MG, Balenko MD, Singh G. Cancer-induced oxidative stress and pain. Curr Pain Headache Rep. 2014;18:384.
Nestler EJ, Barrot M, Dileone RJ, et al. Neurobiology of depression. Neuron. 2002;34:13–25.
Nestler EJ, Gould E, Manji H, et al. Preclinical models: status of basic research in depression. Biol Psychiatry. 2002;52:503–28.
Nestler EJ, Hyman SE. Animal models of neuropsychiatric disorders. Nat Neurosci. 2010;13:1161–9.
Neumeister A, Nugent AC, Waldeck T, et al. Neural and behavioral responses to tryptophan depletion in unmedicated patients with remitted major depressive disorder and controls. Arch Gen Psychiatry. 2004;61:765–73.
Ng CG, Boks MP, Zainal NZ, et al. The prevalence and pharmacotherapy of depression in cancer patients. J Affect Disord. 2011;131:1–7.
Nibuya M, Nestler EJ, Duman RS. Chronic antidepressant administration increases the expression of cAMP response element binding protein (CREB) in rat hippocampus. J Neurosci: (the official journal of the Society for Neuroscience). 1996;16:2365–72.
O’neill S, Posada-Villa J, Medina-Mora ME, et al. Associations between DSM-IV mental disorders and subsequent self-reported diagnosis of cancer. J Psychosom Res. 2014;76:207–12.
Ollenschlager G, Karner J, Karner-Hanusch J, et al. Plasma glutamate–a prognostic marker of cancer and of other immunodeficiency syndromes? Scand J Clin Lab Invest. 1989;49:773–7.
Omote K, Kawamata T, Kawamata M, et al. Formalin-induced release of excitatory amino acids in the skin of the rat hindpaw. Brain Res. 1998;787:161–4.
Pariante CM, Lightman SL. The HPA axis in major depression: classical theories and new developments. Trends Neurosci. 2008;31:464–8.
Parker KJ, Schatzberg AF, Lyons DM. Neuroendocrine aspects of hypercortisolism in major depression. Horm Behav. 2003;43:60–6.
Passik SD, Roth AJ. Anxiety symptoms and panic attacks preceding pancreatic cancer diagnosis. Psycho-oncology. 1999;8:268–72.
Pittenger C, Duman RS. Stress, depression, and neuroplasticity: a convergence of mechanisms. Neuropsychopharmacology: (official publication of the American College of Neuropsychopharmacology). 2008;33:88–109.
Pollak DD, Rey CE, Monje FJ. Rodent models in depression research: classical strategies and new directions. Ann Med. 2010;42:252–64.
Pyter LM, Pineros V, Galang JA, et al. Peripheral tumors induce depressive-like behaviors and cytokine production and alter hypothalamic-pituitary-adrenal axis regulation. Proc Natl Acad Sci USA. 2009;106:9069–74.
Rasmuson T, Ljungberg B, Grankvist K, et al. Increased serum cortisol levels are associated with high tumour grade in patients with renal cell carcinoma. Acta Oncol. 2001;40:83–7.
Reddy BY, Greco SJ, Patel PS, et al. RE-1-silencing transcription factor shows tumor-suppressor functions and negatively regulates the oncogenic TAC1 in breast cancer cells. Proc Natl Acad Sci USA. 2009;106:4408–13.
Rivera S, Lopez-Soriano FJ, Azcon-Bieto J, et al. Blood amino acid compartmentation in mice bearing Lewis lung carcinoma. Cancer Res. 1987;47:5644–6.
Robson MJ, Elliott M, Seminerio MJ, et al. Evaluation of sigma (sigma) receptors in the antidepressant-like effects of ketamine in vitro and in vivo. Eur Neuropsychopharmacol: (the journal of the European College of Neuropsychopharmacology). 2012;22:308–17.
Rodin G, Lloyd N, Katz M, et al. The treatment of depression in cancer patients: a systematic review. Support Care Cancer: (official journal of the Multinational Association of Supportive Care in Cancer). 2007;15:123–36.
Rodriguez PL, Jiang S, Fu Y, et al. The proinflammatory peptide substance P promotes blood-brain barrier breaching by breast cancer cells through changes in microvascular endothelial cell tight junctions. Int J Cancer. (Journal international du cancer). 2014;134:1034–44.
Rooney A, Grant R. Pharmacological treatment of depression in patients with a primary brain tumour. Cochrane Database Syst Rev. 2013;5:Cd006932.
Ruhe HG, Mason NS, Schene AH. Mood is indirectly related to serotonin, norepinephrine and dopamine levels in humans: a meta-analysis of monoamine depletion studies. Mol Psychiatry. 2007;12:331–59.
Rush AJ, Fava M, Wisniewski SR, et al. Sequenced treatment alternatives to relieve depression (STAR*D): rationale and design. Control Clin Trials. 2004;25:119–42.
Sanacora G, Treccani G, Popoli M. Towards a glutamate hypothesis of depression: an emerging frontier of neuropsychopharmacology for mood disorders. Neuropharmacology. 2012;62:63–77.
Savitz J, Lucki I, Drevets WC. 5-HT(1A) receptor function in major depressive disorder. Prog Neurobiol. 2009;88:17–31.
Schafer ZT, Brugge JS. IL-6 involvement in epithelial cancers. J Clin Invest. 2007;117:3660–3.
Schaur RJ, Fellier H, Gleispach H, et al. Tumor host relations. I. Increased plasma cortisol in tumor-bearing humans compared with patients with benign surgical diseases. J Cancer Res Clin Oncol. 1979;93:281–5.
Schaur RJ, Semmelrock HJ, Schauenstein E, et al. Tumor host relations. II. Influence of tumor extent and tumor site on plasma cortisol of patients with malignant diseases. J Cancer Res Clin Oncol. 1979;93:287–92.
Seidlitz EP, Sharma MK, Saikali Z, et al. Cancer cell lines release glutamate into the extracellular environment. Clin Exp Metastasis. 2009;26:781–7.
Seidlitz EP, Sharma MK, Singh G. A by-product of glutathione production in cancer cells may cause disruption in bone metabolic processes. Can J Physiol Pharmacol. 2010;88:197–203.
Seidlitz EP, Sharma MK, Singh G. Extracellular glutamate alters mature osteoclast and osteoblast functions. Can J Physiol Pharmacol. 2010;88:929–36.
Sharma MK, Seidlitz EP, Singh G. Cancer cells release glutamate via the cystine/glutamate antiporter. Biochem Biophys Res Commun. 2010;391:91–5.
Sheline YI, Gado MH, Kraemer HC. Untreated depression and hippocampal volume loss. Am J Psychiatry. 2003;160:1516–8.
Shore PA, Silver SL, Brodie BB. Interaction of reserpine, serotonin, and lysergic acid diethylamide in brain. Science. 1955;122:284–5.
Smith QR. Transport of glutamate and other amino acids at the blood-brain barrier. J Nutr. 2000;130:1016s–22s.
Somerset W, Stout SC, Miller AH et al. Breast cancer and depression. Oncology. 2004;18:1021–34; discussion 1035–26, 1047–28.
Soygur H, Palaoglu O, Akarsu ES, et al. Interleukin-6 levels and HPA axis activation in breast cancer patients with major depressive disorder. Prog Neuropsychopharmacol Biol Psychiatry. 2007;31:1242–7.
Starkman MN, Gebarski SS, Berent S, et al. Hippocampal formation volume, memory dysfunction, and cortisol levels in patients with Cushing’s syndrome. Biol Psychiatry. 1992;32:756–65.
Ungard RG, Seidlitz EP, Singh G. Inhibition of breast cancer-cell glutamate release with sulfasalazine limits cancer-induced bone pain. Pain. 2014;155:28–36.
Van Der Pompe G, Antoni MH, Heijnen CJ. Elevated basal cortisol levels and attenuated ACTH and cortisol responses to a behavioral challenge in women with metastatic breast cancer. Psychoneuroendocrinology. 1996;21:361–74.
Van Esch L, Roukema JA, Ernst MF, et al. Combined anxiety and depressive symptoms before diagnosis of breast cancer. J Affect Disord. 2012;136:895–901.
Warner-Schmidt JL, Duman RS. VEGF is an essential mediator of the neurogenic and behavioral actions of antidepressants. Proc Natl Acad Sci USA. 2007;104:4647–52.
Watts S, Leydon G, Birch B, et al. Depression and anxiety in prostate cancer: a systematic review and meta-analysis of prevalence rates. BMJ Open. 2014;4:e003901.
Williams S, Dale J. The effectiveness of treatment for depression/depressive symptoms in adults with cancer: a systematic review. Br J Cancer. 2006;94:372–90.
Willner P. Validity, reliability and utility of the chronic mild stress model of depression: a 10-year review and evaluation. Psychopharmacology. 1997;134:319–29.
Yan HC, Cao X, Das M, et al. Behavioral animal models of depression. Neurosci Bull. 2010;26:327–37.
Yang LM, Yu L, Jin HJ, et al. Substance P receptor antagonist in lateral habenula improves rat depression-like behavior. Brain Res Bull. 2014;100:22–8.
Yang M, Kim J, Kim JS, et al. Hippocampal dysfunctions in tumor-bearing mice. Brain Behav Immun. 2014;36:147–55.
Ye ZC, Sontheimer H. Glioma cells release excitotoxic concentrations of glutamate. Cancer Res. 1999;59:4383–91.
Young JJ, Bruno D, Pomara N. A review of the relationship between proinflammatory cytokines and major depressive disorder. J Affect Disord. 2014;169c:15–20.
Zarate CA Jr, Brutsche NE, Ibrahim L, et al. Replication of ketamine’s antidepressant efficacy in bipolar depression: a randomized controlled add-on trial. Biol Psychiatry. 2012;71:939–46.
Zarate CA Jr, Singh JB, Carlson PJ, et al. A randomized trial of an N-methyl-D-aspartate antagonist in treatment-resistant major depression. Arch Gen Psychiatry. 2006;63:856–64.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Nashed, M.G., Frey, B.N., Rosebush, P., Singh, G. (2016). Oncodynamic Effect of Cancer on Depression. In: Singh, G. (eds) Oncodynamics: Effects of Cancer Cells on the Body. Springer, Cham. https://doi.org/10.1007/978-3-319-28558-0_6
Download citation
DOI: https://doi.org/10.1007/978-3-319-28558-0_6
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-28556-6
Online ISBN: 978-3-319-28558-0
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)