Abstract
In patients with subarachnoid haemorrhage, pulsatile intracranial pressure (ICP) is more strongly associated with adverse events than mean ICP. Furthermore, patients with idiopathic normal-pressure hydrocephalus (iNPH), and pulsatile ICP of 5 mmHg or more, gain more benefit from cerebrospinal fluid (CSF) shunting than those whose pulsatile ICP is lower than 5 mmHg.
Our study aims to investigate the morphological relationship between ICP pulsations, aortic pressure pulsations and radial artery pulsations. Central aortic pulse pressure has been known to be the best predictor of adverse cardiac events, whereas radial artery pulse pressure is generally measured and displayed in intensive care environments.
We studied 10 patients with iNPH, and their ICP and aortic and radial pressures were digitised, ensemble-averaged and compared in the time and frequency domains. The ICP wave contour was quite different to the radial pressure waveform. By contrast, the ICP waveform was similar to the aortic pressure wave contour. The ICP amplitude averaged <10 % of aortic pulse pressure. In the frequency domain, the relative amplitude of the first three harmonics was similar for the ICP and aortic pressure. Hence, monitoring central aortic pressure through derivation from the radial pressure wave is superior to measurement of radial pressure alone.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Pulsations of pressure in the brain or in the aorta are directly related to cardiovascular and cerebrovascular adverse events. Central aortic pulse pressure is the best blood pressure predictor of cardiac events [1]. For the brain, pulsatile intracerebral pressure is more closely related to adverse events than mean pressure following subarachnoid haemorrhage or head injury [2, 3]. In patients with idiopathic normal-pressure hydrocephalus (iNPH), more benefit is gained from cerebrospinal fluid (CSF) shunting in those with higher (>5 mmHg) than in those with lower (≤5 mmHg) pulsatile intracranial pressure (ICP) [4].
Lacunar artifacts are more prevalent among people whose carotid arterial pressure or flow waves show greater late systolic augmentation [5–7]. Patients with lower aortic pressure augmentation during systole have better survival prospects following head injury than those with high augmentation [3]. High-pressure augmentation is the most common cause of isolated systolic hypertension in older persons, and the most common cause of cardiac failure and stroke [1]. Both flow and pressure augmentation are markedly reduced by the systemic arterial vasodilator nitroglycerine, with little effect on mean pressure or flow [3, 6, 8].
This study seeks to clarify the relationship among ICP pulsations, central aortic pressure pulsations and pulsations in the radial artery, where pressure is most conveniently measured in intensive care situations.
Materials and Methods
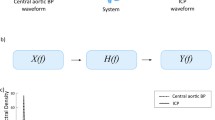
Ten patients with iNPH had ICP measured by a Codman catheter system, simultaneous with radial pressure before therapeutic CSF shunting to the peritoneal cavity. The central aortic pressure waveform was estimated from the radial pressure waveform using a US Food and Drug Administration–validated generalised transfer function [3]. The three pressure waveforms were digitised, ensemble-averaged and then compared in the time and frequency domains. Details of patients are given in Table 1.
Results
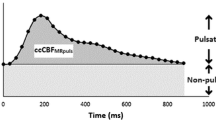
In these iNPH patients, mean ICP was within the normal range (−7.1 to 9.9 mmHg), and pressure pulsations were of low amplitude (2.9–12.0 mmHg), on average <10 % of aortic pulse pressure. The ICP wave contour was quite different from the radial pressure wave contour. In all radial waveforms, the initial systolic peak, some 100 ms after the foot of the wave, was lower than the second systolic peak, whereas the ICP second systolic peak was dominant in all patients, averaging 35 % of total waveform height. In contrast to the radial waveform, the central aortic pressure waveform was almost identical to the ICP waveform, at least during the period of systole, and the augmentation index (height of the secondary wave ÷ amplitude of the wave) was 30 % and similar to that of ICP (Fig. 1). In the frequency domain, relative amplitudes of the first to third harmonics were similar for the aortic and ICP waveforms (p = 0.55, modulus; p = 0.14, phase).
Discussion
There are many reasons why the central aortic pressure wave is preferred to the radial pressure wave for monitoring cerebral vascular haemodynamics. These include:
-
1.
The radial aortic pressure wave is normally amplified by up to 70 % in the upper limb (Fig. 1); thus, the radial artery pulse pressure may be 5–25 mmHg greater than the central aortic pulse pressure. Amplification depends on the shape of the aortic and radial waveforms, and is corrected through use of the generalised transfer function process [3].
-
2.
The aortic pressure waveform is similar to that in the carotid and vertebral arteries, and is the waveform that dilates the cerebral arteries with each beat of the heart, thereby generating the ICP waveform.
-
3.
The pressure (and flow) waveforms that perfuse the brain have two components; the first an impulse generated by ventricular ejection, with a peak some 100 ms after the foot of the wave, and the second a broader, wider wave that boosts (augments) pressure during the latter part of systole and contributes at least in these patients, almost half of the pressure wave amplitude. The importance of this wave, caused by wave reflection from the lower part of the body, is not apparent on the radial artery tracing because (at least in these older subjects) it is not as high as the initial pressure wave. The aortic pressure waveform provides a better guide to the stresses that are applied to the cerebral vasculature than the radial wave.
-
4.
Reduction in wave reflection from the lower body is readily achieved with arterial (in contrast to arteriolar) vasodilators, such as nitroglycerine. This can reduce wave reflection from the lower body by 60 % or more (Fig. 2), thereby markedly reducing pressure and flow pulsations in the aorta and cerebral arteries [9]. The ill-effects of central pressure pulsations on the cerebral vasculature are readily apparent from the contour of the aortic waveform. There is every reason to believe that reducing wave reflection from the lower body with drugs such as nitroglycerine improves recovery from cerebral insults, as has already been shown for the heart [6, 8]. This has yet to be confirmed for the brain, but it is a definite possibility, and one that can be readily monitored by the measurement of intracranial and central aortic pressure in routine intensive care.
Fig. 2 Effect of nitroglycerine on pressure waveforms, as published in Pauca et al. [9]
In conclusion, monitoring of central aortic pressure through the use of radial pressure wave convolution is superior to radial pressure wave monitoring, because:
-
1.
It eliminates the variable amplification between the aorta and the radial artery under different conditions and in different subjects.
-
2.
It closely corresponds to the contour of the ICP, at least during systole
-
3.
It identifies a surge of pressure with each heart beat, which is potentially injurious to the vasculature of a damaged brain
-
4.
It can be used to monitor the potentially beneficial effects of drugs that reduce wave reflection.
References
Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Bohm M, Christiaens T, Cifkova R, DeBacker G, Dominiczak A, Galderisi M, Grobbee DE, Jaarsma T, Kirchhof P, Kjeldsen SE, Laurent S, Manolis AJ, Nilsson PM, Ruilope LM, Schmieder RE, Sirnes PA, Sleight P, Viigimaa M, Waeber B, Zannad F (2013) 2013 ESH/ESC Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens 31:1281–357
Eide PK, Sorteberg A, Bentsen G, Marthinsen PB, Stubhaug A, Sorteberg W (2012) Pressure-derived versus pressure wave amplitude-derived indices of cerebrovascular pressure reactivity in relation to early clinical state and 12-month outcome following aneurysmal subarachnoid hemorrhage. J Neurosurg 116:961–71
Nichols WW, O’Rourke MF, Vlachopoulos C (2011) McDonald’s blood flow in arteries, 6th edn. Arnold Hodder, London
Eide PK, Park EH, Madsen JR (2010) Arterial blood pressure vs intracranial pressure in normal pressure hydrocephalus. Acta Neurol Scand 122:262–9
Hirata K, Yaginuma T, O’Rourke MF, Kawakami M (2006) Age-related change in the carotid artery flow and pressure pulses implications to cerebral microvascular disease. Stroke 37:2552–6
Hirata K, O’Rourke MF, Momomura S (2007) Favourable effect of sublingual nitrate on carotid flow and pressure augmentation index. J Clin Hypertens 9(Suppl A):A29
Hirata K, O’Rourke MF, Momomura S (2008) Flow augmentation index as a major risk factor for silent lacunar infarction. J Hypertens 26(Suppl 1):S395
Pauca AL, O’Rourke MF, Kon ND (2001) Prospective evaluation of a method for estimating ascending aortic pressure from the radial artery pressure waveform. Hypertension 38:932–7
Pauca AL, Kon ND, O’Rourke MF (2005) Benefits of nitroglycerine on arterial stiffness is directly due to effects on peripheral arteries. Heart 91:1428–32
Conflict of Interest Statement
Dr O’Rourke is a founding director of AtCor Medical P/L, manufacturer of the pulse wave analysis system, SphygmoCor, and of Aortic Wrap P/L, the developer of methods to reduce aortic stiffness, and is consultant to Novartis and Merck. Other authors have nothing to disclose.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Kim, M.O., Eide, P.K., O’Rourke, M.F., Adji, A., Avolio, A.P. (2016). Intracranial Pressure Waveforms are More Closely Related to Central Aortic than Radial Pressure Waveforms: Implications for Pathophysiology and Therapy. In: Ang, BT. (eds) Intracranial Pressure and Brain Monitoring XV. Acta Neurochirurgica Supplement, vol 122. Springer, Cham. https://doi.org/10.1007/978-3-319-22533-3_12
Download citation
DOI: https://doi.org/10.1007/978-3-319-22533-3_12
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-22532-6
Online ISBN: 978-3-319-22533-3
eBook Packages: MedicineMedicine (R0)