Abstract
Retention of middle molecular weight (MMW) uremic toxins has been related to mortality in patients with end-stage kidney disease (ESKD). Therefore, interest has shifted from pure diffusive dialysis techniques, such as low-flux hemodialysis (HD), which remove only small water solutes, towards convective therapies, such as hemodiafiltration (HDF), which remove larger compounds as well. Controversy exists, however, as to whether the positive effect of HDF on MMW solutes translates in a superior clinical outcome. Here, we describe the results of three recent large randomized controlled trials (RCT), comparing online post-dilution HDF with HD, and four systematic reviews on convective therapy, and discuss the discrepancies between these studies. Actually, it appears that the concept of ‘convective therapy’ is confusing, as it is not strictly defined and differently interpreted. When convection volumes >21 L/session are applied, especially cardiovascular (CV) mortality is markedly reduced, while the incidence non-CV death due to infections or malignancies, remains unaltered. Echocardiographic analysis suggests that left ventricular (LV) function and structure worsen in HD and remain stable in HDF. Moreover, intradialytic hemodynamic stability appears better preserved during HDF. Currently, there is no convincing evidence that HDF lowers CV mortality by improvements in inflammation, nutrition, CKD-mineral and bone disease, dyslipidemia and anemia control.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Hemodialysis
- Hemodiafiltration
- Survival
- Mortality
- Hemodynamic stability
- Mechanisms
- Non-cardiovascular mortality
- Convection volume
- Pathophysiology
- Heparin
- Uremic toxins
Introduction
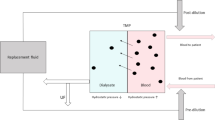
HD is the standard renal replacement therapy for patients with ESKD. Despite major technological improvements over the last decades, however, overall survival remains poor. Standard HD with low permeable membranes has shown to be an effective treatment for removing small water soluble substances, such as urea by diffusion, but simply increasing urea clearance did not improve survival [1]. To remove MMW uremic toxins more efficiently, high permeable dialyzers were introduced, which however, also did not reduce mortality [1, 2]. To enhance the clearance of MMW, HDF was developed, which combines diffusive transport of small molecules with an effective removal of larger solutes by convection. In modern HDF, fluid balance is maintained by the administration of online prepared ultrapure substitution fluid which can be infused before (predilution), midway (middilution) and after (postdilution) the dialyzer. As the majority of recent clinical studies is performed in the postdilution mode, this overview deals particularly with this type of treatment. Currently, controversy exists as to whether the positive effect of HDF on MMW solutes translates into a superior clinical outcome. In addition, the amount of convection required to obtain optimal benefit, is unknown [3]. In the present chapter, a summary is given of current literature on all-cause, CV and non-CV mortality, and a possible dose-response effect. In addition, potential mechanisms behind the beneficial effects of high volume HDF on survival are discussed.
Clinical Aspects: Overall and Cardiovascular Mortality
Recently, three large RCTs, comparing online post-dilution HDF with HD, were published [4–6]. While the Dutch CONTRAST and the Turkish HDF Study (THDFS) showed no differences in clinical outcome between treatment arms, in the Spanish ESHOL study a favorable effect of HDF on overall survival was found (Table 19.1). Both ESHOL and THDFS showed a lower, but non-significant, incidence in cardiovascular events in HDF patients.
To further answer the question whether dialysis treatment with ‘convective therapies’ improves clinical outcome, in the last 2 years four large meta-analyses have been published, which, however, showed a discordant outcome [7–10]. Yet, as discussed more extensively in Chap. 16, it appeared that these analyses differ in the number of studies and patients included, the definitions of comparator and intervention therapy, and type of studies, varying from small observational to large prospective RCTs.
In one meta-analysis low-flux HD was the reference therapy [9], while both low-flux and high-flux HD were reference therapies in three others [7, 8, 10]. Considering the intervention arm, inclusion covered different combinations of high-flux HD, off-line HDF, hemofiltration (HF), acetate-free biofiltration (AFB) and on-line postdilution HDF. Some of these modalities, however, can hardly be considered modern convective therapies, as convection volumes of 10–12 L/session are similar to the amount of internal filtration in high-flux HD and completely different from high volume HDF (>21 L/ session) [11]. In our opinion, a statement on today’s convective therapies should be based on a convection volume of at least 17–19 L/session in the postdilution mode [12]. The only meta-analysis which largely fulfills this criterion clearly shows an all cause and CV survival advantage of HDF over HD [7]. Interestingly, after removing AFB and off-line HDF from the meta-analysis by Nistor et al. [8], all cause mortality was superior in HDF patients [RR 0.82 (95 % CI 0.72–0.93)], Table 19.2 [12].
The latter findings were confirmed in an individual participant data meta-analysis (IPD), using data from CONTRAST, ESHOL, THDFS and a fourth not yet published French HDF study. Recent data indicate that HDF reduces the risk of all-cause mortality by 14 % (HR 0.86 [95 % CI 0.75–0.99]) and cardiovascular mortality by 23 % (HR 0.77 [95 % CI 0.61–0.97]) [4–6, 13].
Causes of Cardiovascular Death in HD and HDF
As shown by the meta-analysis by Mostovaya et al. [7], CV mortality is reduced by 27 %, and perhaps even further (55 %) when high volumes are applied.[5] In theory, both a decrease in the incidence in heart failure, which is difficult to diagnose in ESKD, ischemic heart disease, sudden death and stroke may play a role in this respect. Interestingly, in ESHOL a reduction in stroke was found, while the incidence of heart failure and ischemic heart disease was similar [5]. None of the three recent RCTs found a difference in sudden death between HDF and HD.
Cardiovascular Abnormalities in HD and HDF
Echocardiographic analysis may provide an answer to the question whether variations in LV structure and function explain the CV survival benefit of HDF. Indeed, the scarce studies performed showed improvement or stabilization in the HDF group and cardiac worsening in HD patients [14, 15]. Interestingly, from a small RCT in incident patients it appeared that treatment with predilution HF, a pure convective therapy, was associated with a more favorable development of LV mass (LVM) than low-flux HD [16]. Analysis of a large subset of the CONTRAST cohort revealed that, whereas both LVM and ejection fraction deteriorated over time in HD patients, these parameters remained stable in the HDF group [17]. Moreover, in a small RCT it was recently shown that high volume HDF (>22 L/session) prevented the endothelial dysfunction and stiffening of conduit arteries that was observed in HD patients [18].
Relation Between Clinical Outcome and Magnitude of the Convection Volume
Post hoc analysis of all three recent RCTs suggested a positive relationship between convection volume and clinical outcome, Fig. 19.1 (see also Chap. 16). Similar findings were suggested before by DOPPS [19]. Although the optimal convection volume is unclear, a minimum of 21 L/session appears appropriate [7].
Association between hazard ratio for mortality and convection volume in the different tertiles (or below/above the median) of convection volume in RCTs on hemodiafiltration: CONTRAST [4]: CONvective TRAnsport STudy, THDFS [6]: Turkish HDF Study, ESHOL [5]: Estudio de Supervicencia de Hemodiafiltracion OnLine
Hemodynamic Aspects
Intradialytic hypotension (IDH) is a common problem in HD, which has been related to cardiac stunning, bowel ischaemia and brain hypoperfusion. By echocardiography, during HD a compromised cardiac function was found in 65 % of the patients, which depended on the ultrafiltration rate and severity of IDH [20]. Moreover, patients with marked IDH have higher serum levels of cardiac enzymes [21] and reduced life expectancy [22]. Interestingly, treatment with cooled dialysate (CD-HD) reduced IDH, HD-induced brain injury [23] and improved CV survival [24]. In two large RCTs, blood pressure stability during HDF was superior to HD [5, 25] but not in a third [6]. When cool dialysate was used both in HDF and HD, hemodynamic changes, as measured by blood pressure, blood volume, cardiac output and microcirculation, did not differ [26]. Similarly, solute movements between the intra and extracellular compartments during HDF and CD-HD were similar [27]. Hence, it appears that intradialytic hemodynamic stability is better preserved during HDF than during standard HD, but analogous to CD-HD. Unfortunately, none of the recent RCTs reported dialysate temperature.
Clinical Aspects: Non-cardiovascular Mortality
Besides a high risk of CV death, ESKD patients have an elevated risk of non-CV mortality. As shown in a large study from the ERA-EDTA registry, the standardized mortality risks were equally increased, if compared to the general population (RR 8.8; 95 % CI 8.6–9.0 and RR 8.1; 95 % CI 7.9–8.3, resp.) [28]. Since the excess mortality in ESKD shows a ‘normal’ distribution, it is vital to know whether HDF decreases not only CV death, but also non-CV events.
Infection-Related Mortality
Infectious complications, which account for one quarter of total mortality in patients with ESKD, [29] are usually linked to bacterial spread from vascular access, particularly in case of central venous catheters (CVC). Whereas no overall difference was found in CONTRAST [30], infection-related mortality in ESHOL was lowest in HDF patients (HR 0.45, 95 % CI 0.21–0.96) [5]. Whether this outcome results from a lower CVC use in the HDF group (7 % versus HD 13 %) or from the high convection volumes applied remains to be established. Unpublished data from the IPD meta-analysis, as outlined before, showed a similar incidence of infection-related mortality (HDF HR 0.94; 95 %CI 0.66–1.30) in both treatment arms [13].
Other Causes of Death
None of the meta-analyses or RCTs reported a decline in other causes of death, such as withdrawal from dialysis [29] or malignancies. Considering this ‘rest group’, unpublished findings from the IPD meta-analysis showed similar mortality rates: HDF HR 0.92; 95 %CI 0.73–1.15.
Pathophysiological Aspects
Both classical risk factors, such as high blood pressure and cholesterol levels, and non-traditional risk factors, including the toxicity of uremia itself and the bio-incompatibility of the extra-corporeal system, have been implicated in the high mortality risk of ESKD.
Classical Risk Factors
Blood Pressure
From a large sub-study of CONTRAST, it appeared that mean arterial pressure (MAP) decreased over time, mainly due to a reduction in peripheral resistance. As cardiac output remained unaltered, the authors speculated that loss of functioning renal tissue ultimately leads to a reduced stimulation of the renin-angiotensin-aldosteron- and sympathic systems [17], which are overactivated in CKD [31]. Differences between the HD and HDF groups, however, were not observed. By meta-analysis, HDF treatment did not influence systolic BP, diastolic BP, MAP or prescription of anti-hypertensive drugs [8, 9]. In accordance with these findings, Georgianos et al. found that HDF did not have beneficial effects on arterial stiffness, wave reflections or central aortic pressure [32].
Dyslipidemia
Dyslipidemia is frequently observed in ESKD. Controversy exists as to whether high lipid levels contribute to the greatly elevated CV risk in these patients. Whereas HDL-C exerts potent anti-thrombotic, anti-inflammatory and anti-apoptotic effects in the general population, in CKD fundamental structural alterations of this particle have been identified [33]. Therefore, the mere measuring of lipid profiles may not reliably reflect CV risk. In short term HDF studies, confusing data were published, from higher HDL-C and lower triglyceride (TG) levels to increased LDL-C and stable TG values [34, 35]. A recent meta-analysis showed a reduction in TG and stabilization of total cholesterol and LDL-C [9]. Interpretation, however, is difficult as the mere raising of HDL and lowering of LDL does not automatically entail return of their (anti) atherogenic properties.
Other Risk Factors
Large RCTs comparing high-flux with low-flux HD suggested that besides diabetics, patients with a albumin <40 g/L and subjects with a dialysis vintage >30 months would benefit from ‘convective therapy’ [1, 2]. However, with the exception of a high co-morbidity index in ESHOL, none of the meta-analyses or recent large RCTs showed different effects of HDF in these and other selected subgroups, such as age and gender.
Non-traditional Risk Factors
Inflammation and Oxidative Stress
A chronic low grade inflammatory state is common in ESKD [36]. Besides uremia-related factors, such as accumulation of uremic toxins, dialysis-related factors, including the bio-incompatibility of the extracorporeal system, have been implicated in this process. HDF may decrease inflammatory activity by enhanced clearance of MMW uremic toxins; on the other hand, the infusion of large amounts of substitution fluid may aggravate the micro-inflammatory state. Whereas some observational studies reported on a decrease of inflammation and oxidative stress after treatment with convective therapies [37, 38], several small RCTs did not [39]. Comparison in observational studies is often hampered by the fact that, while in HDF ultrapure (UP) dialysis fluid (micro-organisms <0.1 CFU/ml; endotoxins <0.025 EU/ml) is mandatory, in HD the dialysis fluid is frequently consistent with ‘standard quality’ (<100 CFU/ml; <0.25 EU/ml) [40, 41]. Of note, use of UP fluid in HD resulted not only in a decline in markers of inflammation and oxidative stress, but also in increased serum albumin and hemoglobin levels [42]. As the same water treatment system was used in both arms of CONTRAST and ESHOL, it is unlikely that differences in clinical outcome, as observed in ESHOL and in the high volume group of CONTRAST, result from a dissimilar quality of dialysis fluid. Moreover, CRP levels did not differ between treatment arms in either study (Table 19.3).
CKD-Mineral and Bone Disorder
Chronic kidney disease-mineral and bone disorder (CKD-MBD) is the term used to describe a constellation of abnormalities that may lead to bone disturbances and extra-skeletal calcifications in soft tissues and arteries. Biochemically this syndrome is characterized by abnormalities in serum phosphate, parathyroid hormone (PTH), fibroblast growth factor 23 (FGF23), calcium and vitamin D.
Retention of phosphate has been implicated in all cause and CV mortality [43, 44]. Phosphate levels are generally lower during treatment with convective therapies than with low-flux HD [9]. When comparing HDF with high-flux HD, results are contradictory [26, 45]. Actually, treatment of hyperphosphatemia consists of both phosphate-binding agents and dialysis. Hence, when comparing phosphate control between modalities, phosphate levels as well as the amount of phosphate-binding drugs should be taken into account. Both in CONTRAST and the PAN Thames Renal Audit, phosphate levels were lower in HDF than in HD patients treated with low-flux dialyzers [46, 47]. By contrast, neither in THDFS nor in ESHOL differences were observed between (high-flux) HD and HDF (Table 19.3) [5, 6].
Phosphate is excreted by the kidney in response to PTH (9.5 kD) and FGF23 (see below). High serum PTH levels in ESKD have been related to a poor clinical outcome [48], although suppression by cinacalcet did not reduce mortality [49]. In THDFS as well in ESHOL, PTH levels were similar in both treatment arms (Table 19.3). Of note, previously it was shown that PTH levels decrease after a session with low volume HDF, but increase after high volume HDF, possible as a result of a negative calcium balance [50]. In a meta-analysis comparing convective therapies with low-flux HD, differences between treatment strategies were not found [9].
Both human and animal data suggest that an increased FGF23 (32 kD) value is the earliest detectable biochemical alteration in CKD-MBD [51]. Levels of this phosphatonin, which is produced by bone marrow cells, are 100–1000-fold higher in ESKD than in healthy individuals. While no intra-dialytical changes were observed during low-flux HD [52], FGF23 removal was markedly higher during HDF than during high-flux HD [26, 53]. As FGF23 has been related to LVH [54] and CV events, especially congestive heart failure [55, 56], reduction by HDF may lower CV mortality in ESKD.
Other Conditions Which Have Been Related to Mortality in ESKD
Worsening of the nutritional state is a well known feature in ESKD. The term Protein Energy Wasting (PEW) describes a state of decreased body stores of protein and energy fuels [57]. Various score systems have been applied to measure PEW, such as the Subjective Global Assessment (SGA), Malnutrition Inflammation Score (MIS), Geriatric Nutritional Risk Index (GNRI) and the composite Protein Energy Nutrition Score (cPENS) [58]. Recent observations from CONTRAST indicate that SGA and MIS predict mortality no better than a single albumin measurement [58, 59]. While in the THDFS, time averaged albumin levels were lower in HDF patients, both in ESHOL and CONTRAST albumin levels decreased over time, without differences between groups (Table 19.3) [5, 60].
Anemia is a hallmark of ESKD. Besides a reduced production of erythropoietin (EPO) and EPO resistance, a diminished enteric uptake of iron and a shortened lifespan of red blood cells may play a role. EPO resistance has been associated with (functional) iron deficiency, impaired nutritional state, chronic micro-inflammation and retention of MMW solutes. As for the latter, it was suggested that convective treatment would improve EPO resistance and hence anemia [61]. Against expectations, however, a large RCT did not show any advantage of HDF [62]. Moreover, in CONTRAST, ESHOL and THDFS, neither Hb values, nor transferrin saturation index or ferritin levels differed between groups (Table 19.3) [5, 6, 63]. With respect to the EPO resistance index in HDF patients, contradictory results were obtained, being lower in THDFS, and similar in ESHOL and CONTRAST. In a sub-analysis of CONTRAST, EPO resistance did not differ between low (<18 L) and high (>22 L) volume HDF [63].
Accumulating evidence indicates that mild acidosis in ESKD is related to an adverse clinical outcome. Correction has been positively associated with SGA, residual renal function and normalized protein appearance rate [64], shorter hospitalization and lower mortality [65]. In a cross-over study, net bicarbonate gain was slightly higher during HDF, while at the end of the session acid-base status was similar to HD [66]. In THDFS, a positive trend was observed between bicarbonate levels and convection volume (Table 19.3) [6]. Hence, although not yet convincingly demonstrated, a better correction of acidosis during HDF may contribute to the improved survival in this patient group.
Treatment-Related Aspects
Platelet Activation and (Anti)coagulation
In HD, unfractionated heparin or low-molecular-weight heparin (LMWH) is administered to prevent clotting. During HDF, however, the intra-dialyzer transmembrane pressure is considerable higher and, due to the high ultrafiltration rate, blood viscosity increased [67]. Consequently, platelet activation and coagulation are more pronounced. Indeed, in THDFS the heparin dose was 25 % higher in HDF than in HD patients, while in CONTRAST the LMWH dose was 10 % higher [6, 68]. Currently, however, it is unknown whether increased platelet activation and coagulation at the one hand and use of additional heparin or LMWH on the other is beneficial or harmful to the patients. The use of relatively high doses, three times per week, year after year, may reduce CV events in subjects with a high cardiovascular risk profile. In addition, malfunctioning and chronic depleted platelets, as demonstrated before in HD patients [67, 69], may protect against vascular disease [70]. Alternatively, it is conceivable that these side effects of HDF actually harm the patients.
Clearance of Low-Molecular Weight, Middle-Sized and Protein-Bound Solutes
Uremic solutes are generally subdivided in three major classes: (1) water soluble compounds (<500 Da), which are easily removed by any dialysis strategy, (2) MMW substances (0.5–40 kD), which can only be removed by convection, and (3) protein-bound uremic toxins, which are difficult to remove [71]. With respect to the adequacy parameter Kt/Vurea, a measure of small water soluble molecule clearance, all three recent RCTs showed an improvement in HDF patients (Table 19.3), while mortality was only reduced in ESHOL [4–6]. Considering MMW solutes, high beta-2-microglobulin (β2M) levels have been shown to be independently associated with overall and CV mortality [72]. However, while in CONTRAST and ESHOL β2M levels were lower in HDF than in HD patients, only ESHOL showed a benefit of HDF (Table 19.3). Multiple toxic effects have been attributed to protein-bound phenolic compounds, such as p-cresylsulfate. P-cresol is generated by intestinal bacteria and conjugated to p-cresylsulfate and p-cresylglucuronide. In-vitro these compounds induce toxic effects on endothelial integrity and leucocyte rolling [73]. Clinically, these substances have been associated with an adverse CV outcome [71]. Whereas high-flux HD did not augment the reduction of protein-bound toxins, addition of convective transport by HDF improved the removal of these compounds slightly [74].
Summary and Conclusions
Is Online Post-Dilution HDF Associated with an Improved Survival?
From this overview it appears first, that all-cause mortality is significantly reduced by HDF, CV events almost exclusively accounting for this beneficial effect. Other causes of mortality, such as infections and sudden death, are not different between HDF and HD. Second, it remains unclear whether the reduction in CV mortality is caused by a decline in stroke, heart failure or ischemic heart disease. Third, a convection volume of at least 21 L/session appears required for the desired effect.
Why Is High Volume HDF Associated with Improved Survival?
Having illustrated that high volume HDF is related to an improved CV survival, what are the underlying mechanisms? Are the aforementioned RCTs confounded by a favorable clinical profile of HDF patients beforehand? Although this option was not discussed in this chapter and cannot completely be ruled out, it should be mentioned that extensive corrections were made in all RCTs. Moreover, we recently showed that centre policy, rather than patient factors, determine the magnitude of the convection volume [75]. Indeed, recent data from a large prospective observational study indicate that at least 21 L of substitution fluid is feasible in more than 80 % of ESKD patients [76]. As published in individual RCTs and by meta-analysis, predialysis blood pressure was not different between groups, but HDF may improve intra-dialytic hemodynamic stability. Analysis by echocardiography indicated that the functional and structural deterioration of the LV over time in HD patients was mitigated or even absent in HDF. Convincing arguments are not available that HDF reduces CV mortality by improvements in traditional or non-traditional risk factors. With respect to solute removal, neither Kt/Vurea nor β2M was related to survival. By contrast, FGF23 appears a promising candidate toxin for the HDF-induced benefit on survival. Whether high doses of heparin or better correction of acidosis adds to the reduced mortality in HDF is a matter for future research.
Teaching Points
-
High volume online post-dilution HDF is associated with improved overall survival
-
This advantage results entirely from a lower cardiovascular mortality, possibly due to better preservation of left ventricular mass and function
-
High volume online post-dilution HDF offers no benefits in terms of non-cardiovascular mortality
-
The beneficial effect of high volume online post-dilution HDF on survival is not restricted to selected subgroups, such as age, co-morbidity or dialysis-vintage
-
Both removal of MMW uremic toxins and improved intra-dialytical blood pressure stability may contribute to the beneficial effect of high volume online post-dilution HDF on survival
-
There is no compelling evidence that high volume online post-dilution HDF reduces mortality by improvements in traditional and non-traditional risk factors
-
The middle molecular weight molecule FGF23 and the protein-bound solutes p-cresyl sulfate and indoxyl sulfate are putative uremic toxins that are removed by high volume online post-dilution HDF and may explain part of its survival benefit
References
Eknoyan G, Beck GJ, Cheung AK, Daugirdas JT, Greene T, Kusek JW, et al. Effect of dialysis dose and membrane flux in maintenance hemodialysis. N Engl J Med. 2002;347(25):2010–9.
Locatelli F, Martin-Malo A, Hannedouche T, Loureiro A, Papadimitriou M, Wizemann V, et al. Effect of membrane permeability on survival of hemodialysis patients. J Am Soc Nephrol. 2009;20(3):645–54.
Farrington K, Davenport A. The ESHOL study: hemodiafiltration improves survival-but how? Kidney Int. 2013;83(6):979–81.
Grooteman MP, van den Dorpel MA, Bots ML, Penne EL, van der Weerd NC, Mazairac AH, et al. Effect of online hemodiafiltration on all-cause mortality and cardiovascular outcomes. J Am Soc Nephrol. 2012;23(6):1087–96.
Maduell F, Moreso F, Pons M, Ramos R, Mora-Macia J, Carreras J, et al. High-efficiency postdilution online hemodiafiltration reduces all-cause mortality in hemodialysis patients. J Am Soc Nephrol. 2013;24(3):487–97.
Ok E, Asci G, Toz H, Ok ES, Kircelli F, Yilmaz M, et al. Mortality and cardiovascular events in online haemodiafiltration (OL-HDF) compared with high-flux dialysis: results from the Turkish OL-HDF Study. Nephrol Dial Transplant. 2013;28(1):192–202.
Mostovaya IM, Blankestijn PJ, Bots ML, Covic A, Davenport A, Grooteman MP, et al. Clinical evidence on hemodiafiltration: a systematic review and a meta-analysis. Semin Dial. 2014;27(2):119–27.
Nistor I, Palmer SC, Craig JC, Saglimbene V, Vecchio M, Covic A, et al. Convective versus diffusive dialysis therapies for chronic kidney failure: an updated systematic review of randomized controlled trials. Am J Kidney Dis. 2014;63(6):954–67.
Susantitaphong P, Siribamrungwong M, Jaber BL. Convective therapies versus low-flux hemodialysis for chronic kidney failure: a meta-analysis of randomized controlled trials. Nephrol Dial Transplant. 2013;28(11):2859–74.
Wang AY, Ninomiya T, Al-Kahwa A, Perkovic V, Gallagher MP, Hawley C, et al. Effect of hemodiafiltration or hemofiltration compared with hemodialysis on mortality and cardiovascular disease in chronic kidney failure: a systematic review and meta-analysis of randomized trials. Am J Kidney Dis. 2014;63(6):968–78.
Ronco C, Brendolan A, Lupi A, Metry G, Levin NW. Effects of a reduced inner diameter of hollow fibers in hemodialyzers. Kidney Int. 2000;58(2):809–17.
Grooteman MP, Blankestijn PJ, Nube MJ. Not all convective dialysis therapies are equal. Am J Kidney Dis. 2014;64(5):819–20.
Peters SAE, Bots ML, Canaud B, Davenport A, Grooteman MPC, Kircelli F, et al. Haemodiafiltration and mortality in end stage kidney disease patients. A pooled individual participant data meta-analysis from four randomised controlled trials. Nephrol Dial Transplant. 2015. doi:10.1093/ndt/gfv349.
Czifra A, Pall A, Kulcsar J, Barta K, Kertesz A, Paragh G, et al. Hemodialysis and hemodiafiltration differently modulate left ventricular diastolic function. BMC Nephrol. 2013;14:76.
Ohtake T, Oka M, Ishioka K, Honda K, Mochida Y, Maesato K, et al. Cardiovascular protective effects of on-line hemodiafiltration: comparison with conventional hemodialysis. Ther Apher Dial. 2012;16(2):181–8.
Alvestrand A, Ledebo I, Hagerman I, Wingren K, Mattsson E, Qureshi AR, et al. Left ventricular hypertrophy in incident dialysis patients randomized to treatment with hemofiltration or hemodialysis: results from the ProFil study. Blood Purif. 2011;32(1):21–9.
Mostovaya IM, Bots ML, van den Dorpel MA, Grooteman MP, Kamp O, Levesque R, et al. A randomized trial of hemodiafiltration and change in cardiovascular parameters. Clin J Am Soc Nephrol. 2014;9(3):520–6.
Bellien J, Freguin-Bouilland C, Joannides R, Hanoy M, Remy-Jouet I, Monteil C, et al. High-efficiency on-line haemodiafiltration improves conduit artery endothelial function compared with high-flux haemodialysis in end-stage renal disease patients. Nephrol Dial Transplant. 2014;29(2):414–22.
Canaud B, Bragg-Gresham JL, Marshall MR, Desmeules S, Gillespie BW, Depner T, et al. Mortality risk for patients receiving hemodiafiltration versus hemodialysis: European results from the DOPPS. Kidney Int. 2006;69(11):2087–93.
Burton JO, Jefferies HJ, Selby NM, McIntyre CW. Hemodialysis-induced cardiac injury: determinants and associated outcomes. Clin J Am Soc Nephrol. 2009;4(5):914–20.
Hung SY, Hung YM, Fang HC, Yeh JH, Hung GC, Wu CJ, et al. Cardiac troponin I and creatine kinase isoenzyme MB in patients with intradialytic hypotension. Blood Purif. 2004;22(4):338–43.
Iseki K, Shoji T, Nakai S, Watanabe Y, Akiba T, Tsubakihara Y. Higher survival rates of chronic hemodialysis patients on anti-hypertensive drugs. Nephron Clin Pract. 2009;113(3):c183–90.
Eldehni MT, Odudu A, McIntyre CW. Randomized clinical trial of dialysate cooling and effects on brain white matter. J Am Soc Nephrol. 2015;26(4):957–65.
Hsu HJ, Yen CH, Hsu KH, Lee CC, Chang SJ, Wu IW, et al. Association between cold dialysis and cardiovascular survival in hemodialysis patients. Nephrol Dial Transplant. 2012;27(6):2457–64.
Locatelli F, Altieri P, Andrulli S, Bolasco P, Sau G, Pedrini LA, et al. Hemofiltration and hemodiafiltration reduce intradialytic hypotension in ESRD. J Am Soc Nephrol. 2010;21(10):1798–807.
Cornelis T, van der Sande FM, Eloot S, Cardinaels E, Bekers O, Damoiseaux J, et al. Acute hemodynamic response and uremic toxin removal in conventional and extended hemodialysis and hemodiafiltration: a randomized crossover study. Am J Kidney Dis. 2014;64(2):247–56.
Kumar S, Khosravi M, Massart A, Potluri M, Davenport A. Haemodiafiltration results in similar changes in intracellular water and extracellular water compared to cooled haemodialysis. Am J Nephrol. 2013;37(4):320–4.
de Jager DJ, Grootendorst DC, Jager KJ, van Dijk PC, Tomas LM, Ansell D, et al. Cardiovascular and noncardiovascular mortality among patients starting dialysis. JAMA. 2009;302(16):1782–9.
den Hoedt CH, Bots ML, Grooteman MP, Mazairac AH, Penne EL, van der Weerd NC, et al. Should we still focus that much on cardiovascular mortality in end stage renal disease patients? The CONvective TRAnsport STudy. PLoS One. 2013;8(4):e61155.
den Hoedt CH, Grooteman MP, Bots ML, Blankestijn PJ, van der Tweel I, van den Weerd NC, et al. The effect of HDF on infections: results from the CONvective TRAnsport STudy. PLoSone 2015;10(8):e0135908.
Blankestijn PJ, Ligtenberg G, Klein IH, Koomans HA. Sympathetic overactivity in renal failure controlled by ACE inhibition: clinical significance. Nephrol Dial Transplant. 2000;15(6):755–8.
Georgianos PI, Sarafidis PA, Karpetas A, Kosmidis D, Sioulis A, Liakopoulos V, et al. Hemodiafiltration does not have additional benefits over hemodialysis on arterial stiffness, wave reflections and central aortic pressures. Blood Purif. 2014;37(1):18–26.
Speer T, Zewinger S, Fliser D. Uraemic dyslipidaemia revisited: role of high-density lipoprotein. Nephrol Dial Transplant. 2013;28(10):2456–63.
Panichi V, Rizza GM, Paoletti S, Bigazzi R, Aloisi M, Barsotti G, et al. Chronic inflammation and mortality in haemodialysis: effect of different renal replacement therapies. Results from the RISCAVID study. Nephrol Dial Transplant. 2008;23(7):2337–43.
Vaslaki L, Major L, Berta K, Karatson A, Misz M, Pethoe F, et al. On-line haemodiafiltration versus haemodialysis: stable haematocrit with less erythropoietin and improvement of other relevant blood parameters. Blood Purif. 2006;24(2):163–73.
Yao Q, Lindholm B, Stenvinkel P. Inflammation as a cause of malnutrition, atherosclerotic cardiovascular disease, and poor outcome in hemodialysis patients. Hemodial Int. 2004;8(2):118–29.
Calo LA, Naso A, Carraro G, Wratten ML, Pagnin E, Bertipaglia L, et al. Effect of haemodiafiltration with online regeneration of ultrafiltrate on oxidative stress in dialysis patients. Nephrol Dial Transplant. 2007;22(5):1413–9.
Filiopoulos V, Hadjiyannakos D, Metaxaki P, Sideris V, Takouli L, Anogiati A, et al. Inflammation and oxidative stress in patients on hemodiafiltration. Am J Nephrol. 2008;28(6):949–57.
Leurs P, Lindholm B, Stenvinkel P. Effects of hemodiafiltration on uremic inflammation. Blood Purif. 2013;35 Suppl 1:11–7.
Akoglu H, Dede F, Piskinpasa S, Falay MY, Odabas AR. Impact of low- or high-flux haemodialysis and online haemodiafiltration on inflammatory markers and lipid profile in chronic haemodialysis patients. Blood Purif. 2013;35(4):258–64.
den Hoedt CH, Mazairac AH, van den Dorpel MA, Grooteman MP, Blankestijn PJ. Effect of hemodiafiltration on mortality, inflammation and quality of life. Contrib Nephrol. 2011;168:39–52.
Susantitaphong P, Riella C, Jaber BL. Effect of ultrapure dialysate on markers of inflammation, oxidative stress, nutrition and anemia parameters: a meta-analysis. Nephrol Dial Transplant. 2013;28(2):438–46.
Gutierrez OM, Mannstadt M, Isakova T, Rauh-Hain JA, Tamez H, Shah A, et al. Fibroblast growth factor 23 and mortality among patients undergoing hemodialysis. N Engl J Med. 2008;359(6):584–92.
Kovesdy CP, Anderson JE, Kalantar-Zadeh K. Outcomes associated with serum phosphorus level in males with non-dialysis dependent chronic kidney disease. Clin Nephrol. 2010;73(4):268–75.
Minutolo R, Bellizzi V, Cioffi M, Iodice C, Giannattasio P, Andreucci M, et al. Postdialytic rebound of serum phosphorus: pathogenetic and clinical insights. J Am Soc Nephrol. 2002;13(4):1046–54.
Davenport A, Gardner C, Delaney M. The effect of dialysis modality on phosphate control: haemodialysis compared to haemodiafiltration. The Pan Thames Renal Audit. Nephrol Dial Transplant. 2009;24(10):3209–15.
Penne EL, van der Weerd NC, van den Dorpel MA, Grooteman MP, Levesque R, Nube MJ, et al. Short-term effects of online hemodiafiltration on phosphate control: a result from the randomized controlled Convective Transport Study (CONTRAST). Am J Kidney Dis. 2010;55(1):77–87.
Kovesdy CP, Ahmadzadeh S, Anderson JE, Kalantar-Zadeh K. Secondary hyperparathyroidism is associated with higher mortality in men with moderate to severe chronic kidney disease. Kidney Int. 2008;73(11):1296–302.
Chertow GM, Block GA, Correa-Rotter R, Drueke TB, Floege J, Goodman WG, et al. Effect of cinacalcet on cardiovascular disease in patients undergoing dialysis. N Engl J Med. 2012;367(26):2482–94.
Rius A, Hernandez-Jaras J, Pons R, Garcia PH, Torregrosa E, Sanchez Canel JJ, et al. Kinetic of calcium, phosphate, magnesium and PTH variations during hemodiafiltration. Nefrología. 2007;27(5):593–8.
Isakova T, Wahl P, Vargas GS, Gutierrez OM, Scialla J, Xie H, et al. Fibroblast growth factor 23 is elevated before parathyroid hormone and phosphate in chronic kidney disease. Kidney Int. 2011;79(12):1370–8.
Urena TP, Friedlander G, de Vernejoul MC, Silve C, Prie D. Bone mass does not correlate with the serum fibroblast growth factor 23 in hemodialysis patients. Kidney Int. 2008;73(1):102–7.
Patrier L, Dupuy AM, Granger VA, Chalabi L, Morena M, Canaud B, et al. FGF-23 removal is improved by on-line high-efficiency hemodiafiltration compared to conventional high flux hemodialysis. J Nephrol. 2013;26(2):342–9.
Marsell R, Grundberg E, Krajisnik T, Mallmin H, Karlsson M, Mellstrom D, et al. Fibroblast growth factor-23 is associated with parathyroid hormone and renal function in a population-based cohort of elderly men. Eur J Endocrinol. 2008;158(1):125–9.
Scialla JJ, Wolf M. Roles of phosphate and fibroblast growth factor 23 in cardiovascular disease. Nat Rev Nephrol. 2014;10(5):268–78.
Seiler S, Rogacev KS, Roth HJ, Shafein P, Emrich I, Neuhaus S, et al. Associations of FGF-23 and sKlotho with cardiovascular outcomes among patients with CKD stages 2–4. Clin J Am Soc Nephrol. 2014;9(6):1049–58.
Fouque D, Kalantar-Zadeh K, Kopple J, Cano N, Chauveau P, Cuppari L, et al. A proposed nomenclature and diagnostic criteria for protein-energy wasting in acute and chronic kidney disease. Kidney Int. 2008;73(4):391–8.
Mazairac AH, de Wit GA, Grooteman MP, Penne EL, van der Weerd NC, van den Dorpel MA, et al. A composite score of protein-energy nutritional status predicts mortality in haemodialysis patients no better than its individual components. Nephrol Dial Transplant. 2010;26(6):1962–7.
de Roij van Zuijdewijn CL, ter Wee PM, Chapdelaine I, Bots ML, Blankestijn PJ, van den Dorpel MA, et al. A comparison of 8 nutrition-related tests to predict mortality in hemodialysis patients. J Ren Nutr. 2015;25(5):412–9.
den Hoedt CH, Bots ML, Grooteman MP, van der Weerd NC, Penne EL, Mazairac AH, et al. Clinical predictors of decline in nutritional parameters over time in ESRD. Clin J Am Soc Nephrol. 2014;9(2):318–25.
Macdougall IC. Present and future strategies in the treatment of renal anaemia. Nephrol Dial Transplant. 2001;16 Suppl 5:50–5.
Locatelli F, Altieri P, Andrulli S, Sau G, Bolasco P, Pedrini LA, et al. Predictors of haemoglobin levels and resistance to erythropoiesis-stimulating agents in patients treated with low-flux haemodialysis, haemofiltration and haemodiafiltration: results of a multicentre randomized and controlled trial. Nephrol Dial Transplant. 2012;27(9):3594–600.
van der Weerd NC, den Hoedt CH, Blankestijn PJ, Bots ML, van den Dorpel MA, Levesque R, et al. Resistance to erythropoiesis stimulating agents in patients treated with online hemodiafiltration and ultrapure low-flux hemodialysis: results from a randomized controlled trial (CONTRAST). PLoS One. 2014;9(4):e94434.
Szeto CC, Wong TY, Chow KM, Leung CB, Li PK. Oral sodium bicarbonate for the treatment of metabolic acidosis in peritoneal dialysis patients: a randomized placebo-control trial. J Am Soc Nephrol. 2003;14(8):2119–26.
Kovesdy CP, Anderson JE, Kalantar-Zadeh K. Association of serum bicarbonate levels with mortality in patients with non-dialysis-dependent CKD. Nephrol Dial Transplant. 2009;24(4):1232–7.
Morel H, Jaffrin MY, Lux C, Renou M, Fessier C, Petit A, et al. A comparison of bicarbonate kinetics and acid-base status in high flux hemodialysis and on-line post-dilution hemodiafiltration. Int J Artif Organs. 2012;35(4):288–300.
Gritters-van den Oever M, Grooteman MP, Bartels PC, Blankestijn PJ, Bots ML, van den Dorpel MA, et al. Post-dilution haemodiafiltration and low-flux haemodialysis have dissimilar effects on platelets: a side study of CONTRAST. Nephrol Dial Transplant. 2009;24(11):3461–8.
de Roij van Zuijdewijn C, Nube MJ, Blankestijn PJ, ter Wee PM, van den Dorpel MA, Bots ML, et al. The prescribed dose of low molecular weight heparin increases after assigning patients to hemodiafiltration (HDF) treatment. 2014;11:292A.
Schoorl M, Schoorl M, Nube MJ, Bartels PC. Platelet depletion, platelet activation and coagulation during treatment with hemodialysis. Scand J Clin Lab Invest. 2011;71(3):240–7.
Borissoff JI, Spronk HM, ten Cate H. The hemostatic system as a modulator of atherosclerosis. N Engl J Med. 2011;364(18):1746–60.
Neirynck N, Vanholder R, Schepers E, Eloot S, Pletinck A, Glorieux G. An update on uremic toxins. Int Urol Nephrol. 2013;45(1):139–50.
Liabeuf S, Lenglet A, Desjardins L, Neirynck N, Glorieux G, Lemke HD, et al. Plasma beta-2 microglobulin is associated with cardiovascular disease in uremic patients. Kidney Int. 2012;82(12):1297–303.
Pletinck A, Glorieux G, Schepers E, Cohen G, Gondouin B, Van LM, et al. Protein-bound uremic toxins stimulate crosstalk between leukocytes and vessel wall. J Am Soc Nephrol. 2013;24(12):1981–94.
Meert N, Waterloos MA, Van LM, Dhondt A, Ledebo I, Glorieux G, et al. Prospective evaluation of the change of predialysis protein-bound uremic solute concentration with postdilution online hemodiafiltration. Artif Organs. 2010;34(7):580–5.
Chapdelaine I, Mostovaya IM, Blankestijn PJ, Bots ML, van den Dorpel MA, Levesque R, et al. Treatment policy rather than patient characteristics determines convection volume in online post-dilution hemodiafiltration. Blood Purif. 2014;37(3):229–37.
Marcelli D, Scholz C, Ponce P, Sousa T, Kopperschmidt P, Grassmann A, et al. High-volume postdilution hemodiafiltration is a feasible option in routine clinical practice. Artif Organs. 2015;39(2):142–9.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Nubé, M.J. (2016). Why Is High Volume Online Post-dilution Hemodiafiltration Associated with Improved Survival?. In: Nubé, M., Grooteman, M., Blankestijn, P. (eds) Hemodiafiltration. Springer, Cham. https://doi.org/10.1007/978-3-319-23332-1_19
Download citation
DOI: https://doi.org/10.1007/978-3-319-23332-1_19
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-23331-4
Online ISBN: 978-3-319-23332-1
eBook Packages: MedicineMedicine (R0)