Abstract
Fortunately the frequency of mutagenic drug candidates recognized in early drug development is very low because positive Ames bacterial mutagenicity test results usually have severe ramifications with APIs dropped from further development. While negative results in the appropriate follow-up tests (e.g., mouse carcinogenicity studies) could enable progression of API development, pragmatically the cost and long duration required for these tests means that most pharmaceutical companies drop mutagenic APIs from development and quickly move on to another drug candidate.
Positive in vitro mammalian genotoxicity tests are far more frequently encountered but most times do not prevent further development of an API. When positive in vitro mammalian genotoxicity test results are obtained, follow-up studies in complementary in vitro or in vivo assays are quickly conducted to understand the biological relevance of the initial positive response. In the majority of cases the additional testing allows the sponsor to demonstrate lack of biological relevance or establish a safety threshold (generally ≥10×) based on exposures in animals at the no observed genotoxic effect level (NOGEL) relative to highest clinical exposure. For all these reasons, follow-up testing in response to an in vitro mammalian cell positive test is generally pursued and often results in continued development of the API.
This chapter focuses on genotoxicity testing strategies and includes case studies where follow-up studies were used to effectively de-risk positive in vitro genotoxicity test results. The regulatory guidelines (e.g., ICH S2(R1)) dictating which tests are required and which follow-up tests are acceptable are also presented. Because the regulatory guidelines list acceptable follow-up tests with little to no guidance on how to select them, this chapter provides recommendations on how to design the most appropriate follow-up testing strategy.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Genotoxicity
- Ames bacterial mutagenicity test
- DNA damage
- Clastogenicity
- ICH S2(R1)
- No-observed genotoxic effect level (NOGEL)
3.1 Introduction
Genotoxicity is the process by which chemicals interact with or damage DNA and/or the cellular apparatus which regulates the accuracy and efficiency of the DNA replication and repair processes [UK COM 2000]. Many in vitro and in vivo tests have come and gone over the years but they all measure mutation, chromosome damage, DNA damage or repair, or numeric change in chromosome number. Genotoxicity testing has been used since the 1970s as a quick surrogate for long-term rodent carcinogenicity studies. This testing was initiated due to concerns regarding a chemical’s direct potential to induce somatic cell mutations responsible for cancer initiation or indirect modes of action responsible for cancer progression. Initially, germ-cell genotoxicity assays were considered important for assessing potential chemical mutations that could have far reaching implications for future generations. Today, only somatic cell genotoxicity tests are required since they identify all known germ-cell genotoxicants.
In the last decade there has been a dramatic move from small molecule drugs created via organic synthesis to large molecule biologics (antibodies, peptides, proteins) harvested from cultured cells and combinations such as antibody drug conjugates. Genotoxicity testing is required for small molecules but not for the majority of biologicals. For this reason, testing strategies and recommendations in this chapter will refer to small molecules.
Once a drug candidate is selected for possible clinical development, it is subjected to an extensive battery of genotoxicity tests conducted under good laboratory practices (GLP) using protocols accepted by international regulatory authorities. These studies are submitted to regulatory health authorities as part of the overall nonclinical safety data package to support most Phase 1 clinical trials. In the US, the nonclinical safety data to support Phase 1 clinical trials are summarized in an Investigational New Drug (IND) application. Since new drugs are often tested first in healthy human volunteers who receive no benefit from the drug, the investigational drug must pose a very low health risk to those volunteers. Drugs are not evaluated for potential carcinogenicity until much later in drug development, so genotoxicity testing is conducted prior to Phase 1 clinical trials to protect human volunteers from exposure to potential carcinogens. Genotoxicity tests evaluate endpoints associated with initiation or progression of tumorigenesis using short-term in vitro and in vivo assays. These tests measure mutations, DNA strand breaks, chromosome damage, and changes in chromosome numbers.
3.2 Mechanisms of Genotoxicity
Genotoxic effects can arise through multiple mechanisms. From a broad perspective these effects can be categorized as direct or indirect genotoxicity. Direct genotoxicity is due to the interaction of a chemical API and/or its metabolite(s) with DNA. In contrast, indirect effects are associated with a chemical or metabolite(s) interacting with non-DNA targets and subsequent generation of genetic damage. An understanding of mechanism is critical for assessing clinical risks as well as determining appropriate strategies for following-up testing to further characterize positive results.
3.2.1 Direct Genotoxicity
The direct genotoxic mechanisms of primary concern in drug development are the induction of gene mutations and structural chromosomal damage (i.e., clastogenicity). Gene mutations include base-pair substitutions and frameshift mutations arising through addition or deletion of a single nucleotide. Clastogens cause DNA strand breaks which, if not repaired properly, can lead to the addition, deletion, or rearrangement of genetic information. Because mechanisms of direct genotoxicity have been associated with the multi-step process of carcinogenicity, positive results in assays capable of detecting gene mutations or clastogens are a significant concern for clinical trial subjects.
3.2.2 Indirect Genotoxicity
There are many examples of genotoxicity that result from indirect mechanisms of action. Of particular importance to drug development is an alteration in the number of an individual chromosomes. This process, known as aneugenicity, is the product of mitotic spindle apparatus disruption leading to the loss or gain of a whole chromosome. Another numerical chromosome effect is polyploidy, duplications of the entire chromosomal complement. Aneugenicity is associated with carcinogenicity and is a critical component of genotoxicity testing to support drug development. Additional indirect genotoxic mechanisms include inhibition of DNA synthesis, nucleotide pool imbalance, inhibition of topoisomerase, and in vivo body temperature changes.
3.2.3 Thresholds
Thresholds are defined as the dose or exposure above which an effect becomes discernable from background. Thresholds can be an important consideration when genetic toxicology testing yields positive results. Although there is mounting scientific evidence to suggest otherwise, genotoxicity associated with a direct mechanism is often treated as though no threshold exists. This outcome is likely related to (1) the complex nature of establishing thresholds for test articles capable of inducing gene mutations or clastogenic effects and/or (2) the negative outlook for developing genotoxic drugs.
In contrast, thresholds have been identified for indirect acting genotoxic compounds. When indirect mechanisms are suspected, it may be possible to identify no observed genotoxic effect levels (NOGELs) in appropriate in vivo testing. Development of a drug may proceed when acceptable margins of safety are shown to exist.
3.3 Regulatory Recommendations
The primary regulatory guideline addressing the genetic toxicology testing of small molecule drugs is the International Conference for Harmonization (ICH) S2(R1) guideline (ICH, 2011). This globally adopted guideline provides recommendations regarding the battery of genetic toxicology tests needed to support drug development (see below). In addition, the document describes the proper conduct of assays (e.g., test conditions, appropriate test systems, doses, etc.), evaluation of results, and appropriate follow-up for positive findings.
3.3.1 ICH Guidelines
Although quantitative risk assessment may be possible, genetic toxicology assays used to support drug development are primarily intended as hazard identification tools. Because there is no single genetic toxicology assay capable of effectively evaluating all genotoxic mechanisms, ICH S2(R1) recommends conducting a battery of tests to maximize the potential of identifying relevant effects. Due to the established association with carcinogenicity, the effects of most concern in drug development are gene mutations, structural chromosomal damage (i.e., clastogenicity), and numerical chromosomal damage (e.g., aneugenicity). The guideline offers flexibility by providing two testing options.
The Option 1 battery includes in vitro assays intended to evaluate gene mutations and chromosomal damage as well as an in vivo evaluation of chromosome level effects. The potential to induce gene mutations is evaluated through the bacterial reverse-mutation assay (i.e., Ames assay). In vitro chromosomal damage can be evaluated using the chromosomal aberration assay, micronucleus assay, or mouse lymphoma assay. All three of these assays are considered equivalent for regulatory use. In addition to the overall positive or negative assay result, additional information may be obtained to establish mechanism of action. For instance, the in vitro micronucleus assay can distinguish between clastogens and aneugens through the use of special staining procedures or flow cytometry. Likewise, mechanistic information can be gained from the mouse lymphoma assay through sizing of mutant colonies. Option 1 also requires an in vivo assay. This is most often the micronucleus assay in rodent hematopoietic cells; however, the chromosomal aberration assay is also acceptable. As with the in vitro assay, mechanistic data can be used to support the identification of clastogenic vs. aneugenic drugs.
Option 2 also involves conduct of an in vitro bacterial reverse mutation assay but requires in vivo evaluation of two genotoxic endpoints in two tissues. A possible combination to satisfy the in vivo requirements would be the micronucleus assay in rodent hematopoietic cells and the Comet assay. While the liver may be the default target organ for the Comet assay, understanding of metabolism and target organ toxicity can be used to justify selection of other tissue(s) as well.
Details of the regulatory genetic toxicology assays, including sources of standardized protocols (e.g., OECD guidelines), are summarized in Table 3.1 below. Following standardized protocols assures experiments are conducted according to widely accepted methodology, a critical consideration for regulatory use.
ICH M3(R2) describes timelines for submitting genetic toxicology data to support small molecule development. Under Option 1 the in vitro assays should be submitted prior to a Phase 1 clinical trial and the in vivo assay prior to Phase 2. While not explicitly stated in ICH M3(R2), a general assumption is that all assays will be submitted prior to initiating Phase 1 clinical trials when Option 2 is selected. A more limited evaluation, in some cases requiring no genetic toxicology data, may be acceptable for exploratory clinical trials. The timing of assays conducted to follow-up a positive result will vary. However, it is worth noting that, in some instances, a positive genotoxicity finding may result in a clinical hold until the risk is mitigated. Note that the timing of genetic toxicology testing is different for anticancer drugs. Per ICH S9, results of genotoxicity testing need only be performed to support submission of a marketing application.
ICH S6 (R1) addresses the safety evaluation of biological drugs such as proteins, peptides, monoclonal antibodies, etc. Standard genotoxicity testing is usually unnecessary as these molecules are unlikely to react with DNA. An exception is when an organic moiety is used to link 2 moieties together (e.g., therapeutic protein and PEG).
3.3.2 FDA Guidance
In addition to the ICH S2(R1) guideline, other sources of regulatory recommendations regarding genetic toxicology testing are available. For instance, the U.S. Food and Drug Administration (FDA) provides guidance on the evaluation and integration of genetic toxicology data (FDA, 2006). The FDA also addresses genetic toxicology evaluation of drug metabolites formed uniquely or disproportionately in humans (FDA, 2008). When these metabolites are encountered, the initial evaluation should include in vitro data for point mutations and chromosomal aberrations. No further testing is needed if in vitro results are negative; however, additional data may be warranted to further characterize genotoxic potential if positive results are obtained.
3.4 Pre-candidate Genotoxicity Screening
With few exceptions, mutagenicity is considered an unacceptable risk and companies usually drop the drug candidate from development due to the extensive amount of work required to demonstrate safety prior to initiating human clinical trials and the low probability of success. Mechanistic data may be used to demonstrate that mutagenicity is not relevant to human safety (e.g. bacterial specific metabolite, rat S9 specific metabolite, etc.). But aside from oncology drugs, and drugs targeting serious or life threatening diseases, most companies will not invest in these de-risking strategies and will quickly move on to another drug candidate. Therefore, pharmaceutical companies have implemented screening strategies during discovery and lead compound optimization to quickly identify mutagens as well as other serious safety liabilities. Screening strategies vary greatly between companies with no consensus on the best test(s) to use or the exact timing on when these tests should be conducted. However, the majority of pharmaceutical companies use a common strategy of first assessing the chemical structure for the presence of known mutagenic and carcinogenic structural alerts. If a decision is not made to eliminate the compound based on the structure-based assessment, a mutagenicity screening assay is usually conducted prior to selecting a lead compound. Some companies also perform screening assays for other genotoxicity endpoints such as DNA or chromosome damage, or change in chromosome number. Not all companies conduct these additional screening assays because as long as the drug is not a direct acting mutagen, it may still be developed if no genotoxicity is observed in vivo or as long as a sufficiently large margin is achieved between the genotoxic and clinical doses/exposures.
3.4.1 Structural Assessment
Computational structural assessments do not require actual drug synthesis and hence are usually the first safety evaluation conducted for drug candidates. Structural assessments may be conducted via literature review or by using commercially available software packages. There are several commercially available software programs that currently meet FDA basic requirements for transparency, predictive accuracy and other parameters. Refer to Chap. 2 by Stavistkaya, Aubrecht, and Khrulak for an in depth discussion on this topic.
3.4.2 Bacterial Mutagenicity Screening
Compounds that contain structural alerts for mutagenicity are further evaluated in a screening bacterial mutagenicity test to confirm the computational prediction. Prior to full development, only limited quantities of drug are generally available for early efficacy and safety studies. For these reasons genotoxicity testing using the regulatory GLP assay protocols are not normally conducted. In response to this limitation in drug supply, protocols have been developed that use small amounts of drug (mg quantities) but are sufficiently robust to identify the vast majority of mutagenic drugs before extensive resources have been expended on larger scale chemical synthesis and other drug development activities. Some tests are limited versions of the regulatory GLP test, detecting the exact same endpoint, while using fewer than the GLP required 5-bacterial strains, modified strains or entirely different bacterial strains, fewer replicate plates, smaller plates, lower top doses, colorimetric read-out rather than counting revertant colonies or a surrogate endpoint other than mutation. In this sense, the mutagenicity screening tests can be viewed as more “high-throughput” assays compared to the standard GLP study while maintaining high sensitivity with moderate to significant reductions in compound requirement. Table 3.2 lists a few of the most widely used bacterial screening assays comparing the amount of compound required for each and the strengths and weaknesses [1]. The performance of each of these assays was evaluated using a different number of reference compounds and different reference compounds, so the ability of each assay to identify mutagens cannot be directly compared. However, the performance of most of these assays can be increased if consideration is given to the results of the structural alert assessment. Several of the software systems provide detailed information regarding the strain or metabolic conditions associated with the mutagenic prediction. This information can be used to design an intelligent screening assay tailoring the strain or assay conditions to enable confirmation or de-risking a mutagenic structural alert.
For example, boronic acids and esters are a chemical class recently recognized to have mutagenic potential and such knowledge has been incorporated into recent mainstream computational software. Structural alerts and experience has shown that these compounds are often uniquely positive in E. coli or TA1535, strains not typically included in routine screening unless computational prediction is considered.
A second example, alkyl halides, have long been recognized to have mutagenic activity. Experienced researchers know that many compounds in this class are mutagenic in strains TA1535 and less potently in TA100. Use of structural alert software and knowledge based assessments can provide this information quickly without requiring extensive mutagenicity testing or literature searches.
3.5 GLP Battery Selection Strategy (Option 1 vs. Option 2)
Several factors should be considered when choosing between ICH S2(R1) Option 1 and Option 2 battery. Option 1 is based on the previously accepted testing battery described in ICH S2A/B. This option is preferred when an Ames assay may not be appropriate for a specific test article (e.g., antibacterials) or when non-clinical systemic exposure provides insufficient coverage relative to clinical systemic exposure. Although Option 2 has not previously existed as a stand-alone testing battery, the approach is consistent with follow-up tests recommended for de-risking in vitro mammalian cell positives. This Option may be preferred in cases where short-lived reactive metabolites are expected to form in the liver or if a non-GLP screening study indicates a positive result would be expected in the GLP in vitro mammalian cell assay. Under these situations consider using Option 2 with evaluation of both genotoxicity endpoints (micronucleus and Comet) integrated into a single in vivo study to reduce animal use and maximize data acquired.
3.6 High-Dose Selection
In order to adequately characterize genotoxic potential for both in vitro and in vivo assays, it is important to test to appropriately high doses. This dose must be sufficiently high to detect relevant genotoxic responses but not overly high as several well-understood phenomena leading to irrelevant positives can occur. Important considerations for in vitro assays include test article solubility and cytotoxicity. The selection of an appropriate limit dose for in vivo assays also factors in the duration of dosing and whether genetic toxicology endpoints are combined with a general toxicology study. Specific details, as described in ICH S2(R1) are summarized below.
3.6.1 Ames Assay
For readily soluble and non-cytotoxic test articles, the maximum recommended dose for bacterial reverse mutation assay is 5000 μg/plate. When limits of solubility are exceeded, the lowest dose yielding precipitation should be scored as the top dose assuming no cytotoxicity is encountered. The top dose may also be limited to a level providing a significant degree of cytotoxicity (e.g., reduced background revertants or background lawn).
3.6.2 In Vitro Mammalian Cell Assays
The maximum recommended concentration is the lower of 1 mM or 0.5 mg/mL when solubility and cytotoxicity are not limiting. For insoluble but non-cytotoxic test articles, the top concentration should produce minimal precipitation as long as scoring is still possible. For cytotoxic test articles, top concentrations should need not exceed a ~50 % reduction in cell growth for chromosomal aberration or ~55 % reduction for micronucleus assays. When cytotoxicity is used to limit concentrations evaluated in the mouse lymphoma assay, the relative total growth should be ~10–20 %.
3.6.3 In Vivo Assays
The maximum recommended dose for acute studies (e.g., one to three dose administrations) is 2000 mg/kg/day or a dose producing the maximum tolerated dose (MTD). For testing conducted with in vitro mammalian assay positive test articles or when Option 2 is utilized, selection of a top dose must take into account several factors. These include the MTD (e.g., based on consideration of lethality following acute administration), maximum feasible dose (MFD) based on solubility, limit dose of 1000 mg/kg/day for studies ≥14 days, saturation of systemic exposure, and target tissue toxicity. In cases where the in vitro mammalian cell assay is negative and Option 1 is being followed, evaluation of a genetic toxicology endpoint can be combined with a standard general toxicology study. In such cases, it is reasonable for top dose selection to support clinical development as described in ICH M3(R2).
3.7 Follow-Up Testing for Ames Positives
Unless gene mutations are deemed an acceptable liability (e.g., acute treatment, life-threatening indication, etc.), it is often difficult to develop drugs that are positive in the Ames assay. The exception is positive results due to experimental artifact or those with questionable clinical relevance. Examples of artifact include the presence of histidine or tryptophan [2–5]. Positive results considered to be of questionable relevance are those related to mutagenic impurities that are not present in the clinical batch or formation of mutagenic metabolites through a rodent S9 or bacterial specific pathway (e.g., nitroreductase).
For relevant Ames positive drugs, there is no clear follow-up testing strategy. ICH S2(R1) simply indicates that “extensive follow-up testing” is needed to further characterize potential in vivo mutagenicity and carcinogenicity. Currently there is no single assay deemed sufficient to mitigate concerns with an Ames positive finding. However, there are multiple assays to consider as potential components of a follow-up testing strategy. For instance, evaluating the formation of large colonies in the mouse lymphoma assay provides a rapid in vitro assessment of gene mutations in mammalian cells. Two in vivo options are available to directly assess gene mutation events. One option is the transgenic gene mutation assays which is most often used as a tool to evaluate mechanism of action (e.g., establish potential of carcinogenic compounds to induce gene mutations as follow-up to a 2 year rodent bioassays). In addition, this assay can also be used to further characterize the in vivo relevance of an Ames positive finding. This assay allows evaluation of mutations in multiple tissues but requires 28 days of test article administration (specific models discussed in more detail in OECD TG488) [6]. Another recently developed in vivo option for assessing Ames positive findings is the Pig-a gene mutation assay (covered in a special issue of EMM) [7]. The Pig-a mutation is detected only in reticulocytes so tissue coverage is limited. A key advantage of this assay is the ability to integrate the endpoint in general toxicology studies using standard animal models. Pig-a mutations can also be measured in clinical samples. Additional in vivo options include evaluation of primary DNA damage in the UDS and comet assays as well as measurement of DNA adduct formation. These endpoints are potentially related to but do not directly measure gene mutations. The comet assay and measurement of DNA adducts can be applied to many tissues while UDS is restricted to the liver. UDS is generally considered to be an insensitive endpoint, with the potential exception of drugs that induce bulky DNA adduct formation. DNA adducts can be measured using relatively rapid and sensitive techniques, such as liquid chromatography – mass spectrometry based methods, but are not often submitted in support of regulatory decision making. Overall, the utility of the primary DNA damage assays is limited but perhaps useful for contributing to the weight of evidence against reactive potential.
In some cases, data from a short-term transgenic mouse carcinogenicity study (e.g., p53+/− or rasH2) has been requested by regulators. While providing definitive data on the endpoint of clinical concern (i.e., carcinogenicity), the studies require large number of transgenic animals and 6 months of dosing.
Ultimately, the ability to proceed with clinical administration of an Ames positive molecule depends on the strength of evidence demonstrating an acceptable risk:benefit profile.
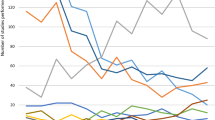
3.8 Follow-Up Testing for In Vitro Mammalian Cell Positives
In vitro mammalian cell assay positives are more prevalent during drug development than bacterial mutation positives and are far less likely to prevent continued drug development. The rate of bacterial mutagens encountered is only ~10–12 % during lead compound identification, if synthetic intermediates and reactive synthetic reagents are discounted, while the rate of in vitro mammalian cell positives varies across experimental systems and can range as high as 25–30 % [8]. However, in many cases the positive in vitro response may not be relevant to safety at human exposure levels.
Under option 1 in ICH S2(R1), drugs should be evaluated for genotoxicity potential in mammalian cells in vitro. The sponsor has the choice of conducting an in vitro metaphase chromosome aberration assay (CAA), an in vitro micronucleus assay (IVTMN) or a mouse lymphoma L5178Y cell TK+/− (thymidine kinase) gene mutation assay (MLA). Selection of which in vitro mammalian cell assay to conduct is a decision each sponsor must make. Things to consider when selecting which assay to conduct is what endpoints are detected in each system, and for those conducting these studies in-house, equipment and expertise of those evaluating the data. CAA detects structural chromosome damage and numerical aberrations (i.e. polyploidy). IVTMN detects structural chromosome damage in addition to aneuploidy and qualitatively cell cycle perturbations, when evaluated using flow cytometry. MLA detects both point mutations and chromosomal mutations based upon the ratio of large and small mutant colonies. Time and cost required to conduct the CAA and MLA historically have been similar. The IVTMN test option was recently added as an option with the 2012 update of ICH S2(R1). All three assays (CAB, IVTMN and MLA) may be evaluated using manual microscopic methods but the IVTMN assay has the option of using automated flow cytometric evaluation which can reduce study duration to 1 week compared with 4–5 weeks for CAA and MLA.
Several approaches can be taken to investigate the relevance of in vitro positives including defining the mode of action (MOA) or accumulating more data and generating a weight-of-evidence (WOE) argument. Because defining an acceptable MOA argument is more difficult and potentially more time consuming, usually a WOE approach is taken within industry. A first step for any investigation should be to consider the reproducibility of the initial positive response and to consider repeating the test using a different cell line to rule out cell line specifics such as p53 status. A positive response should be reproducible and fall outside of the laboratory historical control range. Also, since pharmaceuticals are designed to have a pharmacological effect, consider whether the positive in vitro response could be due to exaggerated pharmacology.
3.8.1 Irrelevant In Vitro Positives
Irrelevant positive in vitro responses can generally be divided into three categories: (a) activity specific to in vitro culture; (b) non-DNA interactions with components of critical cellular functions; and (c) direct DNA damage at concentrations above a threshold due to disruption of basic cellular homeostasis.
The first step to evaluating any positive experimental data is to consider whether the test substance was sufficiently pure and stable, or whether an impurity or degradant could be responsible for the positive response. A broad spectrum of cell culture artifacts such as pH, osmolality, and excessive toxicity have long been recognized as sources of irrelative positive results [9]. In recognition that excessive toxicity could induce an irrelevant positive response, the top dose required for in vitro assays was reduced tenfold in the latest ICH S2(R1) guidance document.
Dimethyl sulfoxide (DMSO) is a commonly used solvent for in vitro assays and there have been occasions when the test substance has reacted with DMSO to generate a substance reported in the literature to be genotoxic. Before conducting additional in vitro studies consider consulting with a chemist on solvent selection to ensure that the test substance does not react with the selected solvent.
The cell line and origin of the cells being used to conduct genotoxicity testing should be considered and periodically re-evaluated. Over time due to poor cell culture, storage or labeling, spurious laboratory results may be attributed to instability of the cell line being used. Some labs have even found that cell lines thought to be of human origin were contaminated with rodent cells at some point. To guard against this as well as simple genetic drift ensure that target cells are performing within published parameters. The HESI Genetic Toxicology Technical Committee is in the process of establishing repositories of characterized L5178Y, TK6, CHO-WBL, CHL, and Hep G2 cells for genotoxicity testing [10]. The repositories will be at Sigma (USA), ECACC (UK), and JCRB (Japan), and a guidance document on good cell culture is in preparation. It’s important to verify that cell lines intended for genotoxicity studies exhibit appropriate background response frequencies, and respond to reference chemicals appropriately.
Cell culture systems are routinely supplemented with S9 liver metabolic fraction to mimic in vivo metabolic activation because the most commonly used immortalized cell lines contain little to no metabolic activity. An exception to this are cell lines genetically engineered to express p450 activity or immortalized hepatocytes. The S9 liver metabolic fraction typically used to supplement in vitro genotoxicity studies originates from rats induced to have high CYP P450 levels by pre-treatment with Aroclor 1254 or phenobarbital/β-napthoflavone prior to preparation of S9. The metabolite profile produced using induced S9 in vitro can be very different than the metabolite profile in un-induced rats or humans. In vitro only phase 1 metabolism is present because the S9 system is only supplemented with CYP co-factor NADPH not co-factors required for phase 2 metabolism. Therefore, a genotoxic metabolite inducing a positive in vitro response, may not be relevant in vivo because it may be detoxified by conjugation or may be produced at very low levels due to competing or alternative CYP pathways dominating in vivo.
Consideration should also be given as to whether the genotoxic effect can be attributed to a non-DNA reactive mechanism. Sometimes test substances do not directly interact with DNA but rather target macromolecules involved in critical cellular functions such as cell division [11–13]. Test substances which bind to elements of the mitotic apparatus generally result in aneuploidy and are easily detected in the IVMN assay and to a lesser extent in the CAA. Examples of non-DNA reactive in vitro cell assay positives have been demonstrated for test substances that inhibit DNA synthesis and repair enzymes, perturb nucleotide pool balance, or generation of reactive oxygen species via lipid peroxidation reaction and others have been described by Scott et al. [9] and Kirkland et al. [14].
Consideration should be given as to whether the positive response is due to direct DNA interaction or only observed above a defined threshold. A common example of this are kinase inhibitors designed to have selectivity at therapeutic exposures that maybe in the nanomolar range, but concentrations required for in vitro genotoxicity testing may be >10,000-fold higher than intended therapeutic doses. At such high concentrations pharmacologic selectivity is lost and the effect is non-specific inhibition of kinases including those kinases responsible for maintaining cellular homeostasis. As a class many kinase inhibitors are positive in CAA and IVTMN assays.
3.8.2 Selection of Appropriate Follow-Up Tests
Follow-up testing strategy is dependent upon the genotoxicity assay in which the positive response was observed and has been the basis of several industry discussions and publications [14–16]. For any of the in vitro assays where the positive result is seen only in the presence of S9 metabolic activation, consideration should be given to comparing the in vitro metabolic profiles from rats and humans. Consideration should also be given as to whether the lack of phase 2 conjugation may be contributing to the positive response. The in vitro study could be repeated with addition of phase 2 co-factors to investigate this possibility. For MLA, selection of follow-up tests depends upon the proportion of small and large colonies. If the positive response was due to predominately small colony mutants then an appropriate follow-up in vitro assay would be one that detects clastogenicity such as CAA or IVTMN. However if large colonies were predominately responsible for the positive response then consideration should be given to an hprt assay or the in vitro comet assay. Positive MLA small colony results would add WOE that a positive CAA response was relevant, because both in vitro assays detect the same chromosome mutation
Generation of WOE information using additional in vitro studies helps clarify the relevance of the initial positive response, but moving directly to an in vivo study may be a faster and more reliable approach to reducing perceived risk. ICH S2(R1) requires negative results for 2 in vivo genotoxicity endpoints to conclude that an in vitro positive response is not biologically relevant. The guidance recommends conducting a comet assay evaluating DNA damage in liver, and potentially known target tissues and a micronucleus assay evaluating induction of chromosome damage in bone marrow or peripheral blood. While a micronucleus evaluation is easily integrated into general toxicity studies, the comet assay cannot be easily integrated due to logistical hurdles arising from the short 3–6 h exposure condition. Whenever a Comet assay is needed, a standalone in vivo genotoxicity study including Comet and micronucleus assays is often the best solution.
For test substances found to be genotoxic in vitro but not in vivo, there should be evidence that the test substance reached the target organ in vivo. This can be addressed for negative micronucleus studies by always measuring test substance exposure in the blood, because the bone marrow is a highly perfused organ. For orally dosed comet assays, site of contact tissues do not require proof of exposure and similar to bone marrow, liver is a highly perfused tissue and generally demonstrating systemic exposure is sufficient proof of tissue exposure.
Consider the in vitro endpoint (mutagenicity, clastogenicity, or aneugenicity) when selecting in vitro or in vivo follow-up tests. Ensure that the follow-up test selected can detect the endpoint that needs to be verified. For test substances inducing only gene mutations in vitro, a transgenic mouse gene mutation assay or rodent Comet assay would be appropriate follow-up studies. These assays have OECD test guidelines describing proper assay conduct. Other follow-up assays could be used with scientific justification even those without formal OECD test guidelines, but care should be taken to design these studies in accordance with scientific literature. For test substances only inducing chromosomal aberrations, appropriate follow-up in vitro tests would include chromosome aberrations in an alternative cell line, micronucleus or comet assay, and an in vivo micronucleus or Comet test. For test substances inducing both gene mutation and clastogenicity in vitro consider an in vivo Comet and micronucleus assay to verify in vitro findings. Sponsors could consider conducting an in vivo mutation endpoint such as a transgenic mouse or Pig-a gene mutation assay to further investigate potential in vivo mutation. For test compounds only inducing genotoxicity in the absence of S9 metabolic activation, consideration should be given to conducting a Comet assay including a site of contact tissue (eg. GI tract, or skin depending upon dosing route) in addition to liver.
3.9 Case Studies
3.9.1 Positive Ames – Peptide
A peptide containing histidine and tryptophan amino acids tested positive in a plate incorporation bacterial mutagenicity test. The positive response was weak, only exceeding the 2.0-fold positive response criteria at the highest dose evaluated. This type of response could have been due to an impurity in the test substance or due to release of histidine from the peptide. Re-purification of the peptide would be labor intensive, so a “feeding effect” from histidine was evaluated first. The Ames test was repeated using the method where the bacteria are pre-incubated with the test substance prior to plating on agar plates. This provided the opportunity to wash the bacteria several times to remove any residual peptide (histidine/tryptophan source) prior to plating the bacteria on agar(2). The pre-incubation method was negative with no increase in revertant colony count and no increase in toxicity. Based on this information the peptide was considered not mutagenic. The small increase in revertant colony counts was attributed to facilitation of growth of auxotrophic colonies by the additional histidine present in the treated plates, but not the vehicle plates.
3.9.2 Genotoxic In Vitro but Non-genotoxic In Vivo
An impurity was mutagenic in the Ames test (four-fold maximum response) and clastogenic in the in vitro micronucleus assay in CHO cells (six-fold maximum response) in the absence of S9 metabolic activation. The genotoxicity response was further evaluated in vivo to provide data supporting the hypothesis that the genotoxic impurity quickly degraded to a non-genotoxic species in the acid pH of the stomach. Rats were orally administered the test substance daily for 1-month with strong systemic exposure to the test substance measured on Day 1 and during Week 4, with Cmax concentrations in vivo equal to or greater than in vitro concentrations where genotoxicity was observed. However, the test substance did not induce a mutant phenotype in the Pig-a gene mutation assay sampled on Day 31, did not induce micronuclei in peripheral blood sampled on Day 14, and did not induce DNA damage (comet assay) in duodenum or liver following 3–6 h or 24-h exposure. Based on the weight of evidence it was concluded that the test substance was not genotoxic in vivo.
The Pig-a erythrocyte mutation assay has been demonstrated to accurately detect mutagenic test substances. The Pig-a assay was selected to evaluate in vivo mutagenic potential rather than one of the lacZ reporter gene based transgenic assays because the Pig-a assay could be integrated into a 1-month rat study using the same strain animal as previous toxicology studies enabling leverage of all information previously gathered for this test substance. Also the Pig-a assay is much cheaper and faster than the lacZ based transgenic assays or the transgenic carcinogenicity models (eg. p53+/−, or rasH2).
3.9.3 Positive In Vitro Chromosome Aberrations with S9 Metabolic Activation Only
A test substance induced structural chromosome aberrations only in the presence of S9 liver metabolic activation from Aroclor induced rats. The metabolite profile generated in the tissue culture media with test substance and S9 but without cells was evaluated and it was postulated that the major metabolite generated in the in vitro S9 system would not accumulate or persist due to rapid detoxification (glucuronidation). The chromosome aberrations assay with S9 metabolic activation only was repeated as before but with the addition of a secondary set of cultures containing glutathione at physiological concentration. The positive response with S9 was reproduced, but the positive response was completely ameliorated in the glutathione containing cultures. Based upon these results, in addition to data demonstrating the test substance did not induce micronuclei in rats, the genotoxic response in the in vitro chromosome aberrations assay was considered biologically irrelevant with no impact on potential patient safety.
3.9.4 Positive In Vitro Micronucleus – Aneugen
A test substance induced a significant increase in micronuclei in vitro in CHO cells both in the presence and absence of S9 liver metabolic activation. A micronucleus assessment was piggybacked on an on-going 2-week rat general toxicology study to evaluate the biological relevance of the positive response. Micronucleus induction was evaluated in peripheral blood collected on Day 7 and rapidly evaluated using flow cytometry. The test substance did not induce micronuclei in rats when tested up to maximum limits. Cmax data indicated that systemic exposures achieved in rats were ~50 % lower than the in vitro concentration where micronuclei were significantly induced. Drug development of the candidate continued.
Another test substance also induced significant increase in micronuclei in vitro in CHO cells and an in vivo micronucleus assessment was piggybacked on a 1-month rat general toxicology study. However, in this case the test substance induced micronuclei in rats at doses that resulted in systemic exposure multiples of 300× the predicted human exposure at the highest anticipated clinical dose. Based on the exposure multiple the test substance continued in development.
A test substance was demonstrated to induce micronuclei in vitro, but based upon a meaningful increase in the hypodiploidy gate observed during flow cytometric evaluation, the response was probably due to aneuploidy (chromosome loss). An aneuploidy response can occur when the test substance interferes with the mitotic apparatus leading to non-disjunction resulting in a micronucleus that contains an entire chromosome. Aneuploidy is widely accepted as an example of a threshold response. Therefore, a second in vitro micronucleus study was conducted to determine whether the origin of the micronuclei was from aneuploidy (kinetochore positive micronuclei) or an acentric chromosome break (kinetochore negative micronuclei). The in vitro kinetochore study demonstrated that >85 % of the micronuclei induced were due to an in-direct aneuploidy mechanism and not direct DNA damage. Therefore it was concluded that the test substance was safe for clinical trial volunteers at exposures less than those that induced aneuploidy.
3.9.5 Positive In Vivo Micronucleus with Elevated Body Temperature
A test substance was found to induce micronuclei formation following acute dosing in rats. The effect was only observed at a dose known to also cause an increase in body temperature in rats. A second in vivo micronucleus assay was performed using a repeat-dose protocol with doses that were not associated with temperature changes. Results from this assay were negative at systemic exposures providing a robust safety margin vs. expected clinical exposures. The sponsor also conducted an in vivo UDS assay in liver to demonstrate a lack of DNA reactivity. The results from this study were also negative. Although there is minimal regulatory confidence in the UDS assay, the results contributed to the weight of evidence argument. Based on the totality of information available, the positive acute in vivo micronucleus results were determined to be the result of an indirect mechanism. The safety margins established in the repeat-dose micronucleus assay were deemed sufficient to allow clinical development to proceed.
Both hyperthermia and hypothermia have been demonstrated to induce micronuclei via an indirect mechanism of action in both mice and rats, so the potential impact of body temperature changes should be considered when evaluating positive in vivo micronucleus results [17–20].
References
Escobar PA, Kemper RA, Tarca J, Nicolette J, Kenyon M, Glowienke S et al (2013) Bacterial mutagenicity screening in the pharmaceutical industry. Mutat Res 752(2):99–118
Khandoudi N, Porte P, Chtourou S, Nesslany F, Marzin D, Le Curieux F (2009) The presence of arginine may be a source of false positive results in the Ames test. Mutat Res 679(1–2):65–71
Thompson C, Morley P, Kirkland D, Proudlock R (2005) Modified bacterial mutation test procedures for evaluation of peptides and amino acid-containing material. Mutagenesis 20(5):345–350
Glatt H, Oesch F (1985) Mutagenicity of cysteine and penicillamine and its enantiomeric selectivity. Biochem Pharmacol 34(20):3725–3728
Aeschbacher HU, Finot PA, Wolleb U (1983) Interactions of histidine-containing test substances and extraction methods with the Ames mutagenicity test. Mutat Res 113(2):103–116
OECD (2013) Test No. 488: Transgenic rodent somatic and germ cell gene mutation assays, OECD guidelines for the testing of chemicals, section 4. OECD Publishing, Paris. doi:http://dx.doi.org/10.1787/9789264203907-en
Special issue of environmental molecular & mutagenesis focused on the Pig-a gene mutation assay (2011) 52(9):681–794
Kirkland D, Pfuhler S, Tweats D, Aardema M, Corvi R, Darroudi F, Elhajouji A, Glatt H, Hastwell P, Hayashi M, Kasper P, Kirchner S, Lynch A, Marzin D, Maurici D, Meunier J-R, Muller L, Nohynek G, Parry J, Parry E, Thybaud V, Tice R, van Benthem J, Vanparys P, White P (2007) How to reduce false positive results when undertaking in vitro genotoxicity testing and thus avoid unnecessary follow-up animal tests: Report of an ECVAM Workshop. Mutat Res 628:31–55
Scott D, Galloway SM, Marshall RR, Ishidate M, Brusick D, Ashby J, Myhr BC (1991) Genotoxicity under extreme culture conditions. A report from ICPEMC task group 9. Mutat Res 257:147–204
Lorge E, Moore MM, Clements J, O’Donovan M, Fellows M, Honma M, Kohara A, Galloway S, Armstrong MJ, Sutter A, Thybaud V, Gollapudi B, Aardema MJ, Tanir JY (2015) Standardized cell sources and recommendations for good cell culture practices in genotoxicity testing. Mutat Res (in preparation)
Parry JM, Parry EM, Boumer R, Doherty A, Ellard S, O’Donovan J et al (1996) The detection and evaluation of aneugenic chemicals. Mutat Res 353(1–2):11–46
Schuler M, Muehlbauer P, Guzzie P, Eastmond DA (1999) Noscapine hydrochloride disrupts the mitotic spindle in mammalian cells and induces aneuploidy as well as polyploidy in cultured human lymphocytes. Mutagenesis 14(1):51–56
Rao CV, Yamada HY, Yao Y, Dai W (2009) Enhanced genomic instabilities caused by deregulated microtubule dynamics and chromosome segregation: a perspective from genetic studies in mice. Carcinogenesis 30(9):1469–1474
Kirkland DJ, Aardema M, Banduhn N, Carmichael P, Fautz R, Meunier J-R, Pfuhler S (2007) In vitro approaches to develop weight of evidence (WoE) and mode of action (MoA) discussions with positive in vitro genotoxicity results. Mutagenesis 22:161–175
Thybaud V, Aardema M, Casciano D, Dellarco V, Embry MR, Gollapudi BB, Hayashi M, Holsapple MP, Jacobson-Kram D, Kasper P, MacGregor JT, Rees R (2007) Relevance and follow-up of positive results in in vitro genetic toxicity assays: an ILSI-HESI initiative. Mutat Res 633(2):67–79
Dearfield KL, Thybaud V, Cimino MC, Custer L, Czich A, Harvey JS, Hester S, Kim JH, Kirkland D, Levy DD, Lorge E, Moore MM, Ouedraogo-Arras G, Schuler M, Suter W, Sweder K, Tarlo K, van Benthem J, van Goethem F, Witt KL (2011) Follow-up actions from positive results of in vitro genetic toxicity testing. Environ Mol Mutagen 52(3):177–204
Asanami S, Shimono K (1997) High body temperature induces micronuclei in mouse bone marrow. Mutat Res 390(1–2):79–83
Asanami S, Shimono K (1997) Hypothermia induces micronuclei in mouse bone marrow cells. Mutat Res 393(1–2):91–98
Asanami S, Shimono K (2000) Effects of chemically- and environmentally-induced hypothermia on micronucleus induction in rats. Mutat Res 471(1–2):81–86
Asanami S, Shimono K (2009) Species-level differences between mice and rats in regards to micronucleus induction with the hypothermia-inducing drug haloperidol. Mutat Res 676(1–2):102–105
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Additional information
Disclaimer
The views expressed are those of the author. No official support or endorsement by the US Food and Drug Administration is provided.
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Custer, L.L., Powley, M.W. (2015). Genotoxicity Testing of API. In: Graziano, M., Jacobson-Kram, D. (eds) Genotoxicity and Carcinogenicity Testing of Pharmaceuticals. Springer, Cham. https://doi.org/10.1007/978-3-319-22084-0_3
Download citation
DOI: https://doi.org/10.1007/978-3-319-22084-0_3
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-22083-3
Online ISBN: 978-3-319-22084-0
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)