Abstract
The principle of stress under controlled conditions derives from the Industrial Revolution: metallic materials undergo endurance tests to identify the breaking load. This approach identifies structural defects, which – although occult in the resting or static state – might show up under real-life loading conditions, leading to a dysfunction of the industrial product. In the same way, a patient with normal findings at rest undergoes a stress test to identify any potential vulnerability of the myocardium to ischemia, if there is clinical suspicion of ischemic heart disease.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Fractional Flow Reserve
- Coronary Flow Reserve
- Coronary Stenosis
- Stress Echocardiography
- Vulnerable Plaque
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
The principle of stress under controlled conditions derives from the Industrial Revolution: metallic materials undergo endurance tests to identify the breaking load. This approach identifies structural defects, which – although occult in the resting or static state – might show up under real-life loading conditions, leading to a dysfunction of the industrial product. In the same way, a patient with normal findings at rest undergoes a stress test to identify any potential vulnerability of the myocardium to ischemia, if there is clinical suspicion of ischemic heart disease.
1 Pathways of Ischemia
Myocardial ischemia is the final common pathway of various morphological and functional substrates. In order to describe the pathways of ischemia, the normal heart can be conveniently schematized into its three fundamental anatomical components, each a potential target of pathological conditions leading to ischemia: epicardial coronary arteries, myocardium, and small coronary vessels (Fig. 2.1).
The pathways of ischemia. Upper panel: The fundamental anatomical components of the normal heart are shown: epicardial coronary arteries (parallel lines), myocardium (square box), and small vessels (circles). Lower panel: The three main pathophysiological conditions that may provoke myocardial ischemia. Left to right: coronary stenosis (either fixed or dynamic), myocardial hypertrophy, and small vessel disease (Redrawn and modified from Marcus [2])
2 Epicardial Coronary Arteries
The alterations of epicardial coronary arteries can be either fixed or dynamic. Fixed epicardial artery stenosis is the target of functional stress testing, but we also know from pathology studies that the degree and number of coronary artery stenoses do not predict onset, course, complications, infarct size, or death in ischemic heart disease [1].
3 Fixed Stenosis
The human body incorporates a functional reserve that allows it to cope with the physiological emergencies and dangers of pathological states. By exploiting its functional reserve, each organ can – for a certain amount of time – play a role that is much more demanding than the usual one, or when a pathological process develops, it can maintain normal function in resting conditions. Coronary circulation is no exception to this rule. Coronary reserve is the ability of the coronary arteriolar bed to dilate in response to increased cardiac metabolic demands [2]. It is fully exhausted when maximal vasodilation is reached, corresponding to about four times the resting coronary blood flow in the normal subject (Fig. 2.2). A fixed atherosclerotic stenosis reduces the coronary reserve in a predictable way according to the curve described in Fig. 2.2 [3]. In this curve, four separate segments can be identified: (a) the hemodynamically silent zone, where stenoses ranging from 0 to 40 % do not affect the coronary flow reserve (CFR) to any detectable extent; (b) the clinically silent zone, where stenoses ranging from 40 to 70 % reduce the flow reserve without reaching the critical threshold required to provoke ischemia with the usual stresses; (c) the zone potentially capable of inducing ischemia, where stenoses exceeding the critical level of 70 % elicit myocardial ischemia when stress is applied, but not in resting conditions; and (d) the zone provoking ischemia at rest, where tight stenoses (>90 %) completely abolish the flow reserve and may critically reduce coronary blood flow even in resting conditions.
Coronary blood flow curve (on the ordinate) for increasing levels of coronary stenosis (on the abscissa) experimentally obtained in resting conditions (lower curve) and at maximal postischemic vasodilation (upper curve). Coronary reserve – i.e., the capacity of the coronary circulation to dilate following increased myocardial metabolic demands – is expressed as the difference between hyperemic flow and the resting flow curve. The dashed area between the two curves identifies a critical value of coronary stenosis (70 %) beyond which the flow reduction is so severe as to make the myocardium vulnerable to ischemia in the presence of increased oxygen consumption (Modified from Gould and Lipscomb [3])
4 Dynamic Stenosis
From a theoretical point of view, dynamic stenoses may be the consequence of three different conditions: increased tone at the level of an eccentric coronary plaque, complete vasospasm caused by local hyperreactivity of the coronary smooth muscle cells, or intravascular thrombosis. The first mechanism can significantly modulate the anginal threshold in patients with chronic stable angina [4], while vasospasm is responsible for variant angina. All three mechanisms coexist in unstable angina [5]. The biochemical mechanisms of coronary vasoconstriction remain somewhat elusive; however, we know that coronary vasoconstriction can be superimposed on any degree of anatomical stenosis and that functional and organic (fixed and dynamic) stenoses can be associated to a variable extent over time, transiently lowering exercise tolerance in the individual patient (Fig. 2.3). Organic stenosis determines the fixed ceiling of flow reserve which cannot be exceeded without eliciting ischemia, whereas dynamic stenosis can modulate exercise capacity in a given patient in a transient, reversible, and unpredictable way [4].
In the presence of a fixed hemodynamically significant stenosis, there is a pathologically reduced “ceiling” of flow reserve (continuous transverse line) which induces ischemia when myocardial oxygen demand exceeds a definite threshold (upper panel). In the presence of a dynamic stenosis (lower panel), the effort tolerance is modulated – in an intermittent, unpredictable way – by fluctuations in coronary tone (dashed line), which may reduce the oxygen supply even in the presence of a normal organic ceiling of flow reserve (Modified from Maseri [4])
5 Myocardium and Small Coronary Vessels
Even in the presence of normal epicardial arteries, myocardial hypertrophy can lower coronary reserve through several mechanisms: vascular growth that is inadequate with respect to myocardial growth, a reduction of the cross-sectional area of resistance of a vessel caused by vascular hypertrophy, and compression of intramural coronary vessels by increased extravascular resistance [2]. Furthermore, hypertrophy determines increased oxygen consumption in resting conditions; the resting flow curve shifts upward with a consequent reduction in coronary reserve (Fig. 2.2). Due to myocardial hypertrophy, as well as accompanying small vessel disease, coronary reserve may also be reduced in both dilated and hypertrophic cardiomyopathy. With normal epicardial coronary arteries and myocardial mass, coronary reserve can still be reduced following increased resistance at the level of the small prearteriolar vessels, which are too small to be imaged by coronary angiography [6].
Small vessel disease can be either primary (as in syndrome X) or secondary (as in arterial hypertension [2]). The decreased flow reserve may be related to a functional and/or an organic factor of the coronary microcirculation. In the former situation, one must assume the inability of the microcirculation to vasodilate appropriately, due to errors in the decoding or transmission of the myocardial metabolic message. In the latter case, anatomical reduction of the microvascular cross-sectional area is likely to occur for medial hyperplasia, which determines an increased wall-to-lumen ratio (Fig. 2.1). This anatomical phenomenon may also determine hyperreactivity to functional stimuli for purely geometric reasons, since minimal caliber reductions cause a marked increase in resistance, with a consequently exaggerated response to normal vasoconstrictive stimuli.
6 The Target of Ischemia: The Subendocardial Layer
The many functional and anatomical pathways of ischemia share a common pathophysiological mechanism: the reduction of coronary reserve. This makes the myocardium vulnerable to ischemia during stress. Regardless of the stress employed and the morphological substrate, ischemia tends to propagate centrifugally with respect to the ventricular cavity [7, 8]: it involves the subendocardial layer, whereas the subepicardial layer is affected only at a later stage if the ischemia persists (Fig. 2.4).
Distribution of flow in the subendocardial and subepicardial layers under different hemodynamic conditions. Upper left panel: In resting conditions, the subendocardial and subepicardial flows overlap. Upper right panel: During stress, the flow increases homogeneously in both layers without affecting the transmural distribution. In the presence of a coronary stenosis, the resting flow is similar to that under normal conditions (upper left panel); however, during stress (lower left panel), flow remains elevated in the subepicardial layer but falls precipitously in the subendocardium, within the region supplied by the stenotic artery. In the presence of a severe stenosis (lower right panel), stress provokes a fall in the subendocardial as well as the subepicardial layer, therefore determining a transmural ischemia (Redrawn and modified from L’Abbate et al. [7])
In fact, extravascular pressure is higher in the subendocardial than in the subepicardial layer; this provokes a higher metabolic demand (wall tension being among the main determinants of myocardial oxygen consumption) and an increased resistance to flow. Selective stress-induced hypoperfusion is especially important for stress echocardiography applications, since regional systolic thickening is linearly and closely related to subendocardial perfusion and only loosely related to subepicardial perfusion [8, 9] (Fig. 2.5).
The relationship between regional blood flow and systolic wall thickening in resting conscious dogs subjected to various degrees of circumflex coronary artery stenosis. Flow is expressed as a decimal fraction of that in a normal region of the ventricle, and percentage wall thickening (%WTh) is expressed as a fraction of the resting value prior to coronary stenosis. (a) Subendocardial blood flow vs. wall thickening, showing a nearly linear relationship (solid line). (b) Subepicardial blood flow vs. wall thickening, showing considerable scatter and no change in subepicardial flow until function is reduced by more than 50 % (Modified from Gallagher et al. [9])
7 The Pitfalls of Coronary Anatomy Diagnostic “Gold Standard”
The results of noninvasive diagnostic tests (Table 2.1) are usually compared with a “gold standard,” that is, angiographically assessed coronary artery disease. Although generally accepted, the gold standard has some limitations of both a theoretical and a practical nature [10].
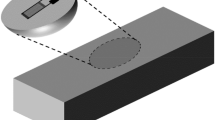
First, coronary stenosis is estimated by angiography through the visually assessed percentage reduction of the vessel lumen. The percent of stenosis is a reliable index of severity only if the vascular segment immediately proximal and distal to the stenotic segment is normal and the lesion concentric and symmetrical. Both assumptions are valid in only a very limited number of cases: atherosclerotic involvement usually extends beyond the point of maximum lumen reduction, and the most frequent type of lesion is eccentric. Second, coronary angiography represents only the vessel lumen, an innocent bystander of atherosclerotic disease, rather than the vessel wall, which is the real victim. Minimal, “nonsignificant” lesions at angiography can harbor a diffuse severe atherosclerotic process [2]. The close correlation between coronary stenosis and CFR found in the experimental animal [3] is replaced in the clinical setting by an impressive scatter of data [11]. It is impossible to predict the physiological meaning of a stenosis solely on the basis of its angiographic appearance – unless selected patients with single vessel disease, no previous myocardial infarction, no collateral circulation, and no left ventricular hypertrophy are enrolled [12]. Coronary stenosis provokes ischemia as a result of hemodynamic consequences on the coronary reserve; however, the two parameters (anatomical and pathophysiological) can diverge, and the individual values of CFR vary substantially for stenoses of intermediate (40–80 %) angiographic severity. In these patients, positive stress test results are more frequently found in patients with depressed CFR (<2.0) than in patients with preserved CFR (>2.0). This is true for all forms of stress testing, including exercise electrocardiography [13–17], stress perfusion scintigraphy [18–21], and stress echocardiography [22–24]. Third, coronary angiography evaluates the anatomical component of myocardial ischemia, while stress tests can induce ischemia through mechanisms that are totally different from the organic stenosis (such as dynamic vasoconstriction) and cannot be assessed by means of a purely morphological, static evaluation of the coronary tree [25]. Extracoronary factors such as myocardial hypertrophy can also reduce CFR and therefore make the myocardium potentially vulnerable to ischemia during stress tests [26, 27]. Finally, the commonly employed visual and subjective assessment of stenosis is burdened by a marked intra- and interobserver variability, even among experienced angiographers, and arbitrary threshold criteria (such as the presence of a 50 % diameter stenosis in at least one major coronary vessel) are introduced to distinguish between “normal” and “sick” patients, when in fact the severity of the atherosclerotic disease ranges over a continuous spectrum. Anatomical coronary artery disease can be assessed much more accurately by intracoronary ultrasound (Fig. 2.6), which substantially improves the representation of atherosclerosis compared with coronary angiography [28]. However, intracoronary ultrasound knows nothing about perfusion territory, which is critical for functional evaluation of coronary stenosis. Functional significance of coronary stenosis cannot be predicted by any intracoronary imaging modality for anatomical assessment of coronary stenosis.
Invasive diagnostic tests for the detection of coronary artery disease. Invasive tests include the luminogram of coronary angiography and the direct visualization of the coronary arterial wall by intracoronary ultrasound (ICUS). The percentage of a stenosis can be expressed in angiographic studies as a percentage reduction in diameter and as a percentage reduction in cross-sectional area. The percentage reduction is greater for area than for diameter because of the quadratic relationship between the diameter (2r) and area (πr 2) of a circle. The two estimates of stenosis correspond perfectly only for zero stenosis and for 100 % stenosis. For each level of stenosis severity, the CFR is expressed with a Doppler tracing before and after a coronary vasodilator (adenosine or dipyridamole). Stenoses of less than 50 % diameter reduction are not hyperemic flow limiting (Redrawn and modified from Erbel [29])
This improvement is comparable to that achieved in left ventricular imaging when moving from chest X-ray to transthoracic echocardiography. Chest X-ray outlines external profiles and provides a rough index of cardiac volumes, whereas transthoracic echocardiography describes tomographically the various heart chambers and the thickness of the walls and identifies within each segment the different layers (endocardium, myocardium, and pericardium). In a similar fashion, coronary angiography offers only a luminogram of the vessel, whereas intracoronary ultrasound imaging provides an assessment of the lumen and of the vessel wall thickness [29]. In addition, at each site, the different layers (intima, media, and adventitia) can also be evaluated. Angiography and intracoronary ultrasound correlate closely in healthy vessels with a nearly circular lumen shape. However, as the lumen becomes progressively more irregular, the correlation between a silhouette imaging method (angiography) and a tomographic modality (ultrasound) diverges significantly. The most substantial disagreement is found in status after angioplasty in which angiography cannot accurately depict the true size of the complex and distorted luminal shape commonly encountered after interventions. Abnormal stress test results can be found in patients with nonsignificant coronary angiographic findings in whom intracoronary sonography may show angiographically unrecognized atherosclerotic changes [30], as typically happens in cardiac allograft vasculopathy [31]. Invasive angiographic gold standards are the obligatory reference for noninvasive stress testing procedures, but not all that glitters is gold [32]. In several conditions, coronary arteries are perfectly smooth, even with intracoronary ultrasound, and the CFR is impaired by transthoracic stress echocardiography, for instance, in aortic stenosis, syndrome X, or dilated cardiomyopathy [33] (Fig. 2.7).
The spectrum of clinical conditions with normal coronary arteries and reduced CFR on the left anterior descending artery by transthoracic vasodilatory stress echocardiography (Redrawn and modified from Rigo [33]). CAD coronary artery disease, CFR coronary flow reserve, HCM hypertrophic cardiomyopathy, IDC idiopathic dilated cardiomyopathy
A “false-positive” result by anatomic criteria (i.e., a reduced CFR with angiographically normal coronary arteries) can become a “true-positive” prognostic response in the long run, and patients with reduced CFR – assessed by complex techniques such as positron emission tomography or simple methods such as transthoracic vasodilatory stress echocardiography – are more likely to experience adverse events in a variety of clinical conditions such as chest pain with normal coronary arteries [34], dilated cardiomyopathy [35, 36], and hypertrophic cardiomyopathy [37, 38].
8 Assessment of Functional Severity of Coronary Lesions
Since coronary angiography is of limited value in defining the functional significance of stenosis, we need to integrate the anatomic information with a functional assessment, either by measuring CFR or intracoronary artery pressure with fractional flow reserve (FFR). CFR measurements depend on the status of the microcirculation, as well as on the severity of the lesion in the epicardial vessel. For practical and methodological reasons, measurement of CFR is not widely used in catheterization laboratories today and hence does not play any role in the patient management in the catheterization lab. The opposite is true in the stress echo lab, where FFR cannot be obtained and decision-making is founded on CFR assessment, obtained during vasodilator stress with Doppler imaging of left anterior descending coronary artery flow or – less frequently – with myocardial contrast echocardiography. FFR is considered nowadays to be the “gold standard” for invasive assessment of stenosis physiologic significance and a helpful tool for decision-making in coronary revascularization. FFR is calculated as the ratio of distal coronary pressure to aortic pressure measured during maximal hyperemia. A normal value for FFR is 1.0, regardless of the status of the microcirculation, and stenoses with an FFR >0.80 are hardly ever associated with exercise-induced ischemia. It provides guidance for the clinician in situations when it is not clear whether a lesion of intermediate angiographic severity causes ischemia, and the use of FFR was upgraded to a Class IA classification in multivessel percutaneous coronary intervention in the European Society of Cardiology guidelines on coronary revascularization [39]. In general, the relation between FFR and angiographic assessment of coronary stenosis is mild to moderate with approximately 1/3 of coronary stenosis either over- or underestimated by angiography. On an individual level, this means that a patient with multivessel disease would have every third coronary stenosis misdiagnosed, with a possible wrong choice for revascularization procedure. It has been shown in the FAME trial [40, 41] that the rate of functional significant stenosis in two-vessel angiography stenosis is 43 % and in angiographically three-vessel coronary artery disease only 14 %. So, not only is there a significant mismatch in angiographic and functional assessment of coronary stenosis, but it seems that we are sometimes functionally blinded with the more severe angiographic appearance of diffuse coronary atherosclerosis.
The assessment of CFR with stress echo can be done upstream to the cath lab – which in practice is often a point of no return toward revascularization; it does not imply the additional cost (about 1000 dollars) [42] and the extra radiation exposure (about 5 milliSievert, corresponding to 250 chest X-rays, in addition to the 7 of a coronary angiography) of FFR performed in the cath lab [43] and provides insight into the functional status of coronary microcirculation, which is a major prognostic determinant independently of coronary stenosis [44]. The randomized trials such as FAME 1 [40] and FAME 2 [41] supporting the evidence-based use of FFR to guide revascularization are conspicuously lacking for CFR. Albeit conceptually different and performed in different operational theaters by different subspecialists (Table 2.2), both methods are useful for gaining insight into the key variable of physiologic assessment of coronary stenosis in the clinical arena [45]. The other emerging point is that concordance between FFR and CFR is not ideal, i.e., in more than 25 % of patients, FFR and CFR do not point in the same diagnostic direction [45]. Where positive CFR and negative FFR are indicative for microvascular disease, positive FFR but negative CFR is both a pathophysiological and a prognostic challenge. Recently, it has been shown that negative CFR carries excellent prognosis even in the presence of positive FFR [46]. So, a combination of FFR and noninvasive or invasive CFR seems to be the mastermind algorithm in current diagnostic workup of the patient.
At present, FFR is recommended as definitely beneficial when noninvasive stress imaging is contraindicated, discordant, nondiagnostic, or unavailable in stable ischemic heart disease. In these conditions, FFR should be used to assess the functional significance of intermediate coronary stenosis (50–70 %) and more severe stenoses (<90 %) [47].
9 Beyond Ischemia and Stenosis: Cardiac Calcification and Plaque Vulnerability
The risk stratification strategies centered on functional stress testing and coronary angiography are practical and effective, yet they recognize a blind spot since clinical complications may depend on plaque composition, not only on plaque size. This blind spot can be at least in part enlightened with an integrated approach also considering cardiac calcification by transthoracic resting echocardiography and identification of the pre-intrusive atherosclerosis and pre-obstructive vulnerable plaque by vascular duplex scan of the carotid artery.
The main purpose of calcium screening is not to identify patients with obstructive coronary artery disease but to detect vessel wall atherosclerosis at a pre-obstructive stage. This information is usually obtained with the Agatston coronary calcification score with CCTA (see Chap. 39) but can also be obtained with a convenient proxy of coronary calcification such as cardiac calcification with baseline echocardiography (Fig. 2.8). A semiquantitative cardiac calcium score index can be derived from a simple assessment of calcification in mitral annulus, aortic root wall, and aortic leaflets and correlates nicely with coronary calcification evaluated with Agatston score and Framingham score, providing additive prognostic information compared to stress echo [48, 49].
A simple assessment of cardiac calcification through scoring of mitral annulus calcification (upper panel a, from 0 = no calcium, to 3 = extensive calcification), aortic root (lower panel b, from 0 = absent, to 1 =, present), and aortic valve leaflets (from 0 = no calcium, to 3 = calcification of all three leaflets) calcification (Modified from Corciu et al. [49]). MAC mitral annulus calcification, ARS aortic root sclerosis, AVS aortic valve sclerosis
A similar assessment of pre-obstructive atherosclerosis is obtained with carotid intima-media assessment, which if increased predicts subsequent events in asymptomatic subjects [50, 51]. Albeit conceptually different and performed in different operational theaters by different subspecialists (Table 2.3), both echo and CCTA are useful for gaining insight into the variable of assessment of inappropriate coronary and cardiovascular calcification and – with intima-media thickness – of prognostically meaningful pre-intrusive atherosclerosis in the clinical arena [52].
Identification of the vulnerable plaque is even more important. Vulnerable plaques are prone to rupture, and their rupture can trigger unfavorable pathology events such as distal embolism, thrombosis, and plaque progression mirrored in clinical events such as (in coronary arteries) unstable angina, myocardial infarction and death, and (in carotid arteries) transient ischemic attacks and stroke [53]. At histology, the vulnerable plaques are rich in lipids and hemorrhages and poor in fibrosis and with thin fibrotic cap and show only spotty calcification and possibly irregular plaque surface border and neovascularization [54]. These histologic features leave ultrasound fingerprints [55–60] and can be recognized by simple visual [61, 62], more objective videodensitometry [63–65] (Fig. 2.9), and quantitative backscatter analysis [66, 67], both noninvasively with duplex scan of the carotid and invasively with virtual histology and radiofrequency-based intracoronary ultrasound. Whatever the method and wherever the district, the ultrasound appearance of the vulnerable plaque can be distinguished from the low-risk stable plaque and identified as a group at higher risk of subsequent cardiovascular events [68–73].
A visual and videodensitometric assessment of carotid plaque morphology. Unstable, soft, lipid-rich plaques are less echogenic and more dishomogeneous than stable, fibrotic plaques. These texture features can also be more objectively described with simple textural analysis with quantitative descriptors of plaque echogenicity such as median gray level or plaque texture such as entropy (lower panels). Stable plaques show higher median gray levels and lower entropy values, related to the spatial disorder of the image (Modified from Mazzone et al. [63])
The carotid unstable plaque is associated with a systemic (not only local) plaque instability, present in different districts (coronary and carotid) and on different sides (both ipsilateral and contralateral to symptomatic side), and is associated with unfavorable events in the follow-up [74, 75]. Hypoechoic or dishomogeneous plaques, with spotty microcalcification and large plaque burden, with plaque neovascularization and surface irregularities by contrast-enhanced ultrasound [76, 77], are more prone to clinical complications than hyperechoic, extensively calcified, homogeneous plaques with limited plaque burden, smooth surface, and absence of neovascularization (Table 2.4). Plaque ultrasound morphology is important, together with plaque geometry, in determining the atherosclerotic prognostic burden in the individual patient. A complex-type plaque coronary morphology at coronary angiography – for any given coronary stenosis – makes the myocardium more susceptible to induced ischemia during SE [78, 79]. With this integrated approach, SE, baseline resting echocardiography for cardiac calcification and carotid scan for intima-media thickness, and plaque geometry and plaque morphology assessment can team up with invasive studies for comprehensive risk stratification of most variables, including those in the blind spot of functional imaging and SE [80].
References
Marzilli M, Merz CN, Boden WE et al (2012) Obstructive coronary atherosclerosis and ischemic heart disease: an elusive link! J Am Coll Cardiol 60:951–956
Marcus ML (1983) The coronary circulation in health and disease. McGraw Hill, New York, pp 65–92
Gould KL, Lipscomb K (1974) Effects of coronary stenoses on coronary flow reserve and resistance. Am J Cardiol 34:48–55
Maseri A (1987) Role of coronary artery spasm in symptomatic and silent myocardial ischemia. J Am Coll Cardiol 9:249–262
Gorlin R, Fuster V, Ambrose JA (1986) Anatomic-physiologic links between acute coronary syndromes. Circulation 74:6–9
Epstein SE, Cannon RO 3rd (1986) Site of increased resistance to coronary flow in patients with angina pectoris and normal epicardial coronary arteries. J Am Coll Cardiol 8:459–461
L’Abbate A, Marzilli M, Ballestra AM et al (1980) Opposite transmural gradients of coronary resistance and extravascular pressure in the working dog’s heart. Cardiovasc Res 14:21–29
Ross J Jr (1989) Mechanisms of regional ischemia and antianginal drug action during exercise. Prog Cardiovasc Dis 31:455–466
Gallagher KP, Matsuzaki M, Koziol JA et al (1984) Regional myocardial perfusion and wall thickening during ischemia in conscious dogs. Am J Physiol 247:H727–H738
Marcus ML, White CW, Kirchner PT (1986) Isn’t it time to reevaluate the sensitivity of noninvasive approaches for the diagnosis of coronary artery disease? J Am Coll Cardiol 8:1033–1034
White CW, Wright CB, Doty DB et al (1984) Does visual interpretation of the coronary arteriogram predict the physiologic importance of a coronary stenosis? N Engl J Med 310:819–824
Uren NG, Melin JA, De Bruyne B et al (1994) Relation between myocardial blood flow and the severity of coronary-artery stenosis. N Engl J Med 330:1782–1788
Legrand V, Mancini GB, Bates ER et al (1986) Comparative study of coronary flow reserve, coronary anatomy and results of radionuclide exercise tests in patients with coronary artery disease. J Am Coll Cardiol 8:1022–1032
Wilson RF, Marcus ML, Christensen BV et al (1991) Accuracy of exercise electrocardiography in detecting physiologically significant coronary arterial lesions. Circulation 83:412–421
De Bruyne B, Bartunek J, Sys SU et al (1995) Relation between myocardial fractional flow reserve calculated from coronary pressure measurements and exercise-induced myocardial ischemia. Circulation 92:39–46
Schulman DS, Lasorda D, Farah T et al (1997) Correlations between coronary flow reserve measured with a Doppler guide wire and treadmill exercise testing. Am Heart J 134:99–104
Piek JJ, Boersma E, Di Mario C et al (2000) Angiographical and Doppler flow-derived parameters for assessment of coronary lesion severity and its relation to the result of exercise electrocardiography. DEBATE study group. Doppler Endpoints Balloon Angioplasty Trial Europe. Eur Heart J 21:466–474
Joye JD, Schulman DS, Lasorda D et al (1994) Intracoronary Doppler guide wire versus stress single-photon emission computed tomographic thallium-201 imaging in assessment of intermediate coronary stenoses. J Am Coll Cardiol 24:940–947
Daimon M, Watanabe H, Yamagishi H et al (2001) Physiologic assessment of coronary artery stenosis by coronary flow reserve measurements with transthoracic Doppler echocardiography: comparison with exercise thallium-201 single photon emission computed tomography. J Am Coll Cardiol 37:1310–1315
Heller LI, Cates C, Popma J et al (1997) Intracoronary Doppler assessment of moderate coronary artery disease: comparison with 201Tl imaging and coronary angiography. FACTS Study Group. Circulation 96:484–490
El-Shafei A, Chiravuri R, Stikovac MM et al (2001) Comparison of relative coronary Doppler flow velocity reserve to stress myocardial perfusion imaging in patients with coronary artery disease. Catheter Cardiovasc Interv 53:193–201
Picano E, Parodi O, Lattanzi F et al (1994) Assessment of anatomic and physiological severity of single-vessel coronary artery lesions by dipyridamole echocardiography. Comparison with positron emission tomography and quantitative arteriography. Circulation 89:753–761
Pijls NH, De Bruyne B, Peels K et al (1996) Measurement of fractional flow reserve to assess the functional severity of coronary-artery stenoses. N Engl J Med 334:1703–1708
Bartunek J, Marwick TH, Rodrigues AC et al (1996) Dobutamine-induced wall motion abnormalities: correlations with myocardial fractional flow reserve and quantitative coronary angiography. J Am Coll Cardiol 27:1429–1436
Bortone AS, Hess OM, Eberli FR et al (1989) Abnormal coronary vasomotion during exercise in patients with normal coronary arteries and reduced coronary flow reserve. Circulation 79:516–527
Scheler S, Motz W, Strauer BE (1992) Transient myocardial ischemia in hypertensives: missing link with left ventricular hypertrophy. Eur Heart J 13(Suppl D):62–65
Motz W, Strauer BE (1996) Improvement of coronary flow reserve after long-term therapy with enalapril. Hypertension 27:1031–1038
Di Mario C, Gorge G, Peters R et al (1998) Clinical application and image interpretation in intracoronary ultrasound. Study Group on Intracoronary Imaging of the Working Group of Coronary Circulation and of the Subgroup on Intravascular Ultrasound of the Working Group of Echocardiography of the European Society of Cardiology. Eur Heart J 19:207–229
Erbel R (1996) The dawn of a new era – non-invasive coronary imaging. Herz 21:75–77
Verna E, Ceriani L, Giovanella L et al (2000) “False-positive” myocardial perfusion scintigraphy findings in patients with angiographically normal coronary arteries: insights from intravascular sonography studies. J Nucl Med 41:1935–1940
Spes CH, Klauss V, Rieber J et al (1999) Functional and morphological findings in heart transplant recipients with a normal coronary angiogram: an analysis by dobutamine stress echocardiography, intracoronary Doppler and intravascular ultrasound. J Heart Lung Transplant 18:391–398
Topol EJ, Nissen SE (1992) Our preoccupation with coronary luminology. The dissociation between clinical and angiographic findings in ischemic heart disease. Circulation 92:2333–2342
Rigo F (2005) Coronary flow reserve in stress-echo lab. From pathophysiologic toy to diagnostic tool. Cardiovasc Ultrasound 3:8
Rigo F, Cortigiani L, Pasanisi E et al (2006) The additional prognostic value of coronary flow reserve on left anterior descending artery in patients with negative stress echo by wall motion criteria. A transthoracic vasodilator stress echocardiography study. Am Heart J 151:124–130
Neglia D, Michelassi C, Trivieri MG et al (2002) Prognostic role of myocardial blood flow impairment in idiopathic left ventricular dysfunction. Circulation 105:186–193
Rigo F, Gherardi S, Galderisi M et al (2006) The prognostic impact of coronary flow-reserve assessed by Doppler echocardiography in non-ischaemic dilated cardiomyopathy. Eur Heart J 27:1319–1323
Cecchi F, Olivotto I, Gistri R et al (2003) Coronary microvascular dysfunction and prognosis in hypertrophic cardiomyopathy. N Engl J Med 349:1027–1035
Cortigiani L, Rigo F, Gherardi S et al (2009) Prognostic implications of coronary flow reserve in hypertrophic cardiomyopathy. A Doppler echocardiographic study. Am J Cardiol 1:36–41
Montalescot G, Sechtem U, Achenbach S et al; Task Force Members (2013) 2013 ESC guidelines on the management of stable coronary artery disease−addenda: the Task Force on the management of stable coronary artery disease of the European Society of Cardiology. Eur Heart J 34:2949–3003
Tonino PA, De Bruyne B, Pijls NH et al; FAME Study Investigators (2009) Fractional flow reserve versus angiography for guiding percutaneous coronary intervention. N Engl J Med 360:213–224
De Bruyne B, Pijls NH, Kalesan B et al; FAME 2 Trial Investigators (2012) Fractional flow reserve-guided PCI versus medical therapy in stable coronary disease. N Engl J Med 367:991–1001
Fearon WF, Bornschein B, Tonino PA et al (2010) Economic evaluation of fractional flow reserve-guided percutaneous coronary intervention in patients with multivessel disease. Circulation 122:2545–2550
Ntalianis A, Trana C, Muller O et al (2010) Effective radiation dose, time, and contrast medium to measure fractional flow reserve. JACC Cardiovasc Interv 3:821–827
Crea F, Camici PG, Bairey Merz CN (2014) Coronary microvascular dysfunction: an update. Eur Heart J 35:1101–1111
Gould KL, Johnson NP, Bateman TM et al (2013) Anatomic versus physiologic assessment of coronary artery disease. Role of coronary flow reserve, fractional flow reserve, and positron emission tomography imaging in revascularization decision-making. J Am Coll Cardiol 62:1639–1653
van de Hoef TP, van Lavieren MA, Damman P et al (2014) (2014). Physiologic basis and long-term clinical outcome of discordance between fractional flow reserve and coronary flow velocity reserve in coronary stenoses of intermediate severity. Circ Cardiovasc Interv 7:301–311
Lotfi A, Jeremias A, Fearon WF et al (2014) Expert consensus statement on the use of fractional flow reserve, intravascular ultrasound, and optical coherence tomography: a consensus statement of the Society of cardiovascular Angiography and Intervention. Catheter Cardiovasc Interv 83:509–518
Gaibazzi N, Sicari R, Agricola E et al (2014) Cardiac calcification of transthoracic echo predicts stress echo results. Int J Cardiol 174:393–395
Corciu AI, Siciliano V, Poggianti E et al (2010) Cardiac calcification by transthoracic echocardiography in patients with known or suspected coronary artery disease. Int J Cardiol 142:288–295
O' Leary DH, Polak JK, Kronmal RA (1999) Carotid intima-media thickness as a risk factor for myocardial infarction and stroke in older adults. Cardiovascular health study collaborative research group. N Engl J Med 340:14–22
Greenland P, Alpert JS, Beller GA et al; American College of Cardiology Foundation; American Heart Association (2010) 2010 ACCF/AHA guideline for assessment of cardiovascular risk in asymptomatic adults: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 56:e50–103
Leipsic J, Abbasa S, Achenbach S et al (2014) SSCT guidelines for the interpretation and reporting of coronary CT angiography: a report of the society of cardiovascular computed tomography guidelines committee. J Cardiovasc Comput Tomogr 8:342–358
Falk E, Shah PK, Fuster V (1995) Coronary plaque disruption. Circulation 92:657–671
Gallino A, Stuber M, Crea F et al (2012) In vivo imaging of atherosclerosis. Atherosclerosis 224:25–36
Picano E, Landini L, Distante A, Sarnelli R, Benassi A, L'Abbate A (1983) Different degrees of atherosclerosis detected by backscattered ultrasound: an in vitro study on fixed human aortic walls. J Clin Ultrasound 11:375–379
Picano E, Landini L, Distante A, Benassi A, Sarnelli R, L'Abbate A (1985) Fibrosis, lipids, and calcium in human atherosclerotic plaque. In vitro differentiation from normal aortic walls by ultrasonic attenuation. Circ Res 56:556–562
Picano E, Landini L, Distante A et al (1985) Angle dependence of ultrasonic backscatter in arterial tissues: a study in vitro. Circulation 72:572–576
Picano E, Landini L, Lattanzi F et al (1986) The use of frequency histograms of ultrasonic backscatter amplitudes for detection of atherosclerosis in vitro. Circulation 74:1093–1098
Picano E, Landini L, Lattanzi F, Salvadori M, Benassi A, L'Abbate A (1988) Time domain echo pattern evaluations from normal and atherosclerotic arterial walls: a study in vitro. Circulation 77:654–659
Wolverson MK, Bashiti HM, Peterson GJ (1983) Ultrasonic tissue characterization of atheromatous plaques using a high resolution real time scanner. Ultrasound Med Biol 9:599–609
Reilly LM, Lusby RY, Hughes L et al (1983) Carotid plaque histology using real time ultrasonography. Clinical and therapeutic implications. Am J Surg 146:188–193
European Carotid Plaque Study Group (1995) Carotid artery composition – relation to clinical presentation and ultrasound B- mode imaging. Eur J Endov Surg 10:23–32
Mazzone AM, Urbani MP, Picano E et al (1995) In vivo ultrasonic parametric imaging of carotid atherosclerotic plaque by videodensitometric technique. Angiology 46:663–672
El-Barghouty NM, Levine T, Ladva S et al (1996) Histological verification of computerized carotid plaque characterization. Eur J Vasc Endovasc Surg 11:414–416
Baroncini LA, Pazin Filho A, Murta Junior LO et al (2006) Ultrasonic tissue characterization of vulnerable carotid plaque: correlation between videodensitometric method and histological exam. Cardiovasc Ultrasound 4:32
Urbani MP, Picano E, Parenti G et al (1993) In vivo radiofrequency-based ultrasonic tissue characterization of the atherosclerotic plaque. Stroke 24:1507–1512
Kawasaki M, Takatsu H, Noda T et al (2001) Noninvasive quantitative tissue characterization and two-dimensional color-coded map of human atherosclerotic lesions using ultrasound integrated backscatter. Comparison between histology and integrated backscatter images before and after death. J Am Coll Cardiol 38:486–492
Gronholdt ML, Nordestgaard BG, Schroeder TV, Vorstrup S, Sillesen H (2001) Ultrasound echolucent carotid plaques predict future strokes. Circulation 104:68–73
Mathiesen EB, B∅onaa KH, Joakimsen O (2001) Echo-lucent plaques Are associated with high risk of ischemic cerebrovascular events in carotid stenosis. Circulation 103:2171–2175
Honda O, Sugiyama S, Kugiyama K et al (2004) Echolucent carotid plaques predict future coronary events in patients with coronary artery disease. J Am Coll Cardiol 43:1177–1184
Biasi GM, Froio AF, Diethrich EB et al (2004) Carotid plaque echolucency increases the risk of stroke in carotid stenting. The Imaging in Carotid Angioplasty and Risk of Stroke (ICAROS) study. Circulation 110:756–762
Petersen C, Pecanha P, Venneri L et al (2006) The impact of carotid plaque presence and morphology on mortality outcome in cardiological patients. Cardiovasc Ultrasound 4:16
Cohen A, Tzourio C, Bertrand B, Chauvel C, Bousser MG, Amarenco P (1997) Aortic plaque morphology and vascular events: a follow-up study in patients with ischemic stroke. FAPS Investigators. French Study of Aortic Plaques in Stroke. Circulation 96:3838–3841
Lombardo A, Biasucci LM, Lanza GA et al (2004) Inflammation as a possible link between coronary and carotid plaque instability. Circulation 109:3158–3163
Ibrahimi P, Jashari F, Johansson E et al (2014) Vulnerable plaques in the contralateral carotid arteries in symptomatic patients: a detailed ultrasonic analysis. Atherosclerosis 235:526–531
Coli A, Magnoni M, Sangiorgi G et al (2008) Contrast-enhanced ultrasound imaging of intraplaque neovascularization in carotid arteries: correlation with histology and plaque echogenicity. J Am Coll Cardiol 52:223–230
Partovi S, Loebe M, Aschnander M et al (2012) Contrast-enhanced ultrasound for assessing carotid atherosclerosis plaque lesions. AJR Am J Roentgenol 198:W13–W19
Lu C, Picano E, Pingitore A et al (1995) Complex coronary artery lesion morphology influences results of stress echocardiography. Circulation 91:1669–1675
Beleslin BD, Ostojic M, Djordjevic-Dikic A et al (1999) Integrated evaluation of relation between coronary lesion features and stress echocardiography results: the importance of coronary lesion morphology. J Am Coll Cardiol 33:717–726
Picano E, Paterni M (2015) Ultrasound tissue characterization of vulnerable atherosclerotic plaque. Int J Mol Sci 16:10121–10133
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Copyright information
© 2015 Springer International Publishing
About this chapter
Cite this chapter
Beleslin, B., Picano, E. (2015). Anatomical and Functional Targets of Stress Testing. In: Stress Echocardiography. Springer, Cham. https://doi.org/10.1007/978-3-319-20958-6_2
Download citation
DOI: https://doi.org/10.1007/978-3-319-20958-6_2
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-20957-9
Online ISBN: 978-3-319-20958-6
eBook Packages: MedicineMedicine (R0)