Abstract
The response of left ventricular function to ischemia is monotonous and independent of the stress employed [1]. The same echocardiographic signs can be found in transient ischemia and acute infarction. The difference lies in the time sequence, and from an echocardiographic viewpoint, myocardial ischemia is a “reversible” myocardial infarction. The cardinal sign of ischemia is the transient, regional wall motion abnormality – the cornerstone of diagnosis. There are other ancillary signs of severity which may occasionally help in disease severity stratification, such as left ventricular cavity dilation, acute severe mitral insufficiency, fall of stroke volume, and the appearance of ultrasound B-lines in the chest. In cutting-edge stress echocardiography environments, today wall motion analysis can be coupled during vasodilator stress with assessment of coronary flow reserve – further expanding our diagnostic and prognostic information during stress echocardiography.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Wall Motion
- Coronary Flow Reserve
- Stress Echocardiography
- Regional Wall Motion Abnormality
- Vasodilator Stress
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
The response of left ventricular function to ischemia is monotonous and independent of the stress employed [1]. The same echocardiographic signs can be found in transient ischemia and acute infarction. The difference lies in the time sequence, and from an echocardiographic viewpoint, myocardial ischemia is a “reversible” myocardial infarction. The cardinal sign of ischemia is the transient, regional wall motion abnormality – the cornerstone of diagnosis. There are other ancillary signs of severity which may occasionally help in disease severity stratification, such as left ventricular cavity dilation, acute severe mitral insufficiency, fall of stroke volume, and the appearance of ultrasound B-lines in the chest. In cutting-edge stress echocardiography environments, today wall motion analysis can be coupled during vasodilator stress with assessment of coronary flow reserve – further expanding our diagnostic and prognostic information during stress echocardiography.
Contrast myocardial perfusion imaging, although technically more complicated and requiring the injection of contrast media, is also potentially clinically useful for diagnosis and prognosis, but to date, its use has remained mostly confined to research (Table 6.1).
1 The Main Sign of Ischemia: Regional Wall Motion Abnormalities
Normal myocardium shows systolic thickening and endocardial movement toward the center of the cavity. The hyperkinesia indicates an increase in normal movement and thickening (Table 6.2).
The hallmark of transient myocardial ischemia is regional asynergy (or dyssynergy) in its three degrees: hypokinesia (decreased movement and systolic thickening), akinesia (absence of movement and systolic thickening), and dyskinesia (paradoxical outward movement and possible systolic thinning). Obviously, this description is arbitrarily focused on three points of a continuous spectrum of mechanical modifications induced by ischemia. From a clinical point of view, the reliability of hypokinesia is reduced because of a greater intra- and interobserver variability. In contrast, akinesia and dyskinesia reflect more marked modifications of regional mechanics with smaller interobserver discordance. From a pathophysiological viewpoint, the severity of dyssynergy is correlated to the severity and transmural extension of the flow deficit [2]. Virtually all approaches and all projections can be utilized to document regional dyssynergy. From each projection, an M-mode line of view can help document the asynergy, thanks to the better axial resolution and the easier quantification of the time-motion tracings when compared with the B-mode images. The M-mode tracing must be perpendicular to the ischemic region and geometrically controlled from the bidimensional image. The evaluation of a segmentary dyssynergy is easier in a ventricle with normal baseline function than in a ventricle with a resting asynergy. In the latter case, the stress can induce a homozonal ischemia in the infarcted area: for instance, a hypokinetic zone becomes akinetic. The stress-induced worsening of a baseline dysfunction (so-called homozonal ischemia) indicates a residual critical stenosis in the infarct-related coronary artery and the presence of jeopardized myocardium in the infarcted area. Homozonal residual ischemia may also involve a segment adjacent to the necrotic area but belonging to the distribution territory of the same coronary artery. In contrast, heterozonal ischemia develops in an area remote from the necrotic segment and supplied by a different coronary artery. Heterozonal ischemia is very specific for multivessel coronary disease. The reduced regional systolic thickening is theoretically more sensitive and specific than wall motion [2]. In fact, the latter – unlike the thickening – can remain unmodified during ischemia due to a passive movement transmitted by neighboring regions where perfusion and contraction are normal. In practice, regional movement and systolic thickening tend to be symmetrically affected with the exception of a few pathological situations (i.e., postsurgical septum after bypass intervention, left bundle branch block, or right ventricular pacing) in which the two parameters may dissociate, with alterations of movement and normal thickening. In these cases, it is essential to evaluate only the systolic thickening both in resting conditions and during stress.
2 Stress Echo in Four Equations
All stress echocardiographic diagnoses can be easily summarized in four equations centered on regional wall function and describing the fundamental response patterns: normal, ischemic, viable, and necrotic (Table 6.3). The possible mechanical patterns are schematically shown in Fig. 6.1 along with their myocardial and coronary correlates.
Stress echographic patterns of normal (upper row), ischemic (second row), viable (third row), and necrotic (fourth row) responses are schematically represented. On the left side, the corresponding schemes of the coronary artery (parallel lines) and the myocardium (box) are shown. A normal myocardium is represented as a white box, a necrotic myocardium as a black box, and a viable myocardium as a gray box. In a normal segment fed by a normal coronary artery, the segment is normokinetic at rest and normal–hyperkinetic during stress (upper row). In a normal myocardium fed by a critically stenosed coronary artery, the segment is normokinetic at rest and hypokinetic, akinetic, or dyskinetic during stress (second row). A viable segment (third row) is akinetic at rest and normal during stress. A necrotic segment shows a fixed wall motion abnormality at rest and during stress (lower row)
The corresponding stress echocardiography patterns are displayed in Fig. 6.2.
Echocardiographic examples of normal (upper row), ischemic (second row), viable (third row), and necrotic (fourth row) responses. On the left side, the end-systolic frames of a rest (left part) and a stress (right part) study are shown. In a viable myocardium with resting dysfunction and fed by a coronary artery with noncritical coronary stenosis, the segment is hypokinetic or akinetic at rest and normokinetic during stress (third row). Necrotic tissue shows unchanged function throughout the test, regardless of the underlying anatomical condition of the infarct-related vessel (fourth row)
In the normal response, a segment is normokinetic at rest and normal–hyperkinetic during stress. In the ischemic response, the function of a segment worsens during stress from normokinesis to dyssynergy. In the viable response, a segment with resting dysfunction improves during stress. In the necrotic response, a segment with resting dysfunction remains fixed during stress. A resting akinesia that becomes dyskinesia during stress reflects a purely passive, mechanical phenomenon of increased intraventricular pressure developed by normally contracting walls and should not be considered a true active ischemia [3]. It is conceptually similar to the increase in ST-segment elevation during exercise in patients with resting Q waves.
In the jeopardized pattern, a segment with resting hypokinesis becomes akinetic or dyskinetic during stress. A viable response at low dose can be followed by an ischemic response at high dose; the “biphasic” response is suggestive of viability and ischemia, with jeopardized myocardium fed by a critically stenosed coronary artery [4].
3 False-Negative Results
A stress echocardiography examination can be normal in the presence of angiographically assessed coronary artery disease (Table 6.4). This happens more frequently with submaximal stresses which do not test the coronary circulation efficiently. With maximal stress, a false-negative response is found more frequently in the presence of less extensive (single-vessel disease) or less severe (50–75 % stenosis) coronary disease and especially on the left circumflex coronary artery [5]. Not all coronary stenoses were created equal and – when a maximal stress is administered – those with a negative stress echocardiography response are less severe from the anatomic [6], functional [7], and prognostic [8] points of view. Antianginal therapy lowers the sensitivity of exercise echocardiography as it does with vasodilator stresses [9, 10]. Dobutamine stress results are much less affected by calcium-channel blockers and nitrate therapy [11, 12]. In some cases, true ischemia occurs but may go undetected by stress echocardiography, especially in less well-imaged segments, such as the inferior wall, because of the inherent limitations of subjective analysis and lack of quantitative criteria. In these cases, cine-magnetic resonance imaging (MRI) documents a true impairment in regional systolic thickening [13]. Contrast echocardiography, applied to achieve better wall motion assessment alone, or even more when taking advantage of myocardial perfusion imaging, increases the sensitivity for the diagnosis of coronary stenosis, at lower cost and logistic complexity than MRI [14–16].
4 False-Positive Results
A transient alteration of regional function represents a very specific sign of myocardial ischemia. Nevertheless, false-positive results in stress echocardiography do exist and occur with (Table 6.5) or without (Table 6.6) true induced ischemia. Even with a nonsignificant stenosis at coronary angiography, a stress test for coronary artery disease can induce true ischemia and asynergy by triggering a coronary vasospasm in susceptible patients. Stress-induced coronary vasospasm has been described with exercise [17], dobutamine [18, 19] (Fig. 6.3), or dipyridamole (more frequently during or following aminophylline) [20].
Normal coronary angiogram (left upper panel), spontaneous spasm of the left anterior descending coronary artery of the same patient (right upper panel, indicated by arrow), and end-systolic frames of the patient in two-chamber view at rest (left lower panel) and at peak stress (right lower panel) with clear akinesia of the apex (Modified from Varga et al. [19])
Coronary spasm is easily recognized when it is associated with transient ST-segment elevation during stress, but frequently it also occurs with ST-segment depression or even with no obvious changes on the ECG. True ischemia can also be found in patients with an angiographic stenosis below the “magic” 50 % but with a physiologically important reduction in flow reserve. In this case, the regional dysfunction during stress echocardiography is a “false-positive” vs the angiographic standard but a “true positive” vs a more accurate descriptor of anatomy such as intracoronary ultrasound [21]. True stress-induced ischemia may occur in the presence of occult cardiomyopathy [22]. The incipient muscle disease may not be overt at rest, but a chronotropic and afterload challenge associated with stress can unmask a true regional dysfunction – destined to progress over time to frank cardiomyopathy. An extreme reduction in coronary flow reserve usually associated with left ventricular hypertrophy [23, 24] may also provoke stress-induced ischemia. As described in Chap. 30, microvascular angina typically occurs with chest pain, ST-segment depression, and perfusion abnormalities without wall motion change [25]. However, in extreme left ventricular hypertrophy and especially in aortic stenosis, in which there is a critical contribution of increased end-systolic wall stress of the left ventricle, true extensive subendocardial hypoperfusion can develop [26] with real wall motion abnormalities [24]. Finally, an excessive systolic blood pressure rise during exercise may increase disproportionately the afterload determining a wall motion abnormality [27] – often severe and in multiple regions – in the left ventricle (Fig. 6.4).
Sensitivity (empty bars) and specificity (full bars) of exercise echocardiography according to peak systolic blood pressure response during exercise (Modified from Ha et al. [27])
Stress-induced high heart rate [28] and high blood pressure [29] may reduce regional systolic thickening in normal subjects as well. False-positive results may occur in the absence of a true ischemic asynergy, due to a mistake in the acquisition and/or interpretation and/or analysis. Human error determining a false-positive result is more frequent with aggressive reading criteria (for instance, lack of hyperkinesia) and with stressors polluting image quality and determining marked increase in heart rate and contractility, which inflate the number of indeterminate or ambiguous results. In fact, a relative lack of hyperkinesis, or even a true hypokinesia, can be a part of the physiological response by a completely normal ventricle to an inotropic stress [30, 31]. False-positive results and angiographically defined stenosis are also more frequently found when using contrast myocardial perfusion imaging, due to its inherent ability to detect minor reductions in the expected normal increase in myocardial blood flow after a given stressor. In fact, these reductions are also seen in microvascular disease, initial cardiomyopathy, and several other conditions, independently from the presence of flow-limiting epicardial coronary artery disease [32].
Last but not least, no left ventricle can be called free of artifactual asynergies. Spurious off-axis projections can create artifactual asynergies – more frequent in basal and inferoposterior regions.
5 The True Meaning of “False” Stress Echo Results
Even the best laboratory will have a “physiological” percentage of false-positive and false-negative results. Obviously, this percentage of stress echocardiography “lies” will be higher with inexperienced readers and with stresses polluting image quality (exercise and dobutamine more than dipyridamole). Patients with variant angina, severe left ventricular hypertrophy, and uncontrolled hypertension have a greater chance of false-positive responses; patients studied under full anti-ischemic therapy will have a greater chance of false-negative responses. If the rate of false responses exceeds the expected average of 20 %, the method should be reassessed. The “angiographic lies” of stress echocardiography can turn out to be striking “prognostic truths” in the long run, overruling the prognostic stratification provided by the anatomic gold standard of coronary angiography. Therefore, in the anatomically defined subset of patients with single-vessel disease, patients with negative stress echocardiography findings (“false negative”) have a good prognosis, better with medical therapy rather than with anatomy-guided revascularization [8]. Patients with angiographically normal coronary arteries and with stress echocardiography positivity (false-positive result) have a greater chance of adverse events in the long run [33].
6 Ancillary Signs of Ischemia
With stress scintigraphy, left ventricular cavity dilation and lung tracer uptake reflect late signs of global pump dysfunction and increase in pulmonary wedge pressure with interstitial lung edema. Also during stress echocardiography, we can sometimes observe poorly sensitive but highly specific signs of extensive ischemia, severe underlying coronary artery disease, and ominous prognostic outcome (Fig. 6.5): a stroke volume fall [34, 35]; a transient dilation of the left ventricular cavity (>20 % from baseline of end-systolic diameter) [36]; the development of severe acute mitral insufficiency [37, 38]; an increase in B-lines, a sign of extravascular lung water accumulation (detectable with lung ultrasound by placing the cardiac echocardiography probe on the third right intercostal space) [39, 40]; and the rise in pulmonary artery systolic pressure [41].
The main ancillary signs of severity and their frequently used cutoff values are summarized in Table 6.7.
7 Beyond Regional Wall Motion: Coronary Flow Reserve
In the last decade, the old dream of combining wall motion with a simultaneous assessment of coronary flow reserve became a reality in the echocardiography laboratory. There are conceptual and methodological differences between myocardial perfusion and coronary flow reserve, since perfusion requires contrast opacification of the myocardium and coronary flow reserve assesses the vasodilating capacity of the coronary artery (see Chap 9). However, both mirror information on coronary vasodilating capability, which requires the full integrity of the epicardial (proximal, upstream) and microcirculatory (distal, downstream) components of the coronary circulation. In the nuclear medicine and cardiovascular magnetic resonance stress laboratory, perfusion is usually evaluated. In the stress echocardiography laboratory, more than a decade of attempts with myocardial contrast echocardiography led to disappointing results, due to the long learning curve required to perform and interpret contrast myocardial perfusion imaging [42]. On the contrary, the diffusion of assessment of coronary flow reserve in the left anterior descending coronary artery was rapidly accepted in the clinical arena and led to a remodeling of our diagnostic equations. There are differences between wall motion and reduction of coronary flow reserve as diagnostic markers, since only the former requires true ischemia, is affected by antianginal therapy, and is sensitive to epicardial stenosis and much less sensitive to purely microvascular coronary impairment (Table 6.8).
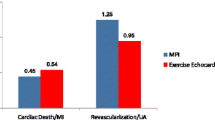
As a consequence, the diagnostic signs shown in Fig. 6.1 can be expanded to include coronary flow reserve as shown in Fig. 6.6. Normal function with normal coronary flow reserve (in the left anterior descending and right coronary artery) expresses the absence of anatomic and functionally significant stenosis of the epicardial artery and microcirculatory integrity. On the contrary, a normal wall motion with abnormal coronary flow reserve is associated with either a mild-to-moderate hemodynamically significant epicardial stenosis or significant microcirculatory disease [46]. The two markers are also prognostically complementary, since wall motion abnormalities identify troublemakers in the short run (months) and coronary flow reserve reduction – in the absence of wall motion disturbances – identifies troublemakers in the long run (years). With the abovementioned limitation of significant technical complexity, the addition of contrast myocardial perfusion imaging to stress echocardiography has also demonstrated diagnostic and prognostic advantages over stand-alone wall motion assessment, similar to Doppler coronary flow reserve in the left anterior descending artery, but with the additional advantage of full coverage of the three coronary artery territories [14–16, 44].
Pathophysiological and prognostic heterogeneity behind normal wall motion response during stress. In the upper panel, we show epicardial coronary arteries: normal in the first two columns, with moderate disease in the third column and moderate-to-severe disease but concomitant, effective anti-ischemic therapy in the last column. The myocardium is shown as a square box, with small vessels as circles. Coronary small vessel disease is shown (second column) as bold circles (structural or functional impairment). All four very different pathophysiological conditions show the negativity of wall motion response. The abnormal coronary flow reserve (CFR) response is present in the last three columns, with abnormality of micro- or macrocirculation. Reversible myocardial perfusion defects behave similarly to CFR, since in fact they reflect myocardial blood flow reserve, with the advantage that myocardial perfusion imaging can indifferently assess all of the three coronary territories. In case of microvascular disease, the strictly subendocardial perfusion defects typically extend across the boundaries of a single coronary territory (Modified from Rigo et.al. [46])
8 Contrast Perfusion Stress Echocardiography
Stress echocardiography has been revolutionized by the availability of stable gas-filled microbubbles, which via a simple peripheral venous injection may offer the following multifaceted advantages:
-
(a)
Opacification of heart chambers (Fig. 6.7), making wall motion assessment of the left ventricle:
Fig. 6.7 The use of contrast for the enhancement of the LAD color flow in technically difficult cases, in which rest coronary flow is difficult to localize. Figure (lower part) also shows the downside of noisier pulsed-wave Doppler tracings, although quality is usually sufficient for the measurement of diastolic peak velocities
-
More reproducible among different readers [47]
-
Slightly but significantly more accurate [48] and
-
More feasible for almost the totality of patients, including the small but existing percentage of technically inadequate patients in whom stress echocardiography was previously precluded and stress MRI was considered as the only alternative for wall motion assessment
-
-
(b)
Enhancement of color Doppler imaging of the mid-distal left anterior descending artery, increasing feasibility of coronary flow reserve measurement for nonexperts or in very difficult patients (Fig. 6.8). The downside of color Doppler contrast enhancement is that PW Doppler tracing technical quality may degrade.
Fig. 6.8 The appearance of four-chamber, two-chamber, and three-chamber end-systolic frames, both at rest (mid) and stress (right) phases, when using low-mechanical index real-time imaging in conjunction with contrast. The same setting is used for myocardial perfusion imaging, as shown in Fig. 6.9, with the addition of flash-replenishment sequences to assess myocardial replenishment after microbubble-destructive impulses
-
(c)
Assessment of myocardial perfusion (Fig. 6.9) which, although technically demanding and adequate for most but not all 17 segments of the left ventricle, boosts sensitivity very significantly to diagnose coronary artery disease in all coronary territories, although with a minor loss in specificity, compared with isolated.
Fig. 6.9 Stress phase in a patient who underwent contrast dipyridamole echocardiography (0.84 mg/kg/6 min). The upper part of figure shows four-chamber contrast flash-replenishment sequence (from left to right), which demonstrates black areas in the subendocardial region of the true apex and apical–septal, apical, mid, and basal lateral segments (arrows) up to four cycles after microbubble destruction, representing perfusion defects. Lower part shows the three-chamber view (contrast flash-replenishment sequence from left to right), similarly demonstrating the perfusion defect (arrows), in this case almost transmural, in the inferolateral segments. Angiogram on the left side of the figure shows left main disease (50–60 % stenosis, arrow) and LAD disease (arrow), while the angiogram on the right shows the very severe stenosis of the left circumflex artery (arrow), which in fact caused a more profound reduction in myocardial blood flow, with inferolateral transmural perfusion defect. Myocardial perfusion defects may underscore the presence of “balanced disease” in which regional differences in wall motion may often be absent or difficult to detect, at any severity of coronary artery disease (mild or severe); subendocardial stress perfusion defects in several territories are apparent in these cases, due to epicardial/endocardial “vertical” steal phenomenon, although the horizontal would mostly go undetected
-
(d)
Assessment of wall motion [14–16, 48]; myocardial perfusion also demonstrates incremental accuracy for prognostication [44, 45].
The microbubbles that constitute contrast agents are biologically inert and safe: they remain entirely within the vascular space and have an intravascular rheology that is similar to that of erythrocytes [49–52]. An important aspect is that all ultrasound contrast agents are pure intravascular tracers, which is almost unique among commonly used tracers in cardiac imaging (see Chap. 24). The key technical advance was online signal processing of ultrasound signal from insonified microbubbles, which made it possible to separate bubble signals (nonlinear) from myocardial tissue backscatter (linear), with no need for time-consuming offline processing [53]. With the use of signal processing/filtering techniques, the nonlinear signals (non-multiple frequencies or amplitudes) produced by microbubbles can be selectively amplified, while the linear signals from myocardial tissue can be filtered out by cancellation pulse sequences; this results in a prevalent visualization of returning signals from the microbubbles. Ultrasound imaging hardware/software that selectively receives the nonlinear responses produces a much better signal-to-noise ratio and more sensitive detection of microbubbles than would occur using conventional imaging software. The major hurdles for clinical use of myocardial contrast echocardiography are regulatory, financial, and technical. No agent has received FDA approval. There is lack of reimbursement in most settings. The technique is still a bit too complex and misses clinical cutoffs easy to handle for busy physicians. These limitations may explain why the technique is not yet routinely employed in most stress echo laboratories despite extensive scientific evidence [54].
References
Picano E (1992) Stress echocardiography. From pathophysiological toy to diagnostic tool. Circulation 85:1604–1612
Ross J Jr (1991) Myocardial perfusion-contraction matching. Implications for coronary heart disease and hibernation. Circulation 83:1076–1083
Arnese M, Fioretti PM, Cornel JH et al (1994) Akinesis becoming dyskinesis during high-dose dobutamine stress echocardiography: a marker of myocardial ischemia or a mechanical phenomenon? Am J Cardiol 73:896–899
Chen C, Li L, Chen LL et al (1995) Incremental doses of dobutamine induce a biphasic response in dysfunctional left ventricular regions subtending coronary stenoses. Circulation 92:756–766
Gibbons RJ, Chatterjee K, Daley J et al (1999) ACC/AHA/ACP-ASIM guidelines for the management of patients with chronic stable angina: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Management of Patients With Chronic Stable Angina). J Am Coll Cardiol 33:2092–2197
Sheikh KH, Bengtson JR, Helmy S et al (1990) Relation of quantitative coronary lesion measurements to the development of exercise-induced ischemia assessed by exercise echocardiography. J Am Coll Cardiol 15:1043–1051
Picano E, Parodi O, Lattanzi F et al (1994) Assessment of anatomic and physiological severity of single-vessel coronary artery lesions by dipyridamole echocardiography. Comparison with positron emission tomography and quantitative arteriography. Circulation 89:753–761
Cortigiani L, Picano E, Landi P et al (1998) Value of pharmacologic stress echocardiography in risk stratification of patients with single-vessel disease: a report from the Echo-Persantine and Echo-Dobutamine International Cooperative Studies. J Am Coll Cardiol 32:69–74
Lattanzi F, Picano E, Bolognese L et al (1991) Inhibition of dipyridamole-induced ischemia by antianginal therapy in humans. Correlation with exercise electrocardiography. Circulation 83:1256–1262
Ferrara N, Longobardi G, Nicolino A et al (1992) Effect of beta-adrenoceptor blockade on dipyridamole-induced myocardial asynergies in coronary artery disease. Am J Cardiol 70:724–727
Dodi C, Pingitore A, Sicari R et al (1997) Effects of antianginal therapy with a calcium antagonist and nitrates on dobutamine-atropine stress echocardiography. Comparison with exercise electrocardiography. Eur Heart J 18:242–247
San Roman JA, Vilacosta I, Castillo JA et al (1996) Dipyridamole and dobutamine-atropine stress echocardiography in the diagnosis of coronary artery disease. Comparison with exercise stress test, analysis of agreement, and impact of antianginal treatment. Chest 110:1248–1254
Nagel E, Lehmkuhl HB, Bocksch W et al (1999) Noninvasive diagnosis of ischemia-induced wall motion abnormalities with the use of high-dose dobutamine stress MRI: comparison with dobutamine stress echocardiography. Circulation 99:763–770
Thomas D, Xie F, Smith LM, O'Leary E et al (2012) Prospective randomized comparison of conventional stress echocardiography and real-time perfusion stress echocardiography in detecting significant coronary artery disease. J Am Soc Echocardiogr 25:1207–1214
Gaibazzi N, Rigo F, Reverberi C (2010) Detection of coronary artery disease by combined assessment of wall motion, myocardial perfusion and coronary flow reserve: a multiparametric contrast stress-echocardiography study. J Am Soc Echocardiogr 23:1242–1250
Elhendy A, O'Leary EL, Xie F, McGrain AC, Anderson JR, Porter TR (2004) Comparative accuracy of real-time myocardial contrast perfusion imaging and wall motion analysis during dobutamine stress echocardiography for the diagnosis of coronary artery disease. J Am Coll Cardiol 44:2185–2191
Specchia G, de Servi S, Falcone C et al (1981) Significance of exercise-induced ST-segment elevation in patients without myocardial infarction. Circulation 63:46–53
Kawano H, Fuji H (1995) Induction of coronary spasm during dobutamine stress echocardiography. Circulation 92:1–89
Varga A, Cortigiani L, Rossi PC et al (1999) Coronary vasospasm as a source of false positive results during dobutamine echocardiography. Cardiologia 44:907–912
Picano E, Lattanzi F, Masini M et al (1988) Aminophylline termination of dipyridamole stress as a trigger of coronary vasospasm in variant angina. Am J Cardiol 62:694–697
Spes CH, Mudra H, Schnaack SD et al (1996) Dobutamine stress echocardiography for noninvasive diagnosis of cardiac allograft vasculopathy: a comparison with angiography and intravascular ultrasound. Am J Cardiol 78:168–174
Franchini M, Traversi E, Cannizzaro G et al (2000) Dobutamine stress echocardiography and thallium-201 SPECT for detecting ischaemic dilated cardiomyopathy in patients with heart failure. Eur J Echocardiogr 1:109–115
Bach DS, Muller DW, Gros BJ et al (1994) False positive dobutamine stress echocardiograms: characterization of clinical, echocardiographic and angiographic findings. J Am Coll Cardiol 24:928–933
Baroni M, Maffei S, Terrazzi M et al (1996) Mechanisms of regional ischaemic changes during dipyridamole echocardiography in patients with severe aortic valve stenosis and normal coronary arteries. Heart 75:492–497
Picano E, Palinkas A, Amyot R (2001) Diagnosis of myocardial ischemia in hypertensive patients. J Hypertens 19:1177–1183
Rajappan K, Rimoldi OE, Dutka DP et al (2002) Mechanisms of coronary microcirculatory dysfunction in patients with aortic stenosis and angiographically normal coronary arteries. Circulation 105:470–476
Ha JW, Juracan EM, Mahoney DW et al (2002) Hypertensive response to exercise: a potential cause for new wall motion abnormality in the absence of coronary artery disease. J Am Coll Cardiol 39:323–327
Beker B, Vered Z, Bloom NV et al (1994) Decreased thickening of normal myocardium with transient increased wall thickness during stress echocardiography with atrial pacing. J Am Soc Echocardiogr 7:381–387
Hirshleifer J, Crawford M, O’Rourke RA et al (1975) Influence of acute alterations in heart rate and systemic arterial pressure on echocardiographic measures of left ventricular performance in normal human subjects. Circulation 52:835–841
Borges AC, Pingitore A, Cordovil A et al (1995) Heterogeneity of left ventricular regional wall thickening following dobutamine infusion in normal human subjects. Eur Heart J 16:1726–1730
Carstensen S, Ali SM, Stensgaard-Hansen FV et al (1995) Dobutamine-atropine stress echocardiography in asymptomatic healthy individuals. The relativity of stress-induced hyperkinesia. Circulation 92:3453–3463
Abdelmoneim SS, Mankad SV, Bernier M et al (2009) (2009) Microvascular function in Takotsubo cardiomyopathy with contrast echocardiography: prospective evaluation and review of literature. J Am Soc Echocardiogr 22:1249–1255
Sicari R, Palinkas A, Pasanisi E et al (2005) Long-term survival of patients with chest pain syndrome and angiographically normal or near-normal coronary arteries: the additional prognostic value of dipyridamole echocardiography test (DET). Eur Heart J 26:2136–2141
Harrison MR, Smith MD, Friedman BJ et al (1987) Uses and limitations of exercise Doppler echocardiography in the diagnosis of ischemic heart disease. J Am Coll Cardiol 10:809–817
Agati L, Arata L, Neja CP et al (1990) Usefulness of the dipyridamole-Doppler test for diagnosis of coronary artery disease. Am J Cardiol 65:829–834
Olson CE, Porter TR, Deligonul U et al (1994) Left ventricular volume changes during dobutamine stress echocardiography identify patients with more extensive coronary artery disease. J Am Coll Cardiol 24:1268–1273
Zachariah ZP, Hsiung MC, Nanda NC et al (1987) Color Doppler assessment of mitral regurgitation induced by supine exercise in patients with coronary artery disease. Am J Cardiol 59:1266–1270
Pierard LA, Lancellotti P (2006) Dyspnea and stress testing. N Engl J Med 354:871–873
Picano E, Frassi F, Agricola E et al (2006) Ultrasound lung comets: a clinically useful sign of extravascular lung water. J Am Soc Echocardiogr 19:356–363
Agricola E, Picano E, Oppizzi M et al (2006) Assessment of stress-induced pulmonary interstitial edema by chest ultrasound during exercise echocardiography and its correlation with left ventricular function. J Am Soc Echocardiogr 19:457–463
Ristow B, Ali S, Ren X, Whooley MA, Schiller NB (2007) Elevated pulmonary artery pressure by Doppler echocardiography predicts hospitalization for heart failure and mortality in ambulatory stable coronary artery disease: the Heart and Soul Study. J Am Coll Cardiol 49:43–49
Sicari R, Nihoyannopoulos P, Evangelista A et al (2008) Stress echocardiography expert consensus statement: European Association of Echocardiography (EAE) (a registered branch of the ESC). Eur J Echocardiogr 9:415–437
Zoghbi GJ, Dorfman TA, Iskandrian AE (2008) The effects of medications on myocardial perfusion. J Am Coll Cardiol 52:401–416
Gaibazzi N, Reverberi C, Lorenzoni V, Molinaro V, Porter TR (2011) Prognostic value of high dose dipyridamole stress myocardial contrast perfusion echocardiography. Circulation 126:1182–1184
Tsutsui JM, Elhendy A, Anderson JR et al (2005) Prognostic value of dobutamine stress myocardial contrast perfusion echocardiography. Circulation 112:1444–1450
Rigo F, Sicari R, Gherardi S et al (2008) The additive prognostic value of wall motion abnormalities and coronary flow reserve during dipyridamole stress echo. Eur Heart J 29:79–88
Hoffmann R, von Bardeleben S, Kasprzak JD et al (2006) Analysis of regional left ventricular function by cineventriculography, cardiac magnetic resonance imaging, and unenhanced and contrast-enhanced echocardiography: a multicenter comparison of methods. J Am Coll Cardiol 47:121–128
Moir S, Shaw L, Haluska B et al (2007) Left ventricular opacification for the diagnosis of coronary artery disease with stress echocardiography: an angiographic study of incremental benefit and cost-effectiveness. Am Heart J 154:510–518
Skyba DM, Camarano G, Goodman NC et al (1996) Hemodynamic characteristics, myocardial kinetics, and microvascular rheology of FS-069, a second-generation echocardiographic contrast agent capable of producing myocardial opacification from a venous injection. J Am Coll Cardiol 28:1292–1300
Lindner JR, Firschke C, Wei K et al (1998) Myocardial perfusion characteristics and hemodynamic profile of MRX-115, a venous echocardiographic contrast agent, during acute myocardial infarction. J Am Soc Echocardiogr 11:36–46
Jayaweera AR, Edwards N, Glasheen WP et al (1994) In-vivo myocardial kinetics of air-filled albumin microbubbles during myocardial contrast echocardiography: comparison with radiolabeled red blood cells. Circ Res 74:1157–1165
Wei K, Skyba DM, Firschke C et al (1997) Interaction between microbubbles and ultrasound: in vitro and in vivo observations. J Am Coll Cardiol 29:1081–1088
Kaul S (2002) Instrumentation for contrast echocardiography: technology and techniques. Am J Cardiol 90:8J–14J
Pathan F, Marwick TH (2015) Myocardial perfusion imaging using contrast echocardiography. Prog Cardiovasc Dis 57:632–643
Author information
Authors and Affiliations
Corresponding author
Table of Contents Video Companion
Table of Contents Video Companion
-
See stress echo primer, case 6 (intracoronary contrast stress echo).
-
See also in section “Illustrative cases: Case numbers 26, 27, and 28” (by Nicola Gaibazzi, MD, Parma, Italy).
-
Springer Extra Materials available at http://extras.springer.com/2015/978-3-319-20957-9
Rights and permissions
Copyright information
© 2015 Springer International Publishing
About this chapter
Cite this chapter
Gaibazzi, N., Picano, E. (2015). Echocardiographic Signs of Ischemia. In: Stress Echocardiography. Springer, Cham. https://doi.org/10.1007/978-3-319-20958-6_6
Download citation
DOI: https://doi.org/10.1007/978-3-319-20958-6_6
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-20957-9
Online ISBN: 978-3-319-20958-6
eBook Packages: MedicineMedicine (R0)