Abstract
A 71-year-old female presented to our clinic with a 3-month history of recurrent abdominal pain, nausea, and fatigue. She had a history of coronary artery disease, hypertension, and osteoarthritis. She denied significant alcohol use and was a nonsmoker. She also denied any therapeutic radiation exposure or family history of cancer. On clinical examination, she appeared dehydrated and lethargic but was hemodynamically stable. A right-sided firm, irregular, non-tender mass was palpable in the area of the right thyroid lobe measuring approximately 3 cm by examination.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Recurrent Laryngeal Nerve
- Parathyroid Adenoma
- Parathyroid Carcinoma
- Thyroid Lobe
- Recurrent Abdominal Pain
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Case Study
A 71-year-old female presented to our clinic with a 3-month history of recurrent abdominal pain, nausea, and fatigue. She had a history of coronary artery disease, hypertension, and osteoarthritis. She denied significant alcohol use and was a nonsmoker. She also denied any therapeutic radiation exposure or family history of cancer. On clinical examination, she appeared dehydrated and lethargic but was hemodynamically stable. A right-sided firm, irregular, non-tender mass was palpable in the area of the right thyroid lobe measuring approximately 3 cm by examination.
Laboratory investigations showed raised levels of total serum calcium 14.0 mg/dL (nl. 8.9–10.1), phosphorus 2.2 mg/dL (nl. 2.5–4.5), and parathyroid hormone (PTH) 239 pg/mL (nl. 10–65). Cervical ultrasonography (Fig. 10.1) revealed a 3.5-cm heterogeneous, hypervascular lobulated mass with calcification along the posterior aspect of the right lower thyroid lobe. There was no concerning cervical lymphadenopathy. Tc-99 m sestamibi single-photon emission computed tomography (SPECT-CT) showed a large focus of heterogeneous sestamibi uptake in a region corresponding with the mass identified on cervical ultrasound.
Sonogram of the right side of the neck, sagittal view. (a) A mass (PC) measuring approximately 3.5 × 2.6 × 2.9 cm is seen lying along the inferior and posterior aspect of the right lobe of the thyroid gland (TG). It is heterogeneous with lobulated margins and has internal calcifications. Both lobes of the thyroid are normal in size with normal vascularity. (b) The mass is hypervascular on color Doppler flow imaging
Diagnosis and Assessment
Our patient’s clinical presentation is consistent with hypercalcemia due to primary hyperparathyroidism. Parathyroid carcinoma (PC) is a rare endocrine malignancy, accounting for around 1 % of cases of primary hyperparathyroidism [1]. This infrequent, but potentially life-threatening, clinical entity was first reported by Wilder of Mayo Clinic in 1929 [2]. Conditions that appear to result in an increased risk of PC include multiple endocrine neoplasia type 1 [3], autosomal dominant familial isolated hyperparathyroidism [4], and hyperparathyroidism-jaw tumor syndrome due to mutation of the CDC73 gene [5].
PC presents a diagnostic and therapeutic challenge due to overlapping features with benign primary hyperparathyroidism and the lack of specific differentiating characteristics for malignancy. However, patients with PC typically have a serum PTH greater than five times the upper limit of normal and calcium levels in excess of 14 mg/dL, significantly higher than those with parathyroid adenoma or hyperplasia [6]. Unlike parathyroid adenoma, which has a female preponderance, PC affects both sexes equally, with an earlier median age of diagnosis in the fifth decade [7]. The findings of a palpable neck mass and dysphonia related to recurrent laryngeal nerve palsy as well as the combination of severe renal and bone disease are also suggestive of malignancy [7, 8].
The diagnosis of PC relies on a high index of suspicion, taking into account the patient’s clinical presentation, laboratory studies, imaging, and histopathology. The vast majority of PCs are functioning neoplasms, with clinical features and symptoms resulting from excessive secretion of PTH rather than local infiltration or mass effect from the neoplasm itself. Initial laboratory evaluation should include measurement of total serum calcium, PTH, and serum creatinine and an assessment of overall fluid and electrolyte status.
Ultrasound and sestamibi scintigraphy provide information on localization and the extent of the neoplasm, though neither is specific for carcinoma. Nonetheless, evidence of tumor invasion, irregular margins, and cervical node enlargement on ultrasound may raise suspicion for PC [9]. SPECT-CT with sestamibi, as utilized in this case, provides three-dimensional information with improved sensitivity for the detection of hyperfunctioning parathyroid glands [10]. Computerized tomography and magnetic resonance imaging, although not typically utilized on initial evaluation, may be useful adjuncts to ultrasonography in assessing for distant metastases in the chest or abdomen. Selective venous catheterization and PTH measurement may also be useful if noninvasive tests are equivocal or negative.
Fine needle aspiration (FNA) is not recommended in the setting of suspected PC due to the inability of cytology to differentiate between benign and malignant disease and the potential risk of ectopic tumor seeding [11].
Management
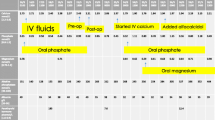
Prior to operative intervention, patients may require urgent management of dehydration, hypercalcemia, and associated metabolic abnormalities. Our patient was admitted for aggressive hydration with saline, initiation of a loop diuretic to promote calcium excretion, and administration of pamidronate. Following this, the decision was made to proceed to the operating room.
The gold standard treatment for PC is en bloc surgical resection [8]. Removal of any contiguous tissues to which the neoplasm adheres is necessary to achieve complete resection. This frequently includes the ipsilateral thyroid lobe and may necessitate resection of the ipsilateral recurrent laryngeal nerve. Ipsilateral compartment VI central neck dissection with removal of all lymphatic tissue should be performed. Care must be taken to avoid rupturing the capsule of the neoplasm, as this increases the likelihood of malignant parathyromatosis [12]. As highest chance of cure is obtainable if en bloc resection is carried out at the initial operation, a high index of suspicion for PC is therefore paramount. Chemotherapy and radiation have generally shown disappointing results [13].
Histopathological diagnosis is challenging, and while early pathologic criteria suggested the presence of a trabecular growth pattern, capsular invasion, vascular invasion, dense fibrous bands, and mitotic figures as suggestive of malignancy [14], later studies have shown that none of these are pathognomonic and may exist in parathyroid adenomas [15, 16]. Thus, the only unequivocal proof of malignancy is the local invasion of contiguous structures noted during surgery or the presence of distant metastasis.
In the postoperative period, serum calcium levels should be closely monitored. Adequate replacement with oral calcium, calcitriol, and intravenous calcium gluconate may be necessary to avoid symptomatic hypocalcemia associated with the “hungry bone syndrome.” When intravenous calcium supplementation is necessary, we recommend utilizing a central venous route as peripheral venous calcium supplementation can rarely result in local tissue necrosis [17].
Recurrence occurs in more than 50 % of cases [8, 18], most commonly in the neck, followed by the lungs, liver, and bone [19]. The majority of patients benefit from debulking of recurrent disease, if technically feasible, as palliation from the effects of hypercalcemia and hyperparathyroidism. Unfortunately, reoperation is rarely curative and eventual relapse is likely.
Outcome
Intraoperatively, a 3.5-cm heterogeneous, firm mass was found posterior to the right thyroid lobe with invasion into the thyroid parenchyma and involving the right recurrent laryngeal nerve. En bloc resection of the right parathyroid carcinoma with right thyroid lobectomy, right recurrent laryngeal nerve excision, and ipsilateral central lymph node dissection was therefore performed. Intraoperative PTH dropped from a baseline of 193–17.4 pg/mL 15 min after removal. The patient was discharged the following day without evidence of hypocalcemia. At 6-month follow-up, serum calcium and parathyroid hormone were within normal limits, and cervical ultrasound demonstrated no evidence of recurrent or persistent structural disease.
Clinical Pearls/Pitfalls
-
PC is a rare cause of hyperparathyroidism.
-
Overlapping features with benign hyperparathyroidism can make the diagnosis challenging.
-
Compared with benign primary hyperparathyroidism, patients with PC are more likely to present with symptoms, a neck mass, bone and renal disease, marked hypercalcemia, and very high serum PTH levels.
-
Ultrasound, sestamibi, and SPECT-CT are helpful in localizing and identifying the extent of the tumor. FNA should be avoided.
-
A definitive diagnosis of PC can only be made if the tumor is noted to be invading into surrounding tissues or distant metastases are found.
-
Patients have the highest chance of cure if en bloc resection is carried out at the initial operation. Thus, preoperative suspicion and intraoperative recognition of PC are essential.
-
Correction of hypercalcemia and dehydration preoperatively is essential in preventing possible renal failure and cardiac arrest.
References
Givi B, Shah JP. Parathyroid carcinoma. Clin Oncol (R Coll Radiol). 2010;22(6):498–507.
Wilder RM. Hyperparathyroidism: tumor of the parathyroid glands associated with osteitis fibrosa. Endocrinology. 1929;13:231–44.
Wassif WS, Moniz CF, Friedman E, et al. Familial isolated hyperparathyroidism: a distinct genetic entity with an increased risk of parathyroid cancer. J Clin Endocrinol Metab. 1993;77:1485–9.
Agha A, Carpenter R, Bhattacharya S, Edmonson SJ, Carlsen E, Monson JP. Parathyroid carcinoma in multiple endocrine neoplasia type 1 (MEN1) syndrome: two case reports of an unrecognised entity. J Endocrinol Invest. 2007;30:145e149.
Sharretts JM, Simonds WF. Clinical and molecular genetics of parathyroid neoplasms. Best Pract Res Clin Endocrinol Metabol. 2010;24(3):491–502.
Robert JH, Trombetti A, Garcia A, Pache JC, Herrmann F, Spiliopoulos A, Rizzoli R. Primary hyperparathyroidism: can parathyroid carcinoma be anticipated on clinical and biochemical grounds? Report of nine cases and review of the literature. Ann Surg Oncol. 2005;12(7):526.
Wynne AG, van Heerden J, Carney JA, Fitzpatrick LA. Parathyroid carcinoma: clinical and pathologic features in 43 patients. Medicine (Baltimore). 1992;71(4):197–205.
Shane E. Clinical review 122: parathyroid carcinoma. J Clin Endocrinol Metab. 2001;86:485e493.
Johnston LB, Carroll MJ, Britton KE, Lowe DG, Shand W, Besser GM, et al. The accuracy of parathyroid gland localization in primary hyperparathyroidism using Sestamibi radionuclide imaging. J Clin Endocrinol Metab. 1996;81:346.
Chen CC, Holder LE, Scovili WA, Tehan AM, Gann DS. Comparison of parathyroid imaging with technetium-99m-pertechnetate/sestamibi subtraction, double-phase technetium-99m-sestamibi and technetium-99m-sestamibi SPECT. J Nucl Med. 1997;38(6):834–9.
Spinelli C, Bonadio AG, Berti P, Materazzi G, Miccoli P. Cutaneous spreading of parathyroid carcinoma after fine needle aspiration cytology. J Endocrinol Invest. 2000;23:255e257.
Koea JB, Shaw JH. Parathyroid cancer: biology and management. Surg Oncol. 1999;8:155e165.
Obara T, Fujimoto Y. Diagnosis and treatment of patients with parathyroid carcinoma: an update and review. World J Surg. 1991;15(6):738.
Schantz A, Castleman B. Parathyroid carcinoma. A study of 70 cases. Cancer. 1973;31:600e605.
McKeown PP, McGarity WC, Sewell CW. Carcinoma of the parathyroid gland: is it overdiagnosed? A report of three cases. Am J Surg. 1984;147:292e298.
Bondeson L, Sandelin K, Grimelius L. Histopathological variables and DNA cytometry in parathyroid carcinoma. Am J Surg Pathol. 1993;17(8):820–9.
Klein R. Hypocalcemia. In: Loriaux L, editor. Endocrine emergencies: recognition and treatment. New York: Springer; 2010. p. 149–60.
Kebebew E. Parathyroid carcinoma. Curr Treat Options Oncol. 2001;2:347e354.
Kebebew E, Arici C, Duh QY, Clark OH. Localization and reoperation results for persistent and recurrent parathyroid carcinoma. Arch Surg. 2001;136(8):878–85.
Conflicts of Interest
All authors state that they have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Mayo Foundation for Medical Education and Research
About this chapter
Cite this chapter
Shariq, O.A., McKenzie, T.J. (2016). Parathyroid Carcinoma. In: Kearns, A., Wermers, R. (eds) Hyperparathyroidism. Springer, Cham. https://doi.org/10.1007/978-3-319-25880-5_10
Download citation
DOI: https://doi.org/10.1007/978-3-319-25880-5_10
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-25878-2
Online ISBN: 978-3-319-25880-5
eBook Packages: MedicineMedicine (R0)