Abstract
Cervical cancer is an important cause of morbidity and mortality worldwide, with significant disparities between low- and high-resource settings. Effective preventive measures exist for this devastating disease, including Pap screening and HPV vaccination; however, access to care remains an important barrier. The ED, which is an important safety net for underserved populations, could serve as a site for education and screening for HPV. ED visits are a missed opportunity for preventive health measures including cervical cancer prevention and detection. The potential for HPV vaccination in the ED remains to be seen, given that the focus of ED visits has not been on preventive care for this disease.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Cervical cancer
- Human papillomavirus
- Papanicolaou smear
- HPV vaccine
- Dysplasia
- Herd immunity
- Prophylactic
- Quadrivalent
- Sexually transmitted disease
- Electronic medical records

Background
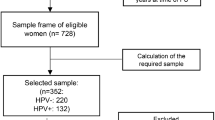
Cervical cancer is the third most commonly diagnosed cancer worldwide, only behind breast cancer and colorectal cancer. There are significant disparities in the incidence of cervical cancer between high- and low-resource settings. Cervical cancer is the second most commonly diagnosed cancer (453,300 women in 2008) compared to the ninth most common (76,500 women in 2008) in developing versus developed countries, respectively [1]. These incidence rates have additional ramifications for public health, as developing countries are less likely to have readily available access to preventive care, including cervical cancer screening and the decreased financial capacity to obtain the human papillomavirus (HPV) vaccine, which is a newly available preventive option [2].
In the United States, there are approximately 12,000 new cases and 4000 deaths due to cervical cancer each year. A 2014 report released by the Centers for Disease Control and Prevention (CDC) noted that 93 % of cervical cancer diagnoses could be prevented through screening and HPV vaccination. Eight million (11 %) US women between the ages of 21 and 65 did not receive cervical cancer screening within the last 5 years [2].
Worldwide, there were 529,800 new cases in 2008, with approximately 85 % of these cases occurring in developing countries, primarily Central and South America, sub-Saharan Africa, Southern Asia, and the Caribbean [1, 3]. Nonetheless, the majority of deaths associated with cervical cancer occur in developing countries—approximately 90 % in 2008. The disparities in new cases and deaths are largely attributed to the lack of screening in low-resource areas, specifically the lack of availability of Papanicolaou (Pap) smear [3].
High-Risk Populations
Globally, women in developing countries are at the highest risk to develop cervical cancer. The burden of cervical cancer in these underserved areas has been attributed to limited resources [1, 2, 4]. Poverty, race and ethnicity (primarily African American and Hispanic), and the inability to obtain preventive care are also linked to areas with high rates of cervical cancer diagnosis [4, 5]. A large proportion of women diagnosed with cervical cancer, approximately 80 % in developing countries, present with advanced stages of the disease [6].
In comparison, in the United States, cervical cancer has one of the highest successful treatment rates of all cancer types, approximately a 91 % survival rate, when diagnosed during the early stages of the disease. However, survival rates drop to 17 % if diagnosed during the more advanced stages of the disease [3]. Low-income women are at the highest risk for cervical cancer diagnosis due to their lack of access to preventive care, including Pap smears. Regions of the United States with higher diagnosis rates are also underserved and stricken with poverty, consistent with regions around the world with the higher diagnosis rates [4]. The incidence of cervical cancer in the United States is highest in African American and Hispanic women, which has been attributed to the population’s lack of screening, which is likely due to diminished access to health care within these groups [5]. Populations at high risk are also less likely to complete follow-up after an abnormal Pap smear result [7].
In a study of male and female patients visiting an emergency department (ED) in New York City, immigrants received less preventive health care when compared to nonimmigrants, even after adjusting for level of income, education, health insurance coverage, language, and length of residence. Limited access to preventive health care leaves these populations at higher risk for illnesses than patients with regular access to health care [8]. In many areas, immigrants are only guaranteed health-care services by emergency medical services; however, some areas offer federally qualified health centers (FQHCs) or public health clinics as alternatives for uninsured or low-income patients. However, there may be limited knowledge of these options. Thus, a large proportion of populations with limited access to care visit the ED for primary care, including their preventive health concerns [8].
Tools for Cervical Cancer Prevention and Detection
Papanicolaou (Pap) Smear
A Pap smear is a laboratory test performed on a sample of cervical cells collected during a pelvic examination and detects abnormal cells associated with cervical cancer [3, 9]. Current recommendations are for women between the ages of 21 and 65 to have a Pap test every 3 years. After the age of 30, it is recommended that women also have an HPV test every 5 years [2]. According to 2010 survey responses, the US Preventive Services Task Force found that 83.0 % of women reported having a Pap smear performed in the previous 3 years. However, only 64.9 % of women with no usual preventive health care and 63.8 % of uninsured women reported having had a Pap test within 3 years [10].
HPV Vaccine
Gardasil, one of the two HPV vaccine options, is a prophylactic, quadrivalent vaccine licensed in 2006 and protects against the four most common HPV strains that cause cervical cancer and genital warts [11]. It is recommended for adolescent girls between the ages of 11 and 12 years old. For females who do not receive the vaccine at that time, the CDC recommends a “catch-up” vaccination for females between the ages of 13 and 26 years old [12]. The CDC also recommends vaccination of males at the ages of 11–12 years old and up to 21 years of age for prevention of anal cancer and genital warts. Vaccination is also recommended for any male that has had sex with another male or men diagnosed with human immunodeficiency virus (HIV) through the age of 26, only if they had not been vaccinated at a younger age [13]. A second option, Cervarix, protects against two of the most common high-risk types [11].
Several types of HPV strains have been associated with cervical cancer. HPV is the most common sexually transmitted disease (STD), with multiple different strains causing approximately 6.2 million new infections annually [12]. Approximately 15 strains of HPV are linked to cervical cancer, with 70 % of cervical cancer diagnoses caused by two strains, types 16 and 18 [1, 3, 14]. Approximately 90 % of HPV infections, primarily low-risk strains, typically clear without medical intervention within a few years of initial infection [3, 11, 14]. The infections that are unable to be eliminated may lead to the formation of lesions and tumors [11].
The number of adolescent girls who have received the HPV vaccine has increased significantly over the past few years. From 2012 to 2013, HPV vaccine coverage, with one or more doses, increased from 53.8 % to 57.3 % in females. For males, coverage with one or more doses increased from 20.8 % to 34.6 %. Of females who received one or more doses of HPV vaccine in 2013, 70.4 % completed the three-dose series compared to 48.3 % of males [15]. Even after HPV vaccination, patients need to be reminded of the necessity for future cancer screening and continued Pap testing.
Prior research has found that women are interested in education surrounding the risk of HPV and cervical cancer. A study employing focus groups of women found differences between the preferred information of women with different demographic information, including age and ethnicities. For instance, younger women preferred more low-risk HPV strain information, specifically the associated symptoms of an infection, whereas older women preferred more information on risks of the high-risk HPV strains commonly associated with cervical cancer [16]. The study participants also expressed confusion over whether they should be concerned following a positive HPV test result, as well as the differences between low-risk and high-risk HPV strains. They also found that women of all ages were aware of the connection between HPV and cervical cancer but overestimated the possibility of a cervical cancer diagnosis following a positive HPV result. This concern and disconnect of information among adult women could be alleviated or improved if more information is provided in a nontraditional way to patients without regular health-care access [16]. Education could be incorporated into the ED waiting room through the use of public health advocates or through additional discharge education materials and referrals for further follow-up.
HPV Vaccination Barriers
After the HPV vaccine was approved, several states attempted to mandate vaccination for girls between the ages of 11 and 12 with varying success. States with success in mandating HPV vaccination incorporated a parental “opt-out” option, but some parents still questioned whether they should vaccinate their children against HPV. Parental concerns included: the possibility of promoting early sexual activity, the use of unsafe sexual practices, and the unknown long-term effects of the vaccine [12, 17].
The majority of parents have been enthusiastic in regard to vaccinating their daughters against STDs [18]. Olshen et al. found that parents who considered their children at risk for HPV infection were more likely to accept vaccination, while parents who did not consider their children to be at immediate risk were more likely to decline the vaccine. Parents also report concern for vaccine administration at a young age, which could possibly condone premature sexual activity and the possibility for an increase in risky behavior [14, 19].
Public health authorities have expressed concerns surrounding HPV transmission in comparison to other diseases with mandated vaccinations for children. Since HPV is only spread through sexual activity, many parents opposed to vaccination question the immediate risk of spreading the disease in a school environment. Many public health authorities have also noted that mandated vaccination would not create herd immunity within the population but would reduce the number of infections [12]. Herd immunity occurs when majority of a population is vaccinated against a specific contagious disease, which leads to protection for the portion of the population unable to receive the vaccines. This is observed in many diseases with vaccines, including influenza, measles, and mumps [18]. The justification for mandatory HPV vaccination is that women will be protected against the high-risk HPV strains, which would decrease the likelihood of future cervical cancer diagnosis as a result of HPV infection [12].
Another potential barrier to HPV vaccination is its cost, which is $300–$900 for the three-dose regimen charged to the patient [11, 12]. This also concerns physicians and pediatricians because acquiring, stocking, and offering the vaccine are costly, and they are unsure they will receive full reimbursement of the total cost for uninsured patients [12]. This creates yet another barrier for high-risk populations because they are typically uninsured or unable to afford their standard health-care needs, let alone an additional three-dose vaccine regimen.
Physician Attitudes Regarding HPV Vaccination
Pediatricians come in contact with the patients and parents requiring HPV and cervical cancer risk education. In a survey, pediatricians noted strategies that might increase vaccination including: insurance coverage, reasonable cost, and affordability for the uninsured and underinsured [20]. Pediatricians responded they were more likely to recommend the vaccine and educate the parents of a female patient rather than male patients on HPV and the connection to cervical cancer. Many studies have found that parental acceptance of HPV vaccination could increase with pediatrician recommendation [20, 21].
Some pediatricians report reluctance to recommend HPV vaccination to younger patients due to their beliefs that these patients have not yet started sexual activity and thus are low risk for HPV infection. Some also report discomfort discussing sexual topics with young patients and the parents [21]. However, studies have found that approximately 28 % of female adolescents entering the ninth grade have initiated sexual activity [22]. Vaccine administration is recommended prior to an individual’s first sexual contact; thus HPV vaccine administration prior to age 14 would provide adequate protection [21]. Having these difficult and potentially uncomfortable conversations may need to occur earlier than previously thought.
Cervical Cancer Prevention and Screening in the ED
Screening
For women lacking regular medical care access, the ED could evaluate the patient’s potential need for preventive care screening . These patients could benefit, not only from education on screening and contraceptive use but also having an initial Pap testing and/or HPV vaccine administration with a referral for follow-up visits and vaccinations [23].
Current standard of care pelvic exams in the ED do not include a Pap smear. Many preventive health measures have not been incorporated into ED standard of care for a variety of reasons, including being outside the scope of urgent or emergent care and due to the potential necessity of multiple follow-up visits after receiving results. However, patient expectations of ED care may differ from standard practice. For instance, a prospective, observational study conducted at an urban ED found that 74 % of women believed a Pap test was performed during their pelvic exam. These patients did not receive education from the physician. On the other hand, 56 % of participating women who received Pap test education from the physician still believed they had a Pap smear completed [9]. They also noted that women who correctly answered what a Pap smear tested for were still under the impression that they had a Pap smear during their ED visit [9].
This leads to a false sense of cervical cancer screening compliance among women. Patients unsure of when Pap smears are collected could potentially inform their physicians that they have completed the necessary screening, when in fact, a standard pelvic examination was performed. If providers ask more specific questions about their patient’s preventive health screening history, they will have the opportunity to educate the patient on specific areas of concern.
Despite recent advances in the screening and prevention of cervical cancer with the development of the HPV vaccine, there remains a significant gap in knowledge of preventable diseases in high-risk populations that frequent the ED for primary care. Studies have shown gaps in knowledge of what Pap smears test for, primarily in known high-risk populations. The limited knowledge has been associated with women opting out of preventive health screenings, underutilization of the necessary exams, and the misperceptions of their health-care needs [9, 24].
A self-administered survey of female ED patients in a Rhode Island hospital found that those who expressed negative opinions about cancer screening and contraceptive measures were more likely to never have had screening or did not use contraceptives. Pap smears had the highest percentage, 46 %, of negative opinions. Survey respondents with negative opinions described Pap smears as “embarrassing” or “painful” [23]. Interestingly, women expressing negative opinions also viewed the screenings as necessary for preventive health [23].
Up to 25 % of women surveyed in a Canadian ED reported that they were overdue for a Pap smear. These women were offered a Pap smear in the ED; however, all women elected for a referral for outpatient care instead. At follow-up, consisting of phone calls at 1, 2, and 3 months following the initial visit, fewer than half of the respondents had received their outpatient Pap smear [25], suggesting that there may be an important role for incorporating cervical cancer screening in the ED. A separate randomized trial of cervical cancer screening in an urgent care setting found that 22 % of women had an abnormal Pap smear result, with only five returning for follow-up [26], demonstrating patient follow-up as a potentially major barrier to recommending routine cervical cancer screening in the ED, as well as time constraints, lack of personnel with appropriate training, and poor linkages to care outside of the ED. Additional research needs to be conducted to determine the best methods for delivery of cervical cancer screening, as well as improving access to care and follow-up for patients seen in the ED.
Incorporating preventive health screening into an ED visit could be beneficial to high-risk populations. For example, patients receiving a pelvic exam in the ED could be offered additional information concerning HPV, Pap smears, and cervical cancer, as well as the option to have a Pap smear performed during the physical exam. Multiple studies have determined the feasibility of Pap tests in the ED and urgent care settings, but follow-up is constantly a limitation in ED [7, 27, 28].
Concerns exist the ability of the ED or urgent care to provide proper follow-up to patients with abnormal Pap smear results, especially in regard to high-risk populations, where incorporating cancer screening and education into ED is most beneficial [26]. This population includes women who are homeless, uninsured, and with limited access to a primary care physician.
Women considered high risk for cervical cancer likely utilize the ED because they are unable to see their PCP, are unsure if their PCP can treat their symptoms, or are uninsured, while others may utilize other sites, such as community health centers, FQHCs, homeless shelters, or mobile vans. These sites are typically unable to provide timely follow-up, so patients requiring follow-up after their initial ED visit typically require a referral to another medical facility [7]. A randomized study at an ED with a large population of high-risk patients evaluated the efficacy of high-intensity follow-up after an abnormal Pap smear result, consisting of multiple follow-up phone calls and case management. They found that 65 % of participants went to a follow-up appointment within 6 months [7]. Interventions that could improve or incorporate high-intensity follow-up in EDs with limited resources should be further evaluated.
A study performed at an urban ED found that cervical cancer screening was more effective when completed during the ED pelvic exam instead of referring the patient to screening at a later time. A high prevalence of abnormal cervical sample results was noted in the study’s population. Of the abnormal results, it was noted that there was a higher prevalence of dysplasia, in this specific ED population, approximately 8 %, in comparison to the 2 % rate observed in populations with access to and compliance with routine screening and medical care [28]. This same study found a higher rate of follow-up, approximately 70 %, after high-intensity follow-up methods, which included: multiple follow-up phone calls, sending mail, home visits, and contacting the patient’s family members [28]. In addition, the quality of the samples was found to be consistent with the hospital’s outpatient offices, and physicians reported minimal difficulty during sample collection [26, 28].
Although cervical cancer screening can be improved by incorporating Pap smears into a standard of care pelvic exam, follow-up will continue to be a barrier for the high-risk population, including the homeless. Evaluation of patient follow-up in this population is necessary, because noncompliance with care following abnormal results leads to loss of the benefits the initial screening process provides [7].
HPV Vaccination
No studies to date have been conducted on HPV vaccination in the ED setting. There is, however, a precedent for potentially offering vaccinations in the ED, given the significant waiting that may occur in the ED [28]. A cross-sectional study focused on patient willingness vaccination by a pharmacist in the ED for influenza found that 41 % (62/149) agreed to be vaccinated. Eighty-seven patients declined vaccination, with 38 (44 %) reporting a perceived low risk for infection [29]. Implementation of decision support tools in the electronic health record may assist urgent care and ED settings in increasing vaccination uptake [30]. Another study found that incorporating immunization protocols enhanced vaccination feasibility for pneumococcus and influenza [31]; however, the challenge is that multiple doses of the vaccine are required for HPV. Implementation of the initial dose of HPV vaccination as standard of care in the ED is beneficial to a large portion of urban ED populations. Ensuring each patient who receives the vaccine is given a referral to the appropriate follow-up care will be essential. This could even be incorporated into the patient’s electronic health record, which may ensure continuation of care after the initial ED visit. Further research should be conducted on the feasibility of offering HPV vaccination or referring patients to outpatient providers from the ED for further vaccination and screening.
When evaluating the feasibility of influenza and pneumococcal vaccination in the ED, barriers consistent with current HPV vaccine administration were found, including: lack of insurance, young age, and low perceived need for vaccine administration [32]. A cross-sectional study performed in an inner-city ED found that vaccinating in the ED gave uninsured patients and adolescent patients access to vaccinations they would otherwise be unable to obtain [32].
When considering vaccine administration to adolescents in the ED, there are some concerns because parents can give inaccurate immunization histories, with some data showing approximately 45 % inaccurate vaccination history given to providers [33]. This provides a potential barrier to the emergency department’s ability to administer required immunizations to their patients. ED access to pediatric electronic medical records (EMRs) could assist and alleviate physician concerns.
Administration of influenza and pneumococcal vaccine to the elderly in the ED has been considered feasible when immunization protocols are in place [31]. Creating and incorporating protocols specific to immunization in the ED could benefit the populations without access to primary medical and preventive care needs [34].
Methods to Promote Immunization in the Emergency Department
Wait times in the ED have continued to increase over the past few decades [35]. Some hospitals have started using these long wait times as an educational opportunity for their patients’ preventive health-care concerns. Some academic centers have utilized medical students, while other areas utilize public health advocates and their nursing staff for education in the waiting room [25, 35]. Furthermore, the information offered in the ED waiting room would not be limited to registered patients, as staff could reach out to all visitors [35].
Conclusion
In summary, cervical cancer is an important cause of morbidity and mortality worldwide. Effective preventive measures exist for this devastating disease; however, access to care remains an important barrier. Early work demonstrated the feasibility of conducting Pap tests in the ED, although follow-up was poor. Administration of HPV vaccine is feasible, although linkage to aftercare is needed for this three-vaccine series. The ED could serve as a site for education and screening for HPV. The potential for vaccination in the ED remains yet to be seen.
References
Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61(2):69–90. doi:10.3322/caac.20107.
CDC Vital Signs. Nov 2014. http://www.cdc.gov/vitalsigns/cervical-cancer/index.html. Accessed 5 Nov 2014.
Global cancer facts & figures. 2nd ed. Atlanta: American Cancer Society; 2011. http://www.cancer.org/research/cancerfactsfigures/globalcancerfactsfigures/global-facts-figures-2nd-ed. Accessed 5 Nov 2014.
Corwin T. Millions of women fail to receive cancer screenings, vaccine. The Augusta Chronicle. 6 Nov 2014. http://chronicle.augusta.com/latest-news/2014-11-05/majority-women-fail-recieve-cancer-screeings-vaccines. Accessed 6 Nov 2014.
Goldie SJ, Kuhn L, Denny L, Pollack A, Wright TC. Policy analysis of cervical cancer screening strategies in low-resource settings. JAMA. 2001;285(24):3107–15. doi:10.1001/jama.285.24.3107.
Cancer health disparities. National Cancer Institute. 11 Mar 2008. http://www.cancer.gov/cancertopics/factsheet/disparities/cancer-health-disparities. Accessed 6 Nov 2014.
Engelstad LP, Stewart SL, Nguyen BH, Bedeian KL, Rubin MM, Pasick RJ, et al. Abnormal pap smear follow-up in a high-risk population. Cancer Epidemiol Biomarkers Prev. 2001;10:1015–20.
Jacobs DH, Tovar JM, Hung OL, Kim M, Ye P, Chiang WK, et al. Behavioral risk factor and preventive health care practice survey of immigrants in the emergency department. Acad Emerg Med. 2002;9(6):599–608. doi:10.1197/aemj.9.6.599.
Lyons MS, Lindsell CJ, Trott AT. Emergency department pelvic examination and pap testing: addressing patient misperceptions. Acad Emerg Med. 2004;11(4):405–8. doi:10.1197/j.aem.2003.10.031.
Centers for Disease Control and Prevention (CDC). Cancer Screening—United States, 2010. MMWR Morb Mortal Wkly Rep. 2012;61(3):41–5.
Matthews KRW, Matsumoto MM. Human papillomavirus vaccine: a public health opportunity for Texas. Policy Brief. Rice University’s Baker Institute for Public Policy. 06 Oct 2014.
Gostin LO, DeAngelis CD. Mandatory HPV vaccination public health vs private wealth. JAMA. 2007;297(17):1921–3. doi:10.1001/jama.297.17.1921.
HPV vaccines. Centers for Disease Control and Prevention. 26 Jan 2015. http://www.cdc.gov/hpv/vaccine.html. Accessed 7 Apr 2015.
HPV and cancer. National Cancer Institute. 15 Mar 2012. http://www.cancer.gov/cancertopics/factsheet/Risk/HPV. Accessed 6 Nov 2014.
Elam-Evans LD, Yankey D, Jeyarajah J, Singleton JA, Curtis R, MacNeil J, et al. National, regional, state, and selected local area vaccination coverage among adolescents aged 13–17 years—United States, 2013. MMWR Morb Mortal Wkly Rep. 2014;63(29):625–33.
Anhang R, Wright TC, Smock L, Goldie SJ. Women’s desired information about human papillomavirus. Cancer. 2004;100(2):315–20. doi:10.1002/cncr.20007.
Olshen E, Woods ER, Austin B, Luskin M, Bauchner H. Parental acceptance of the human papillomavirus vaccine. J Adolesc Health. 2005;37:248–51. doi:10.1016/j.jadohealth.2005.05.016.
Community immunity (“Herd immunity”). NIAID. Vaccines.gov. 27 Nov 2013. http://www.vaccines.gov/basics/protection. Accessed 6 Nov 2014.
Zimet GD, Perkins SM, Sturm LA, Bair RM, Juliar BE, Mays RM. Predictors of STI vaccine acceptability among parents and their adolescent children. J Adolesc Health. 2005;37:179–86. doi:10.1016/j.jadohealth.2005.06.004.
Kahn JA, Zimet GD, Bernstein DI, Riedesel JM, Lan D, Huang B, et al. Pediatricians’ intention to administer human papillomavirus vaccine: the role of practice characteristics, knowledge, and attitudes. J Adolesc Health. 2005;37:502–10. doi:10.1016/j.jadohealth.2005.07.014.
Riedesel JM, Rosenthal SL, Zimet GD, Bernstein DI, Huang B, Lan D, et al. Attitudes about human papillomavirus vaccine among family physicians. J Pediatr Adolesc Gynecol. 2005;18:391–8. doi:10.1016/j.jpag.2005.09.004.
Lo B. HPV vaccine and adolescents’ sexual activity. BMJ. 2006;332:1106–7. doi:10.1136/bmj.332.7550.1106.
Merchant RC, Gee EM, Bock BC, Becker BM, Clark MA. Negative opinions about cancer screening and contraceptive measures by female emergency department patients. J Prim Prev. 2008;29:517–33. doi:10.1007/s10935-008-0154-8.
Merchant RC, Gee EM, Bock BC, Becker BM, Clark MA. Correlates of women’s cancer screening and contraceptive knowledge among female emergency department patients. BMC Womens Health. 2007;7:7. doi:10.1186/1472-6874-7-7.
Cummings GE, Francescutti LH, Predy G, Cummings G. Health promotion and disease prevention in the emergency department: a feasibility study. CJEM. 2006;8(2):100–5. doi:10.1016/j.jpag.2005.09.004.
Batal H, Biggerstaff S, Dunn T, Mehler PS. Cervical cancer screening in the urgent care setting. J Gen Intern Med. 2000;15:389–94. doi:10.1046/j.1525-1497.2000.08001.x.
Mandelblatt J, Freeman H, Winczewski D, Cagney K, Williams S, Trowers R, et al. Implementation of a breast and cervical cancer screening program in a public hospital emergency department. Ann Emerg Med. 1996;28(5):493–8. doi:10.1016/S0196-0644(96)70111-7.
Hogness CG, Engelstad LP, Linck LM, Schorr KA. Cervical cancer screening in an urban emergency department. Ann Emerg Med. 1992;21(8):933–9. doi:10.1016/S0196-0644(05)82931-2.
Cohen V, Jellinek-Cohen SP, Likourezos A, Lum D, Zimmerman DE, Willner MA, et al. Feasibility of a pharmacy-based influenza immunization program in an academic emergency department. Ann Pharmacother. 2013;47(11):1440–7. doi:10.1177/1060028013502456.
Venkat A, Chan-Tompkins NH, Hegde GG, Chuirazzi DM, Hunter R, Szczesiul JM. Feasibility of integrating a clinical decision support tool into an existing computerized physician order entry system to increase seasonal influenza vaccination in the emergency department. Vaccine. 2010;28:6058–64. doi:10.1016/j.vaccine.2010.06.090.
Rodriguez RM, Baraff LJ. Emergency department immunization of the elderly with pneumococcal and influenza vaccines. Ann Emerg Med. 1993;22(11):1729–32. doi:10.1016/S0196-0644(05)81313-7.
Rimple D, Weiss SJ, Brett M, Ernst AA. An emergency department-based vaccination program: overcoming the barriers for adults at high risk for vaccine-preventable diseases. Acad Emerg Med. 2006;13(9):922–30. doi:10.1197/j.aem.2006.04.022.
Olson JJ, Mannenbach MS, Moore BR, Smith VD, Rosekrans JA, Jacobson RM. A reexamination of the feasibility of the administration of routine childhood vaccines in emergency departments in the era of electronic vaccine registries. Pediatr Emerg Care. 2005;21(9):565–7. doi:10.1097/01.pec.0000177192.60784.8b.
Slobodkin D, Kitlas JL, Zielske PG. A test of the feasibility of pneumococcal vaccination in the emergency department. Acad Emerg Med. 1999;6(7):724–7. doi:10.1111/j.1553-2712.1999.tb00443.x.
Llovera I, Ward MF, Ryan JG, LaTouche T, Sama A. A survey of the emergency department population and their interest in preventative health education. Acad Emerg Med. 2003;10(2):155–60. doi:10.1197/aemj.10.2.155.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
May, L., Ware, C. (2016). Cervical Cancer Prevention. In: Todd, K., Thomas, Jr., C. (eds) Oncologic Emergency Medicine. Springer, Cham. https://doi.org/10.1007/978-3-319-26387-8_9
Download citation
DOI: https://doi.org/10.1007/978-3-319-26387-8_9
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-26385-4
Online ISBN: 978-3-319-26387-8
eBook Packages: MedicineMedicine (R0)