Abstract
Among exercise-independent stresses, the most popular are dobutamine and dipyridamole. Dobutamine is the prototype of pharmacological adrenergic or inotropic stress. It was initially proposed for the diagnosis of coronary artery disease in combination with perfusion imaging [1] and later with two-dimensional (2D) echocardiography by the Liège group [2]. Other sympathomimetic agents have been proposed for stress echocardiography, including isoproterenol [3] and epinephrine [4], but these drugs often bring more pronounced arrhythmogenic side effects. Following the demonstration of low-dose dobutamine as a test of myocardial viability in 1990 [5], in the subsequent decade dobutamine has been extensively adopted in pharmacological stress echocardiography. The evolution of dobutamine stress paralleled that of other pharmacological stresses. With echocardiography, it began at relatively “low” doses (20 μg kg−1 min−1), which gave low sensitivity values [6]; later, more aggressive doses were adopted (up to 40 μg kg−1 min−1) [7, 8], and finally it was coadministered with atropine [9], which overcame the limitation of less than ideal sensitivity to minor forms of coronary artery disease.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Myocardial Viability
- Coronary Flow Reserve
- Stress Echocardiography
- Pharmacological Stress
- Dobutamine Stress
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Historical Background
Among exercise-independent stresses, the most popular are dobutamine and dipyridamole. Dobutamine is the prototype of pharmacological adrenergic or inotropic stress. It was initially proposed for the diagnosis of coronary artery disease in combination with perfusion imaging [1] and later with two-dimensional (2D) echocardiography by the Liège group [2]. Other sympathomimetic agents have been proposed for stress echocardiography, including isoproterenol [3] and epinephrine [4], but these drugs often bring more pronounced arrhythmogenic side effects. Following the demonstration of low-dose dobutamine as a test of myocardial viability in 1990 [5], in the subsequent decade dobutamine has been extensively adopted in pharmacological stress echocardiography. The evolution of dobutamine stress paralleled that of other pharmacological stresses. With echocardiography, it began at relatively “low” doses (20 μg kg−1 min−1), which gave low sensitivity values [6]; later, more aggressive doses were adopted (up to 40 μg kg−1 min−1) [7, 8], and finally it was coadministered with atropine [9], which overcame the limitation of less than ideal sensitivity to minor forms of coronary artery disease.
2 Pharmacology and Pathophysiology
Dobutamine is a synthetic catecholamine resulting from the modification of the chemical structure of isoproterenol. It acts directly and mainly on beta-1 adrenergic receptors of the myocardium, producing an increase in heart rate, enhancement of atrioventricular conduction, and increased contractility (Fig. 12.1). In fact, alpha-adrenergic activity can mediate systemic vasoconstriction and an increase in blood pressure and – at the coronary level – increased constriction up to coronary vasospasm, especially when the alpha-mediated vasoconstriction is enhanced by chronic or acute beta-blockade. Stimulation of beta-2 receptors on coronary arterioles may induce coronary arteriolar vasodilation. However, endothelial dysfunction and enhanced alpha-adrenergic tone contribute to the loss of dobutamine-induced vasodilation in coronary atherosclerosis [10]. The short half-life (2 min) of dobutamine allows rapid resolution of its effects once the intravenous infusion is discontinued. However, the alpha-mediated coronaro-constrictive and platelet-aggregating effects are not reversed, and may be potentiated, by beta-blockers and peak at 30–45 min after the end of infusion.
Dobutamine provokes ischemia mainly through the inotropic and chronotropic response to stimulation of myocardial beta-1 receptors determining an increase in myocardial oxygen demand (see Fig. 5.4 in Chap. 5). Heart rate increases two- to threefold, systolic arterial pressure increases 1.5- to twofold, and myocardial contractility increases four- to eightfold versus baseline. Other proischemic mechanisms are the flow maldistribution mediated by beta-2 receptors of coronary arterioles [11] and coronary vasospasm mediated by alpha-adrenoreceptors present on smooth muscle cells of epicardial arteries. The dobutamine dose usually employed for stress echocardiography testing causes a two- to threefold increase in coronary blood flow [12].
3 Methodology
The protocol displayed in Fig. 12.2 is the most widely used, the only one validated in a large-scale multicenter prospective trial [13], and it has been recently proposed as the state-of-the-art protocol by both the American [14] and European [15] recommendations. Doses lower than those shown in Fig. 12.2 are associated with insufficient sensitivity, while higher doses are associated with an unacceptable high rate of side effects. For viability assessment, steps of 5 min are used, starting from 5 up to 10 mcg [5]. However, to fully recruit the inotropic reserve in patients with heart failure and usually with beta-blocker therapy, high doses (without atropine) are required [16].
Alternatively, on the pharmacology basis that atropine may take up to 3 min to achieve maximum effect, there are studies suggesting that an early administration of atropine, at a starting dose of up to 20 μg kg−1 min−1, is more effective and equally accurate and may even be safer than a late atropine injection [17–20] and is also included in the American recommendations [14].
4 Feasibility and Safety
Minor but limiting side effects preclude the achievement of maximal pharmacological stress in about 10 % of patients [13, 21]. In order of frequency, these side effects are complex ventricular tachyarrhythmias (frequent, polymorphic, premature ventricular beats, couplets and triplets, nonsustained ventricular tachycardia), nausea and/or headache, hypotension (>30 mmHg drop in blood pressure) and/or bradycardia, supraventricular tachyarrhythmias (supraventricular tachycardia or atrial fibrillation), and hypertension. Limiting side effects are more often asymptomatic with dobutamine and more often symptomatic with dipyridamole [21]. Side effects usually disappear upon interruption of drug infusion, since the half-life is 2–3 min. When symptoms or ischemia persist, IV beta-blockers – usually the short-acting drug esmolol – are given.
Both the patient and the physician should be aware of the rate of major complications that may occur during dobutamine stress. As concordantly shown by meta-analysis [22], single-center experiences [23–28], multicenter studies [13], and retrospective registries [29–31], major life-threatening side effects occur in 1 of 300–350 cases (Table 12.1).
The proliferating anecdotal reports of catastrophes also contribute in assessing the safety of the test. Cardiac rupture [32–35], ventricular fibrillation [36, 37], refractory coronary vasospasm [38, 39], myocardial infarction [40, 41], cardiac asystole [42, 43], and acute Tako-tsubo syndrome [44] have all been described during dobutamine testing. Tachyarrhythmias are the most frequent complication occurring during dobutamine stress echocardiography. In some cases they are subsequent to pharmacologically induced myocardial ischemia during the test and therefore are associated with a transient wall motion abnormality. However, in many cases they are independent of ischemia and can also develop at low dobutamine doses. The mechanism of their onset can be attributed to the direct adrenergic arrhythmogenic effect of dobutamine, through myocardial β-receptor stimulation, which is particularly evident in patients with ischemic heart disease. Dobutamine infusion can also lower the blood potassium level, thereby contributing to the genesis of ventricular ectopy through a depolarizing effect on the cell membrane [45] (Fig. 12.3).
Significant hypotension, sometimes associated with bradyarrhythmias, including asystole, is another frequent adverse reaction during dobutamine echocardiography. In some cases this finding has been attributed to dynamic interventricular obstruction provoked by inotropic action of dobutamine, especially in hypertrophic hearts [46]. A vasodepressor reflex triggered by left ventricular mechanoreceptor stimulation (Bezold–Jarisch reflex) due to excessive inotropic stimulation may be an alternative mechanism [47]. These effects can be almost abolished if atropine is injected earlier.
Late and long-lasting transmural myocardial ischemia, with persistent ST segment elevation, is probably due to the coronary vasoconstrictive effect of dobutamine, through α-receptor stimulation, sometimes involving multiple coronary segments. Moreover, dobutamine can induce increased platelet aggregation, possibly provoking coronary occlusion, prolonged myocardial ischemia, and acute myocardial infarction on the anatomic substrate of a vulnerable, possibly noncritical, plaque unable to induce ischemia during stress [13, 48].
5 Diagnostic Results for Detection of Coronary Artery Disease
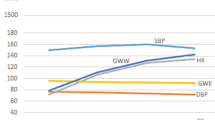
The accuracy in detecting angiographically assessed coronary artery disease has been consistently reported to be high, with sensitivity and specificity of 81 and 84 %, respectively, in a meta-analysis of 102 studies with over 7900 patients [49]. The diagnostic accuracy is similar to other forms of stress testing, such as exercise echocardiography [49, 50], dipyridamole echocardiography [49, 50], or stress SPECT [49]. In particular, the sensitivity and accuracy are identical to dipyridamole stress echocardiography when state-of-the-art protocols are used for both stresses (Fig. 12.4), as shown by two meta-analyses including 5 studies on 435 patients [50, 51].
The diagnostic accuracy for noninvasive detection of coronary artery disease of dobutamine echocardiography versus dipyridamole echocardiography (all protocols) and state-of-the-art (high dose with atropine or fast high dose) dipyridamole echocardiography (From meta-analysis of Noguchi et al. [50] and Picano et al. [51])
One of the strategies in order to improve sensitivity of dobutamine stress echocardiography is a rapid injection of (5 mg in 1 min) metoprolol at peak stress with the acquisition of post-metoprolol images in a maximum interval of 3 min after the end of dobutamine infusion in negative studies where patients are not hypertensive at peak stress. This strategy may increase the sensitivity (mainly in single-vessel disease patients) up to 92 % without loss in specificity (Fig. 12.5) [52]. A possible mechanism is the unmasking of coronary vasospasm mediated by unopposed alpha-adrenoreceptors.
(a) Example of a patient with a 90 % LAD stenosis without NWMA at peak developed only after metoprolol. Apical four-chamber view at end-systole with normal thickening at rest (HR of 46 beats min−1, rate-pressure product of 6578 mmHg min−1 and LVESVI 15.7 ml m−2) and low doses. At peak, HR was 139 beats min−1, rate-pressure product was 20,850 mmHg min−1, and LVESVI was 12.8 ml m−2. After metoprolol (Met), there is a lack of thickening in the apical septum (white arrows) (HR of 103 beats min−1, rate-pressure product of 15,450 mmHg min−1, and LVESVI 33.3 ml m−2). (b) EKG from patient in (a) demonstrating ST changes in leads D1, D2, aVF, V5, and V6 only during metoprolol
6 Identification of Myocardial Viability
Low-dose dobutamine recognizes myocardial viability with high specificity and good sensitivity, with excellent diagnostic [53] and prognostic [54] value. In patients with preserved global left ventricular function, myocardial viability identifies a greater risk to subsequent development of ischemia and nonfatal reinfarction early after acute myocardial infarction [55]. In patients with severe resting left ventricular dysfunction, a large amount of myocardial viability identified by low-dose dobutamine echocardiography is associated with a better survival [56]. This finding has been consistently described both in medically treated patients studied early after acute myocardial infarction [56] (a model of stunned myocardium) (Fig. 12.6) and in revascularized patients studied after chronic myocardial infarction (a model of hibernating myocardium) [57–59]. A contractile reserve identified by high-dose dobutamine (up to 40 mcg) identifies patients with dilated cardiomyopathy and better response to medical therapy and cardiac resynchronization therapy [60, 61].
Kaplan–Meier survival curves (considering only death as an end point) in patients stratified according to presence or absence of echocardiographically assessed viability and ischemia at low and high doses of dobutamine, respectively. Best survival is observed in patients with low-dose viability and no inducible ischemia; worst survival, in patients without viability and with inducible ischemia. Viability + and viability − indicate the presence or absence of myocardial viability at low-dose dobutamine, respectively; Dase + and Dase−, the presence or absence of myocardial ischemia at high-dose dobutamine, respectively (From Picano et al. [56])
Although the results of the STICH (Surgical Treatment for Ischemic Heart Failure) trial have cast doubt on the role of dobutamine stress echocardiography and other imaging modalities for the assessment of viability, the results are still predictive of a positive outcome [61]. When these are taken into consideration with previous studies [52–58], it becomes reasonable to recommend viability assessment when treating patients with coronary artery disease and left ventricular dysfunction [62].
7 Prognostic Value
The presence, site, timing, extent, and severity of dobutamine-induced wall motion abnormalities have a clear prognostic impact, as shown by over 50 studies on over 10,000 patients, including patients with or suspected coronary artery disease [63–72], evaluated early after acute myocardial infarction [73–77], and patients undergoing major noncardiac vascular surgery [78–85]. These studies concordantly show that dobutamine stress echocardiography results predict subsequent death, on the basis of coexistent fixed resting wall motion abnormalities, dobutamine dose required to induce ischemia (Fig. 12.7), and peak wall motion score index (Fig. 12.8). The prognostic value of dobutamine stress echocardiography is independent and additive to resting echocardiography and exercise electrocardiography and comparable to dipyridamole echocardiography [68, 86, 87] and stress SPECT [82, 88].
Kaplan–Meier survival curves event-free of cardiac death in patients with negative and positive dobutamine echocardiography test results (DOB). Survival is worse in patients with positive DOB. In patients with positive DOB, a progressively worse survival is identified with positivity after atropine, high and low dose (From Pingitore et al. [68])
Kaplan–Meier survival curves event-free of cardiac death in patients with negative and positive dobutamine echocardiography test results (DOB). In patients with positive DOB, a progressively worse survival is identified for patients with higher changes in peak wall motion score index (WMSI) (From Pingitore et al. [68])
8 Pitfalls
The limitations of dobutamine stress are related to feasibility, safety, technical difficulty of echocardiographic interpretation, suboptimal possibility to combine coronary flow reserve and wall motion information, and inability to predict physiologic therapy-induced changes on exercise stress results. Minor but limiting side effects occur in 5–10 % of tests, and submaximal results have limited diagnostic and prognostic power. The test is less safe than other pharmacological stresses, such as vasodilators, and much less safe than exercise, with major life-threatening complications being 2–3 times more frequent with dobutamine than with dipyridamole and 4–5 times more frequent than with exercise. The echocardiographic image degradation during stress is less than with exercise, but significant, since high heart rate and hypercontractility make the wall motion interpretation more challenging. Changes exerted by anti-ischemic therapy (especially beta-blockers) on dobutamine stress are unrelated to physiologic effects of that same therapy on exercise, and therefore the test cannot be used to monitor pharmacological interventions in ischemic heart disease [89].
9 Indications and Contraindications
High-dose dobutamine is an appropriate choice for pharmacological stress echocardiography used for the detection of coronary artery disease, especially in patients with inability to exercise or contraindications to exercise [90] or with resting images of borderline quality which may make the more technically difficult exercise stress echocardiography a challenging task [91] (Table 12.2). It is also appropriate in intermediate-risk patients undergoing elective high-risk noncardiac surgery. Low-dose dobutamine is the first choice for identification of myocardial viability in patients with severe left ventricular dysfunction [90]. It is also appropriate in low-flow, low-gradient aortic stenosis to separate true from pseudosevere aortic stenosis [92]. Appropriateness is uncertain in intermediate-risk patients undergoing intermediate-risk noncardiac surgery [90, 93]. In women who cannot exercise, dobutamine stress echocardiography may be preferred than other modalities [93, 94]. Patients with a history of complex atrial (paroxysmal atrial fibrillation, paroxysmal supraventricular tachycardia) or ventricular arrhythmias (sustained ventricular tachycardia or ventricular fibrillation) or with moderate to severe hypertension should probably not undergo dobutamine stress testing and be referred for safer vasodilator stress [95].
10 Emerging and Promising Technologies
10.1 Coronary Flow and Microvascular Measurements
Dobutamine allows a combined dual imaging of wall motion and coronary flow reserve with either coronary flow velocity reserve, myocardial contrast echocardiography, or deformation parameters of left ventricular function. In a recent study, the outcomes of 651 patients with normal wall motion response during stress echocardiography with dobutamine or dipyridamole stress to evaluate coronary flow velocity reserve (CFVR) were evaluated in diabetic patients. CFVR was calculated simultaneously in the distal territory of the left anterior descending coronary artery. Diabetes increased risk only in patients with abnormal CFVR (<2.0) independently of the pharmacological stress technique used [96]. The use of CFVR was also evaluated in 20 patients with Tako-tsubo cardiomyopathy. The authors demonstrated that hyperemic CFVR increased significantly after recovery leading to a greater CFVR (2.9 + 0.3 vs. 2.1 + 0.4) and concluded that there was a transient impairment of CFR at the acute phase of TTC, which was due to a reduced vasodilating capacity [97]. Dynamic changes in microcirculatory blood flow at each stage of DASE can also be detected using real-time myocardial contrast echocardiography. The best parameter for detecting CAD in all stages was β reserve, which could highly accurately separate patients with from without coronary artery disease [98].
10.2 Myocardial Function and Deformation Parameters
The need for a more quantitative method for the interpretation of stress echocardiography depended on the development of new imaging modalities. Tissue Doppler and myocardial strain derived from Doppler measurements, or two-dimensional (strain and strain rate), has been considered an important alternative to better quantify regional contraction at rest or during stress [99, 100].
Tissue Doppler is feasible during stress tests, however is limited by the need of a high frame rate of at least 140 (s-1), and is angle dependent. These constraints limit the accurate deformation analysis of apical segments [101].
Classically, myocardial ischemia is defined as the transient reduction of myocardial thickening during induction of stress through pharmacological or exercise stress. However, myocardial ischemia can also cause early and late systolic thickening, which unfortunately cannot be detected subjectively by the human eye, which has poor temporal resolution (30 frames per second), but can easily be measured by two-dimensional speckle tracking, a technique that is able to define deformation parameters known as Strain (fiber shortening) and Strain rate (fiber shortening over time) that are angle independent, making it more suitable for clinical practice. The results have been excellent in the experimental setting [102] and encouraging in the clinical realm [103], although some limitations do exist – as discussed in Chap. 23.
Real-time three-dimensional echocardiography during dobutamine stress has also been proposed to evaluate the extent and severity of CAD with good results and better specificity in multislice compared to multiplanar mode [104].
References
Mason JR, Palac RT, Freeman ML et al (1984) Thallium scintigraphy during dobutamine infusion: nonexercise-dependent screening test for coronary disease. Am Heart J 107:481–485
Berthe CN, Pierard LA, Hienaux M et al (1986) Predicting the extent and location of coronary artery disease in acute myocardial infarction by echocardiography during dobutamine infusion. Am J Cardiol 58:1167–1172
Fujita T, Ajisaka R, Matsumoto R et al (1986) Isoproterenol infusion stress two-dimensional echocardiography in diagnosis of coronary artery disease in elderly patients: comparison with the other stress testing methods. Jpn Heart J 27:287–297
Ferrara N, Leosco D, Longobardi G et al (1986) Use of epinephrine test in diagnosis of coronary artery disease. Am J Cardiol 158:256–260
Pierard LA, De Landsheere CM, Berthe C et al (1990) Identification of viable myocardium by echocardiography during dobutamine infusion in patients with myocardial infarction after thrombolytic therapy: comparison with positron emission tomography. J Am Coll Cardiol 15:1021–1031
Mannering D, Cripps T, Leech G et al (1988) The dobutamine stress test as an alternative to exercise testing after acute myocardial infarction. Br Heart J 59:521–526
Previtali M, Lanzarini L, Ferrario M et al (1991) Dobutamine versus dipyridamole echocardiography in coronary artery disease. Circulation 83(Suppl 3):27–31
Cohen JL, Greene TO, Ottenweller J et al (1991) Dobutamine digital echocardiography for detecting coronary artery disease. Am J Cardiol 67:1311–1318
McNeill AJ, Fioretti PM, EI-Said EM et al (1992) Enhanced sensitivity for detection of coronary artery disease by addition of atropine to dobutamine stress echocardiography. Am J Cardiol 170:41–46
Barbato E, Bartunek J, Wyffels E et al (2003) Effects of intravenous dobutamine on coronary vasomotion in humans. J Am Coll Cardiol 42:1596–1601
Warltier DC, Zyvoloski M, Gross GJ et al (1981) Redistribution of myocardial blood flow distal to a dynamic coronary arterial stenosis by sympathomimetic amines: comparison of dopamine, dobutamine and isoproterenol. Am J Cardiol 48:269–279
Severi S, Underwood R, Mohiaddin RH et al (1995) Dobutamine stress: effects on regional myocardial blood flow and wall motion. J Am Coll Cardiol 26:l187–l195
Picano E, Mathias W Jr, Pingitore A et al; on behalf of the EDIC study group (1994) Safety and tolerability of dobutamine-atropine stress echocardiography: a prospective, large-scale, multicenter trial. Lancet 344:1190–1192
Pellikka PA, Nagueh SF, Elhendy AA et al; American Society of Echocardiography (2007) American Society of Echocardiography recommendations for performance, interpretation, and application of stress echocardiography. J Am Soc Echocardiogr 20:1021–1041
Sicari R, Nihoyannopoulos P, Evangelista A et al; European Association of Echocardiography (2008) Stress echocardiography expert consensus statement: European Association of Echocardiography (EAE) (a registered branch of the ESC). Eur J Echocardiogr 9:415–437
Pratali L, Picano E, Otasevic P et al (2001) Prognostic significance of the dobutamine echocardiography test in idiopathic dilated cardiomyopathy. Am J Cardiol 88:1374–1378
Lewandowski T, Armstrong W, Bach D (1998) Reduced test time by early identification of patients requiring atropine during dobutamine stress echocardiography. J Am Soc Echocardiogr 11:236–243
Burger A, Notarianni M, Aronson D (2000) Safety and efficacy of an accelerated dobutamine stress echocardiography protocol in the evaluation of coronary artery disease. Am J Cardiol 86:825–829
Tsutsui JM, Lario FC, Fernandes DR et al (2005) Safety and cardiac chronotropic responsiveness to the early injection of atropine during dobutamine stress echocardiography in the elderly. Heart 91:1563–1567
Tsutsui JM, Osório AFF, Lario F et al (2004) Comparison of safety and efficacy of the early injection of atropine during dobutamine stress echocardiography with the conventional protocol. Am J Cardiol 94:1367–1372
Pingitore A, Picano E, Colosso MQ et al (1996) The atropine factor in pharmacologic stress echocardiography. Echo Persantine (EPIC) and Echo Dobutamine International Cooperative (EDIC) Study Groups. J Am Coll Cardiol 27:1164–1170
Lattanzi F, Picano E, Adamo E et al (2000) Dobutamine stress echocardiography: safety in diagnosing coronary artery disease. Drug Saf 22:251–262
Mertes H, Sawada S, Ryan T et al (1993) Symptoms, adverse effects, and complications associated with dobutamine stress echocardiography. Experience in 1118 patients. Circulation 88:15
Poldermans D, Fioretti PM, Boersma E et al (1994) Safety of dobutamine-atropine stress echocardiography in patients with suspected or proven coronary artery disease: experience in 650 consecutive examinations. Am J Cardiol 73:456–459
Zahn R, Lotter R, Nohl H et al (1996) Feasibility and safety of dobutamine stress echocardiography: experiences with 1,000 studies. Z Kardiol 85:28–34
Secknus MA, Marwick TH (1997) Evolution of dobutamine echocardiography protocols and indications: safety and side effects in 3,011 studies over 5 years. J Am Coll Cardiol 29:1234–1240
Bremer ML, Monahan KH, Stussy VL et al (1998) Safety of dobutamine stress echocardiography supervised by registered nurse sonographers. J Am Soc Echocardiogr 11:601–605
Mathias W Jr, Arruda A, Santos FC et al (1999) Safety of dobutamine-atropine stress echocardiography: a prospective experience of 4,033 consecutive studies. J Am Soc Echocardiogr 12:785–791
Pezzano A, Gentile F, Mantero A et al (1998) RITED (Registro Italiano Test Eco-Dobutamina): side effects and complications of echo-dobutamine stress test in 3041 examinations. G Ital Cardiol 28:102–111
Beckmann SH, Haug G (1999) National registry 1995–1998 on 150,000 stress echo examinations: side effects and complications in 60,448 examinations of the registry 1997–1998. Circulation 100(suppl):3401
Varga A, Garcia MA, Picano E, International Stress Echo Complication Registry (2006) Safety of stress echocardiography (from the International Stress Echo Complication Registry). Am J Cardiol 98:541–543
Reisenhofer B, Squarcini G, Picano E (1998) Cardiac rupture during dobutamine stress test. Ann Intern Med 128:605
Orlandini AD, Tuero EI, Diaz R et al (2000) Acute cardiac rupture during dobutamine-atropine echocardiography stress test. J Am Soc Echocardiogr 13:152–153
Daniels CJ, Orsinelli DA (1997) Cardiac rupture with dobutamine stress echocardiography. J Am Soc Echocardiogr 10:979–981
Zamorano J, Moreno R, Almeria C et al (2002) Left ventricular free wall rupture during dobutamine stress echocardiography. Rev Esp Cardiol 55:312–314
Varga A, Picano E, Lakatos F (2000) Fatal ventricular fibrillation during a low-dose dobutamine stress test. Am J Med 108:352–353
Shaheen J, Mendzelevski B, Tzivoni D (1996) Dobutamine-induced ST segment elevation and ventricular fibrillation with nonsignificant coronary artery disease. Am Heart J 132:1058–1060
Yamagishi H, Watanabe H, Toda I et al (1998) A case of dobutamine-induced coronary arterial spasm with ST-segment elevation. Jpn Circ J 62:150–151
Alvarez L, Zamorano J, Mataix L et al (2002) Coronary Spasm after Administration of Propranolol during Dobutamine Stress Echocardiography. Rev Esp Cardiol 55:778–781
Weidmann B, Lepique CU, Jansen W et al (1997) Myocardial infarction as a complication of dobutamine stress echocardiography. J Am Soc Echocardiogr 10:768–771
Takeuchi M, Sonoda S, Hanada H et al (1997) Acute myocardial infarction in a patient during dobutamine stress echocardiography. Cathet Cardiovasc Diagn 41:404–406
Lanzarini L, Previtali M, Diotallevi P (1996) Syncope caused by cardiac asystole during dobutamine stress echocardiography. Heart 75:320–321
Salustri A, Biferali F, Palamara A (1997) Cardiac arrest during dobutamine stress echocardiography. G Ital Cardiol 27:69–71
Martinez-Quintana E, Miranda-Garcia C, Gopar-Gopar S et al (2014) Transient apical ballooning syndrome during dobutamine stress echocardiography – Clin Investig Arterioscler 26:200–203
Coma-Canella I (1991) Changes in plasma potassium during the dobutamine stress test. Int J Cardiol 33:55–59
Tanimoto M, Pai RG, Jintapakorn W, Shah PM (1995) Mechanisms of hypotension during dobutamine stress echocardiography in patients with coronary artery disease. Am J Cardiol 76:26–30
Heinle SK, Tice FD, Kisslo J (1995) Hypotension during dobutamine stress echocardiography: is it related to dynamic intraventricular obstruction? Am Heart J 130:314–317
Galloway MT, Paglieroni TG, Wun T et al (1995) Platelet activation during dobutamine stress echocardiography. Am Heart J 135:888–900
Heijenbrok-Kal MH, Fleischmann KE, Hunink MG (2007) Stress echocardiography, stress single-photon-emission computed tomography and electron beam computed tomography for the assessment of coronary artery disease: a meta-analysis of diagnostic performance. Am Heart J 154:415–423
Noguchi Y, Nagata-Kobayashi S, Stahl JE et al (2005) A meta-analytic comparison of echocardiographic stressors. Int J Cardiovasc Imaging 21:189–207
Picano E, Molinaro S, Pasanisi E (2008) The diagnostic accuracy of pharmacological stress echocardiography for the detection of coronary artery disease: a meta-analysis. Cardiovasc Ultrasound 6:30
Mathias W Jr, Tsutsui JM, Andrade JL et al (2003) Value of rapid beta-blocker injection at peak dobutamine-atropine stress echocardiography for detection of coronary artery disease. J Am Coll Cardiol 41:1583–1589
Bax JJ, Poldermans D, Elhendy A, Boersma E, Rahimtoola SH (2001) Sensitivity, specificity, and predictive accuracies of various noninvasive techniques for detecting hibernating myocardium. Curr Probl Cardiol 26:141–186
Allman KC, Shaw LJ, Hachamovitch R, Udelson JE (2002) Myocardial viability testing and impact of revascularization on prognosis in patients with coronary artery disease and left ventricular dysfunction: a meta-analysis. J Am Coll Cardiol 39:1151–1158
Sicari R, Picano E, Landi P et al (1997) Prognostic value of dobutamine-atropine stress echocardiography early after acute myocardial infarction. Echo Dobutamine International Cooperative (EDIC) Study. J Am Coll Cardiol 29:254–260
Picano E, Sicari R, Landi P et al (1998) Prognostic value of myocardial viability in medically treated patients with global left ventricular dysfunction early after an acute uncomplicated myocardial infarction: a dobutamine stress echocardiographic study. Circulation 15:1078–1084
Meluzin J, Cerny J, Frelich M et al (1998) Prognostic value of the amount of dysfunctional but viable myocardium in revascularized patients with coronary artery disease and left ventricular dysfunction. Investigators of this Multicenter Study. J Am Coll Cardiol 32:912–920
Senior R, Kaul S, Lahiri A (1999) Myocardial viability on echocardiography predicts long-term survival after revascularization in patients with ischemic congestive heart failure. J Am Coll Cardiol 33:1848–1854
Sicari R, Picano E, Cortigiani L, Borges AC, Varga A, Palagi C, Bigi R, Rossini R, Pasanisi E, VIDA (Viability Identification with Dobutamine Administration) Study Group (2003) Prognostic value of myocardial viability recognized by low-dose dobutamine echocardiography in chronic ischemic left ventricular dysfunction. Am J Cardiol 92:1263–1266
Ciampi Q, Villari B (2007) Role of echocardiography in diagnosis and risk stratification in heart failure with left ventricular systolic dysfunction. Cardiovasc Ultrasound 5:34
Bonow RO, Maurer G, Lee KL et al (2011) Myocardial viability and survival in ischemic left ventricular dysfunction. N Engl J Med 364:1617–1625
Yancy CW, Jessup M, Bozkurt B et al; American College of Cardiology Foundation; American Heart Association Task Force on Practice Guidelines (2013) 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 62:e147–239
Afridi I, Quinones MA, Zoghbi WA, Cheirif J (1994) Dobutamine stress echocardiography: sensitivity, specificity and predictive value for future cardiac events. Am Heart J 127:1510
Poldermans D, Fioretti PM, Boersma E et al (1994) Dobutamine-atropine stress echocardiography and clinical data for predicting late cardiac events in patients with suspected coronary artery disease. Am J Med 97:119–125
Marcovitz PA, Shayna V, Horn RA, Hepner A, Armstrong WF (1996) Value of dobutamine stress echocardiography in determining the prognosis in patients with known or suspected coronary artery disease. Am J Cardiol 78:404–408
Steinberg EH, Madmon L, Patel CP et al (1997) Long-term prognostic significance of dobutamine echocardiography in patients with suspected coronary artery disease: results of a 5-Year follow-up study. J Am Coll Cardiol 29:269–273
Chuah SC, Pellikka PA, Roger VL, McCully RB, Seward JB (1998) Role of dobutamine stress echocardiography in predicting outcome in 860 patients with known or suspected coronary artery disease. Circulation 97:1474–1480
Pingitore A, Picano E, Varga A et al (1999) Prognostic value of pharmacological stress echocardiography in patients with known or suspected coronary artery disease: a prospective, large-scale, multicenter, head-to-head comparison between dipyridamole and dobutamine test. Echo-Persantine International Cooperative (EPIC) and Echo-Dobutamine International Cooperative (EDIC) Study Groups. J Am Coll Cardiol 34:1769–1777
Krivokapich J, Child JS, Walter DO, Garfinkel A (1999) Prognostic value of dobutamine stress echocardiography in predicting cardiac events in patients with known or suspected coronary artery disease. J Am Coll Cardiol 33:708–716
Poldermans D, Fioretti PM, Boersma E et al (1999) Long-term prognostic value of dobutamine-atropine stress echocardiography in 1737 patients with known or suspected coronary artery disease: a single-center experience. Circulation 99:757–762
Marwick TH, Case C, Sawada S et al (2001) Prediction of mortality using dobutamine echocardiography. J Am Coll Cardiol 37:754–760
Sicari R, Pasanisi E, Venneri L et al; Echo Persantine International Cooperative (EPIC) Study Group; Echo Dobutamine International Cooperative (EDIC) Study Group (2003) Stress echo results predict mortality: a large scale multicenter prospective international study. J Am Coll Cardiol 41:589–595
Carlos ME, Smart SC, Wynsen JC, Sagar KB (1997) Dobutamine stress echocardiography for risk stratification after myocardial infarction. Circulation 18:1402–1410
Greco CA, Salustri A, Seccareccia F et al (1997) Prognostic value of dobutamine echocardiography early after uncomplicated acute myocardial infarction: a comparison with exercise electrocardiography. J Am Coll Cardiol 29:261–267
Swinburn JM, Senior R (2006) Myocardial viability assessed by dobutamine stress echocardiography predicts reduced mortality early after acute myocardial infarction determining the risk of events after myocardial infarction (DREAM) study. Heart 92:44–48
Previtali M, Fetiveau R, Lanzarini L et al (1998) Prognostic value of myocardial viability and ischemia detected by dobutamine stress echocardiography early after acute myocardial infarction treated with thrombolysis. J Am Coll Cardiol 32:380–386
Sicari R, Landi P, Picano E et al (2002) Exercise-electrocardiography and/or pharmacological stress echocardiography for non-invasive risk stratification early after uncomplicated myocardial infarction. A prospective international large scale multicentre study. Eur Heart J 23:1030–1037
Eichelberger JP, Schwarz KQ, Black ER, Green RM, Ouriel K (1993) Predictive value of dobutamine echocardiography just before noncardiac vascular surgery. Am J Cardiol 72:602–607
Davila-Roman VG, Waggoner AD, Sicard GA et al (1993) Dobutamine stress echocardiography predicts surgical outcome in patients with an aortic aneurysm and peripheral vascular disease. J Am Coll Cardiol 21:957–963
Poldermans D, Arnese M, Fioretti PM et al (1995) Improved cardiac risk stratification in major vascular surgery with dobutamine atropine stress echocardiography. J Am Coll Cardiol 26:648–653
Poldermans D, Arnese M, Fioretti PM et al (1997) Sustained prognostic value of dobutamine stress echocardiography for late cardiac events after major noncardiac vascular surgery. Circulation 195:53–58
Shaw LJ, Peterson ED, Kesler K, Hasselblad V, Califf RM (1996) Meta-analysis of intravenous dipyridamole-thallium-201 imaging (1985 to 1994) and dobutamine echocardiography (1991 to 1994) for risk stratification before vascular surgery. Am J Cardiol 78:1327–1337
Kertai MD, Boersma E, Bax JJ et al (2003) A meta-analysis comparing the prognostic accuracy of six diagnostic tests for predicting perioperative cardiac risk in patients undergoing major vascular surgery. Heart 89:1327–1334
Beattie WS, Abdelnaem E, Wijeysundera DN (2006) A meta-analytic comparison of preoperative stress echocardiography and nuclear scintigraphy imaging. Anesth Analg 102:8–16
Vahanian A, Alfieri O, Al-Attar N et al; European Association of Cardio-Thoracic Surgery; European Society of Cardiology; European Association of Percutaneous Cardiovascular Interventions (2008) Transcatheter valve implantation for patients with aortic stenosis: a position statement from the European Association of Cardio-Thoracic Surgery (EACTS) and the European Society of Cardiology (ESC), in collaboration with the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur Heart J 29:1463–1470
Minardi G, Di Segni M, Manzara CC et al (1997) Diagnostic and prognostic value of dipyridamole and dobutamine stress echocardiography in patients with Q-wave acute myocardial infarction. Am J Cardiol 80:847–851
Schröder K, Wieckhorst A, Völler H (1997) Comparison of the prognostic value of dipyridamole and dobutamine stress echocardiography in patients with known or suspected coronary artery disease. Am J Cardiol 79:1516–1518
Schinkel AF, Bax JJ, Elhendy A, van Domburg RT et al (2004) Long-term prognostic value of dobutamine stress echocardiography compared with myocardial perfusion scanning in patients unable to perform exercise tests. Am J Med 117:1–9
Dodi C, Pingitori A, Sicari R et al (1997) Effects of Antianginal therapy with a calcium antagonist and nitrates on dobutamine stress echocardiography. Eur Heart J 18:242–248
Wolk MJ, Bailey SR, Doherty JU et al; American College of Cardiology Foundation Appropriate Use Criteria Task Force (2014) ACCF/AHA/ASE/ASNC/HFSA/HRS/SCAI/SCCT/SCMR/STS 2013 multimodality appropriate use criteria for the detection and risk assessment of stable ischemic heart disease: a report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, American Heart Association, American Society of Echocardiography, American Society of Nuclear Cardiology, Heart Failure Society of America, Heart Rhythm Society, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, Society for Cardiovascular Magnetic Resonance, and Society of Thoracic Surgeons. J Am Coll Cardiol 63:380–406
Beleslin BD, Ostojic M, Stepanovic J et al (1994) Stress echocardiography in the detection of myocardial ischemia. Head-to-head comparison of exercise, dobutamine, and dipyridamole tests. Circulation 90:1168–1176
McMurray JJ, Adamopoulos S, Anker SD et al (2012) ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012. The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail 14:803–869
Montalescot G, Sechtem U, Achenbach S et al (2013) 2013 ESC guidelines on the management of stable coronary artery disease: the Task Force on the management of stable coronary artery disease of the European Society of Cardiology. Eur Heart J 34:2949–3003
Cordovil A, Mathias W, Andrade JL et al (2004) Role of dobutamine-atropine stress echocardiography in prognostic evaluation of 300 women. Echocardiography 21:113–118
Cortigiani L, Bigi R, Rigo F et al; Echo Persantine International Cooperative Study Group (2003) Diagnostic value of exercise electrocardiography and dipyridamole stress echocardiography in hypertensive and normotensive chest pain patients with right bundle branch block. J Hypertens 21:2189–2194
Lowenstein JA, Caniggia C, Rousse G et al (2014) Coronary flow velocity reserve during pharmacologic stress echocardiography with normal contractility adds important prognostic value in diabetic and nondiabetic patients. J Am Soc Echocardiogr 27:1113–1119
Meimoun P, Malaquin D, Benali T et al (2009) Transient impairment of coronary flow reserve in Tako-tsubo cardiomyopathy is related to left ventricular systolic parameters. Eur J Echocardiogr 10:265–270
Mathias W Jr, Kowatsch I, Saroute AN et al (2011) Dynamic changes in microcirculatory blood flow during dobutamine stress assessed by quantitative myocardial contrast echocardiography. Echocardiography 28:993–1001
Urheim S, Edvardsen T, Torp H et al (2000) Myocardial strain by Doppler echocardiography. Validation of a new method to quantify regional myocardial function. Circulation 102:1158–1164
Voigt JU, Exner B, Schmiedehausen K et al (2003) Strain- rate imaging during dobutamine stress echocardiography provides objective evidence of inducible ischemia. Circulation 107:2120–2126
Castro PL, Greenberg NL, Drinko J et al (2000) Potential pitfalls of strain rate imaging: angle dependency. Biomed Sci Instrum 36:197–202
Reant P, Labrousse L, Lafitte S et al (2008) Experimental validation of circumferential, longitudinal, and radial 2-dimensional strain during dobutamine stress echocardiography in ischemic conditions. J Am Coll Cardiol 51:149–157
Hwang J, Lee HM, Yang IH et al (2014) The value of assessing myocardial deformation at recovery after dobutamine stress echocardiography. J Cardiovasc Ultrasound 22:127–133
Yoshitani H, Takeuchi M, Mor-Avi V et al (2009) Comparative diagnostic accuracy of multiplane and multislice three-dimensional dobutamine stress echocardiography in the diagnosis of coronary artery disease. J Am Soc Echocardiogr 22:437–442
Author information
Authors and Affiliations
Table of Contents Video Companion
Table of Contents Video Companion
-
See stress echo primer, cases 8, 9, 10, 11, and 12.
-
See also, in the section illustrative cases, cases 11 (coronary artery disease), 32 to 35 (valvular heart disease), and 36 (heart transplant).
-
See also in the section “Nuovo Cinema Paradiso Remastered” the 2 short movies: Myocardial viability, a moonlight serenade, and Rocky Horror stress echo picture show.
-
See also in the section “Selected presentations: Angels in the stress echo lab.”
-
Springer Extra Materials available at http://extras.springer.com/2015/978-3-319-20957-9
Rights and permissions
Copyright information
© 2015 Springer International Publishing
About this chapter
Cite this chapter
Mathias, W., Picano, E. (2015). Dobutamine Stress Echocardiography. In: Stress Echocardiography. Springer, Cham. https://doi.org/10.1007/978-3-319-20958-6_12
Download citation
DOI: https://doi.org/10.1007/978-3-319-20958-6_12
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-20957-9
Online ISBN: 978-3-319-20958-6
eBook Packages: MedicineMedicine (R0)