Abstract
As the number of elderly continues to increase worldwide, age-related neurological disorders, such as Alzheimer’s disease and vascular dementia, are a growing concern. In some cases, vascular dementia and cognitive decline in aging are associated with nutritional status and elevated homocysteine, suggesting that improving nutritional status can play a meaningful role in the prevention of cognitive impairment. The research described in this chapter represents current understanding on the relationships of folate and vitamin B12 nutritional status with cognitive function and dementia in adults and elderly. Low B vitamin status is associated with increased homocysteine levels and there is evidence that insufficient B vitamin intake is associated with lower cognitive scores in comparison to adequate intake. However, higher rates of cognitive decline have been reported with high levels of folate and folic acid intake in adults, and memory performance may be impaired with high folate intake in individuals with low vitamin B12 status. Overall, studies reported lower folate blood levels and a higher prevalence of deficiency among subjects with dementia. In general, vitamin B12 serum levels were lower in patients with dementia relative to nondemented individuals; however, this relationship was not as consistent as that for folate. Subsequent to mandatory folic acid fortification, stroke mortality has decreased at a greater rate in the USA and Canada, suggesting a positive effect of fortification on cerebrovascular health. Interventions with folic acid and with combinations of B vitamins were able to improve cognitive function or prevent decline, especially in subjects with low nutrient status. As with the data for blood nutrient levels, evidence that vitamin B12 treatment improves cognitive function is conflicting and less positive.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Aging
- Alzheimer’s disease
- B vitamins
- Cerebrovascular disease
- Cognition
- Dementia
- Folate
- Folic acid
- Vitamin B6
- Vitamin B12
-
Cognitive decline in aging is associated with small vessel abnormalities and nutritional status, notably with folate, vitamin B12 and with elevated homocysteine.
-
Homocysteine levels can be lowered through nutritional supplementation with B vitamins including folic acid, vitamin B12, and vitamin B6.
-
Blood levels of folate are more strongly associated with cognitive function.
-
Intervention trials with B vitamins have shown mixed findings with respect to cognitive performance.
-
Supplementation with adequate doses of B vitamins appears to be effective in preventing cognitive decline in individuals with low nutrient intake and status.
1 Introduction
As the number of elderly in the USA and globally continues to increase, age-related neurological disorders, such as Alzheimer’s disease and vascular dementia , are a growing concern. The loss of memory, emotional changes, and impairments in general cognitive functioning frequently result in social isolation, loss of independence, and institutionalization. However, cognitive decline is not an inevitable consequence of growing old. Indeed, although some forms of cognitive disorders may have a genetic component, cognitive decline is also influenced by nutritional factors and may be secondary to nutritionally mediated conditions such as diabetes or vascular disease. As such, there is a strong need to identify modifiable nutritional factors that regulate the proper maintenance of brain function to facilitate healthy aging.
The relationship between diet and vascular disease is well established. The nutritional foundation of cardiovascular disease prevention is a diet high in fruits and vegetables and fiber and low in saturated fat. One of the prevailing risk factors for cardio- and cerebrovascular disease is elevated blood levels of homocysteine. Plasma homocysteine may be considered a functional indicator of B vitamin status, including that of folate and vitamin B12 and, to a lesser extent, vitamin B6. High plasma homocysteine concentrations can be largely attributed to inadequate status of these vitamins [1]. Data from several laboratories indicate that plasma homocysteine increases with age independent of vitamin status and that hyperhomocysteinemia is highly prevalent in the elderly. Several studies have shown consistent and strong relationships between homocysteine concentration, heart disease, and other vascular outcomes including cerebrovascular disease [2, 3].
2 Vascular Cognitive Impairment and Dementia
Individuals at high risk for vascular disease are also at greater risk for cognitive decline [4]. Vascular cognitive impairment ranges in severity from subtle neuropsychological deficits to frank dementia and frequently coexists with and possibly contributes to other neurodegenerative conditions such as Alzheimer’s disease [5]. Where memory loss is often the first clinical indication of Alzheimer’s disease, loss of executive function—the cognitive domain that includes planning, cognitive flexibility, and inhibition of inappropriate actions—may be a marker for vascular cognitive impairment or dementia [6]. Epidemiological studies have shown that while case-mortality of stroke has decreased over the past three decades, the rate of stroke has not changed significantly over time, and the risk of dementia after stroke has increased substantially [7]. Better understanding of potentially modifiable risk factors for vascular disease can aid in developing long-term intervention strategies for controlling or preventing the cognitive dysfunction attributable to large and small vessel cerebrovascular disease [4].
There is some evidence that small vessel disease is the most common cause of vascular cognitive impairment [8]. The presence of silent brain infarcts on MRI increases the risk of dementia and predicts a steeper decline in cognitive function [9]. White matter hyperintensities (WMHI ), which are also thought to primarily reflect small vessel disease, have been shown to be associated with cognitive impairment [8], although this finding is not always consistent [10]. Mild to moderate elevation of plasma homocysteine concentration has been implicated as a risk factor for cardiovascular disease [11], stroke [12], dementia [13], and cognitive impairment [14–16]. While research had initially focused on the relationship between homocysteine, atherosclerosis, and large vessel disease [12], some have suggested that homocysteine is a greater risk factor for small vessel disease as opposed to other subtypes of stroke [16–19]. Not all studies, however, have been able to confirm this finding [20]. While the mechanisms underlying small vessel disease are not entirely clear, chronic endothelial dysfunction may play a role. Homocysteine has been found to be toxic to the endothelium both in vitro [21] and in vivo [18], giving biological plausibility for a role as an independent risk factor. In a study by Pavlovic and colleagues [22] homocysteine levels were strongly associated with cognitive and functional status and the severity of WMHI in patients with cerebral small vessel disease.
3 B Vitamins, Homocysteine, and Brain Function
Possible biochemical interpretations of the putative effects of low B vitamin status and high homocysteine on cognitive decline can be made on the basis of one-carbon metabolism (Fig. 17.1). Folate serves as a carrier of one-carbon groups for the methylation cycle. In this cycle, methionine with its available methyl group is activated by adenosine triphosphate to form S-adenosylmethionine, which is the universal methyl donor in a multitude of methyl transfer reactions including many that are of vital importance to central nervous function. Through the transfer of its methyl group, S-adenosylmethionine is converted to S-adenosylhomocysteine, which is hydrolyzed to homocysteine. Homocysteine can regenerate methionine for an additional methylation cycle by acquiring a new methyl group from methyl tetrahydrofolate in a reaction that is catalyzed in all tissues by vitamin B12-requiring methionine synthase [23]. Excess intracellular homocysteine can also be removed from the methylation pathway by conversion to cystathionine in the trans-sulfuration pathway or through export into circulation [23]. It has been proposed that cognitive impairment in the elderly is due in part to vasotoxic effects of homocysteine and/or to impaired methylation reactions in brain tissue [24]. While it has yet to be determined if hyperhomocysteinemia is a cause of vascular disease or indicative of some other physiological change leading to vascular damage, current data demonstrate that homocysteine is strongly associated with cognitive dysfunction in aging [14, 25, 26].
Use of S-adenosylmethionine as the methyl donor for biological methylation reactions results in the formation of S-adenosylhomocysteine. Homocysteine is formed from the hydrolysis of S-adenosylhomocysteine. Homocysteine may be remethylated to form methionine by a folate-dependent reaction that is catalyzed by methionine synthase, a vitamin B12-dependent enzyme. Alternately, homocysteine may be metabolized to cysteine in reactions catalyzed by two vitamin B6-dependent enzymes (Adapted from [27])
4 B Vitamin Deficiency and Cognitive Impairment
It has long been known that severe deficiency of vitamins such as niacin, vitamin B12, and thiamine causes cognitive impairment [2] and that replacement of deficient nutrients can prevent or ameliorate those forms of cognitive impairment that are caused by deficiency (i.e., [28]). While more severe vitamin deficiencies or congenital defects are not common in the USA, these milder subclinical B vitamin deficiencies are prevalent in the elderly [14, 29, 30]. Decreased intestinal absorption and poor appetite contribute to these subclinical deficiencies. Studies suggest that even moderately low or subclinical levels of B vitamins are associated with cognitive impairment, dementia, and other psychiatric disorders [31–33].
Extensive research supports the hypothesis that B vitamin deficiencies moderate cognitive brain functioning through effects on cerebrovascular health, DNA synthesis, and neurotransmitter metabolism [2, 34]. Vitamin B12 and folate are closely linked in the methylation process, such that a B12 deficiency can lead to a secondary folate deficiency through a decrease in the retention of folate. It is proposed that low levels of B12 are linked with peripheral neuropathy and subacute combined degeneration of the spinal cord, whereas folate may have more of a role in cognition and mood, perhaps through effects on serotonin, dopamine, and noradrenergic systems [34, 35].
5 Dietary B Vitamins and Cognition
In a seminal study, healthy, independently living elderly individuals with subclinical malnutrition (i.e., low dietary intake of protein and selected vitamins including vitamin B12) scored lower on tests of verbal memory and nonverbal abstract reasoning than did their peers with normal intake [36]. However, subsequent studies have yielded conflicting results with respect to nutrient intake and cognitive function. In a prospective cohort study [37] examining the relation between nutritional intake and daily functioning, dietary intakes were not associated with a change in functional decline over a 6-month period in nursing home residents. In a retrospective case–control study [38] comparing patients with Alzheimer’s disease with healthy controls, cases and controls were asked to recall their past food consumption using a food-frequency questionnaire during three age periods: 20–39, 40–59, and 60 or more years of age. It was found that those with Alzheimer’s disease had lower mean dietary intakes of vitamin B6 and folate than controls in the over-60 age group, but not in younger age groups. However, there was no relationship between either folate intake and homocysteine levels or homocysteine levels and cognitive status. Finally, adding to the complexity of these findings, some research [39] shows a slower decline in cognitive test performance over a 6-year period in subjects with high vitamin B12 intake but faster decline among subjects with a high folate intake (>400 μg/day) from either food sources or supplements.
6 B Vitamin Blood Level Associations with Cognition and Dementia
Poor B vitamin status and/or high homocysteine is associated with poorer cognitive performance [15, 40–43]. Previous studies have found that patients with dementia, especially those with Alzheimer’s disease, have lower serum concentrations of B vitamins [14, 44, 45]; moreover, serum levels of these micronutrients are associated with the severity of the disease [46]. Several cross-sectional studies have found that patients with Alzheimer’s dementia had significantly higher levels of serum total homocysteine than did age-matched hospitalized controls [34, 47] and healthy community-dwelling elderly individuals [47, 48]. In a longitudinal study, higher levels of homocysteine in Alzheimer’s patients were associated with greater progression of hippocampal atrophy as measured by medial temporal lobe thickness, as well as a similar trend in Mini Mental State Evaluation score decline [49]. More recent studies have found inconsistent results with respect to the predictive value of high homocysteine or low B vitamin status and cognitive performance in the elderly [50, 51].
7 Vitamin B12
A number of studies have investigated a potential correlation between serum vitamin B12 levels and cognitive function or diagnosis of several types of dementia and cognitive impairment [52]. Most of these studies have focused on Alzheimer’s disease. Based on longitudinal studies, serum vitamin B12 levels did not affect the risk of developing Alzheimer’s disease or dementia. The existing evidence from studies that implemented a cognitive function assessment instrument did not support any correlation between serum vitamin B12 levels and cognitive function. Among cross-sectional studies, there was a tendency for vitamin B12 serum levels to be lower in patients with Alzheimer’s disease or other types of dementia, which in certain studies reached statistical significance. However, this trend was not consistent. Finally, an inverse relationship between vitamin B12 levels and duration of Alzheimer’s disease has been reported. In general, evidence from longitudinal cohort and case–control studies suggests that there is no significant association between blood concentrations or the dietary intake of vitamin B12 and cognitive test performance or the progression of Alzheimer’s disease. Although some studies reported higher vitamin B12 blood concentrations to be associated with better cognitive test performance, no consistent pattern of association with a particular cognitive domain has been reported.
8 Folate
With respect to folate, Miller and colleagues [53] showed that blood folate levels are predictive of homocysteine levels. Elevated homocysteine levels , in turn, are associated with poorer performance on several cognitive tasks. In this study, however, there was no clear relationship between folate status and cognitive performance. Teunissen and colleagues [54] found that serum levels of homocysteine were negatively correlated with verbal learning and memory at baseline testing only, whereas higher serum folate levels were associated with better delayed recall performance. Elevated homocysteine was associated with poorer functioning on several cognitive tasks looking at immediate recall, attention, and performance during a 6-year follow-up period and there were no further associations with folate status. Morris and colleagues [42, 55] reported similar findings with respect to folate and recall. Folate status was positively correlated with recall performance. Moreover, elevated levels of homocysteine were associated with poor recall. When looking at folate and homocysteine levels, low folate levels in combination with higher levels of homocysteine (above the 80th percentile) were associated with significantly poorer performance than low folate or lower homocysteine levels alone [55].
Recent research shows an association with folate levels and mild cognitive impairment (MCI) and some forms of dementia . In these studies, people with the lowest serum levels of folate were at greater risk for Alzheimer’s disease, MCI, and dementia. Snowdon and coworkers [46] examined atrophy in the brains of deceased nuns with Alzheimer’s disease and compared these data with serum folate levels that had been determined earlier in the nuns’ lives. They found an inverse relationship between folate status and severity of atrophy. This effect was seen even in participants without significant atherosclerosis or brain infarcts, suggesting further that the role of folate is not limited to its relationship with homocysteine and homocysteine’s putative vascular effects. While there is abundant evidence to indicate an association between folate status and the development or progression of cognitive decline or dementia, a causative role is not clear-cut. On the one hand, some data suggest that folate inadequacy precedes onset of cognitive impairment or dementia. On the other hand, there is evidence to suggest that dietary intakes of folate are lower in people with Alzheimer’s disease. In contrast to the data on vitamin B12, the majority of studies evaluating blood folate concentrations reported a positive association between low folate levels and poor cognitive test performance.
9 Fortification with Folic Acid and Cerebrovascular Effects
A number of countries have instituted mandatory folic acid fortification of wheat flour and cereal grains, with the aim of reducing neural tube defects in developing fetuses. Fortification has not been implemented in many countries, particularly in Europe, due in part to concerns about the potential for high levels of folic acid intake to exacerbate the neurological consequences of a vitamin B12 deficiency. Indeed, some of the research discussed in this chapter suggests that high levels of folate or folic acid in people with low vitamin B12 status have negative effects on memory and cognition. However, in the USA, since the initiation of fortification, positive effects have been seen with respect to increased blood folate levels and reduced homocysteine levels [56–58]. As described above, homocysteine levels are associated with severity of cerebrovascular disease, including stroke and cerebral atherosclerosis. Furthermore, low folate and high homocysteine are known risk factors for vascular disease, and population-wide reduction of these risk factors may be proposed to reduce incidence of vascular disease, stroke, and subsequent vascular dementia. Supporting this proposal, there has been a reduction in cardiovascular and stroke mortality in the USA and Canada since the introduction of folic acid fortification [59]. It remains to be seen whether folic acid fortification is associated with a change in the incidence of vascular dementia and cognitive decline.
10 Intervention Trials with B Vitamins
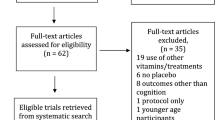
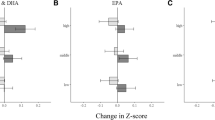
High-dose supplementation with B vitamins, particularly in combination, can decrease homocysteine levels, but the effects on cognition are not clear-cut and the results of intervention trials vary [60]. A study of high-dose supplementation with a combination of vitamins B12, B6, and folic acid in mild to moderate Alzheimer’s disease found no effect on cognitive decline over 18 months [61]. A few studies have shown worsening of cognitive functioning following B vitamin intervention [62–64]. Others, however, have shown benefit. In a study of community dwelling elders, homocysteine lowering with 800 μg daily oral folic acid for 3 years had a beneficial effect on memory, information processing speed, and sensorimotor speed [65]. A recent study has also shown that homocysteine lowering with vitamins B6, B12, and folic acid was efficacious in slowing the rate of brain atrophy and cognitive decline in those individuals with amnestic or non-amnestic MCI [66, 67].
There is some evidence that the effect of B vitamin supplementation on cognitive function may depend on nutritional status at baseline. For example, Bryan and colleagues [68] provided women with 750 μg folate for 35 days and conducted cognitive and mood tests pre- and post-supplementation. They found that folate significantly improved performance in a speed-of-processing task for women with initially lower folate levels. In younger women, they found that folate significantly enhanced recall for those with initially lower folate levels. However, the effects of folate supplementation were not consistent across the study or across different age groups. In a trial of B vitamin supplementation in women with or at risk for cardiovascular disease, the results showed no B vitamin supplementation on cognition in women with sufficient dietary intake of B vitamins at baseline, but found that supplementation appeared to preserve cognition among women with low baseline dietary intake [69].
In older adults with cognitive decline, baseline nutrient status or plasma total homocysteine concentrations may also modify the effects of B vitamin supplementation. In a 1997 study by Fioravanti et al. [70], 30 older adults with “abnormal cognitive decline” and folate levels below 3 ng/mL were supplemented with folic acid for 60 days. Their results showed significant improvement in memory and attention efficiency when compared with a placebo group, and found that the degree of improvement in memory was positively correlated with baseline severity of folate deficiency. Nilsson and colleagues [71] studied vitamin B12 and folic acid supplementation in older patients with mild-to-moderate dementia. Performance on cognitive tasks was measured before and after 2 months supplementation with 5 mg/day folic acid and 1 mg/day cyanocobalamin. They found that in patients with elevated homocysteine, vitamin supplementation decreased homocysteine levels and patients improved on measures of attention, memory, and orientation. Similarly, de Jager and her colleagues [67] evaluated the efficacy of homocysteine lowering with B vitamins on cognitive function in individuals with MCI. While there was an overall treatment effect for executive function, there was an interaction with baseline plasma total homocysteine where those participants with homocysteine levels above 11.3 μmol/L and in the active treatment group had significant benefit in global cognition, episodic memory, and semantic memory. The same study showed a similar interaction between treatment and baseline homocysteine status in the MRI measurement of loss of gray matter over 2 years [72].
There are several considerations in interpreting the findings on vitamin supplementation and cognition. First, as outlined above, the relationship between baseline nutrient status and homocysteine status should be considered. Second, there is no standard dose of vitamin or duration of treatments that is recommended for this type of trial. Third, many trials may have had too few participants to sufficiently determine an effect on cognitive performance. Finally, in people with dementia or other cognitive impairment, the severity of impairment alone is of importance. For example, Nilsson and colleagues [71] excluded severely demented patients from their study because the patients were unable to complete testing either before or after supplementation. As a correlative, the ability of vitamin supplementation to offset existing cognitive decline is somewhat dependent upon the duration and consequent irreversibility of cognitive decline.
11 Conclusions
The evidence for an association between elevated plasma homocysteine and cognitive dysfunction is compelling. Elevated plasma total homocysteine has been reproducibly linked to diseases of the aging brain including subtle age-related cognitive decline, cerebrovascular disease and stroke, vascular dementia, and Alzheimer’s disease. Nevertheless, it is unclear whether elevated homocysteine mediates or is otherwise associated with vascular brain aging. Epidemiological data provide the basis for a hypothesis implicating homocysteine as a mediator of vascular and neuronal pathology. If this is true, then homocysteine-lowering therapies could reduce the incidence of cognitive decline, stroke, and dementia. The evidence for this is not consistent. Highlighting the importance of prevention, some research shows that supplementation with B vitamins, while successful at lowering homocysteine, is not beneficial in mediating cognitive function in individuals with irreversible compromised brain function. However, the role of homocysteine lowering in the long-term prevention of cognitive decline, whether via promotion of vascular health or via direct neural effects, has yet to be adequately established.
The research described in this chapter represents current understanding on the relationships of folate and vitamin B12 nutritional status with cognitive function and dementia in adults and elderly. There is evidence that insufficient B vitamin intake is associated with lower cognitive scores in comparison to adequate intake. Low B vitamin status is associated with increased homocysteine levels. However, higher rates of cognitive decline have been reported with high levels of folate and folic acid intake in adults, and memory performance may be impaired with high folate intake in individuals with low vitamin B12 status. Overall, studies reported lower folate blood levels and a higher prevalence of deficiency among subjects with dementia. In general, vitamin B12 serum levels were lower in patients with dementia relative to nondemented individuals; however, this relationship was not as consistent as that for folate. Stroke mortality has decreased at a greater rate in the USA and Canada subsequent to mandatory folic acid fortification, suggesting a positive effect of fortification on cerebrovascular health. Interventions with folic acid and with combinations of B vitamins were able to improve cognitive function or prevent decline, albeit inconsistently, especially in subjects with low nutrient status. As with the data for blood nutrient levels, evidence that vitamin B12 treatment improves cognitive function is conflicting and less positive.
Overall, there is support for the concept that diets rich in B vitamins, especially folate and vitamin B12, are beneficial in maintaining brain function in aging. Some smaller experimental trials show that supplementation with vitamin B12 and folic acid may prevent cognitive decline or improve cognitive function to some degree, particularly in individuals with low baseline levels of these nutrients. To date, intervention trials indicate that supplementation with B vitamins for a period of 1.5–3 years, even while adequate to reduce circulating levels of homocysteine, may not be sufficient to prevent cognitive decline. Furthermore, some research indicates that high levels of supplementation with folic acid may have negative consequences on cognitive performance in vitamin B12-deficient individuals.
12 Recommendations
Adhering to a diet rich in whole grains, leafy greens, as well as lean meats and low-fat dairy may confer the greatest benefit in prevention of decline and maintaining cognitive function. Moreover, following such a diet should be considered a life-long goal rather than an immediate action to treat current decline. Folic acid supplementation is beneficial in those with folate-deficient diets, but may be harmful at high doses in the presence of low vitamin B12 status. Low B12 status is more prevalent in elders than previously known and steps for prevention need to be considered. Given the high prevalence of populations in the low and marginal folate and vitamin B12 status, the results presented here support the concern that cognitive function and risk of age-related decline represent a nutritionally modifiable public health problem.
References
Selhub J, et al. Vitamin status and intake as primary determinants of homocysteinemia in an elderly population. JAMA. 1993;270(22):2693–8.
Rosenberg IH, Miller JW. Nutritional factors in physical and cognitive functions of elderly people. Am J Clin Nutr. 1992;55(6 Suppl):1237S–43.
Smith AD. The worldwide challenge of the dementias: a role for B vitamins and homocysteine? Food Nutr Bull. 2008;29(2 Suppl):S143–72.
Gorelick PB, et al. Vascular contributions to cognitive impairment and dementia: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2011;42(9):2672–713.
Huang CW, et al. Impact of homocysteine on cortical perfusion and cognitive decline in mild Alzheimer’s dementia. Eur J Neurol. 2013;20(8):1191–7.
Muller M, et al. Brain atrophy and cognition: interaction with cerebrovascular pathology? Neurobiol Aging. 2011;32(5):885–93.
Ukraintseva S, et al. Increasing rates of dementia at time of declining mortality from stroke. Stroke. 2006;37(5):1155–9.
Geerlings MI, et al. Association of white matter lesions and lacunar infarcts with executive functioning: the SMART-MR study. Am J Epidemiol. 2009;170(9):1147–55.
Vermeer SE, et al. Silent brain infarcts and the risk of dementia and cognitive decline. N Engl J Med. 2003;348(13):1215–22.
Stavitsky K, et al. White matter hyperintensity and cognitive functioning in the racial and ethnic minority cohort of the Framingham Heart Study. Neuroepidemiology. 2010;35(2):117–22.
Bostom AG, et al. Nonfasting plasma total homocysteine levels and all-cause and cardiovascular disease mortality in elderly Framingham men and women. Arch Intern Med. 1999;159(10):1077–80.
Yoo JH, Chung CS, Kang SS. Relation of plasma homocyst(e)ine to cerebral infarction and cerebral atherosclerosis. Stroke. 1998;29(12):2478–83.
Seshadri S, et al. Plasma homocysteine as a risk factor for dementia and Alzheimer’s disease. N Engl J Med. 2002;346(7):476–83.
Selhub J, et al. B vitamins, homocysteine, and neurocognitive function in the elderly. Am J Clin Nutr. 2000;71(2):614S–20.
Tucker KL, et al. High homocysteine and low B vitamins predict cognitive decline in aging men: the Veterans Affairs Normative Aging Study. Am J Clin Nutr. 2005;82(3):627–35.
Scott TM, et al. Plasma homocysteine predicts executive dysfunction and MRI findings of cerebrovascular pathology: the Nutrition, Aging, and Memory in the Elderly (NAME) study. In: The 8th International Conference on Homocysteine Metabolism, Lisbon; 2011.
Fassbender K, et al. Homocysteine in cerebral macroangiography and microangiopathy. Lancet. 1999;353(9164):1586–7.
Hassan A, et al. Homocysteine is a risk factor for cerebral small vessel disease, acting via endothelial dysfunction. Brain. 2004;127(Pt 1):212–9.
Kloppenborg RP, et al. Homocysteine and progression of generalized small-vessel disease: the SMART-MR study. Neurology. 2014;82(9):777–83.
Lindgren A, et al. Plasma homocysteine in the acute and convalescent phases after stroke. Stroke. 1995;26(5):795–800.
Wall RT, et al. Homocysteine-induced endothelial cell injury in vitro: a model for the study of vascular injury. Thromb Res. 1980;18(1–2):113–21.
Pavlovic AM, et al. Increased total homocysteine level is associated with clinical status and severity of white matter changes in symptomatic patients with subcortical small vessel disease. Clin Neurol Neurosurg. 2011;113(9):711–5.
Selhub J. Homocysteine metabolism. Annu Rev Nutr. 1999;19:217–46.
Troen A, Rosenberg I. Homocysteine and cognitive function. Semin Vasc Med. 2005;5(2):209–14.
Morris MS, et al. Serum total homocysteine concentration is related to self-reported heart attack or stroke history among men and women in the NHANES III. J Nutr. 2000;130(12):3073–6.
Wald DS, Law M, Morris JK. Homocysteine and cardiovascular disease: evidence on causality from a meta-analysis. BMJ. 2002;325(7374):1202.
Selhub J, Miller JW. The pathogenesis of homocysteinemia: interruption of the coordinate regulation by S-adenosylmethionine of the remethylation and transsulfuration of homocysteine. Am J Clin Nutr. 1992;55(1):131–8.
van Asselt DZ, et al. Cobalamin supplementation improves cognitive and cerebral function in older, cobalamin-deficient persons. J Gerontol A Biol Sci Med Sci. 2001;56(12):M775–9.
Joosten E, et al. Metabolic evidence that deficiencies of vitamin B-12 (cobalamin), folate, and vitamin B-6 occur commonly in elderly people. Am J Clin Nutr. 1993;58(4):468–76.
Lindenbaum J, et al. Prevalence of cobalamin deficiency in the Framingham elderly population. Am J Clin Nutr. 1994;60(1):2–11.
Bell IR, et al. Vitamin B12 and folate status in acute geropsychiatric inpatients: affective and cognitive characteristics of a vitamin nondeficient population. Biol Psychiatry. 1990;27(2):125–37.
Riggs KM, et al. Relations of vitamin B-12, vitamin B-6, folate, and homocysteine to cognitive performance in the Normative Aging Study. Am J Clin Nutr. 1996;63(3):306–14.
Tucker KL, Riggs KM, Siro AL. Nutrient intake is associated with cognitive function: the Normative Aging Study. Gerontologist. 1999;39:149.
Bottiglieri T, et al. Homocysteine, folate, methylation, and monoamine metabolism in depression. J Neurol Neurosurg Psychiatry. 2000;69(2):228–32.
Alpert M, Silva RR, Pouget ER. Prediction of treatment response in geriatric depression from baseline folate level: interaction with an SSRI or a tricyclic antidepressant. J Clin Psychopharmacol. 2003;23(3):309–13.
Goodwin JS, Goodwin JM, Garry PJ. Association between nutritional status and cognitive functioning in a healthy elderly population. JAMA. 1983;249(21):2917–21.
Deijen JB, et al. Nutritional intake and daily functioning of psychogeriatric nursing home residents. J Nutr Health Aging. 2003;7(4):242–6.
Mizrahi EH, et al. Plasma total homocysteine levels, dietary vitamin B6 and folate intake in AD and healthy aging. J Nutr Health Aging. 2003;7(3):160–5.
Morris MS, et al. Folate and vitamin B-12 status in relation to anemia, macrocytosis, and cognitive impairment in older Americans in the age of folic acid fortification. Am J Clin Nutr. 2007;85(1):193–200.
Clarke R, et al. Low vitamin B-12 status and risk of cognitive decline in older adults. Am J Clin Nutr. 2007;86(5):1384–91.
Haan MN, et al. Homocysteine, B vitamins, and the incidence of dementia and cognitive impairment: results from the Sacramento Area Latino Study on Aging. Am J Clin Nutr. 2007;85(2):511–7.
Kado DM, et al. Homocysteine versus the vitamins folate, B6, and B12 as predictors of cognitive function and decline in older high-functioning adults: MacArthur Studies of Successful Aging. Am J Med. 2005;118(2):161–7.
Quadri P, et al. Homocysteine, folate, and vitamin B-12 in mild cognitive impairment, Alzheimer disease, and vascular dementia. Am J Clin Nutr. 2004;80(1):114–22.
Ikeda T, et al. Vitamin B12 levels in serum and cerebrospinal fluid of people with Alzheimer’s disease. Acta Psychiatr Scand. 1990;82(4):327–9.
Karnaze DS, Carmel R. Low serum cobalamin levels in primary degenerative dementia. Do some patients harbor atypical cobalamin deficiency states? Arch Intern Med. 1987;147(3):429–31.
Snowdon DA, et al. Serum folate and the severity of atrophy of the neocortex in Alzheimer disease: findings from the Nun study. Am J Clin Nutr. 2000;71(4):993–8.
Joosten E, et al. Is metabolic evidence for vitamin B-12 and folate deficiency more frequent in elderly patients with Alzheimer’s disease? J Gerontol A Biol Sci Med Sci. 1997;52(2):M76–9.
Clarke R, et al. Variability and determinants of total homocysteine concentrations in plasma in an elderly population. Clin Chem. 1998;44(1):102–7.
Clarke R, et al. Folate, vitamin B12, and serum total homocysteine levels in confirmed Alzheimer disease. Arch Neurol. 1998;55(11):1449–55.
Ellinson M, Thomas J, Patterson A. A critical evaluation of the relationship between serum vitamin B, folate and total homocysteine with cognitive impairment in the elderly. J Hum Nutr Diet. 2004;17(4):371–83. quiz 385–7.
Ravaglia G, et al. Homocysteine and cognitive function in healthy elderly community dwellers in Italy. Am J Clin Nutr. 2003;77(3):668–73.
Raman G, et al. Heterogeneity and lack of good quality studies limit association between folate, vitamins B-6 and B-12, and cognitive function. J Nutr. 2007;137(7):1789–94.
Miller JW, et al. Homocysteine and cognitive function in the Sacramento Area Latino Study on Aging. Am J Clin Nutr. 2003;78(3):441–7.
Teunissen CE, et al. Homocysteine: a marker for cognitive performance? A longitudinal follow-up study. J Nutr Health Aging. 2003;7(3):153–9.
Morris MS, et al. Hyperhomocysteinemia associated with poor recall in the third National Health and Nutrition Examination Survey. Am J Clin Nutr. 2001;73(5):927–33.
Choumenkovitch SF, et al. Folic acid fortification increases red blood cell folate concentrations in the Framingham study. J Nutr. 2001;131(12):3277–80.
Jacques PF, et al. The effect of folic acid fortification on plasma folate and total homocysteine concentrations. N Engl J Med. 1999;340(19):1449–54.
Ganji V, Kafai MR. Trends in serum folate, RBC folate, and circulating total homocysteine concentrations in the United States: analysis of data from National Health and Nutrition Examination Surveys, 1988–1994, 1999–2000, and 2001–2002. J Nutr. 2006;136(1):153–8.
Yang Q, et al. Improvement in stroke mortality in Canada and the United States, 1990 to 2002. Circulation. 2006;113(10):1335–43.
Balk EM, et al. Vitamin B6, B12, and folic acid supplementation and cognitive function: a systematic review of randomized trials. Arch Intern Med. 2007;167(1):21–30.
Aisen PS, et al. High-dose B vitamin supplementation and cognitive decline in Alzheimer disease: a randomized controlled trial. JAMA. 2008;300(15):1774–83.
Sommer BR, Hoff AL, Costa M. Folic acid supplementation in dementia: a preliminary report. J Geriatr Psychiatry Neurol. 2003;16(3):156–9.
Hvas AM, et al. No effect of vitamin B-12 treatment on cognitive function and depression: a randomized placebo controlled study. J Affect Disord. 2004;81(3):269–73.
Eussen SJ, et al. Effect of oral vitamin B-12 with or without folic acid on cognitive function in older people with mild vitamin B-12 deficiency: a randomized, placebo-controlled trial. Am J Clin Nutr. 2006;84(2):361–70.
Durga J, et al. Effect of 3-year folic acid supplementation on cognitive function in older adults in the FACIT trial: a randomised, double blind, controlled trial. Lancet. 2007;369(9557):208–16.
Smith AD, et al. Homocysteine-lowering by B vitamins slows the rate of accelerated brain atrophy in mild cognitive impairment: a randomized controlled trial. PLoS One. 2010;5(9), e12244.
de Jager CA, et al. Cognitive and clinical outcomes of homocysteine-lowering B-vitamin treatment in mild cognitive impairment: a randomized controlled trial. Int J Geriatr Psychiatry. 2012;27(6):592–600.
Bryan J, Calvaresi E, Hughes D. Short-term folate, vitamin B-12 or vitamin B-6 supplementation slightly affects memory performance but not mood in women of various ages. J Nutr. 2002;132(6):1345–56.
Kang JH, et al. A trial of B vitamins and cognitive function among women at high risk of cardiovascular disease. Am J Clin Nutr. 2008;88(6):1602–10.
Fioravanti M, et al. Low folate levels in the cognitive decline of elderly patients and the efficacy of folate as a treatment for improving memory deficits. Arch Gerontol Geriatr. 1998;26(1):1–13.
Nilsson K, Gustafson L, Hultberg B. Improvement of cognitive functions after cobalamin/folate supplementation in elderly patients with dementia and elevated plasma homocysteine. Int J Geriatr Psychiatry. 2001;16(6):609–14.
Douaud G, et al. Preventing Alzheimer’s disease-related gray matter atrophy by B-vitamin treatment. Proc Natl Acad Sci U S A. 2013;110(23):9523–8.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Scott, T.M., D’Anci, K.E., Rosenberg, I.H. (2015). B Vitamins Influence Vascular Cognitive Impairment. In: Bendich, A., Deckelbaum, R. (eds) Preventive Nutrition. Nutrition and Health. Springer, Cham. https://doi.org/10.1007/978-3-319-22431-2_17
Download citation
DOI: https://doi.org/10.1007/978-3-319-22431-2_17
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-22430-5
Online ISBN: 978-3-319-22431-2
eBook Packages: MedicineMedicine (R0)