Abstract
To be familiar with anatomy and the microflora of the esophagus
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Foreign Body
- Transjugular Intrahepatic Portosystemic Shunting
- Esophageal Perforation
- Cervical Esophagus
- Food Bolus
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
FormalPara Objectives-
To be familiar with anatomy and the microflora of the esophagus
-
To assess and diagnose nontraumatic esophageal emergencies
-
To apply initial treatment in esophageal emergencies
-
To be familiar with surgical approach to the esophagus
-
To recognize prognostic determinants in esophageal emergencies
1 Introduction
Esophageal emergencies are associated with life-threatening complications when overlooked or subjected to delayed management. Nontraumatic esophageal emergencies encountered by the acute care surgeon comprise mainly esophageal perforation, caustic ingestion, foreign body obstruction, and esophageal hemorrhage.
1.1 Anatomical Considerations
-
The esophagus begins at the level of the sixth cervical vertebra/cricoid cartilage and extends to the cardia of the stomach, measuring 25–35 cm (40–50 cm from incisors) in length.
-
The cervical esophagus lies behind the trachea, anterior to the cervical spine between the common carotid arteries.
-
At the thoracic inlet, the esophagus is located behind the great vessels and trachea. It gradually assumes an almost left paravertebral location in the lower left chest.
-
The abdominal esophagus passes through the esophageal hiatus to join the cardia of the stomach.
-
-
Thyroid arteries, tracheobronchial arteries, branches of the descending aorta, left gastric artery, and splenic artery provide the arterial supply.
-
Two sphincter muscles, the UES (upper esophageal sphincter) and LES (lower esophageal sphincter), prevent regurgitation.
-
The esophagus has three major levels of constrictions; UES, aortic arch impression, and LES (Fig. 12.1).
-
The absence of a serosal layer in the esophagus increases risk of perforation and, when perforation occurs, adds greater likelihood of bacterial contamination.
1.2 Esophageal Microflora and Appropriate Antimicrobials
-
A mixed aerobic and anaerobic microflora inhabits the esophagus. Streptococci, Staphylococci, Klebsiella pneumoniae, and Escherichia coli predominate. The anaerobic species include Prevotella, Porphyromonas, Bacteroides fragilis, Fusobacterium, and Peptostreptococcus, in addition to frequent colonization with yeast found in obstructive diseases.
-
The optimal antimicrobial treatment in esophageal perforation is broad-spectrum antimicrobials such as cefoxitin sodium, clindamycin phosphate, beta-lactamase-resistant penicillins, and antifungal agents when appropriate.
2 Esophageal Perforation
-
The most frequent cause of esophageal perforation is instrumentation.
-
Diagnostic flexible endoscopy carries a relatively low overall perforation risk of 1:3000. Despite the low risk, it is a widely used diagnostic modality resulting in a significant number of esophageal perforations.
-
Diagnostic interventions such as Maloney bougienage, Savary pneumatic dilatation, through-the-endoscope hydrostatic balloon dilators, Sengstaken-Blakemore tube deployment, sclerotherapy, and banding in esophageal varices, and endotracheal intubation increase the risk of perforation, particularly in patients with esophageal pathology.
-
Dilatation in achalasia and strictures carry relatively higher perforation rates at 2–6 % and 0.3 %, respectively.
-
Esophageal perforation can occur also after surgical interventions such as fundoplication, esophageal myotomy, vagotomy, lung resection, thyroid surgery, tracheostomy, chest tube placement, mediastinoscopy, or spine surgery.
-
-
Spontaneous rupture of the esophagus caused by voluminous vomiting or retching is named after Dutch physician Hermann Boerhaave who described the condition in 1724.
-
The classic presentation of spontaneous perforation includes sudden retrosternal pain radiating to the neck associated with tachycardia and tachypnea.
-
Hematemesis is rarely seen in spontaneous perforation which helps distinguish it from the Mallory-Weiss tear.
-
Spontaneous rupture has been observed following blunt chest trauma, severe coughing, weightlifting, and childbirth.
-
2.1 Assessment and Diagnosis
-
The initial investigation includes history, examination, and chest radiography.
-
Signs and symptoms
-
Severe pain is the keystone manifestation of esophageal perforation.
-
Cervical or thoracic perforation is associated with sudden sharp pain in the neck or substernal area, respectively, shortly after the spontaneous perforation or esophageal instrumentation.
-
In addition, odynophagia, dysphagia, fever, subcutaneous emphysema, hemoptysis, or blood in nasogastric tube may be present.
-
-
Chest X-ray
-
Shows nonspecific findings such as mediastinal emphysema or pleural effusion in majority of cases (90 %).
-
An unexplained pleural effusion on chest radiography is suspicious for esophageal perforation.
-
Commonly, the perforation is confirmed with contrast esophagography (Fig. 12.2). The study is performed initially with water-soluble gastrografin because it is less harmful if it leaks into the mediastinum. However, if aspirated into the tracheobronchial tree or leaks through a tracheoesophageal fistula into the lungs, gastrografin may cause severe pneumonitis.
-
The optimal diagnostic accuracy is obtained with thin barium esophagography performed in decubitus position for slower-contrast transit time through the esophagus. Barium contrast has superior radiologic density and delineates mucosa better. With negative good-quality barium study, the perforation is unlikely.
-
-
Multidetector computed tomography (MDCT) and MDCT esophagography has shown a high accuracy for esophageal perforations. Screening chest MDCT may depict mediastinal air, air-fluid collections communicating with esophageal air, or an abscess adjacent to esophagus. Directed MDCT esophagography may confirm perforation demonstrating leakage of contrast media into mediastinum or pleural space. In patients with empyema, thoracentesis may yield pus-containing food particles.
-
In summary, a high index of suspicion must be maintained in suspected esophageal perforation because outcome depends entirely on timely diagnosis and prompt management.
2.2 Treatment
-
Therapeutic options in esophageal perforation depend on the anatomical site of the perforation, underlying pathology, time to diagnosis, signs of severe sepsis, and extent of the perforation and leak.
-
Although surgery is the gold standard in the management of esophageal perforation, not all esophageal perforations require operative management.
2.2.1 Nonoperative Management (NOM)
-
Is feasible in patients suffering small, contained perforations with no signs of sepsis, especially in the cervical esophagus
-
Criteria for NOM include intramural perforation, contained perforation communicating with esophagus, non-stricture and nonmalignant perforation associated with mild degree of sepsis.
-
Some recent evidence advocates nonoperative “aggressive conservatism” that includes antibiotic treatment, aggressive drainage of mediastinal and chest collections, and sequential imaging
-
The principles of NOM include restriction of oral intake, broad-spectrum antibiotics, CT-guided drainage of any fluid collections in the neck or the mediastinum, and parenteral nutrition.
-
Endoscopically placed stents in selected cases have been used with good success (Fig. 12.3).
2.2.2 Operative Management
2.2.2.1 Surgery
-
The cornerstone of therapy in uncontained perforations and in all patients with severe sepsis or septic shock.
-
Options include drainage alone, primary repair, diversion, or esophagectomy depending on the site of perforation, pathology, severity of sepsis, and the interval from perforation to diagnosis. While immediate diagnosis of perforation without preexisting pathology allows primary repair, in those patients with preexisting disease or delay in diagnosis, primary repair will likely fail with devastating septic complications. Even after meticulous surgical repair, leak rates range from 25 % to 50 % mandating placement of closed suction drains near the repair.
2.2.2.2 Surgical Approaches
2.2.2.2.1 Cervical Esophagus
-
The cervical esophagus is relatively easy to approach using the left unilateral sternocleidomastoid incision.
-
Two-layer repair should be used: a running absorbable suture to the mucosa followed by an interrupted suture line to the muscular layer.
-
It is crucial to extend the myotomy to assess the entire mucosal length of the defect.
-
The mucosal primary repair can be carried out over a large bougie.
-
-
The sternocleidomastoid or omohyoid muscle can be placed over the repair
-
There is no evidence that nasogastric tube following cervical esophageal repair provides diversion of saliva and may compromise the tenuous repair and healing of the wound.
2.2.2.2.2 Thoracic Esophagus
-
Thoracic esophageal perforations are repaired through a right fourth to fifth or a left sixth to seventh intercostal posterolateral thoracotomy (Fig. 12.4).
-
Running absorbable suture line for mucosa and interrupted absorbable for muscular layer is appropriate.
-
In mid and lower esophageal repairs, a diaphragmatic buttress flap can be utilized.
-
For that purpose, rotation-flap constructed from the posterior aspect of diaphragm is sutured over the esophageal repair. The diaphragmatic defect is primarily closed.
-
-
In preexisting disease without significant contamination, resection of a tumor, myotomy for strictures, or antireflux procedure may be feasible.
-
Esophagectomy with primary reconstruction.
-
May be successful in minimal contamination.
-
In severe contamination and inflammation, diversion is appropriate. Closure of the perforation with proximal and distal staple line, resection of the diseased segment, and a proximal esophagostomy is established with wide drainage and gastrostomy tube for feeding. Major esophageal reconstruction is required at later stage.
-
Another option includes closure of the wound over a 24-French T-tube drainage brought out to the chest wall and placement of chest drainage (Fig. 12.5).
-
2.2.2.2.3 Abdominal Esophagus
-
Abdominal esophagus is accessed via laparotomy or more often via a thoracoabdominal incision.
-
A self-retaining retractor system is of great value for optimal exposure of the gastroesophageal junction.
-
-
The defect with minor contamination is debrided and repaired in two layers added by buttressing with a stomach patch around the repair site. More destructive injuries may require resection of the affected segment, mobilization of the stomach, and esophagogastrostomy in the chest.
-
In benign conditions with extensive tissue loss, resection of the esophagus and reconstruction with colon interposition may be needed.
3 Caustic Ingestion
-
Most commonly encountered in children and in young adults when ingestion is accidental or intentional, respectively.
-
The degree of injury depends on the nature of the ingested substance, concentration, quantity, and duration of the caustic agent exposure.
-
Hence, adults frequently sustain more severe injuries as the ingested volumes are larger.
-
-
The most prominent sites of caustic lesions are the natural narrowings of the esophagus including UES, aortic impression, and LES.
-
Alkaline agents cause liquefying necrosis resulting in deep burns, whereas acids cause coagulative necrosis resulting in eschar that limits deep tissue penetration.
3.1 Assessment and Diagnosis
-
Signs and symptoms
-
The typical patient presents with oral pain, extensive drooling, and dysphagia.
-
Stridor and hoarseness are signs of impending airway obstruction.
-
Retrosternal and abdominal pain are signs of possible intrathoracic or intra-abdominal perforation.
-
Extensive supraglottic edema may require emergent tracheotomy.
-
-
Investigations:
-
Chest and abdominal radiography are obtained to exclude extraluminal air.
-
Multidetector CT is more sensitive for mediastinal air indicating perforation.
-
-
Indications
-
In established perforation, septic shock or peritonitis mandates immediate operative intervention.
-
All patients with stridor, intentional ingestion, and symptomatic children require endoscopy to evaluate extent of injury within 24 h.
-
Asymptomatic children and patients who require surgery precludes need for endoscopy.
-
Endoscopic evaluation classifies injuries into first degree (edema, hyperemia), second degree (ulceration), and third degree (black discoloration indicating full-thickness injury).
-
3.2 Treatment
-
Immediate goal of therapy is airway assessment, fluid resuscitation, and careful monitoring.
-
No oral neutralizing agents have shown to improve outcomes, and nasogastic tube is contraindicated as it may cause perforation or emesis and aspiration.
-
-
First-degree injuries
-
Require at least 24 h observation prior to diet advancement
-
-
Second-degree injuries
-
More extensive second-degree injuries that do not require surgery should be treated with antibiotics and gastric acid suppression and monitored closely.
-
Deep second-degree caustic injuries develop strictures in 70 % and should be monitored for a minimum of 48 h (Fig. 12.6).
-
Patients who will be able to swallow saliva and show no signs of sepsis can advance diet as tolerated. Repeat swallow studies are planned 3 weeks, 3 months, and 6 months after injury.
-
Steroids are of no benefit, do not reduce the incidence or severity of late strictures in second-degree injuries, and may increase the risk of infectious complications.
-
-
Third-degree injuries
-
Develop strictures in up to 90 % and progress to perforation in 25 % of cases.
-
Signs of full-thickness caustic injury include peritonitis, depressed mental status, shock, severe acidosis, and free air on abdominal film.
-
If surgery is indicated:
-
The optimal approach to the esophagus is via the abdominal cavity as it allows evaluation of the stomach, resection of adjacent injured organs, establishment of feeding jejunostomy, and esophagectomy through a transhiatal approach.
-
Cervical esophagectomy is performed through the neck incision.
-
-
Nutrition will be provided via gastrostomy/jejunostomy.
-
-
Unlike other inflammatory causes of the foregut scarring, caustic scarring is aggressive and may progress beyond a year after injury.
-
Options for delayed reconstruction are colonic interposition or gastric pull-up if the stomach sustained less significant insult.
4 Esophageal Foreign Bodies
-
Acute care surgeons frequently encounter patients with foreign body ingestion or food impaction. The vast majority of swallowed material will pass the gut uneventfully. Nevertheless, 10–20 % will require nonoperative intervention, and 1 % or less will require surgery. Recent series have reported low mortality rates in these instances. However, overall 1500 individuals die worldwide annually due to ingested foreign bodies in the foregut. The history should focus on the type of foreign body and symptoms suggesting gut perforation.
4.1 Causes
-
Foreign body
-
Occurs predominantly in children with the highest incidence from 6 months to 3 years.
-
Battery ingestion with impaction in the esophagus requires emergent intervention (common in children) because of risk of direct alkaline injury to the esophagus.
-
-
In the adult population, there is a strong association with psychiatric diseases. Other risk factors for foreign body obstruction include dentures, bridge work, and preexisting esophageal pathology.
-
Impaction occurs in areas of esophageal narrowing; UES (15–17 cm from incisors), the aortic impression (23 cm), the left mainstem bronchus (27 cm), and the LES (36–38 cm).
-
-
Food bolus impaction
-
A common esophageal emergency, especially in elderly people.
-
4.2 Food Impaction
-
Meat bolus is the predominant offending agent causing 80–90 % of food obstructions.
-
More frequently noted in elderly and in the edentulous.
-
Signs and symptoms
-
Food bolus impaction in the cervical esophagus may present with stridor, dysphagia, odynophagia, or shortness of breath. The Heimlich maneuver is the treatment.
-
More frequently, a complete obstruction occurs in the distal esophagus and the patient presents with significant sialorrhea and regurgitation.
-
History should include preexisting esophageal conditions such as previous dysphagia or dilatation, Nissen fundoplication, gastric bypass, or stent placement.
-
-
Management
-
Medical therapy utilizing glucagon is the initial modality. Glucagon relaxes the LES, decreasing the resting LES pressures up to 60 %. The common initial dose is 0.5 mg and can be increased to 2 mg intravenously. Some reports describe using glucagon and diazepam simultaneously with high success rates.
-
Most patients with an impacted food particle require flexible endoscopy for extraction or push of the particle distally to the stomach. Early removal is recommended to avoid pressure-induced ischemia in the esophagus.
-
Extraction of the food bolus is attempted first, particularly if the bolus is large and contains sharp particles such as bones or if a preexisting stricture is present.
-
A Roth retrieval net can be used with the advantage of complete encompassment of the food bolus precluding aspiration.
-
Another option for extraction is a polypectomy snare. In this setting, the endoscope along with snared food bolus is extracted to the level of UES and pulled against the endoscope while the patients’ neck is extended and the endoscope is removed with food bolus.
-
If extraction of the foreign body fails, push method is used.
-
Push method can be considered only when the bolus is soft and contains no sharp objects and no esophageal stricture is present.
-
In this technique, slight pressure can be applied to the right side of the food bolus as the bolus passes from right to left more easily.
-
-
A combination of scope-pushing and intravenous glucagon has been reported as a successful intervention.
-
In all instances, preexisting esophageal disease work-up is considered.
-
-
-
4.3 Indigestible Foreign Body Obstruction
-
The variety of ingestible foreign bodies is extensive in the literature including bones, pills, dental hardware, toothpicks, safety pins, glass, coins, and batteries (Fig. 12.7).
-
Signs and symptoms
-
A complete esophageal obstruction is rarely encountered and saliva can be swallowed.
-
Careful initial examination is mandatory to exclude esophageal perforation and impending sepsis.
-
-
Diagnosis
-
The chest radiography may demonstrate a radiopaque foreign body.
-
Abdominal X-ray may reveal passage or previously ingested foreign bodies or free air.
-
-
Management
-
Majority of ingested foreign bodies will pass in the stool; however, those obstructing the esophagus are lodged commonly in the proximal esophagus.
-
Objects found in the pharynx or UES are removed by direct or rigid laryngoscopy.
-
Foreign bodies in the esophagus without sharp edges such as coins, toothbrushes, and batteries can be extracted with flexible endoscopy.
-
Batteries lodged in esophagus should in general be removed. Many batteries contain alkaline substances and can result in alkaline injury.
-
-
Endoscopy
-
Use the largest scope suitable for the patient with the biggest suction channel for debris and saliva suction.
-
Polypectomy snare, Roth retrieval net, or grasp forceps are utilized for extraction (Fig. 12.8). In difficult cases, a rigid scope may be more effective for the extraction. After the object is snared or grasped, the endoscope is extracted along with the object to the level of cricopharyngeal muscle, and then the object is snugly brought against the scope and extracted together with the endoscope. Neck extension may help, and care should be given not to lose the grasp as it may be aspirated into the airway.
-
Sharp objects in the esophagus must be retrieved because the perforation risk is considerable at 15–35 %. The sharp objects can be grasped with endoscopy forceps and removed through an overtube or with rotatable removal basket.
-
-
5 Esophageal Bleeding
-
Rare
-
The common etiology of esophageal hemorrhage includes gastroesophageal reflux disease (GERD), Mallory-Weiss mucosal tear, or variceal bleeding
-
GERD
-
Although the hemorrhage due to GERD esophagitis is fairly uncommon, the relatively high overall incidence of GERD makes this clinical entity quite frequent (Fig. 12.9).
-
The diagnosis and the extent of the disease are confirmed by endoscopy. Any bleeding source in the stomach and duodenum should be excluded.
-
Management
-
Discontinue aspirin and NSAIDs and treat with proton pump inhibitors intravenously, in conjunction with resuscitation.
-
The definitive treatment in GERD is abolishing the acid reflux either by prolonged proton pump inhibitors or fundoplication.
-
-
-
Mallory-Weiss tear
-
More common in male patients.
-
Aspirin or alcohol use is frequently noted in the history (31–80 %).
-
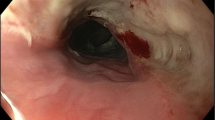
The typical patient presents with hematemesis following retching or vomiting. In 5–10 % of cases, hemodynamic compromise and massive hematemesis are seen. The diagnosis is confirmed by endoscopy with the common finding a mucosal tear within 2 cm from the gastroesophageal junction (Fig. 12.10).
-
Other preexisting esophageal lesions are frequently observed at endoscopy.
-
About 90 % of patients with Mallory-Weiss hemorrhage stop bleeding without intervention.
-
-
Esophageal varices (Fig. 12.11)
-
Diagnosis is easy in the context of liver cirrhosis.
-
Primary intervention includes airway protection, insertion of nasogastric tube, establishment of reliable intravenous access, transfusion of blood products, reversal of coagulopathy, proton pump inhibitor, and emergent endoscopy with sclerorotherapy and/or variceal ligation (Fig. 12.12).
-
Overall, 5–10 % of variceal bleeding is not controlled with endoscopic treatment and requires Sengstaken-Blakemore or Linton-Nachlas tube for hemorrhage control while considering interventional radiological percutaneous transhepatic embolization or transjugular intrahepatic portosystemic shunting (TIPS) (Fig. 12.13).
-
Adjuvant medical therapy with nonselective beta-blockers, vasopressin analogues, and octreotide may be considered.
-
-
Selected Reading
Biancari F, D’Andrea V, Paone R, et al. Current treatment and outcomes of esophageal perforations in adults: meta-analysis and meta-regression of 75 studies. World J Surg. 2013;37:1051–9.
Brinster CJ, Singhal S, Lee L, Marshall MB, Kaiser LR, Kucharczuk JC. Evolving options in the management of esophageal perforation. Ann Thorac Surg. 2004;77(4):1475–83. doi:10.1016/j.athoracsur.2003.08.037.
Cameron JL, Kieffer RF, Hendrix TR, Mehigan DG, Baker RR. Selective nonoperative management of contained intrathoracic esophageal disruptions. Ann Thorac Surg. 1979;27(5):404–8.
Cattan P, Munoz-Bongrand N, Berney T, Halimi B, Sarfati E, Celerier M. Extensive abdominal surgery after caustic ingestion. Ann Surg. 2000;231(4):519–23.
de Jong AL, Macdonald R, Ein S, Forte V, Turner A. Corrosive esophagitis in children: a 30-year review. Int J Pediatr Otorhinolaryngol. 2001;57(3):203–11.
Duncan M, Wong RK. Esophageal emergencies: things that will wake you from a sound sleep. Gastroenterol Clin North Am. 2003;32(4):1035–52.
Fulton JA, Hoffman RS. Steroids in second degree caustic burns of the esophagus: a systematic pooled analysis of fifty years of human data: 1956–2006. Clin Toxicol (Phila). 2007;45(4):402–8. doi:10.1080/15563650701285420.
Garcia-Pagan JC, Morillas R, Banares R, et al. Propranolol plus placebo versus propranolol plus isosorbide-5-mononitrate in the prevention of a first variceal bleed: a double-blind RCT. Hepatology. 2003;37(6):1260–6. doi:10.1053/jhep.2003.50211.
Longstreth GF, Longstreth KJ, Yao JF. Esophageal food impaction: epidemiology and therapy. A retrospective, observational study. Gastrointest Endosc. 2001;53(2):193–8.
Muir AD, White J, McGuigan JA, McManus KG, Graham AN. Treatment and outcomes of oesophageal perforation in a tertiary referral centre. Eur J Cardiothorac Surg. 2003;23(5):799–804; discussion 804.
Patch D, Sabin CA, Goulis J, et al. A randomized, controlled trial of medical therapy versus endoscopic ligation for the prevention of variceal rebleeding in patients with cirrhosis. Gastroenterology. 2002;123(4):1013–9.
Suarez-Poveda T, Morales-Uribe CH, Sanabria A, Llano-Sánchez A, Valencia-Delgado AM, Rivera-Velázquez LF, Bedoya-Ospina JF. Diagnostic performance of CT esophagography in patients with suspected esophageal rupture. Emerg Radiol. 2014;21(5):505–10. doi:10.1007/s10140-014-1222-4. Epub 2014.
Tanomkiat W, Galassi W. Barium sulfate as contrast medium for evaluation of postoperative anastomotic leaks. Acta Radiol. 2000;41(5):482–5.
van Heel NC, Haringsma J, Spaander MC, Bruno MJ, Kuipers EJ. Short-term esophageal stenting in the management of benign perforations. Am J Gastroenterol. 2010;105(7):1515–20. doi:10.1038/ajg.2010.104.
Vicari JJ, Johanson JF, Frakes JT. Outcomes of acute esophageal food impaction: success of the push technique. Gastrointest Endosc. 2001;53(2):178–81.
Vogel SB, Rout WR, Martin TD, Abbitt PL. Esophageal perforation in adults: aggressive, conservative treatment lowers morbidity and mortality. Ann Surg. 2005;241(6):1016–21; discussion 1021–3.
Zwischenberger JB, Savage C, Bidani A. Surgical aspects of esophageal disease: perforation and caustic injury. Am J Respir Crit Care Med. 2002;165(8):1037–40.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Demetriades, D., Talving, P., Lam, L. (2016). Esophageal Emergencies. In: Fingerhut, A., Leppäniemi, A., Coimbra, R., Peitzman, A., Scalea, T., Voiglio, E. (eds) Emergency Surgery Course (ESC®) Manual. Springer, Cham. https://doi.org/10.1007/978-3-319-21338-5_12
Download citation
DOI: https://doi.org/10.1007/978-3-319-21338-5_12
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-21337-8
Online ISBN: 978-3-319-21338-5
eBook Packages: MedicineMedicine (R0)