Abstract
With the recognition that the 5-hydroxytryptamine receptor was important in mediating cisplatin-induced emesis, work at several pharmaceutical companies focused on creating drugs that interfered with serotonin binding utilizing a variety of medicinal chemistry strategies. The first-generation 5-hydroxytryptamine receptor antagonists (5-HT3 RAs) ondansetron, granisetron, tropisetron, and dolasetron were structurally similar and showed activity in preventing chemotherapy-induced nausea and vomiting. However, complete response during the acute phase after cisplatin was achieved in only 50–70 % of patients and was substantially less effective in the delayed phase for control of both emesis and nausea. The first-generation 5-HT3 RAs do not improve control of delayed CINV over dexamethasone alone [1], nor does prolonged administration provide much additional benefit [2]. In addition, the first-generation 5-HT3 RAs were therapeutically equivalent with several large trials comparing these drugs to one another demonstrating similar efficacy [3, 4]. A plateau in 5-HT3 RA activity had been reached. Efforts persisted to find potentially more active agents based on the understanding of the central importance of this specific serotonin receptor in ameliorating chemotherapy-induced emesis.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Complete Response Rate
- Moderately Emetogenic Chemotherapy
- Palonosetron Group
- CINV Prophylaxis
- Moderately Emetogenic Chemotherapy Regimen
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
With the recognition that the 5-hydroxytryptamine receptor was important in mediating cisplatin-induced emesis, work at several pharmaceutical companies focused on creating drugs that interfered with serotonin binding utilizing a variety of medicinal chemistry strategies. The first-generation 5-hydroxytryptamine receptor antagonists (5-HT3 RAs) ondansetron, granisetron, tropisetron, and dolasetron were structurally similar and showed activity in preventing chemotherapy-induced nausea and vomiting. However, complete response during the acute phase after cisplatin was achieved in only 50–70 % of patients and was substantially less effective in the delayed phase for control of both emesis and nausea. The first-generation 5-HT3 RAs do not improve control of delayed CINV over dexamethasone alone [1], nor does prolonged administration provide much additional benefit [2]. In addition, the first-generation 5-HT3 RAs were therapeutically equivalent with several large trials comparing these drugs to one another demonstrating similar efficacy [3, 4]. A plateau in 5-HT3 RA activity had been reached. Efforts persisted to find potentially more active agents based on the understanding of the central importance of this specific serotonin receptor in ameliorating chemotherapy-induced emesis.
4.1 Development of Palonosetron
In 1993 researchers at Syntex Research in Palo Alto, California, created a new class of 5-HT3 RAs [5] by making various substitutions to the chemical structure of the first-generation 5-HT3 RAs and exploring their interactions with the 5-HT3 receptor. The highest-affinity compound, consisting chemically of a conformationally restrained alkano-bridged quinolone, was termed palonosetron, named for the place of discovery. Most 5-HT3 RAs incorporate a three substituted indole resembling serotonin, whereas palonosetron is a fixed tricyclic ring attached to an isoquinolone moiety yielding a substantially different chemical structure (Fig. 4.1).
Palonosetron displays several pharmacologic characteristics which differ from other first-generation 5-HT3 RAs which may account for its clinical distinction. The binding affinity of palonosetron is 2,500-fold higher than that of serotonin [6]. It has a much higher affinity constant (PK1 = 10.45) for the 5-HT3 receptor than the first-generation agents which are at least tenfold lower [7, 8]. The plasma half-life of palonosetron is approximately 40 h, while the other first-generation 5-HT3 receptor antagonist’s half-life ranges from 5 to 12 h [9, 10]. It is excreted predominantly in the urine, with much of the parent compound excreted unmetabolized in contrast to ondansetron which is heavily metabolized [11].
In addition to these pharmacokinetic differences, palonosetron displays qualitative and quantitative biologic and physiologic differences from the other agents. Using tritium-labeled palonosetron, granisetron, and ondansetron, Rojas et al. [12] demonstrated that palonosetron acts as an allosteric antagonist with positive cooperativity. Palonosetron binds to additional sites in the 5-HT3 receptor besides the ones that bind ondansetron or granisetron inducing a conformational change. Additionally, receptor-associated palonosetron is retained in cell culture experiments after prolonged dilution and washings suggesting that the bound palonosetron is internalized [13].
Support for a functional consequence of allosteric binding comes from experiments demonstrating that granisetron and ondansetron as well as palonosetron inhibit calcium iron influx through the serotonin receptor. Calcium influx is the normal physiologic effect representative of serotonin receptor-triggered signaling when cells are preincubated with granisetron or ondansetron and then rinsed multiple times to remove any trace of the drug, they recover the ability to respond to serotonin. In contrast, when palonosetron is preincubated and cells are washed, interference with calcium influx is retained. These effects were not seen when ondansetron was used as the binding agent to the 5-HT3 receptor and was minimal with granisetron. Long-term calcium influx inhibition may represent one reason why palonosetron is a more effective drug than the first-generation agents.
In further experiments, the same group demonstrated conclusive evidence of receptor internalization when cells were exposed to palonosetron but minimal internalization with granisetron and none with ondansetron [14]. The palonosetron-receptor complex remains internalized for at least 25 h after exposure to palonosetron, indicating that it interferes with receptor exocytosis, in contrast to serotonin where exocytosis and renewal of the cell membrane-associated receptor occur [15]. Overall, the palonosetron-5-HT3 interaction leads to reduced receptor density at the cell surface and may be an additional explanation for the prolonged inhibition of receptor function.
An alternative hypothesis to explain the prolonged effect of palonosetron was proposed by another group of investigators who showed that palonosetron induced a long-term inhibition of the number of available 5-HT3 receptor-binding sites due to slow disassociation from the receptor [16]. Palonosetron did not actually reduce cell surface expression of 5-HT3 receptors and did not affect the rate of receptor endocytosis in these series of experiments. The investigators proposed that palonosetron works by pseudo-irreversible interactions with the 5-HT3 receptors rather than receptor-ligand internalization.
Cross talk between NK1 and 5-HT3 receptor signaling pathways has been reported by several different groups of investigators [17–19]. NK1 antagonists block vagal afferent activation by substance P, and 5-HT3 receptor antagonists block vagal afferent activation by serotonin. This cross talk raises the possibility that palonosetron’s unique efficacy as a 5-HT3 receptor antagonist may be in part due to differential inhibition of the cross talk. In both in vitro and in vivo experiments, palonosetron inhibited NK1 receptor activation from substance P, a potent NK1 agonist [13]. This inhibition was dose dependent and was not seen in parallel experiments with granisetron or ondansetron. Taken together, palonosetron is a structurally unique, pharmacologically distinct agent with various different properties from the first-generation 5-HT3 RAs which underlie its clinical differentiation (Table 4.1).
Palonosetron’s interaction with NK1 was further evaluated experimentally using the potent NK1 antagonist netupitant [20]. Palonosetron exhibited a synergistic effect on inhibition of the substance P response in the presence of netupitant. The effect occurred using concentrations of each receptor antagonist below the threshold of inhibition of the substance P response and also concentrations where maximal inhibition of the substance P response was observed suggesting that in vivo the effect was clinically relevant.
Palonosetron does not inhibit or induce cytochrome P450 isoenzymes at clinically relative concentrations and has a low potential for drug interactions. Its route of excretion is equally contributed by renal and hepatic function [9, 11]. Total body clearance of palonosetron is not significantly affected by gender, age, hepatic impairment, renal impairment, or concomitant medications [21]. Palonosetron is physically and chemically stable in common infusion solutions in PVC bags and is stable when administered with dexamethasone in syringes and PVC bags.
4.2 Safety
Palonosetron exhibits the same class-related adverse affects as the first-generation 5-HT3 RAs. In a meta-analysis of safety signals [22], there was no statistical difference between palonosetron and other agents in rates of constipation, headache, and diarrhea, the most common treatment-emergent adverse events. Dizziness was statistically less common in patients receiving palonosetron, OR 2.15, 95 % CI 1.05–4.41, p = 0.04.
Prolongation of the QTc interval has been recognized as a toxicity of some of the first-generation antagonists. Palonosetron has been carefully evaluated for cardiac effects in cancer patients. Several groups have reported no significant difference in a variety of electrocardiographic parameters, including the QTc interval [23–25]. Three RCTs of palonosetron vs. other 5-HT3 RAs included in the meta-analysis demonstrated minimal and significantly less mean QTc interval prolongation for palonosetron, p = 0.002 [22].
4.3 Clinical Development of Palonosetron
A phase 2 dose-ranging study was performed with weight-based single IV dosing [26]. Complete response rates in the 40–50 % range were observed with doses ranging from 3 to 90 mcg/kg. Pharmacokinetic studies revealed a prolonged plasma half-life of approximately 40 h. Based on this trial, dose selection for the phase 3 trials was selected at fixed doses of 0.25 mg (approximately 3 mcg/kg) and 0.75 mg (approximately 10 mcg/kg).
Palonosetron was compared to the first-generation 5-HT3 RAs in two multicentered multinational randomized double-blind phase 3 studies with identical study designs utilizing moderately emetogenic chemotherapy (MEC) including anthracyclines and cyclophosphamide [27, 28]. Patients received a single IV dose of palonosetron, either 0.25 mg or 0.75 mg intravenously, or ondansetron 32 mg IV as the active comparator in study 1 or dolasetron 100 mg IV in study 2. The primary endpoint for each of these trials was complete response (CR), defined as no emesis and no use of rescue medication, during the acute phase lasting 0–24 h from chemotherapy. Secondary endpoints included complete response and complete control (CC), defined as no emesis, no use of rescue medications, and no significant nausea in the delayed phase, from 24 to 120 h after chemotherapy. In the MEC-1 trial about half of the patients had breast cancer and two-thirds received cyclophosphamide with half also receiving anthracyclines [27]. The acute phase CR rate was 81 % for palonosetron 0.25 mg compared to 69 % for ondansetron, and the delayed CR rate was 75 % for palonosetron vs. 55 % for ondansetron both endpoints statistically significant. The overall phase CR rates for palonosetron were 69 % vs. 50 %, with all endpoints statistically significant. Complete control was improved in the delayed and overall phases, and number of emetic episodes was significantly reduced with superiority for palonosetron as well. Treatment-related adverse events were similar across arms: approximately 5 % of patients in both palonosetron and ondansetron arms experienced headaches, 1.6–3.2 % had constipation, and a few patients in each arm experienced dizziness.
The MEC-2 trial had an identical design except the active comparator was dolasetron [28]. Additional prophylactic corticosteroids were permitted in this study, but only 5.4 % of patients received such in a balanced fashion. In MEC-2, two-thirds of patients had breast cancer and half received AC. Complete response was 63.0 % vs. 52.9 % in the acute phase, 54.0 % vs. 38.7 % in the delayed phase, both statistically significant and also significant for the overall phase, 46.0 % vs. 34.0 % for palonosetron 0.25 mg vs. dolasetron, respectively. Significantly improved CC rate in the delayed phase and overall 5-day period study were also observed. Suppression of all emesis was statistically significant superior at all time points for palonosetron vs. dolasetron. Toxicity was similar across arms, but in MEC-2 more headache, 14.6–16.5 %, and constipation, 6.2–9.2 %, were reported. A pooled analysis of the two MEC studies [29] revealed 72 % complete response rate for palonosetron 0.25 mg compared to 60.6 % for the first-generation comparator, 64.0 % vs. 46.8 % in delayed phase and 57.7 % vs. 42.0 % overall, all statistically significant at p < 0.025.
The highly emetogenic (HEC) trial compared palonosetron at both doses of 0.25 mg and 0.75 mg to ondansetron 32 mg IV as the active comparator [30]. Two-thirds of patients in this study received corticosteroids in addition to the 5-HT3 RA. The majority of patients received cisplatin chemotherapy at >60 mg/m2. Overall, neither dose of palonosetron achieved a statistically significantly higher delayed complete response rate than ondansetron, but numerically a slight advantage was seen for both doses. For patients receiving concomitant dexamethasone on day 1, both delayed and acute CR rates were significantly better for palonosetron 0.25 mg. Delayed and overall emesis rates were also significantly better for palonosetron.
A study conducted by Saito et al. in Japan [31] compared palonosetron at the 0.75 mg dose plus dexamethasone to granisetron plus dexamethasone with co-primary endpoints of noninferiority of CR rates during the acute phase and superiority during the delayed phase. Patients received anthracycline and cyclophosphamide (43 % of participants) or cisplatin-based regimens (57 %). The large majority of patients were chemotherapy naïve. In this study of 1,114 patients, acute CR rates were nearly identical, 75.3 % for palonosetron and 73.3 % for granisetron, statistically noninferior, while delayed CR rate was 56.8 % for palonosetron compared to 44.5 % for granisetron (p < 0.0001). Overall CR rates were superior as well 51.5 % vs. 40.4 % for palonosetron vs. granisetron, respectively (p = 0.0001). Prespecified AC and cisplatin subsets showed similar, significant improvement with palonosetron similar to the overall study population. Nausea and emesis control was also better during the delayed phase in the palonosetron arm. Adverse events were comparable to the US/EU registrational trials in MEC. Repeat cycle analysis for the HEC trial demonstrated control maintained through four observed cycles. Similar results were reported in follow-up trials of HEC [32] and MEC [33].
Meta-analyses have been conducted for all of the randomized trials to compare the 0.75 mg and 0.25 mg doses. Therapeutic efficacy is statistically and clinically equivalent [74]. Therefore, the lowest fully effective dose, 0.25 mg IV, which is also the approved dose in US/EU, is preferred [34]. Based on the results of the phase 3 trials, palonosetron was approved by various regulatory agencies for use as prophylaxis for CINV. The current US FDA label states it palonosetron is indicated for the prevention of acute and delayed nausea and vomiting associated with initial and repeat course of both MEC and HEC in adults [21].
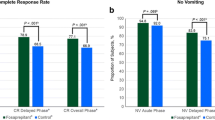
A patient level systematic review aggregated the data from four phase 3 studies of palonosetron + dexamethasone compared to first-generation 5-HT3 RAs for patients receiving HEC or MEC [75]. Palonosetron showed higher CR rates in pooled dose analysis during the delayed phase (P < 0.0001) an overall phase, p = 0.0001 but not the acute phase p = 0.091 with similar results seen for complete control (Fig. 4.2). Results for control of emesis and nausea by severity are shown in Fig. 4.3.
(a) Comparison of palonosetron to other 5-HT3 RAs, complete response = no emetic episodes and no usage of rescue medication, p < 0.0001 palonosetron vs. other 5-HT3 RAs. (b) Complete control = no emetic episodes, no usage of rescue medication, and no more than mild nausea, p < 0.0001 palonosetron vs. other 5-HT3 RAs [75]
(a) Episodes of emesis in the acute, delayed, and overall postchemotherapy phases. PALO palonesetron, other 5-HT 3 RAs, (ondansetron, dolasetron, and granisetron), *p = 0.0066; palonosetron vs. other 5-HT 3 RAs; +p <0.0001 palonosetron vs. other 5-HT3 RAs. (b) Severity of nausea in the acute, delayed and overall postchemotherapy phases. PALO palonesetron, other 5-HT3 RAs (ondansetron, dolasetron, and granisetron); *p=0.0002 palonosetron vs. other 5-HT 3 RAs; +p =0.0112 palonosetron vs. other 5-HT 3 RAs. [75]
4.4 Alternative Formulations
An oral form of palonosetron has also been developed and compared in a prospective, randomized dose finding study to the IV formulation. Oral palonosetron was tested at doses ranging from 0.25 to 0.75 mg, while the comparative was 0.25 mg IV following MEC [35]. The study also randomized patients to receive concurrent dexamethasone or not. While the CR rates in all arms were similar numerically, the 0.5 mg PO dose was best and most comparable to the IV dosing in the delayed and overall phases. The 0.5 mg PO dose also yielded the best results for controlling emesis and nausea. The frequency and severity of all adverse events were similar for the oral doses and the IV dose. This study established comparability between oral palonosetron at 0.50 mg and the IV formulation at 0.25 mg IV. In addition, there was no evidence for a dose response for the oral formulation within the ranges tested, paralleling the results with the IV formulation.A subsequent randomized trial in cisplatin-based HEC compared the 0.5 mg PO dose with 0.25 mg IV [36]. Noninferiority of oral palonosetron was demonstrated in the acute phase with CR rates of 89 % for oral and 86 % for IV. Treatment-related adverse events were numerically less for the oral formulation. Together, these trials have established oral palonosetron 0.5 mg PO as therapeutically equivalent to the IV formulation of the drug.
Additionally, subcutaneous palonosetron has been tested vs. IV in a small group of patients receiving cisplatin in a cross-over design [37]. The PK parameters were similar for the subcutaneous formulation for area under the curve although Cmax was lower. This method of administration might be useful in certain circumstances.
4.5 Multiple-Day Chemotherapy
The best way to utilize palonosetron in the setting of multiple-day chemotherapy has been the subject of some controversy. NCCN guidelines recommend a single dose of palonosetron at the beginning of a 3-day chemotherapy regimen as an alternative to multiple daily doses of other first-generation 5-HT3 receptor antagonists [38]. The database supporting any given alternative schedule for palonosetron is scant, as few randomized trials have been performed [39]. A small pilot trial on palonosetron on days 1, 3, and 5 plus dexamethasone in men receiving 5-day cisplatin-based chemotherapy showed good control during the period of chemotherapy and for 3 days subsequently [40]. A study of palonosetron on day 1 of multiple dosing chemotherapy for hematologic malignancies showed better control compared to a retrospective review of patients treated with ondansetron [41]. Additionally in patients who experienced delayed CINV after multiple-day chemotherapy, there was better response to an additional dose of palonosetron.
In patients receiving high-dose chemotherapy, including both myeloablative and nonmyeloablative regimens over a multiple-day cycle, palonosetron and dexamethasone on day 1 was followed by dexamethasone daily and palonosetron every other day [42]. Overall complete control rates with this regimen were encouraging at 81 % and superior to case-matched controls receiving ondansetron and dexamethasone at 50 %. The use of palonosetron and longer duration of high-dose chemotherapy were independent predictors for an increased likelihood of emesis role.
Other studies [43–46] have also examined palonosetron in the setting of multiday high-dose chemotherapy programs as conditioning prior to stem cell transplant and have shown promising results in pilot trials. The best dose and schedule to utilize palonosetron in this setting remains to be determined. A triple-drug combination of aprepitant, palonosetron, and dexamethasone was more effective than palonosetron plus dexamethasone or ondansetron plus dexamethasone as prophylaxis prior to BEAM chemotherapy in non-Hodgkin’s and Hodgkin’s disease patients undergoing transplant [47].
4.6 Triplet CINV Prophylaxis Regimens including Palonosetron
The addition of an NK1 antagonist to a 5-HT3 RA improves control of delayed CINV [48]. Aprepitant in oral or IV form (fosaprepitant) is an approved NK1 antagonist for this purpose. Aprepitant has been tested along with palonosetron and dexamethasone in a number of trials. A multicenter, single-arm phase II study enrolled patients with MEC including AC demonstrated a 78 % overall CR rate [49] for palonosetron and dexamethasone on day 1 with oral aprepitant on days 1–3. A randomized double-blind multicenter pilot trial randomized patients to palonosetron and aprepitant on day 1 only, palonosetron plus aprepitant on days 1–3, or palonosetron with placebo on days 1–3, each arm receiving dexamethasone on days 1–3 [50]. The arm without aprepitant was terminated for lack of efficacy with an approximate 50 % CR rate. Similar results were seen in the other two arms with aprepitant added on day 1 or for 3 days. A single-day triplet regimen with a dose of aprepitant equivalent to the full 3-day dose showed 76 % CR rate in acute phase and 66 % in delayed phase with no increased toxicity [51].
The triple-drug regimen was utilized in a homogenous population of lung cancer patients receiving HEC with cisplatin [52]. Complete response rates were evaluated for up to six cycles. Palonosetron, aprepitant, and dexamethasone were effective in this population with CR rates ranging from 74 % in cycle 1 to 82 % in the sixth cycle. Emesis was prevented in 90 % of patients across all cycles demonstrating the value of adding the NK1 antagonist to the combination of palonosetron and dexamethasone.
A Japanese trial compared palonosetron 0.75 mg, aprepitant, and dexamethasone to granisetron, aprepitant, and dexamethasone in 827 patients with cisplatin-based HEC [53]. CR rates were identical during the acute phase and statistically significantly higher for the delayed phase: 67 % vs. 59 % for palonosetron vs. granisetron, respectively. The overall CR rate, the primary endpoint for this trial, demonstrated superiority for palonosetron, 66 % vs. 59 %, p = 0.01. The three-drug regimen with aprepitant has also been studied in gynecologic patients receiving HEC, a group that is traditionally difficult to control, with an overall CR rate of 54 % [54]. Palonosetron, aprepitant, and dexamethasone have been evaluated in patients receiving multiple-day chemotherapy in small trials with efficacy established over 3- or 5-day cisplatin regimens with CR rates of 58–90 % [55, 56]. The combination of a 5-HT3 RA and an NK1 RA appears to be cost-effective for the prevention of CINV [57].
Other agents other than NK1 RAs can be substituted to aid protection against delayed nausea and vomiting. Palonosetron has also been studied in combination with olanzapine, an atypical antipsychotic agent with activity against CINV [58]. A randomized trial comparing palonosetron plus dexamethasone plus aprepitant to palonosetron plus dexamethasone plus olanzapine showed no significant difference in CR rates but less nausea in the olanzapine arm in the delayed and overall phases [59]. Toxicity was similar between olanzapine and aprepitant. Olanzapine is therefore an acceptable alternative to an NK1 antagonist for patient in whom a triplet regimen is indicated as noted in the NCCN guidelines.
4.7 Role of Dexamethasone in Delayed Phase after Palonosetron
Given the activity of palonosetron and aprepitant in the delayed phase, studies have evaluated the incremental benefit of dexamethasone given beyond day 1. Dexamethasone is associated with significant side effects when given in antiemetic doses for prolonged periods, including insomnia, gastrointestinal distress, exacerbation of diabetes mellitus, and weight gain. Given the benefit of aprepitant in the delayed phase of CINV, a randomized comparison of dexamethasone vs. aprepitant beyond day 1 in patients receiving AC was conducted [60]. Complete response rates were similar during the acute phase and were identical at 79.5 % during the delayed phase. Significantly less insomnia, heartburn, and improved functional living scores were noted for the aprepitant arm. As such, palonosetron with IV aprepitant and dexamethasone on day 1 or oral aprepitant on days 1–3 appears a reasonable alternative to continuing dexamethasone in patients receiving AC.
Several trials have evaluated palonosetron plus dexamethasone on day 1 vs. continuing dexamethasone on days 2 and 3 in patients receiving AC and/or other MEC regimens. Three noninferiority trials demonstrated no significant difference achieved in each of these studies [61–63]. Therefore, when using palonosetron and dexamethasone as a doublet in non-AC MEC, it appears that the regimen can be limited to a simplified day 1 prophylactic program without sacrificing efficacy but reducing toxicity.
4.8 Cost-Effectiveness of Palonosetron
The cost of cancer care has skyrocketed over the past decade and appears unsustainable [64]. Each new improvement in cancer care, whether therapeutic or supportive in nature, is appropriately subject to scrutiny regarding the cost-effectiveness of the intervention. Standards are slowly emerging to establish value parameters in healthcare with thresholds set for improvement per unit cost.
To this end, the cost of prophylaxis against CINV has been subjected to cost-effectiveness analyses. It is clear that non-prevented CINV events are associated with significant cost to individual patients, families, and the healthcare system as a whole. One retrospective cohort study of over 19,000 adult patients receiving HEC or MEC with CINV prophylaxis examined the cost of uncontrolled CINV [65]. In this cohort 13.8 % of patients had a CINV-associated healthcare visit. Resource utilization included inpatient admissions, unscheduled outpatient visits, and emergency room visits. The mean per-patient CINV-associated cost across all patients treated was $731.00. The mean cost of a CINV event to an individual patient was $5,299.00. Another US study showed a healthcare resource cost in a hospital outpatient setting of $1,855.00 [66]. Despite differences in methodology and cost figures presented by these analyses, there can be no doubt that CINV events are associated with more cost to the healthcare system.
Therefore, strategies that control CINV better are likely to reduce healthcare costs for downstream CINV events. A cost-utility assessment using quality-adjusted life-years (QALY) as the value parameter compared palonosetron to ondansetron + aprepitant in a Monte Carlo simulation model [67]. Incremental cost-effectiveness for the palonosetron regimens was $115,490/QALY for the two-drug regimen, $199,375/QALY for the palonosetron plus aprepitant plus dexamethasone regimen, and $200,525/QALY for the three-drug strategy vs. the ondansetron-based two-drug regimen. These QALYs are in the range of acceptability. Whether QALY is the right metric to use for a supportive care drug that is used broadly is subject to debate; however, even in this context these costs for QALYs are similar to newer biological agents designed for therapeutic intent.
A retrospective analysis of the OptumInsight claims database from years 2005 to 2011, comprised largely of commercially insured members, revealed delayed CINV of 15.6 % across all cycles, utilizing all 5-HT3 receptor antagonists [68]. The lowest rates were demonstrated in patients receiving palonosetron. Over six cycles of chemotherapy per 1,000 patients, ondansetron costs an additional $126,775 and granisetron an additional $169,838 compared to using palonosetron from cycle 1. In a hospital outpatient setting, patients receiving palonosetron had a 14 % decreased rate of CINV per chemotherapy cycle [69].
A systemic review of the literature surrounding cost analyses of CINV in relation to 5-HT3 receptor antagonist utilized was published in 2014 [70]. Thirty-two studies were analyzed including randomized controlled trials. Fourteen reported cost data and 25 studies utilization data. Palonosetron was associated with higher acquisition and treatment costs in the first-generation 5-HT3 RAs. However, healthcare utilization for CINV was reduced in patients receiving palonosetron due to the less need for rescue medication and downstream services such as outpatient visits and emergency room visits. Therefore, the overall costs associated with using palonosetron as the 5-HT3 receptor antagonist of choice appear to be lower than other agents due to reduced service utilization for CINV.
4.9 Pediatric Use
Palonosetron has not been extensively studied in the pediatric population. Retrospective comparison of palonosetron to first-generation 5-HT3 RAs in children showed a significant reduction in emesis on the first 3 days and nausea in the first 4 days in the palonosetron group [71]. A retrospective analysis of children undergoing BMT revealed 43 patients who received palonosetron in a dose of 5 mcg/kg. CINV was controlled in 68 %. A second dose of palonosetron was required on day 5 of the underlying regimen in 17 % of patients [72]. A prospective observational trial examined palonosetron at 5 mcg/kg in children with ALL receiving high-dose methotrexate 5 g/m2. CR was achieved in 84 % in the acute phase and 60 % overall with 90 % free of emesis [73]. Palonosetron is approved in the USA for pediatric use for the prevention of CINV at a dose of 20 mcg/kg [21].
4.10 Meta-Analysis
Several systematic reviews in meta-analysis have been conducted comparing the efficacy and toxicity of the 5-HT3 RAs to one another. Likun reviewed eight RCTs involving 3,592 patients published between 2003 and 2010 [74]. Most trials were noninferiority studies comparing first-generation agents to palonosetron alone. Overall, palonosetron showed superiority for complete response rate with an odds ratio of 0.64 (95 % CI, 0.56–0.74, p < 0.00001). In two studies with HEC comparing palonosetron and dexamethasone to first-generation 5-HT3 RAs plus dexamethasone, there was a trend in favor of palonosetron for acute CINV and statistical benefit for palonosetron in delayed and overall phase. For MEC, palonosetron was superior to prevent acute CINV with an OR of 0.70 (95 % CI, 0.54–0.91, p = 0.008), delayed CINV, and nausea.
The most recent meta-analysis, published in 2014 by Popovic et.al., identified 16 RCTs with over 6,000 patients randomized to palonesetron or other 5-HT3 RAs [22]. Multiple endpoints were analyzed including complete response, complete control, no emesis, no nausea, and no use of rescue medications. Of note, only one of the trials included aprepitant; so this analysis serves as a direct comparison of 5-HT3 RAs to palonosetron alone or as doublet therapy with corticosteroids. Acute, delayed, and overall phases were analyzed separately.
Palonosetron showed statistically significant superiority in the overall phase of CINV for all five endpoints, with odds ratios ranging from 1.51 to 1.54 for each of the endpoints. In subgroup analysis, palonosetron was superior for CR whether or not patients received concomitant corticosteroids. Evaluation by level of emetogenicity demonstrated palonosetron superiority in both HEC and MEC for complete response, complete control, and no emesis endpoints. Palonosetron was also statistically superior in both the acute and delayed phases for CR, CC, no emesis, and no nausea.
MASCC/ESMO guidelines suggest an absolute risk difference of 10 % between antiemetic regimens as a level constituting a clinically relevant result that could prompt guideline revision [76, 77]. Table 4.2 shows the results of the meta-analysis by each of the endpoints for overall, acute, and delayed phases. Of the 15 prespecified endpoints, 3 meet the MASCC/ESMO criteria and 6 approach it. Taken together, the meta-analysis demonstrates that the weight of the evidence from randomized clinical trials conducted over the past decade strongly favors palonosetron as more efficacious in preventing CINV compared to first-generation 5-HT3 RAs.
This study also provided a comprehensive evaluation of safety of the various 5-HT3 RAs. Palonosetron was statistically similar to the other agents with regard to constipation, headache, and diarrhea and safer with regard to dizziness. Evaluation of the three RCTs reporting mean QTc interval change revealed palonosetron was significantly safer than the comparator 5-HT3 RAs with less overall change in QTc interval after drug administration.
4.11 Palonosetron in Antiemetic Guidelines
Multiple guidelines have been created to collate evidence-based recommendations to cancer treatment, including CINV prophylaxis. While the methodology and the frequency of updating vary somewhat, the various organizations use tiered evidence bases +/− expert opinion to generate the recommendations. Recommendations for HEC and MEC from each of these guideline groups are shown in Figs. 4.4 and 4.5. All guidelines recommend palonosetron as the 5-HT3 RA of choice in MEC [38, 77, 78]. In HEC, all guidelines recommend a three drug combination, consisting of a 5-HT3 RA, dexamethasone and an NK1 antagonist (or, in NCCN, olanzapine). Conforming to guideline recommendations improves CINV control; unfortunately adherence remains suboptimal [79, 80]. New strategies to promote guideline usage through educational efforts, and improved awareness of patient experience following chemotherapy by clinicians, possibly using electronic tools, could help this situation [81].
(a) Complete response to NEPA vs. oral palonosetron in cycle 1. Study 1 = dosing-finding study. Study 2 = MEC. (b) Complete response to NEPA vs. other comparators across multiple cycles. Study 2 = MEC. Study 3 = NEPA + dexamethasone vs. palonosetron + aprepitant + dexamethasone [81]
4.12 Netupitant and Palonosetron (NEPA) Fixed Combination
Netupitant is a highly selective NK1 RA which exhibits a high degree of receptor occupancy [81]. In vitro studies have shown a synergistic effect in preventing NK1 response to substance P [20] and an additive effect on NK1 receptor internalization [15]. The plasma half-life of netupitant is approximately 96 h, suggesting that there could be a clinical benefit in the delayed phase of CINV when coadministered with palonosetron. Netupitant is a substrate and moderate inhibitor of CYP3A4. Drugs that are substrates of CYP3A4, such as dexamethasone, should be administered in reduced doses when given with netupitant. Unlike aprepitant, netupitant does not have clinically relevant interactions with oral contraceptives, and no relevant PK interactions are seen when netupitant is co-administered with palonosetron [82].
NEPA has a similar adverse event profile to oral palonosetron given with aprepitant with headache and constipation the most frequently observed toxicities. A comprehensive review of NEPA safety revealed similar treatment-emergent adverse events for NEPA, oral palonosetron alone, or palonosetron and aprepitant combination [83]. No significant effect on QTc interval or impact on other cardiac endpoints was observed across various studies.
NEPA has been evaluated in three trials conducted across a range of emetogenicity in chemotherapy-naïve patients. A phase 2 dose-ranging study compared three different doses of netupitant combined with oral palonosetron to oral palonosetron alone in 694 patients receiving cisplatin-based chemotherapy [84]. The 300 mg dose of netupitant was selected for further evaluation based on numerical superiority in CR rate. Additionally, 300 mg of netupitant was the minimal dose demonstrating NK1 receptor occupancy of >90 % in the brain striatum, the accepted value for efficacy, in a previously performed pharmacodynamic PET study [85]. Overall, NEPA was significantly superior to oral palonosetron for CR in acute, delayed, and overall phases (Fig. 4.4a, Study 1).
A phase 3, multinational double-blind placebo-controlled trial evaluated oral NEPA + dexamethasone compared to oral palonosetron + dexamethasone in 1,455 patients receiving AC-based chemotherapy [86]. Significant improvement in CR rate during the delayed phase of cycle 1, the primary endpoint of the trial, was seen with 77 % of the NEPA group compared to 69 % of the palonosetron group, p = 0.001. Additionally, overall phase CR rate was 74 % vs. 67 %, p = 0.001, and acute phase CR rate was 88 % vs. 85 %, p = 0.047 for NEPA vs. palonosetron, respectively (Fig. 4.4a, Study 2). In other endpoints including delayed and overall phases, no emesis, no significant nausea, and complete protection statistically significant higher rates were also achieved.
A multiple cycle trial in HEC and MEC was conducted primarily to assess cumulative safety [87]. This study included an arm of oral palonosetron and aprepitant compared to NEPA, with both arms receiving dexamethasone according to guidelines. The overall phase CR rate in cycle 1 was 81 % for NEPA and 76 % for palonosetron and aprepitant. No formal statistical comparison was performed. Antiemetic efficacy was maintained well over multiple cycles of therapy, as was also seen in an analysis of the multiple cycle extension study of NEPA during MEC [88] (Fig. 4.4b). NEPA was approved by the US FDA in 2014 for the prevention of acute and delayed nausea and vomiting associated with initial and repeat course of chemotherapy including, but not limited to, highly emetogenic chemotherapy [89]. NEPA is included in NCCN and ASCO guidelines as a prophylactic choice for HEC and MEC.
While NEPA has not yet been subjected to formal cost-effectiveness analyses, the superiority of NEPA over a two-drug regimen on a clinical basis supports the value. The appropriate formal comparison would be NEPA plus dexamethasone to palonosetron with aprepitant and dexamethasone. The fact that NEPA is a fixed combination suggests a potential economic benefit as adherence to fixed dose combinations in general is associated with improved adherence and lower overall treatment cost [57].
4.13 Conclusion
Palonosetron differs chemically, pharmacologically, and, most importantly, clinically from the first-generation 5-HT3 RAs. It confers significant additional protection against delayed nausea and vomiting and in the overall phase of CINV. Multiple prospective randomized trials have demonstrated the benefit of palonosetron over first-generation agents in patients receiving MEC, AC, and HEC regimens. Adding an NK1 antagonist appears to increase the response rate to palonosetron and dexamethasone. Palonosetron is equally effective in IV and oral formulations and is now available in a fixed combination with the NK1 RA netupitant which offers increased convenience and the potential for better adherence.
References
Geling O, Eichler HG (2005) Should 5-hydroxytryptamine-3 receptor antagonists be administered beyond 24 hours after chemotherapy to prevent delayed emesis? Systematic re-evaluation of clinical evidence and drug cost implications. J Clin Oncol Off J Am Soc Clin Oncol 23(6):1289–1294
Hickok JT, Roscoe JA, Morrow GR et al (2005) 5-Hydroxytryptamine-receptor antagonists versus prochlorperazine for control of delayed nausea caused by doxorubicin: a URCC CCOP randomised controlled trial. Lancet Oncol 6(10):765–772
Gralla RJ, Navari RM, Hesketh PJ et al (1998) Single-dose oral granisetron has equivalent antiemetic efficacy to intravenous ondansetron for highly emetogenic cisplatin-based chemotherapy. J Clin Oncol Off J Am Soc Clin Oncol 16(4):1568–1573
Perez EA, Hesketh P, Sandbach J et al (1998) Comparison of single-dose oral granisetron versus intravenous ondansetron in the prevention of nausea and vomiting induced by moderately emetogenic chemotherapy: a multicenter, double-blind, randomized parallel study. J Clin Oncol Off J Am Soc Clin Oncol 16(2):754–760
Clark RD, Miller AB, Berger J et al (1993) 2-(Quinuclidin-3-yl)pyrido[4,3-b]indol-1-ones and isoquinolin-1-ones. Potent conformationally restricted 5-HT3 receptor antagonists. J Med Chem 36(18):2645–2657
Yan D, Schulte MK, Bloom KE, White MM (1999) Structural features of the ligand-binding domain of the serotonin 5HT3 receptor. J Biol Chem 274(9):5537–5541
Eglen RM, Lee CH, Smith WL et al (1995) Pharmacological characterization of RS 25259-197, a novel and selective 5-HT3 receptor antagonist, in vivo. Br J Pharmacol 114(4):860–866
Wong EH, Clark R, Leung E et al (1995) The interaction of RS 25259-197, a potent and selective antagonist, with 5-HT3 receptors, in vitro. Br J Pharmacol 114(4):851–859
Stoltz R, Cyong JC, Shah A, Parisi S (2004) Pharmacokinetic and safety evaluation of palonosetron, a 5-hydroxytryptamine-3 receptor antagonist, in U.S. and Japanese healthy subjects. J Clin Pharmacol 44(5):520–531
Constenla M (2004) 5-HT3 receptor antagonists for prevention of late acute-onset emesis. Ann Pharmacother 38(10):1683–1691
Stoltz R, Parisi S, Shah A, Macciocchi A (2004) Pharmacokinetics, metabolism and excretion of intravenous [l4C]-palonosetron in healthy human volunteers. Biopharm Drug Dispos 25(8):329–337
Rojas C, Stathis M, Thomas AG et al (2008) Palonosetron exhibits unique molecular interactions with the 5-HT3 receptor. Anesth Analg 107(2):469–478
Rojas C, Thomas AG, Alt J et al (2010) Palonosetron triggers 5-HT(3) receptor internalization and causes prolonged inhibition of receptor function. Eur J Pharmacol 626(2–3):193–199
Rojas C, Slusher BS (2012) Pharmacological mechanisms of 5-HT(3) and tachykinin NK(1) receptor antagonism to prevent chemotherapy-induced nausea and vomiting. Eur J Pharmacol 684(1–3):1–7
Rojas C, Raje M, Tsukamoto T, Slusher BS (2014) Molecular mechanisms of 5-HT(3) and NK(1) receptor antagonists in prevention of emesis. Eur J Pharmacol 722:26–37
Hothersall JD, Moffat C, Connolly CN (2013) Prolonged inhibition of 5-HT(3) receptors by palonosetron results from surface receptor inhibition rather than inducing receptor internalization. Br J Pharmacol 169(6):1252–1262
Darmani NA, Chebolu S, Amos B, Alkam T (2011) Synergistic antiemetic interactions between serotonergic 5-HT3 and tachykininergic NK1-receptor antagonists in the least shrew (Cryptotis parva). Pharmacol Biochem Behav 99(4):573–579
Minami M, Endo T, Yokota H et al (2001) Effects of CP-99, 994, a tachykinin NK(1) receptor antagonist, on abdominal afferent vagal activity in ferrets: evidence for involvement of NK(1) and 5-HT(3) receptors. Eur J Pharmacol 428(2):215–220
Hu WP, You XH, Guan BC, Ru LQ, Chen JG, Li ZW (2004) Substance P potentiates 5-HT3 receptor-mediated current in rat trigeminal ganglion neurons. Neurosci Lett 365(2):147–152
Stathis M, Pietra C, Rojas C, Slusher BS (2012) Inhibition of substance P-mediated responses in NG108-15 cells by netupitant and palonosetron exhibit synergistic effects. Eur J Pharmacol 689(1–3):25–30
Aloxi prescribing information (2015) Accessed 12.7.15 www.Aloxi.com/docs/pdf/pi.pdf
Popovic M, Warr DG, Deangelis C et al (2014) Efficacy and safety of palonosetron for the prophylaxis of chemotherapy-induced nausea and vomiting (CINV): a systematic review and meta-analysis of randomized controlled trials. Support Care Cancer Off J Multinatl Assoc Support Care Cancer 22(6):1685–1697
Yavas C, Dogan U, Yavas G, Araz M, Ata OY (2012) Acute effect of palonosetron on electrocardiographic parameters in cancer patients: a prospective study. Support Care Cancer Off J Multinatl Assoc Support Care Cancer 20(10):2343–2347
Gonullu G, Demircan S, Demirag MK, Erdem D, Yucel I (2012) Electrocardiographic findings of palonosetron in cancer patients. Support Care Cancer Off J Multinatl Assoc Support Care Cancer 20(7):1435–1439
Dogan U, Yavas G, Tekinalp M, Yavas C, Ata OY, Ozdemir K (2012) Evaluation of the acute effect of palonosetron on transmural dispersion of myocardial repolarization. Eur Rev Med Pharmacol Sci 16(4):462–468
Eisenberg P, MacKintosh FR, Ritch P, Cornett PA, Macciocchi A (2004) Efficacy, safety and pharmacokinetics of palonosetron in patients receiving highly emetogenic cisplatin-based chemotherapy: a dose-ranging clinical study. Ann Oncol Off J Eur Soc Med Oncol/ESMO 15(2):330–337
Gralla R, Lichinitser M, Van Der Vegt S et al (2003) Palonosetron improves prevention of chemotherapy-induced nausea and vomiting following moderately emetogenic chemotherapy: results of a double-blind randomized phase III trial comparing single doses of palonosetron with ondansetron. Ann Oncol Off J Eur Soc Med Oncol/ESMO 14(10):1570–1577
Eisenberg P, Figueroa-Vadillo J, Zamora R et al (2003) Improved prevention of moderately emetogenic chemotherapy-induced nausea and vomiting with palonosetron, a pharmacologically novel 5-HT3 receptor antagonist: results of a phase III, single-dose trial versus dolasetron. Cancer 98(11):2473–2482
Celio L, Agustoni F, Testa I, Dotti K, de Braud F (2012) Palonosetron: an evidence-based choice in prevention of nausea and vomiting induced by moderately emetogenic chemotherapy. Tumori 98(3):279–286
Aapro MS, Grunberg SM, Manikhas GM et al (2006) A phase III, double-blind, randomized trial of palonosetron compared with ondansetron in preventing chemotherapy-induced nausea and vomiting following highly emetogenic chemotherapy. Ann Oncol Off J Eur Soc Med Oncol/ESMO 17(9):1441–1449
Saito M, Aogi K, Sekine I et al (2009) Palonosetron plus dexamethasone versus granisetron plus dexamethasone for prevention of nausea and vomiting during chemotherapy: a double-blind, double-dummy, randomised, comparative phase III trial. Lancet Oncol 10(2):115–124
Aogi K, Sakai H, Yoshizawa H et al (2012) A phase III open-label study to assess safety and efficacy of palonosetron for preventing chemotherapy-induced nausea and vomiting (CINV) in repeated cycles of emetogenic chemotherapy. Support Care Cancer Off J Multinatl Assoc Support Care Cancer 20(7):1507–1514
Lorusso V, Giampaglia M, Petrucelli L, Saracino V, Perrone T, Gnoni A (2012) Antiemetic efficacy of single-dose palonosetron and dexamethasone in patients receiving multiple cycles of multiple day-based chemotherapy. Support Care Cancer Off J Multinatl Assoc Support Care Cancer 20(12):3241–3246
Kris M, Tonato M, Bria E et al (2011) Consensus recommendations for the presentation of vomiting and nausea following high-emetic-risk chemotherapy. 19: Suppl 1:S25–32.
Boccia R, Grunberg S, Franco-Gonzales E, Rubenstein E, Voisin D (2013) Efficacy of oral palonosetron compared to intravenous palonosetron for the prevention of chemotherapy-induced nausea and vomiting associated with moderately emetogenic chemotherapy: a phase 3 trial. Support Care Cancer Off J Multinatl Assoc Support Care Cancer 21(5):1453–1460
Karthaus M, Tibor C, Lorusso V et al (2015) Efficacy and safety of oral palonesetron compared with IV palonesetron administered with dexamethasone for the prevention of chemotherapy-induced nausea and vomiting (CINV) in patients with solid tumors receiving cisplatin-based highly emetogenic chemotherapy (HEC). Support Care Cancer 23(10):2917–2923.
Sadaba B, del Barrio A, Campanero MA et al (2014) Randomized pharmacokinetic study comparing subcutaneous and intravenous palonosetron in cancer patients treated with platinum based chemotherapy. PLoS One 9(2):e89747
NCCN Antiemesis Guidelines Version 2.2015, Accessed 12.7.15 www.nccn.org/professionals/physician_gls/pdf/antiemesis.pdf
Affronti ML, Bubalo J (2014) Palonosetron in the management of chemotherapy-induced nausea and vomiting in patients receiving multiple-day chemotherapy. Cancer Manag Res 6:329–337
Einhorn LH, Brames MJ, Dreicer R, Nichols CR, Cullen MT Jr, Bubalo J (2007) Palonosetron plus dexamethasone for prevention of chemotherapy-induced nausea and vomiting in patients receiving multiple-day cisplatin chemotherapy for germ cell cancer. Support Care Cancer Off J Multinatl Assoc Support Care Cancer 15(11):1293–1300
Musso M, Scalone R, Bonanno V et al (2009) Palonosetron (Aloxi) and dexamethasone for the prevention of acute and delayed nausea and vomiting in patients receiving multiple-day chemotherapy. Support Care Cancer Off J Multinatl Assoc Support Care Cancer 17(2):205–209
Mirabile A, Celio L, Magni M, Bonizzoni E, Gianni AM, Di Nicola M (2014) Evaluation of an every-other-day palonosetron schedule to control emesis in multiple-day high-dose chemotherapy. Future Oncol 10(16):2569–2578
Musso M, Scalone R, Crescimanno A et al (2010) Palonosetron and dexamethasone for prevention of nausea and vomiting in patients receiving high-dose chemotherapy with auto-SCT. Bone Marrow Transplant 45(1):123–127
Yeh S, Lo W, Hsieh C, Bai L et al (2014) Palonosetron and dexamethasone for the prevention of nausea and vomiting in patients receiving allogeneic hematopoietic stem cell transplantation. Support Care Cancer 22:1199–1206
Chou CW, Chen YK, Yu YB, Chang KH, Hwang WL, Teng CL (2014) Palonosetron versus first-generation 5-hydroxytryptamine type 3 receptor antagonists for emesis prophylaxis in patients undergoing allogeneic hematopoietic stem cell transplantation. Ann Hematol 93(7):1225–1232
Giralt SA, Mangan KF, Maziarz RT et al (2011) Three palonosetron regimens to prevent CINV in myeloma patients receiving multiple-day high-dose melphalan and hematopoietic stem cell transplantation. Ann Oncol Off J Eur Soc Med Oncol/ESMO 22(4):939–946
Pielichowski W, Barzal J, Gawronski K et al (2011) A triple-drug combination to prevent nausea and vomiting following BEAM chemotherapy before autologous hematopoietic stem cell transplantation. Transplant Proc 43(8):3107–3110
Navari RM (2013) Management of chemotherapy-induced nausea and vomiting: focus on newer agents and new uses for older agents. Drugs 73(3):249–262
Grote T, Hajdenberg J, Cartmell A, Ferguson S, Ginkel A, Charu V (2006) Combination therapy for chemotherapy-induced nausea and vomiting in patients receiving moderately emetogenic chemotherapy: palonosetron, dexamethasone, and aprepitant. J Support Oncol 4(8):403–408
Herrington JD, Jaskiewicz AD, Song J (2008) Randomized, placebo-controlled, pilot study evaluating aprepitant single dose plus palonosetron and dexamethasone for the prevention of acute and delayed chemotherapy-induced nausea and vomiting. Cancer 112(9):2080–2087
Grunberg SM, Dugan M, Muss H et al (2009) Effectiveness of a single-day three-drug regimen of dexamethasone, palonosetron, and aprepitant for the prevention of acute and delayed nausea and vomiting caused by moderately emetogenic chemotherapy. Support Care Cancer Off J Multinatl Assoc Support Care Cancer 17(5):589–594
Longo F, Mansueto G, Lapadula V et al (2012) Combination of aprepitant, palonosetron and dexamethasone as antiemetic prophylaxis in lung cancer patients receiving multiple cycles of cisplatin-based chemotherapy. Int J Clin Pract 66(8):753–757
Hashimoto H, Yamanaka T, Shimada Y et al (2013) Palonosetron (PALO) vs. granisetron (GRA) in the triplet regiment with dexamethasone (DEX) and aprepitant (APR) for preventing highly emetogenic chemotherapy (HEC) with cisplatin (CDDP): a randomized double-blind phase III trial. J Clin Oncol. 31(suppl): 9621
Takeshima N, Matoda M, Abe M et al (2014) Efficacy and safety of triple therapy with aprepitant, palonosetron, and dexamethasone for preventing nausea and vomiting induced by cisplatin-based chemotherapy for gynecological cancer: KCOG-G1003 phase II trial. Support Care Cancer Off J Multinatl Assoc Support Care Cancer 22(11):2891–2898
Gao HF, Liang Y, Zhou NN, Zhang DS, Wu HY (2013) Aprepitant plus palonosetron and dexamethasone for prevention of chemotherapy-induced nausea and vomiting in patients receiving multiple-day cisplatin chemotherapy. Intern Med J 43(1):73–76
Hamada S, Hinotsu S, Kawai K et al (2014) Antiemetic efficacy and safety of a combination of palonosetron, aprepitant, and dexamethasone in patients with testicular germ cell tumor receiving 5-day cisplatin-based combination chemotherapy. Support Care Cancer Off J Multinatl Assoc Support Care Cancer 22(8):2161–2166
Schwartzberg L (2014) Addressing the value of novel therapies in chemotherapy-induced nausea and vomiting. Expert Rev Pharmacoecon Outcomes Res 14(6):825–834
Ohzawa H, Miki A, Hozumi Y et al (2015) Comparison between the antiemetic effects of palonosetron and granisetron in breast cancer patients treated with anthracycline-based regimens. Oncol Lett 9(1):119–124
Navari R, Gray S, Kerr A (2011) Olanzapine versus aprepitant for the prevention of chemotherapy-induced nausea and vomiting: a randomized phase III trial. J Support Onc 9(5): 188–195
Roila F, Ruggeri B, Ballatori E, Del Favero A, Tonato M (2014) Aprepitant versus dexamethasone for preventing chemotherapy-induced delayed emesis in patients with breast cancer: a randomized double-blind study. J Clin Oncol Off J Am Soc Clin Oncol 32(2):101–106
Aapro M, Fabi A, Nole F et al (2010) Double-blind, randomised, controlled study of the efficacy and tolerability of palonosetron plus dexamethasone for 1 day with or without dexamethasone on days 2 and 3 in the prevention of nausea and vomiting induced by moderately emetogenic chemotherapy. Ann Oncol Off J Eur Soc Med Oncol/ESMO 21(5):1083–1088
Komatsu Y, Okita K, Yuki S et al (2015) Open-label, randomized, comparative phase III study on effects of reducing steroid use in combination with Palonosetron. Cancer Sci 106(7):891–895
Celio L, Bonizzoni E, Bajetta E, Sebastiani S, Perrone T, Aapro MS (2013) Palonosetron plus single-dose dexamethasone for the prevention of nausea and vomiting in women receiving anthracycline/cyclophosphamide-containing chemotherapy: meta-analysis of individual patient data examining the effect of age on outcome in two phase III trials. Support Care Cancer Off J Multinatl Assoc Support Care Cancer 21(2):565–573
Kantarjian H, Rajkumar SV (2015) Why are cancer drugs so expensive in the United States, and what are the solutions? Mayo Clin Proc 90(4):500–504
Burke TA, Wisniewski T, Ernst FR (2011) Resource utilization and costs associated with chemotherapy-induced nausea and vomiting (CINV) following highly or moderately emetogenic chemotherapy administered in the US outpatient hospital setting. Support Care Cancer Off J Multinatl Assoc Support Care Cancer 19(1):131–140
Craver C, Gayle J, Balu S, Buchner D (2011) Palonosetron versus other 5-HT(3) receptor antagonists for prevention of chemotherapy-induced nausea and vomiting in patients with hematologic malignancies treated with emetogenic chemotherapy in a hospital outpatient setting in the United States. J Med Econ 14(3):341–349
Avritscher EB, Shih YC, Sun CC et al (2010) Cost-utility analysis of palonosetron-based therapy in preventing emesis among breast cancer patients. J Support Oncol 8(6):242–251
Faria C, Li X, Nagl N, McBride A (2014) Outcomes associated with 5-HT3-RA therapy selection in patients with chemotherapy-induced nausea and vomiting: a retrospective claims analysis. Am Health Drug Benefits 7(1):50–58
Balu S, Buchner D, Craver C, Gayle J (2011) Palonosetron versus other 5-HT(3) receptor antagonists for prevention of chemotherapy-induced nausea and vomiting in patients with cancer on chemotherapy in a hospital outpatient setting. Clin Ther 33(4):443–455
Broder MS, Faria C, Powers A, Sunderji J, Cherepanov D (2014) The impact of 5-HT3RA use on cost and utilization in patients with chemotherapy-induced nausea and vomiting: systematic review of the literature. Am Health Drug Benefits 7(3):171–182
Sepulveda-Vildosola AC, Betanzos-Cabrera Y, Lastiri GG et al (2008) Palonosetron hydrochloride is an effective and safe option to prevent chemotherapy-induced nausea and vomiting in children. Arch Med Res 39(6):601–606
Ripaldi M, Parasole R, De Simone G et al (2010) Palonosetron to prevent nausea and vomiting in children undergoing BMT: efficacy and safety. Bone Marrow Transplant 45(11):1663–1664
Nadaraja S, Mamoudou AD, Thomassen H, Wehner PS, Rosthoej S, Schroeder H (2012) Palonosetron for the prevention of nausea and vomiting in children with acute lymphoblastic leukemia treated with high dose methotrexate. Pediatr Blood Cancer 59(5):870–873
Likun Z, Xiang J, Yi B, Xin D, Tao ZL (2011) A systematic review and meta-analysis of intravenous palonosetron in the prevention of chemotherapy-induced nausea and vomiting in adults. Oncologist 16(2):207–216
Schwartzberg L, Barbour S, Morrow G et al (2014) Pooled analysis of Phase III clinical studies of palonesetron versus ondansetron, dolasetron and granisetron in the prevention of chemotherapy-induced nausea and vomiting (CINV). Support Care Cancer 22:469–477
Herrstedt J, Roila F, ESMO guideline working group (2009) Chemotherapy-induced nausea and vomiting: ESMO clinical recommendations for prophylaxis. Ann Oncol 20, suppl 4:156–8
Jordan K, Gralla R, Jahn F, Molassiotis A (2014) International antiemetic guidelines on chemotherapy induced nausea and vomiting (CINV): content and implementation in daily routine practice. Eur J Pharmacol 722:197–202
Hesketh P, Bohlke K, Lyman G et al (2015) Antiemetics: American Society of Clinical Oncology Focused Guideline Update. J Clin Oncol published ahead of print 11.2.15
Aapro M, Molassiotis A, Dicato M et al (2012) The effect of guideline-consistent antiemetic therapy on chemotherapy-induced nausea and vomiting (CINV): the Pan European Emesis Registry (PEER). Ann Oncol Off J Eur Soc Med Oncol/ESMO 23(8):1986–1992
Gilmore JW, Peacock NW, Gu A et al (2014) Antiemetic guideline consistency and incidence of chemotherapy-induced nausea and vomiting in US community oncology practice: INSPIRE Study. J Oncol Pract/ Am Soc Clin Oncol 10(1):68–74
Hesketh P, Aapro M, Jordan K, Schwartzberg L et al (2015) A review of NEPA, a Novel Fixed Antiemetic Combination with the Potential for Enhancing Guideline Adherence and Improving control of chemotherapy-induced nausea and vomiting. Biomed Res Int 2015:651879
Calcagnie S, Lanzarotti C, Rossi G et al (2013) Effect of netupitant, a highly selective NK1 receptor antagonist, on the pharmacokinetics of palonesetron and impact of the fixed dose combination of netupitant and palonesetron when coadministered with ketoconazole, rifampicin, and oral contraceptives. Support Care Cancer 21(10):2879–2887
Aapro M, Gralla R, Karthaus M et al (2014) Multicycle efficacy and safety of NEPA, a fixed-dose antiemetic combination of netupitant and palonesetron, in patients receiving chemotherapy of varying emetogenicity. Ann Oncol 25 (Suppl 4); IV518-IV519, Abst 1484
Hesketh PJ, Rossi G, Rizzi G et al (2014) Efficacy and safety of NEPA, an oral combination of netupitant and palonosetron, for prevention of chemotherapy-induced nausea and vomiting following highly emetogenic chemotherapy: a randomized dose-ranging pivotal study. Ann Oncol Off J Eur Soc Med Oncol/ESMO 25(7):1340–1346
Spinelli T, Calcagnile S, Giuliano C et al (2014) Netupitant PET imaging and ADME studies in humans. J Clin Pharmacol 54(1):97–108
Aapro M, Rugo H, Rossi G et al (2014) A randomized phase III study evaluating the efficacy and safety of NEPA, a fixed-dose combination of netupitant and palonosetron, for prevention of chemotherapy-induced nausea and vomiting following moderately emetogenic chemotherapy. Ann Oncol Off J Eur Soc Med Oncol/ESMO 25(7):1328–1333
Gralla RJ, Bosnjak SM, Hontsa A et al (2014) A phase III study evaluating the safety and efficacy of NEPA, a fixed-dose combination of netupitant and palonosetron, for prevention of chemotherapy-induced nausea and vomiting over repeated cycles of chemotherapy. Ann Oncol Off J Eur Soc Med Oncol/ESMO 25(7):1333–1339
Aapro M, Karthaus M, Schwartzberg L et al (2014) Phase 3 study of NEPA, a fixed dose combination of netupitant and palonosetron for prevention of chemotherapy-induced nausea and vomiting during repeated moderately emetogenic chemotherapy (MEC) cycle. J Clin Oncol, 32:5S, Abstract 9502
Akynzeo prescribing information (2015) Accessed 12.7.15 www.Akynzeo.com/media/Prescribing_Information.pdf
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Schwartzberg, L. (2016). Palonosetron. In: Navari, R. (eds) Management of Chemotherapy-Induced Nausea and Vomiting. Adis, Cham. https://doi.org/10.1007/978-3-319-27016-6_4
Download citation
DOI: https://doi.org/10.1007/978-3-319-27016-6_4
Published:
Publisher Name: Adis, Cham
Print ISBN: 978-3-319-27014-2
Online ISBN: 978-3-319-27016-6
eBook Packages: MedicineMedicine (R0)