Abstract
The non-surgical management of patients with traumatic brain injury is the treatment and prevention of secondary insults, such as low cerebral perfusion pressure (CPP). Most clinical pressure monitoring systems measure pressure relative to atmospheric pressure. If a patient is managed with their head tilted up, relative to their arterial pressure transducer, then a hydrostatic pressure gradient (HPG) can act against arterial pressure and cause significant errors in calculated CPP.
To correct for HPG, the arterial pressure transducer should be placed level with the intracranial pressure transducer. However, this is not always achieved. In this chapter, we describe a pilot study investigating the application of speckled computing (or “specks”) for the automatic monitoring of the patient’s head tilt and subsequent automatic calculation of HPG. In future applications this will allow us to automatically correct CPP to take into account any HPG.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
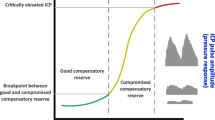
The non-surgical management of patients with traumatic brain injury (TBI) is the treatment and prevention of secondary insults, such as low cerebral perfusion pressure (CPP). CPP is the net pressure gradient that allows blood to flow to the brain. Under normal conditions, the brain autoregulates its blood flow to ensure a constant flow, despite blood pressure. However, these homeostatic controls are often lost after head injury. Areas of the brain that are ischaemic, or at risk of becoming ischaemic, are critically dependent on maintaining CPP. If CPP becomes too low then further, secondary brain injury can occur. For this reason, the widely applied Brain Trauma Guidelines [2] for the management of TBI suggest the maintenance of CPP at 50–70 mmHg. CPP can be calculated by subtracting intracranial pressure (ICP) from the patient’s mean arterial pressure (MAP):
In most modern neuro-intensive care units, ICP readings are taken by an ICP monitor, which is inserted through the patient’s skull and placed in the lateral ventricle or directly into the brain parenchyma [7]. However, these clinical pressure monitoring systems measure pressure relative to atmospheric pressure. A problem with using fluid-filled catheter transducer systems to monitor ICP is the necessity to correct for hydrostatic pressure gradient (HPG). Often the external strain gauge transducer is zeroed at the same level as the arterial pressure transducer. If the patient is managed in the horizontal position, there is no column of fluid between the sites of the two pressure monitors. If a patient is managed with their head tilted up relative to their arterial pressure transducer (i.e. the arterial pressure transducer is not moved to the same height as the ICP monitor) then an HPG is created. The net effect of the HPG is that it acts against the arterial pressure and can cause significant errors in calculated CPP if not corrected. For example, in a man of average height, if the distance between the transducers is 40 cm, the difference in height is 20 cm and the head is tilted at 30°, then an HPG of 14.9 mmHg is created; this results in an error of 25 % in the subsequent CPP reading.
To avoid errors in CPP, it is recommended that the arterial pressure transducer be positioned at the level of the external auditory meatus (EAM) and not at the level of the heart [5]. However, clinical practice surveys have found that blood pressure measurements are often still recorded at the level of the heart [4, 6]. Many centres attempt to correct for HPG by instructing the bedside nurse to move the arterial pressure transducer so that it is at the same height as the ICP transducer; however, it can be difficult to achieve a high level of accuracy doing this manually. Existing fluid-filled catheter transducer system technology for measuring HPG does not lend itself well to either ease of use or low monitoring attendance by bedside nurses in the intensive care environment. What is required is nonintrusive technology that can detect the position of a patient’s head, allowing for automatic corrections of CPP to be made.
In this work we describe an investigation into the application of speckled computing [8], for the automatic monitoring of a patient’s head position relative to an arterial pressure transducer. Speckled computing is a term for the use of very small sensors (or specks) that are able to sense and process information, and to communicate wirelessly with each other or a base station. The use of speckled computing in medicine has previously been demonstrated in the accurate remote monitoring of respiratory rate and flow in patients [1, 3].
Once we are able to establish a patient’s head position using speckled computing it is hoped that we can use this information to automatically calculate HPG and to subsequently generate more accurate CPP readings. This paper describes the initial pilot study applying this technology and evaluates the accuracy of HPG values generated from prototype software.
Materials and Methods
Four subjects and one dummy subject had a prototype speck, contained in a plastic case measuring approximately 5 × 3 cm, placed on their head just above the EAM, and another prototype speck placed on their chest wall approximately level with their heart (Fig. 1). The distance between the chest speck and the subject’s neck and head was recorded. Each speck contains a triaxial accelerometer that is sampled by an on-board analogue-to-digital converter and transmitted using a transceiver.
A fluid-filled catheter, attached to a pressure transducer and connected to a patient monitoring system, was placed on the subject’s head to generate a value for the HPG associated with head position. The bed was tilted through a series of head-up tilt positions and the reported HPG was noted. The head-up tilt positions ranged in increments of 5 mmHg from 0 to 25 mmHg (a total of five readings per subject).
Throughout each of the head-up tilt positions, each speck continuously reported its position via Bluetooth to a base station. A computer program was developed to interpret the data reported by the specks, calculating the height of the patient’s head and the patient’s HPG.
Each speck reports data in a vector consisting of three planes {x, y, z}. At the start of each experiment, when the bed was flat, the specks are zeroed, resulting in the following vector: {0, 0, 0} for each speck. As the bed is tilted, a speck ends up at the coordinate x = {i, j, k}. To automatically determine the height of the patient’s head from these readings, the computer program proceeds through the stages described below.
Smoothing the Data
As the raw positional data reported by the speck is at a high frequency, to reduce the complexity of this data, a moving average algorithm is applied to smooth the data and reduce it to one reading per second (1 Hz).
Scaling the Speck Vectors
The vectors that are returned from the two speck devices are localised to their own coordinate systems. While this is fine for the calculation of angles that are independent of the real world coordinate, this is not the case for our application; consequently the vectors from each speck need to be scaled appropriately. Assuming that the lengths of the head and body segments have been measured and are equal to Ln and L6 respectively and the vectors returned by each speck are
and
, then the resultant vector for both body and head position is:
h
h respectively:
h
To convert each speck vector to the world coordinates they are scaled by L6∕||S6|| and Ln∕||Sn|| respectively:
Calculating the Change in Angle
After scaling the vectors, the reference vector is considered to be the first row of positional data taken from the speck. Subsequent vectors of speck data are then compared against the reference vector to determine the change in angle. The following equation captures this calculation:
Calculating the Hydrostatic Pressure Gradient
For each vector comparison, the resulting change in angle is converted into radians and from this the height of the patient’s head is calculated. This height value is then used to calculate the HPG at that moment in time.
Results
The HPG value calculated by the computer program was compared against the HPG recorded during the experiment. Figure 2 shows a typical output from this comparison. Table 1 displays the average difference between the actual HPG (in mmHg) and the automatically generated value in each of the bed tilt positions for each subject. Although the specks continuously reported the positional data throughout the duration of the experiment, we have only compared the HPG values during the stable middle third of data reporting for each bed tilt; the other two thirds of data were likely to be associated with the movement of the bed between bed tilt positions.
The difference between HPG values varied throughout each experiment and ranged from approximately 0–15 mmHg in the dummy subject and subjects 1, 2 and 4. As to be expected, the dummy produced the strongest results as there is little or no noise generated by other movements of the subject. When the experiment is performed on the other subjects, there is slightly more noise generated by subtle movements to take into consideration. In subject 3, we recorded much higher error rates. However, during this particular experiment, the speck positioned on the subject’s head became loose during the experiment and at times lost attachment to the subject, leading to inaccurate readings being generated.
Discussion
Standard practice in the management of TBI includes the optimization of CPP [2]. Manual adjustment of the arterial pressure transducer introduces the risk of error in this measurement. Technology that could automate the calculation of the HPG would result in continuous correction of CPP for patient position changes and could reduce the demand on nursing time.
The early work reported here is encouraging; the technology clearly has the potential to enable accurate recording of HPG (Fig. 2). However, for each subject, at times, the calculated HPG was significantly over- or underestimated compared with the actual HPG. This may be because the specks became loose, or because we are reporting position data during the transition from one bed tilt position to another, which will not be accurately recorded until the bed is in position. Future work plans include repeating this experiment with an increased number of participants and tighter experimental controls.
Speckled computing also has the future potential to be applied to a number of other areas in the treatment of TBI, for example, in the automatic monitoring of respiratory rates [3], the automatic detection of other types of patient movement (e.g. a patient being turned in the bed) and the automatic detection and recording of treatments administered to a patient.
References
Bates A, Ling M, Geng C, Turk A, Arvind DK (2011) Accelerometer-based respiratory measurement during speech. Proceedings of international conference of body sensor networks (BSN)
Brain Trauma Foundation, American Association of Neurological Surgeons, Congress of Neurological Surgeons et al (2007) Guidelines for the management of severe traumatic brain injury. IX. Cerebral perfusion thresholds. J Neurotrauma 24(Suppl 1):S59–S64
Drummond GB, Bates A, Mann J, Arvind DK (2013) Characterization of breathing patterns during patient-controlled opioid analgesia. Br J Anaesth Dec 111(6):971–978
Kofke WA, Kosty J, Kumar M, Levine J (2011) Comparison of clinician practices for measuring cerebral perfusion pressure: a review of the literature and survey of members of the Neurocritical Care Society. J Neurosurg Anesthesiol 23:400
Matta BF, Menon DK, Turner JM (2000) Textbook of neuroanaesthesia and critical care. Cambridge University Press, Cambridge
Nates JL, Niggemeyer LE, Anderson MB, Tuxen DV (1997) Cerebral perfusion pressure monitoring alert! Crit Care Med 25:895–896
Zhong J, Dujovny M, Park H, Perez E, Perlin A, Diaz F (2003) Advances in ICP monitoring techniques. Neurol Res 25:339–350
http://www.specknet.org/. Accessed 20 Dec 2013
Acknowledgements
The authors would like to acknowledge the work of the BrainIT group investigators and participating centres in the BrainIT data set, without whom this work could not have been conducted: Barcelona, Spain: Prof Sahuquillo; Cambridge, UK: Prof Pickard; Edinburgh, UK: Prof Whittle; Glasgow, UK: Mr Dunn; Gothenburg, Sweden: Dr Rydenhag; Heidelberg, Germany: Dr Kiening; Iasi, Romania: Dr Iencean; Kaunas, Lithuania: Prof Pavalkis; Leipzig, Germany: Prof Meixensberger; Leuven, Belgium: Prof Goffin; Mannheim, Germany: Prof Vajkoczy; Milan, Italy: Prof Stocchetti; Monza, Italy: Dr Citerio; Newcastle upon Tyne, UK: Dr Chambers; Novara, Italy: Prof Della Corte; Southampton, UK: Dr Hell; Uppsala, Sweden: Prof Enblad; Turin, Italy: Dr Mascia; Vilnius, Lithuania: Prof Jarzemaskas; Zurich, Switzerland: Prof Stocker.
Conflict of Interest
There are no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Moss, L., Shaw, M., Piper, I., Arvind, D.K., Hawthorne, C. (2016). Automatic Calculation of Hydrostatic Pressure Gradient in Patients with Head Injury: A Pilot Study. In: Ang, BT. (eds) Intracranial Pressure and Brain Monitoring XV. Acta Neurochirurgica Supplement, vol 122. Springer, Cham. https://doi.org/10.1007/978-3-319-22533-3_52
Download citation
DOI: https://doi.org/10.1007/978-3-319-22533-3_52
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-22532-6
Online ISBN: 978-3-319-22533-3
eBook Packages: MedicineMedicine (R0)