Abstract
In Japan, most postmortem computed tomography angiography (PMCTA) is performed by injecting contrast media from the peripheral venous route in combination with chest compression immediately after confirmation of death in deceased patients brought into the emergency room (ER) in a state of cardiopulmonary arrest (CPA).
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Emergency Room (ER)
- Cardiopulmonary arrest (CPA)
- Cardiopulmonary resuscitation (CPR)
- Chest compression
- Postmortem computed tomography angiography (PMCTA)
In Japan, most postmortem computed tomography angiography (PMCTA) is performed by injecting contrast media from the peripheral venous route in combination with chest compression immediately after confirmation of death in deceased patients brought into the emergency room (ER) in a state of cardiopulmonary arrest (CPA).
An automatic injector was used in PMCTA for injecting contrast media through an intravenous catheter retained for infusion during cardiopulmonary resuscitation (CPR), generally from the cubital vein. The contrast medium for PMCTA was a nonionic iodine agent for clinical use in a prefilled syringe. A dose of 2 mL/kg was injected at a rate of 1.5 mL/s (total dose for an adult case ranged from 100 to 150 mL). While injecting the contrast medium, chest compression was done for 2 min at a rate of 100 times/min (a total of 200 times), in accordance with the 2010 American Heart Association Guidelines for CPR.
Compared with PMCTA in Western countries, Japanese resuscitation PMCTA has the following four benefits despite the simplicity of method: (1) no risk of extravasation of the contrast media caused by increased permeability of the vascular wall, (2) minimal invasiveness to the cadaver, (3) thromboembolism can be detected as a filling defect in the arteries or veins, and (4) short performance time permits its use in clinical CT examination rooms in ordinary hospitals during working hours.
Resuscitation PMCTA is a relatively simple, less invasive, effective procedure as an addition to conventional PMCT for the detection of vascular disease-related causes of death, allowing evaluation of organ damage owing to trauma in deceased patients brought into an ER in a state of CPA.
1 Introduction
In Japan, as a result of a very low rate of conventional autopsy and the highest CT distribution rate per population density in the world, postmortem CT (PMCT) is performed on over 20,000 cases yearly [1]. The majority of these cases involve screening for unusual causes of death of patients brought into emergency rooms (ERs) in a state of CPA and on whom CPR was ineffective.
PMCT is useful in detecting hemorrhagic lesions in cases of nontraumatic death such as subarachnoid hemorrhage, cerebral hemorrhage, aortic dissection, and rupture of aortic aneurysms [1]. PMCT can also detect fatal injuries in many cases of traumatic death. However, with noncontrast PMCT, it is generally difficult to identify ischemic myocardium and coronary artery thromboembolism in acute heart failure, pulmonary artery thromboembolism, and the exact location and extent of parenchymatous organ damage in traumatic death cases. In such cases, PMCTA can provide further diagnostic information.
Several methods of PMCTA in Western countries require surgical techniques [2–5] and thus cannot be performed in clinical CT rooms of ordinary hospitals during working hours. In Japan, most PMCTA is performed by injecting contrast medium from the peripheral venous route in combination with chest compression immediately after confirmation of death in deceased patients brought into the ER in a state of CPA [6–9].
2 Methods
Our subjects were patients for whom death was confirmed after arriving at the ER in a state of CPA. After confirmation of death, consent to perform noncontrast PMCT and resuscitation PMCTA was obtained from the family of each subject. PMCT was performed soon after the confirmation of death using a clinical scanner in the Radiology Department of our institution. Resuscitation PMCTA was then performed with scanning parameters settings the same as those for PMCT.
An automatic injector was used for injecting a contrast medium through the intravenous catheter that was retained for infusion during CPR, generally from the cubital vein. The contrast medium used was a nonionic iodine agent for clinical angiography use and prefilled in a syringe. A dose of 2 mL/kg was injected at a rate of 1.5 mL/s (total dose for an adult case ranged from 100 to 150 mL). While injecting the contrast medium, chest compression was done for 2 min at a rate of 100 times/min (a total of 200 times), in accordance with the 2010 American Heart Association Guidelines for CPR.
Chest compression during CPR increases blood pressure and generates cardiac output of approximately one third to one fourth compared with the normal state of a living human [10]. This phenomenon enables the methodology of resuscitation PMCTA. With chest compression, contrast medium injected from the upper arm (cubital vein) enters the right atrium (RA), moves into the right ventricle (RV), pulmonary artery (PA), pulmonary vein, left atrium, left ventricle, and aorta, with an enhanced image of the arterial route being delineated. Without chest compression, injected contrast medium migrates from the right atrium to the inferior vena cava (IVC) without flowing into the right ventricle or left side of the heart [2]. Since the contrast medium infused into the IVC would not naturally reflux into the heart chamber, chest compression should be continued while injecting the contrast medium.
In our experience, perfusion of the arterial route was sometimes considered insufficient after the contrast medium had passed through the RA, RV, or PA. In such cases, 200 or fewer additional chest compressions were done to generate further circulation. We also found out that when the total number of chest compressions exceeded 400, the image contrast degraded because of greater diffusion of the contrast medium in the body, possibly obscuring intravascular CT values. It is not clear whether the amounts injected, concentrations, flow rates of the contrast medium, or the number of chest compressions we performed were optimal for resuscitation PMCTA. Although we surmise that increased intravascular CT values would be obtained with greater amounts and concentrations of the contrast medium, optimum imaging conditions should be further investigated. A recently reported resuscitation PMCTA method based on injection of a contrast medium followed by saline water injection (chasing) from a catheter retained in the internal carotid artery is known to provide better delineation of the aorta, coronary artery, and PA than injection from the venous route [11].
Compared with PMCTA in Western countries, Japanese resuscitation PMCTA has the following four benefits in spite of the simplicity of the method:
-
1.
Since a CT scan can be performed immediately after death, there is little risk of extravasation of the contrast medium caused by increased permeability of the vascular wall, which occurs several hours after death. In our experience, such extravasation did not occur within a 3-h period after death.
-
2.
Invasiveness of the cadaver is minimal, as only approximately 2 min of chest compression are performed after death.
-
3.
Resuscitation PMCTA revealing a filling defect in the arteries and veins is interpreted as thromboembolism and not as postmortem blood clotting because large amounts of plasminogen activator secreted from the vascular endothelium increase blood fluidity in cases of sudden death.
-
4.
Resuscitation PMCTA can be simply and quickly done in clinical CT examination rooms of ordinary hospitals during working time.
In conclusion, resuscitation PMCTA is a relatively simple, nearly noninvasive, effective procedure as an addition to conventional PMCT for detection of vascular disease-related causes of death, allowing detailed evaluation of organ damage caused by trauma in deceased patients brought into an ER in a state of CPA.
3 Case Reports and Figures
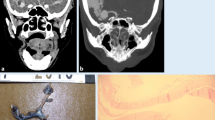
3.1 Case 1: Aortic Dissection
An axial image of noncontrast PMCT at the upper mediastinal level shows bilateral diffuse pulmonary edema (Fig. 9.1a, arrows) and mediastinal hematoma (Fig. 9.1a, arrowheads). An axial image of resuscitation PMCTA at the same level of Fig. 9.1a clearly delineates the intimal flap of the aorta (Fig. 9.1b, arrows), indicating aortic dissection and extravasation of contrast medium into the mediastinal hematoma (Fig. 9.1b, arrowheads). Coronal reconstruction of PMCTA delineates the starting point (entry) of the aortic dissection (Fig. 9.1c, arrow) and dissection in the bilateral common carotid arteries (Fig. 9.1c, arrowheads). Three-dimensional VR (volume rendering) reconstruction of the PMCTA delineates both the coronary arteries (Fig. 9.2a, arrows) and the pulmonary arteries (Fig. 9.2b, arrow).
(a), Bilateral diffuse pulmonary edema (arrows) and mediastinal hematoma (arrowheads). (b), Intimal flap of the aorta (arrows), indicating aortic dissection and extravasation of contrast medium into the mediastinal hematoma (arrowheads). (c), The starting point (entry) of the aortic dissection (arrow) and dissection in the bilateral common carotid arteries (arrowheads)
3.2 Case 2: Pulmonary and Deep Vein Thromboembolism
An axial image of noncontrast PMCT at the level of the carina shows that the diameter of the PA measured at the hilum is greater than that of the mediastinum, suggesting a PA thromboembolism (Fig. 9.3a, arrow). An image after resuscitation PMCTA at the same level of Fig. 9.3a clearly delineates a filling defect in the pulmonary artery, indicating thromboembolism (Fig. 9.3b, arrow). PMCTA also delineates a non–contrast-enhanced aorta (Fig. 9.3b, arrowhead), because pulmonary artery thromboemboli hindered the passage of the contrast medium to the left side of the heart. PMCTA at the level of the sacrum delineates a contrast-enhanced left common iliac vein (Fig. 9.4a, arrow) and thromboemboli in the right common iliac vein (Fig. 9.4b, arrowhead). Reflux of the contrast medium to the venous system enables detection of deep vein thromboembolism.
Resuscitation PMCTA demonstrating a filling defect in the pulmonary artery is interpreted as thromboembolism and not as blood clots occurring after death because a large amount of plasminogen activator secreted from the vascular endothelium increases blood fluidity in cases of sudden death. Additionally, the short postmortem delay in resuscitation PMCT may be one of the reasons for the absence of postmortem clotting.
(a), The diameter of the PA measured at the hilum is greater than that of the mediastinum, suggesting a PA thromboembolism (arrow). (b), A filling defect in the pulmonary artery, indicating thromboembolism (arrow). PMCTA also delineates a non–contrast-enhanced aorta (arrowhead), because pulmonary artery thromboemboli hindered the passage of the contrast medium to the left side of the heart
3.3 Case 3: Multiple Traumatic Injuries
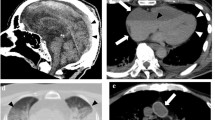
An axial image of non–contrast-enhanced PMCT at the level of the upper abdomen shows free liquid (Figs. 9.5a, b, arrows) and a hematoma around the left kidney (Fig. 9.5b, arrowheads); however, it is difficult to evaluate the extent of the hemorrhage. Images reconstructed after resuscitation PMCTA at the same level of Figs 9.5a, b clearly delineate the contrast-enhanced free liquid (Figs. 9.5c, d, arrows) and extravasation of the contrast medium in the left retroperitoneal space (Fig. 9.5d, arrowheads) indicating both peritoneal and retroperitoneal hemorrhage.
3.4 Case 4: Multiple Traumatic Injuries
Compared with axial non–contrast-enhanced PMCT at the level of the mandible (Fig. 9.6a) and clavicle (Fig. 9.6b), axial images after resuscitation PMCTA at the same level as Figs. 9.6a, b show reflux of contrast medium into the subcutaneous tissue of the neck near the injection point and the vein of the right upper arm (Figs. 9.6c, d, arrows). Axial reconstructions after resuscitation PMCTA at the level of the upper abdomen (Fig. 9.7a) and pelvis (Fig. 9.7b) show reflux to the inferior vena cava, hepatic veins (Fig. 9.7a, arrows), and right iliac vein (Fig. 9.7b, arrow).
In many traumatic cases in which chest compression is not effective, e.g., in the presence of multiple rib fractures and significant loss of blood volume caused by bleeding, contrast enhancement is inadequate because of the lack of effective perfusion of the contrast media in the body; conversely, reflux to the veins increases.
3.5 Case 5: Multiple Traumatic Injuries
An axial image of non–contrast-enhanced PMCT at the level of the upper abdomen shows liquid in the right pleural space (Fig. 9.8a, arrows) and free liquid in the peritoneal cavity on the left side (Fig. 9.8a, arrowhead). Images after resuscitation PMCTA at the same level as Fig. 9.8 .a clearly delineate the position of contrast agent in the right pleural space (Fig. 9.8b, arrows), a contrast medium reflux into the hepatic veins (Fig. 9.8b, arrowheads), as well as extravasation of the contrast medium in the right lobe of the liver (Fig. 9.8b, long arrow) indicating hepatic injury, although the contrast enhancement of the arterial route was inadequate.
(a), Liquid in the right pleural space (arrows) and free liquid in the peritoneal cavity on the left side (arrowhead). Contrast agent in the right pleural space (b, arrows), a contrast medium reflux into the hepatic veins (b, arrowheads), and extravasation of the contrast medium in the right lobe of the liver (b, long arrow)
References
Okuda T, Shiotani S, Sakamoto N, Kobayashi T. Background and current status of postmortem imaging in Japan: short history of “Autopsy imaging (Ai)”. Forensic Sci Int. 2013;225:3–8.
Morgan B, Sakamoto N, Shiotani S, Grabher S. Postmortem computed tomography (PMCT) scanning with angiography (PMCTA): a description of three distinct methods. In: Rutty GN, editor. Essentials of autopsy practice 1. London: Springer; 2014. p. 1–21.
Grabherr S, Djonov V, Yen K, Thali MJ, Dirnhofer R. Postmortem angiography: review of former and current methods. Am J Roentgenol. 2007;188:832–8.
Grabherr S, Dirnhofer R, Jakowski C, Thali MJ. Postmortem angiography. In: Thali MJ, Dirnhofer R, Vock P, editors. The Virtopsy approach. Boca Raton: CRC Press; 2009. p. 443–74.
Saunders SL, Morgan B, Raj V, Robinson CE, Rutty GN. Targeted post-mortem computed tomography cardiac angiography: proof of concept. Int J Legal Med. 2011;125:609–16.
Iizuka K, Sakamoto M, Kawasaki H, Miyoshi T, Komatsuzaki A, Kikuchi S. Examination of the usefulness of the contrast-enhanced postmortem CT imaging diagnosis. Innervision. 2009;24:89–92. (in Japanese).
Sakamoto N, Senoo S, Kamimura Y, Uemura K. Cardiopulmonary arrest on arrival case which underwent contrast-enhanced postmortem CT. J Jpn Assoc for Acute Med. 2009;30:114–5 (in Japanese).
Iizuka K, Sakamoto N, Shiotani S, Komatsuzaki A. Feasibility of resuscitation contrast-enhanced postmortem computed tomography using cardiopulmonary resuscitation technique with chest compression immediately after death. SpringerPlus. 2013;2:663.
Sakamoto T, Sakuragouchi H. Usefulness of contrast-enhanced CT autopsy imaging for diagnosis of cardiovascular disease in cases with sudden death. Eur Congr Radio. 2012. doi:10.1594/ecr2012/C-0618. Scientific Exhibit C-0618.
Jackson RE, Freeman SB. Hemodynamics of cardiac massage. Emerg Med Clin North Am. 1983;1:501–13.
Sakamoto T. Contrast-enhanced cardiac postmortem computed tomography. Innervision. 2014;29:77–80 (in Japanese).
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Sakamoto, N. (2016). Postmortem Computed Tomography Angiography Using Cardiopulmonary Resuscitation Technique: Contrast Media Injection with Chest Compression Immediately After Death. In: Grabherr, S., Grimm, J., Heinemann, A. (eds) Atlas of Postmortem Angiography. Springer, Cham. https://doi.org/10.1007/978-3-319-28537-5_9
Download citation
DOI: https://doi.org/10.1007/978-3-319-28537-5_9
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-28535-1
Online ISBN: 978-3-319-28537-5
eBook Packages: MedicineMedicine (R0)