Abstract
Coronary artery disease (CAD) is the most common cause of death in the whole world. Acute myocardial infarction with ST elevation (STEMI) is a clinical syndrome characterized by the typical symptoms of myocardial ischemia with electrocardiographic ST elevation (persistent for more than 20 min) and following release in cardiac biomarkers. Coronary atherosclerosis complicated by coronary thrombosis with totally occlusion of the coronary artery is the main cause of STEMI. So, mechanical or pharmacological reperfusion should be considered as soon as possible and dual antiplatelet therapy and anticoagulant drugs should be administered. Arrhythmias are very frequent in the acute phase of STEMI, and every kind of arrhythmia could be seen.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Cardiogenic Shock
- Unfractionated Heparin
- Primary Percutaneous Coronary Intervention
- Dual Antiplatelet Therapy
- STEMI Patient
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Case Report
A 44-year-old man was referred to our ICU at 1:30 AM from the medical first aid due to intense, prolonged, non irradiated retrosternal pain, insurgent at 00:30 AM while sleeping, and profuse cold sweating. The medical first aid recorded an ECG immediately, at their arrival, that showed sinus rhythm, third-grade AV block, narrow QRS escape rhythm with a heart rate of 33 bpm, ST elevation in the inferior leads (DII, DIII, aVf) with specular ST depression in DI and aVl, and QRS axis of 105°. Blood pressure was 90/50 mmHg. Therapy with salicylic acid 500 mg IV, unfractionated heparin 4000 UI IV and clopidogrel 300 mg per os therapy was administered. The patient was immediately transferred to our ICU for further evaluation and treatment.
1.1 Medical History and Cardiovascular Risk Factors
-
Cardiovascular risk factors: systemic arterial hypertension and dyslipidemia
-
Family history: no family history of structural heart disease
-
2005: stab wound in the midsternal area
1.2 Allergies
None
1.3 Medications
None
1.4 Vital Signs
-
Temperature: 36.5 °C
-
Heart rate: 33 bpm
-
Arterial blood pressure: 85/50 mmHg
-
Respiratory rate: 20 breaths/min
-
Oxygen saturation: 97 %
1.5 Physical Examination
-
General appearance: well developed, well nourished, alert but confused, suffering from retrosternal pain, with pallor and cold sweat
-
Lungs: dyspnea; clear to percussion and auscultation without rhonchi, wheezing, or diminished breath sounds; presence of bibasilar rales
-
Cardiovascular: normal S1 and S2; no S3, S4, or murmurs; regular rhythm; no vascular murmurs
-
Abdomen: positive bowel sounds, soft and non-distended, no guarding or rebound, no masses
1.6 Routine Laboratory Test
White blood cells 17,000 mmc, total cholesterol 338 mg/dl, triglycerides 853 mg/ml, AST 398 U/L, ALT 117 U/L, LDH 689 U/L, γGT 60 U/L, troponin I highly specific 116 ng/ml, CKMB 222.8 ng/ml, and uric acid 8.4 mg/ml. The remaining laboratory tests were normal.
1.7 Instrumental Examination
The ECG at entrance (Fig. 1.1a, b) confirmed the previous one, already described.
A complete echocardiographic examination was performed and showed normal dimensions of the cardiac chambers, reduced systolic left ventricle function (EF 45 %) due to hypokinesia of the inferior and posterolateral wall, normal right ventricular function (TAPSE 21 mm), and mild mitral and tricuspid regurgitation with normal pulmonary artery systolic pressure.
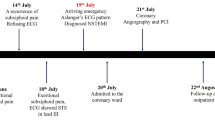
1.8 Clinical Course and Therapeutic Management
These findings all together were suggestive for inferior ST elevation acute coronary syndrome complicated by third-degree AV block.
As soon as possible, a transcutaneous pacing and a continuous electrocardiographic, blood pressure, and oxygen saturation monitoring were placed, and the cath lab team was advised. Therapy with crystalloid and dopamine 5 gamma/kg/min infusion was practiced with blood pressure increase to 120/70 mmHg, and morphine was administered for the transcutaneous pacing pain. At 1:45 AM the patient was transferred to the cath lab to perform coronary angiography and to position a temporary pacing via the right femoral vein. The angiography showed right coronary artery dominance with thrombotic occlusion of its middle tract; no other stenosis was present. At 2:05 AM the patient underwent manual thrombus aspiration (EXPORT) and PTCA with medicated self-expanding stent (STENTYS DES 3.5−4.5 × 17 mm) implantation via the right radial artery. A bolus of abciximab 0.25 mg/kg was administered, and the patient was shifted to prasugrel with a loading dose of 60 mg administered in the cath lab. The residual stenosis was <20 % and TIMI flow was 3. Continuous unfractionated heparin infusion was administered during the 12 h following the procedure. The transvenous pacing was removed 48 h later being the patient again in stable sinus rhythm. Continuous electrocardiographic monitoring during the first 6 days did not show any dangerous tachyarrhythmia or bradyarrhythmia. Therapy with ASA 100 mg od, prasugrel 10 mg od, atorvastatin 80 mg od, losartan 12.5 mg od, and pantoprazole 40 mg od was started since the first day. Metoprolol tartrate 25 mg bid was added the second day. The patient was transferred to our semi-intensive cardiology unit on the third day and then discharged on the seventh day with a follow-up visit, ECG, and echocardiography programmed 2 months later. Therapy at discharge was ASA 100 mg od, prasugrel 10 mg od for 12 months, atorvastatin 80 mg od, losartan 12.5 mg od, pantoprazole 40 mg, and metoprolol tartrate 25 mg bid.
2 ST Elevation Myocardial Infarction (STEMI)
2.1 Definition and Epidemiology
The last ESC guidelines published in 2012 define “acute myocardial infarction” (AMI) as the evidence of myocardial necrosis (elevation of cardiac biomarkers, typical ECG alterations, imaging alterations, or autopsy evidence) in the presence of a clinical setting suggestive for myocardial ischemia [1].
Acute myocardial infarction with ST elevation (STEMI) is a clinical syndrome characterized by the typical symptoms of myocardial ischemia with electrocardiographic ST elevation (persistent for more than 20 min) and following release of cardiac biomarkers [2].
Coronary artery disease (CAD) is the most common cause of death in the whole world. In 2012, 7.4 million people in Europe (which is 13.2 % of all deaths) died from CAD [3].
At present, up to 25–40 % of AMI presentations are STEMI ones [4–7]. The incidence of STEMI hospital admissions is different among countries that belong to ESC [8]. In the last decades there has been a STEMI incidence decrease despite an NSTEMI incidence increase. In the Sweden registry, which is probably the most comprehensive STEMI registry, an incidence of 66 STEMI/100,000/year, similar to those of other countries like the Czech Republic [9], Belgium [8], and the USA [10], has been reported.
The in-hospital mortality of unselected STEMI patients varies from 6 to 14 % [8]. Ejection fraction, the Killip class, age, time delay to treatment and mode of treatment, prior myocardial infarction history, renal dysfunction, diabetes mellitus, and diseased coronary artery number are all factors that influence mortality. Hospitals with a high clinical volume and high rate of invasive procedures have lower mortality rates [11]. STEMI mortality significantly decreased thanks to a frequency care increase [5, 7].
2.2 Pathology and Pathophysiology
2.2.1 Pathology
The causes of STEMI are different, but they can be divided into two principal groups:
-
Coronary atherosclerosis complicated by coronary thrombosis, the main one
-
Non-atherogenic forms that are rare such as arteritis, trauma to coronary arteries, coronary mural thickening with metabolic disease or intimal proliferative disease, emboli to coronary arteries, congenital coronary artery anomalies, myocardial oxygen demand–supply disproportion, hematologic, and miscellaneous [12]
We will focus our attention on the first cause of STEMI, the coronary atherosclerosis.
A previous classification based on ECG evolution divided patients with MI into two groups: patients with a Q-wave infarction, very often considered a transmural infarction, and patients with a non-Q-wave infarction. Currently, a new classification based on pathophysiology divides patients into other two groups: those with STEMI related to an acute thrombotic occlusion of an epicardial coronary artery and those with NSTEMI/unstable angina, due to stenosis of a coronary artery without occlusive thrombi. When there is a chronic total occlusion of the coronary artery, patients do not always have an MI because of collateral blood flow development and other factors.
The most important element on AMI’s physiopathology is the atherosclerotic plaque. The plaque evolution is an active process lasting years that consists in intima lipoprotein accumulation, lipoprotein oxidation and glycation, intima leukocyte migration, foam cell development, intima smooth cell migration with consequent extracellular matrix accumulation, atherosclerotic plaque growth, and a fibrofatty lesion formation with a lipid core surrounded by an acellular fibrous capsule. Cytokines and effector molecules like hypochlorous acid and superoxide anion play an important role in this process.
During this natural evolution, high-risk plaques can undergo plaque disruption [13, 14] that is induced by stressors like intramural blood pressure, coronary vasomotor tone, and tachycardia. So, thrombogenic substances are exposed with secondary activation and aggregation of platelet; moreover, thrombin generation is promoted with subsequent thrombus formation. There is seasonal and circadian variation of some of these key physiologic variations, and that is why STEMI happens more frequently in the winter early morning hours and following natural disasters [15].
Anatomically, two major types of MI can be detected: transmural infarcts characterized by the presence of a full ventricular wall thickness myocardial necrosis and nontransmural or subendocardial MI with necrosis involvement of the subendocardium or intramural myocardium or both. In the first case, there is a completely occlusive thrombus of an epicardial coronary artery that subtends the infarct area with a typical ST-segment elevation. The transmural necrosis can cause a full wall thickness vital myocardial loss and subsequent fibrosis that is evidenced by Q-wave evolution in the leads overlying the infarcted zone. In a few number of patients, there is not a Q-wave evolution but an R-wave height reduction.
There is a specific correlation between the coronary artery occluded, the myocardial area developing necrosis, and the ECG derivation that shows an ST elevation (Fig. 1.2).
Schematic representation of left ventricle segments, Einthoven’s triangle with electrocardiogram derivations. LAD supplies segments nr 1, 2, 6, 7, 8, 12, 13, 14, 15, 16, and 17; LCX supplies segments nr 4, 5, 6, 10, 11, 12, 15, 16, and 17; RCA supplies segments nr 3, 4, 9, 10, 11, 14, 15, 16, and 17. Areas of shared perfusion between LAD, LCX, and RCA are shown in green. The infarct artery can be deduced identifying the leads with ST-segment elevation and correlating these with the segments that these leads explore and so with coronary arteries that supply these segments. For example, ST segment elevated prominently in leads exploring segments 1, 2, 7, 8, 13, 14, and 17 which means that the occluded vessel is the LAD. LAD, left anterior descending; RCA, right coronary artery; LCX, left circumflex
The earliest myocardial ultrastructural changes occurring within the first 20 min are reversible. Changes become irreversible after 20 min up to 120 min of ischemia [16]. After 6–12 h of necrosis onset, myocardium gross alteration can be identified. So, in the first 30 min after ischemia onset, myocardial injury is reversible; subsequently, a progressive viability loss occurs and usually completes at 6–12 h. That is the reason why the reperfusion therapy benefits are greatest when patients are treated early.
Generally, the right ventricle is less involved by infarction. It is interested in approximately 50 % of patients with transmural infarct of the inferoposterior wall and posterior portion of the septum [17]. The right ventricle shows an excellent recovery of systolic function once reperfusion is restored [18].
2.2.2 Pathophysiology
When a coronary artery is occluded, immediate myocardial contractile alteration occurs. There are four sequential patterns of abnormal contraction:
-
Dyssynchrony (adjacent segments do not contract at the same time)
-
Hypokinesia (reduced contraction)
-
Akinesia (cessation of contraction)
-
Dyskinesia (the segment expansion is paradoxical)
As an acute compensation of these alterations, a hyperkinesia of the normal myocardium segments usually firstly develops. It results from sympathetic nervous system activity increase and Frank–Starling mechanism and lasts up to 2 weeks.
If ischemic injury involves >15 % of the myocardium, the systolic–diastolic function of the LV becomes depressed, and a decline of cardiac output, stroke volume, and blood pressure occurs. End-systolic volume and end-diastolic pressure increase and diastolic dysfunction appears. The degree of end-systolic volume increase has been shown to be an important predictor of STEMI mortality [19]. If ischemic injury involves >25 % of the myocardium, clinical heart failure becomes typical, and if the myocardial loss is >40 %, cardiogenic shock appears.
Improvement is possible thanks to the recovery of the stunned (reversibly injured) myocardium after revascularization, but in some patients the infarcted LV may dilate causing LV remodeling. This can be a compensatory mechanism restoring a normal stroke at the expense of a reduced ejection fraction; however, dilation elevates afterload (Laplace’s law) that depresses LV stroke volume and increments the consumption of myocardial oxygen, intensifying myocardial ischemia. The infarct size, patency of the related coronary artery, and renin–angiotensin–aldosterone system (RAAS) influence LV remodeling. For this reason, LV remodeling can be reduced by an antagonist of RAAS. Even aldosterone inhibitors reduce collagen deposition and decrease ventricular arrhythmia development [20].
2.3 Clinical Features
2.3.1 Symptoms
The typical STEMI discomfort is a prolonged (more than 20 min), constricting, oppressing, or compressing pain of variable intensity. It has a retrosternal location and often radiates to the ulnar side of the left arm, or rarely both arms; to the neck, jaw, and shoulders; and rarely to the epigastrium or interscapular region. In some patients, frequently those with an inferior STEMI, the location is the epigastrium simulating abdominal disorders. In these patients nausea and vomiting may occur due to vagal reflex activation or LV receptor stimulation. Symptoms like cold perspiration, palpitations, profound weakness, dizziness, and a sense of imminent death may be present.
In some cases there is an atypical presentation of STEMI-like atypical location of the pain or dyspnea, syncope, profound weakness, or acute indigestion. Some patients are wholly asymptomatic, and STEMI can be unrecognized and discovered in a subsequent routine electrocardiographic examination. These patients have a similar prognosis of symptomatic ones.
In up to half of STEMI patients, a precipitating factor like reduced oxygen supply to the myocardium (hypotension, hypoxemia, pulmonary embolism, etc.) or increased myocardial oxygen demands (aortic stenosis, fever, agitation, tachycardia, emotional stress, unusually heavy exercise) can be identified.
2.3.2 Physical Examination
STEMI patients may appear anxious and agitated. Heart rate varies from bradycardia to tachycardia/tachyarrhythmia, and blood pressure varies from hypotension (patient with right ventricle involvement or cardiogenic shock or low blood pressure acute heart failure) to normotension and even to hypertension due to adrenergic activation.
Fever is present in most patients and resolves within 4–5 days. It is a nonspecific response to tissue necrosis.
Patients with cardiogenic shock or right ventricular infarction infarct have elevated jugular pressure.
Carotid pulse in STEMI patients may be small due to reduced stroke volume. When LV failure develops, rales are audible.
The Killip classification is a prognostic classification dividing STEMI patients according to the presence and severity of heart failure signs:
-
Class I: no rales or third sound
-
Class II: rales in <50 % of pulmonary field with or without third sound
-
Class III: rales in >50 % of pulmonary field (pulmonary edema)
-
Class IV: cardiogenic shock
A third and/or fourth sound may be heard in STEMI patients with severe LV dysfunction that determines elevation of LV filling pressure. When the fourth sound is heard, a corresponding presystolic pulsation is present. Additional systolic murmur (transient/persistent) due to mitral regurgitation as a result of mitral valve apparatus dysfunction may be audible. Along the left and right sternal border, a holosystolic, prominent murmur, accompanied by a thrill, is audible in the presence of interventricular septum rupture. Pericardial friction rubs can be present especially in patients with large infarctions [21]. They are audible along the left sternal border in the first 2 weeks and most commonly on the second or third day.
2.4 Diagnosis
The diagnosis of STEMI starts from symptom assessment: history of chest pain lasting at least 20 min or more; not responding to nitroglycerine is typical.
The confirmation of diagnosis must be completed as soon as possible with a 12-lead ECG, also considering the addition of posterior (V7–V8–V9) or right leads (V4R–V5R, V6R) in patients with high suspicion, respectively, of posterior or right ventricle infarction.
If available, a continuous ECG monitoring should be initiated in all patients to detect life-threatening arrhythmias and allow defibrillation if required.
The diagnostic electrographic sign is a new ST-segment elevation measured at the J point in two contiguous leads with the following thresholds: ≥0.25 mV in men below the age of 40 years, ≥0.2 mV in men over the age of 40 years, or ≥0.15 mV in women in leads V2–V3 and/or ≥0.1 mV in other leads [1]. According to leads involved by ST elevation, the localization of the ischemia is as follows:
-
Anterior MI: V1–V6
-
Septal MI: V1–V4
-
Lateral MI: I, aVL, V5, V6
-
Inferior MI: II, III, aVF
-
Posterior MI: V7–V8–V9 (high R in V1–V3 with ST depression V1–V3)
-
Right ventricle MI: V1, V4R–V5R–V6R
Although not frequently seen, an earlier sign of ischemia could be the presence of hyperacute T waves; later, the ECG alterations evolve in ST elevation in those leads that register the electrical activity of the ischemic myocardium. ST elevation typically presents a concave configuration but over time becomes more pronounced, more convex, and rounded upward. In the absence of reperfusion strategies, the natural evolution of ECG is as follows: the ST gradually returns to isoelectric baseline, there is a reduction of R-wave amplitude with the development of Q waves, and T waves become inverted. The ECG changes usually may take place from few weeks to several hours from presentation.
Moreover, the initial ECG presentation of acute coronary syndrome could be represented by new or presumed new left bundle branch block (LBBB) [1].
The electrocardiographic diagnosis could be more difficult in some categories of patients:
-
Patients with preexistent LBBB: in the presence of intraventricular conduction delay, the diagnosis could be suspected in the presence of concordant ST elevation with QRS or in case of marked ST abnormalities. Two signs are highly specific: Cabrera’s sign, a prominent notching in the ascending limb of S wave in leads V3–V4, and Chapman’s sign, a notching in the ascending limb of R wave in V5–V6 [22]. A scoring system has been developed from the GUSTO-1 trial called Sgarbossa’s criteria [23] but not providing diagnostic certainty.
-
Patients with paced rhythm: in case of clinical strong suspicion, the diagnosis should be confirmed by angiography; reprogramming of the pacemaker with the appearance of intrinsic rhythm and the evaluation of ischemic ECG changes may be considered when feasible.
-
Patients with isolated posterior myocardial infarction: the involvement of the inferobasal portion of the heart may appear as an isolated ST depression ≥0.05 mV in leads V1 through V3. The documentation of ST elevation ≥0.05 mV in the posterior chest wall leads should be treated as STEMI.
-
Patients with left main coronary obstruction: the typical ECG signs are aVR ST elevation and inferolateral ST depression; the presence of ST depression in eight or more surface leads together with ST elevation in aVR and/or V1 suggests ischemia due to multivessel disease or left main coronary artery obstruction.
The following steps are not necessary for the diagnosis; however, they complete the clinical picture of patients with ACS: blood sampling for troponin determination and echocardiography for differential diagnosis and for the assessment of the involved myocardium, left ventricular function, and mechanical complications.
2.5 Therapy
The following recommendations are based on currently accepted European guidelines [1].
Initial therapy of patients with acute coronary syndrome with ST elevation is represented as follows:
-
Oxygen administration in the presence of hypoxia or acute heart failure.
-
Relief of pain and anxiety: IV opioids are very useful, although they must be used with caution for their potential side effects, such as respiratory depression, nausea, vomiting, hypotension, and bradycardia.
The following steps of treatment are related to some crucial aspects: the first one is time from symptom onset and the second one, the availability of a primary PCI center.
Patients with a diagnosis of STEMI within 12 h from symptom onset should be considered for mechanical or pharmacological reperfusion strategy, as soon as possible. Moreover, reperfusion therapy should be taken into account in the presence of ongoing ischemia even if the onset of pain dates back more than 12 h. Primary PCI may also be done in stable patients presenting 12–24 h after symptom onset.
In case of reperfusion strategy, the choice between mechanical and pharmacological methods depends on the availability of a primary PCI center with an experienced team or the time needed to reach the PCI center. PCI strategy is preferred to fibrinolysis when there is a primary PCI hospital or when the transfer to a PCI center could be realized within 120 min from symptom onset. In the other cases, fibrinolysis should be undertaken and followed by consideration of rescue PCI in case of treatment failure or by consideration of routine angiography in all stable patients within 3–24 h.
In case of mechanical reperfusion, only the culprit lesion should be treated with PCI and stenting [24]. Primary multivessel revascularization in addition to the supposed culprit lesion is indicated in case of cardiogenic shock or persistent ischemia, after the culprit lesion treatment [1, 25, 26]. In case of multivessel disease, staged multivessel PCI could be considered as recent meta-analysis showed improvement in short- and long-term survival and reduction of repeated PCI [27]. However, other randomized trials should confirm the benefits of staged multivessel PCI in STEMI.
2.5.1 Primary Percutaneous Coronary Intervention: Pharmacotherapy
The main stones of therapy in acute coronary syndrome are represented by antiplatelet and anticoagulant drugs.
-
1.
Antiplatelet therapy consists of a combination of two antiplatelet agents: the first option is aspirin, both oral and IV, if patients are unable to swallow, and the second one is an adenosine diphosphate (ADP) receptor blocker. For a long time, clopidogrel has been the only and preferred ADP blocker, while in the last years new antiplatelet agents such as prasugrel and ticagrelor have been studied [28, 29] and currently accepted in guidelines and widely used in common clinical practice. Prasugrel and ticagrelor present a more rapid onset of action and higher efficacy when compared to clopidogrel. Therefore, clopidogrel is preferably used when prasugrel or ticagrelor is either not available or contraindicated. Table 1.1 summarizes the main features of old and new antiplatelet agents.
Table 1.1 Old and new antiplatelet agent for acute coronary syndrome The glycoprotein IIb/IIIa (GP IIb/IIIa) antagonists are the most recent additions to the antiplatelet agents available that are given intravenously. Currently, three GPIIb/IIIa antagonists are available: abciximab, eptifibatide, and tirofiban. The role of these agents is debated: in the era of potent oral antiplatelet agents, the upstream use is uncertain; moreover, if bivalirudin is chosen as an anticoagulant, its use does not add further benefits. On the other side, if UFH or enoxaparin is administered, the association of GPIIb/IIIa antagonists remains debatable. Current guidelines suggest the administration of GP IIb/IIIa inhibitors for bailout therapy if there is angiographic evidence of a massive thrombus, slow or no reflow, or thrombotic complication.
-
2.
Anticoagulant therapy in primary PCI-treated patients may be achieved with unfractionated heparin (UFH), enoxaparin, and bivalirudin, with the aim to reduce acute vessel thrombosis risk. Anticoagulants should be started as soon as possible and stopped at the end of PCI procedure, except in the presence of other conditions that require prolongation of anticoagulants, such as atrial fibrillation or mechanical valve or left ventricular thrombosis.
Bivalirudin is a direct thrombin inhibitor, nowadays, recommended by European guidelines over unfractionated heparin and a GP IIb/IIIa blocker (Ib) [1]. As previously reported, when bivalirudin is preferred, addition of GP IIb/IIIa blockers does not add adjunctive benefits, and bivalirudin alone is associated with lower bleeding rates and reduced mortality [32].
Enoxaparin (with or without routine GP IIb/IIIa blocker) may be preferred over unfractionated heparin with a class II of indication, level B; finally, unfractionated heparin with or without routine GP IIb/IIIa blocker must be used in patients not receiving bivalirudin or enoxaparin (I, C) [1].
2.5.2 Fibrinolysis
Fibrinolysis must be considered when mechanical revascularization is not available in recommended timelines [1]. Prehospital treatment with fibrinolytic drugs by emergency medical personnel is strongly suggested, when feasible: the benefits from fibrinolytic therapy are higher in the first 3 h from symptom onset and then rapidly decline [33]. The delay from first patient contact and initiation of fibrinolysis should be within 30 min to improve treatment efficacy, in both hospital and prehospital settings.
There are many absolute and relative contraindications to fibrinolysis, as reported in Table 1.2.
A fibrin-specific agent (tenecteplase, alteplase, reteplase) is recommended (over non-fibrin-specific agents).
Aspirin and clopidogrel must be administered to treated patients. Parenteral anticoagulation is recommended until revascularization (if performed) or for the duration of hospital stay, from at least 48 h up to 8 days. Enoxaparin is preferred over UHF.
Patients treated with fibrinolysis must be transferred to a PCI-capable center: stable patients should be studied within 3–24 h. Rescue PCI is indicated in case of treatment failure (<50 % ST-segment resolution at 60 min), recurrence of ST-segment elevation, or recurrent ischemia. Also patients with heart failure or cardiogenic shock must undergo angiography [1].
2.6 Arrhythmia Management in Acute Phase
Arrhythmias are very frequent in the acute phase of STEMI, and every kind of arrhythmia could be seen [1].
As occurred in our patient, inferior myocardial infarction is frequently associated with bradyarrhythmias, from sinus bradycardia to atrioventricular (AV) blocks. Sinus bradycardia, first-degree AV block, and second-degree AV block type I usually do not require specific treatment; in case of symptoms or severe hypotension, IV atropine should be administered, and if not effective, temporary pacing should be started. All medications interfering with electrical conduction should be withheld. Second-degree, type II, and third-degree atrioventricular blocks usually need temporary pacing, especially if concomitant hypotension or heart failure is present.
AV blocks developing during inferior infarction are usually supra-Hisian and reversible with the restoration of coronary perfusion, and they carry a good prognosis. The ECG shows an escape rhythm with narrow QRS. In case of anterior MI, the presence of an AV block underlines the existence of an extensive necrosis, interesting electrical conduction ways; the block is usually infra-Hisian with a low escape, wide QRS rhythm. A new bundle branch block or a new hemiblock should be highly monitored because they often precede a complete AV block.
Atrial fibrillation is also very common in STEMI patients, especially in the presence of heart failure [34]. Anticoagulation should be started if not contraindicated, and effective rate control achieved in order to reduce myocardial oxygen demand. In case of hemodynamic instability or ongoing ischemia, urgent electrical cardioversion is indicated, while pharmacological cardioversion could be achieved with amiodarone in stable patients with recent arrhythmia onset. For further details on atrial fibrillation management, see Chap. 20.
Ventricular arrhythmias (VA) vary from ventricular premature beats to non-sustained and sustained ventricular tachycardias (VT) to ventricular fibrillation. The prevalence of ventricular arrhythmias has been investigated in the fibrinolytic era [35] and, later, in the primary percutaneous coronary intervention era [36]: VA remain fairly common even if the real incidence may be underestimated because MI resulting in prehospital sudden cardiac death could have not been considered in evaluating studies.
Ventricular premature beats and non-sustained VT are really common in the first days from MI. Treatment is not recommended [1] unless non-sustained VT causes hemodynamic instability.
Sustained monomorphic VT are often not tolerated, especially in the presence of worse left ventricular dysfunction; moreover, they may produce ischemia and degenerate in ventricular fibrillation.
In hemodynamically unstable patients, electrical cardioversion is mandatory. In stable VT, diagnosis and treatment should be prompt because of the risk of rapid deterioration of clinical and hemodynamic conditions. If the patient is stable, IV amiodarone, sotalol, or lidocaine could be attempted, even if conversion rates are low.
For polymorphic VT and ventricular fibrillation, the first therapy consists of immediate defibrillation [37]. If polymorphic VT develop in the setting of bradycardia, a temporary pacing at higher rate should be started.
For further details in the management of ventricular arrhythmias and long-term risk evaluation for sudden death, see Chap. 18.
2.7 Long-Term Therapies for ST-Segment Elevation Myocardial Infarction
Long-term management of patients with acute coronary syndrome with ST elevation consists of lifestyle changes, risk factor control, and long-term drug therapy.
Lifestyle changes are mainly represented by interruption of smoking, diet and weight control, and regular physical activity. Blood pressure should be regularly controlled with the following target: systolic pressure <140 mmHg.
If available, exercise-based rehabilitation is strongly recommended; different studies showed positive effects of cardiac rehabilitation in terms of mortality, reinfarction, and quality of life [38]. Rehabilitation also favors achievement of a better risk factor control and correct titration of accepted therapy, as beta-blockers.
Aspirin therapy is indicated indefinitely after STEMI, or if not tolerated, clopidogrel should be used. The combination of dual antiplatelet therapy is recommended for up to 12 months after STEMI, with a minimum of 1 month for patients receiving PCI and bare-metal stents and 6 months for patients receiving PCI and drug-eluting stent. Dual antiplatelet therapy should be maintained up to 1 year in patients with STEMI who did not receive a stent.
Oral beta-blockers must be introduced during hospital stay and continued thereafter in all patients without contraindications. High-dose statins early after admission are indicated in all STEMI patients without contraindication or history of intolerance, regardless of initial cholesterol concentrations. A target value of <70 mg of LDL cholesterol must be reached, and regularly a lipid profile must be assessed.
Angiotensin-converting enzyme, or if not tolerated angiotensin receptor blocker, is indicated in patients with an impaired ejection fraction (EF < 40 %), with heart failure in the early phase, and with diabetes. However, they may be considered in all STEMI patients for their modest effect on mortality.
Finally, aldosterone antagonists should be considered for patients with at least mild left ventricular dysfunction (EF ≤ 40 %) and heart failure or for diabetic patients, provided that no renal failure or hyperkalemia is present.
References
Steg PG, James SK, Atar D, Badano LP, Blömstrom-Lundqvist C, Borger MA, Di Mario C, Dickstein K, Ducrocq G, Fernandez-Aviles F, Gershlick AH, Giannuzzi P, Halvorsen S, Huber K, Juni P, Kastrati A, Knuuti J, Lenzen MJ, Mahaffey KW, Valgimigli M, van’t Hof A, Widimsky P, Zahger D (2012) ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J 33(20):2569–2619
O’Gara PT, Kushner FG, Ascheim DD, Casey DE, Chung MK, de Lemos JA, Ettinger SM, Fang JC, Fesmire FM, Franklin BA, Granger CB, Krumholz HM, Linderbaum JA, Morrow DA, Newby LK, Ornato JP, Radford MJ, Tamis-Holland JE, Tommaso CL, Tracy CM, Woo YJ, Zhao DX (2013) ACCF/AHA guideline for the management of ST-elevation myocardial infarction. J Am Coll Cardiol 61(4):e78–e140
WHO Fact sheet 310. Updated 2012, http://www.who.int/mediacentre/factsheets/fs310/en/index2.html
Mehta RH, Parsons L, Rao SV et al (2012) Association of bleeding and in-hospital mortality in black and white patients with ST-segment elevation myocardial infarction receiving reperfusion. Circulation 125:1727–1734
Fox KAA, Steg PG, Eagle KA et al (2007) Decline in rates of death and heart failure in acute coronary syndromes, 1999–2006. JAMA 297:1892–1900
Yeh RW, Sidney S, Chandra M et al (2010) Population trends in the incidence and outcomes of acute myocardial infarction. N Engl J Med 362:2155–2165
Mandelzweig L, Battler A, Boyko V et al (2006) The second Euro Heart Survey on acute coronary syndromes: characteristics, treatment, and outcome of patients with ACS in Europe and the Mediterranean Basin in 2004. Eur Heart J 27:2285–2293
Widimsky P, Wijns W, Fajadet J, de Belder M, Knot J, Aaberge L, Andrikopoulos G, Baz JA, Betriu A, Claeys M, Danchin N, Djambazov S, Erne P, Hartikainen J, Huber K, Kala P, Klinceva M, Kristensen SD, Ludman P, Ferre JM, Merkely B, Milicic D, Morais J, Noc M, Opolski G, Ostojic M, Radovanovic D, De Servi S, Stenestrand U, Studencan M, Tubaro M, Vasiljevic Z, Weidinger F, Witkowski A, Zeymer U (2010) Reperfusion therapy for ST elevation acute myocardial infarction in Europe: description of the current situation in 30 countries. Eur Heart J 31:943–957
Widimsky P, Zelizko M, Jansky P, Tousek F, Holm F, Aschermann M (2007) The incidence, treatment strategies, outcomes of acute coronary syndromes in the “reperfusion network” of different hospital types in the Czech Republic: results of the Czech evaluation of acute coronary syndromes in hospitalized patients (CZECH) registry. Int J Cardiol 119:212–219
McManus DD, Gore J, Yarzebski J, Spencer F, Lessard D, Goldberg RJ (2011) Recent trends in the incidence, treatment, and outcomes of patients with STEMI and NSTEMI. Am J Med 124:40–47
Birkhead JS, Weston C, Lowe D (2006) Impact of specialty of admitting physician and type of hospital on care and outcome for myocardial infarction in England and Wales during 2004–5: observational study. BMJ 332:1306
Cheitlin MD, McAllister HA, de Castro CM (1975) Myocardial infarction without atherosclerosis. JAMA 231:951
Achenbach S (2008) Can CT detect the vulnerable coronary plaque? Int J Cardiovasc Imaging 24:311
Fox JJ, Strauss HW (2009) One step closer to imaging vulnerable plaque in the coronary arteries. J Nucl Med 50:497
Manfredini R, Boari B, Salmi R et al (2005) Circadian rhythms and reperfusion in patients with acute ST-segment elevation myocardial infarction. JAMA 294:2846
Schoen FJ (2010) The heart. In: Kumar V, Abbas AK, Fausto N (eds) Robbins & Cotran pathologic basis of disease, 8th edn. WB Saunders, Philadelphia, pp 529–587
Hamon M, Agostini D, Le Page O, Riddell JW (2008) Prognostic impact of right ventricular involvement in patients with acute myocardial infarction: meta-analysis. Crit Care Med 36:2023
Popescu BA, Antonini-Canterin F, Temporelli PL et al (2005) Right ventricular functional recovery after acute myocardial infarction: relation with left ventricular function and interventricular septum motion. GISSI-3 echo substudy. Heart 91:484
Funaro S, La Torre G, Madonna M et al (2009) Incidence, determinants, and prognostic value of reverse left ventricular remodelling after primary percutaneous coronary intervention: results of the Acute Myocardial Infarction Contrast Imaging (AMICI) multicenter study. Eur Heart J 30:566
Konstam MA (2008) Patterns of ventricular remodeling after myocardial infarction: clues toward linkage between mechanism and morbidity. JACC Cardiovasc Imaging 1:592
Dorfman TA, Aqel R (2009) Regional pericarditis: a review of the pericardial manifestations of acute myocardial infarction. Clin Cardiol 32:115
Lopes RD, Siha H, Fu Y, Mehta RH, Patel MR, Armstrong PW, Granger CB (2011) Diagnosing acute myocardial infarction in patients with left bundle branch block. Am J Cardiol 108:782–788
Sgarbossa EB, Pinski SL, Barbagelata A, Underwood DA, Gates KB, Topol EJ, Califf RM, Wagner GS (1996) Electrocardiographic diagnosis of evolving acute myocardial infarction in the presence of left bundle-branch block. GUSTO-1 (Global Utilization of Streptokinase and Tissue Plasminogen Activator for Occluded Coronary Arteries) investigators. N Engl J Med 334:481–487
Kornowski R, Mehran R, Dangas G, Nikolsky E, Assali A, Claessen BE, Gersh BJ, Wong SC, Witzenbichler B, Guagliumi G, Dudek D, Fahy M, Lansky AJ, Stone GW (2011) Prognostic impact of staged vs. “one-time” multivessel percutaneous intervention in acute myocardial infarction: analysis from the HORIZONS-AMI (Harmonizing Outcomes with RevascularIZatiON and stents in Acute Myocardial Infarction) trial. J Am Coll Cardiol 58:704–711
Hussain F, Philipp RK, Ducas RA, Elliott J, Dzavik V, Jassal DS, Tam JW, Roberts D, Garber PJ, Ducas J (2011) The ability to achieve complete revascularization is associated with improved in-hospital survival in cardiogenic shock due to myocardial infarction: Manitoba cardiogenic SHOCK Registry investigators. Catheter Cardiovasc Interv 78:540–548
Mylotte D, Morice MC, Eltchaninoff H, Garot J, Louvard Y, Lefèvre T, Garot P (2013) Primary percutaneous coronary intervention in patients with acute myocardial infarction, resuscitated cardiac arrest, and cardiogenic shock: the role of primary multivessel revascularization. JACC Cardiovasc Interv 6(2):115–125
Bainey KR, Mehta SR, Lai T, Welsh RC (2014) Complete vs culprit-only revascularization for patients with multivessel disease undergoing primary percutaneous coronary intervention for ST-segment elevation myocardial infarction: a systematic review and meta-analysis. Am Heart J 167(1):1–14
Wallentin L, Becker RC, Budaj A, Cannon CP, Emanuelsson H, Held C, Horrow J, Husted S, James S, Katus H, Mahaffey KW, Scirica BM, Skene A, Steg PG, Storey RF, Harrington RA, Freij A, Thorsen M (2009) Ticagrelor versus clopidogrel in patients with acute coronary syndromes. N Engl J Med 361:1045–1057
Wiviott SD, Braunwald E, McCabe CH, Montalescot G, Ruzyllo W, Gottlieb S, Neumann FJ, Ardissino D, De Servi S, Murphy SA, Riesmeyer J, Weerakkody G, Gibson CM, Antman EM (2007) Prasugrel versus clopidogrel in patients with acute coronary syndromes. N Engl J Med 357:2001–2015
Yusuf S, Zhao F, Mehta SR, Chrolavicius S, Tognoni G, Fox KK, Clopidogrel in Unstable Angina to Prevent Recurrent Events Trial Investigators (2001) Effects of clopidogrel in addition to aspirin in patients with acute coronary syndromes without ST-segment elevation. N Engl J Med 345(7):494–502
Mehta SR, Yusuf S, Peters RJ, Bertrand ME, Lewis BS, Natarajan MK, Malmberg K, Rupprecht H, Zhao F, Chrolavicius S, Copland I, Fox KA (2001) Effects of pretreatment with clopidogrel and aspirin followed by long-term therapy in patients undergoing percutaneous coronary intervention: the PCI-CURE study. Lancet 358:527–533
Mehran R, Lansky AJ, Witzenbichler B, Guagliumi G, Peruga JZ, Brodie BR, Dudek D, Kornowski R, Hartmann F, Gersh BJ, Pocock SJ, Wong SC, Nikolsky E, Gambone L, Vandertie L, Parise H, Dangas GD, Stone GW (2009) Bivalirudin in patients undergoing primary angioplasty for acute myocardial infarction (HORIZONS-AMI): 1-year results of a randomised controlled trial. Lancet 374:1149–1159
Morrison LJ, Verbeek PR, McDonald AC, Sawadsky BV, Cook DJ (2000) Mortality and pre-hospital thrombolysis for acute myocardial infarction: a meta-analysis. JAMA 283:2686–2692
Schmitt J, Duray G, Gersh BJ, Hohnloser SH (2009) Atrial fibrillation in acute myocardial infarction: a systematic review of the incidence, clinical features and prognostic implications. Eur Heart J 30:1038–1045
Newby KH, Thompson T, Stebbins A, Topol EJ, Califf RM, Natale A (1998) Sustained ventricular arrhythmias in patients receiving thrombolytic therapy: incidence and outcomes. The GUSTO investigators. Circulation 98(23):2567
Mehta RH, Starr AZ, Lopes RD, Hochman JS, Widimsky P, Pieper KS, Armstrong PW, Granger CB, APEX AMI Investigators (2009) Incidence of and outcomes associated with ventricular tachycardia and fibrillation in patients undergoing primary percutaneous coronary intervention. JAMA 301(17):1779
Neumar RW, Otto CW, Link MS, Kronick SL, Shuster M, Callaway CW, Kudenchuk PJ, Ornato JP, McNAlly B, Silvers EP, Passman RS, White RD, Hess EP, Tang W, Davis D, Sinz E, Morrison LJ (2010) Part 8: adult advanced cardiovascular life support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 122(18 Suppl 3):S729
Lawler PR, Filion KB, Eisenberg MJ (2011) Efficacy of exercise-based cardiac rehabilitation post-myocardial infarction: a systematic review and meta-analysis of randomized controlled trials. Am Heart J 162(4):571–584 e572
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Matassini, M.V., Shkoza, M. (2015). ST Elevation Related to the Site of Coronary Occlusion. In: Capucci, A. (eds) Clinical Cases in Cardiology. Springer, Cham. https://doi.org/10.1007/978-3-319-19926-9_1
Download citation
DOI: https://doi.org/10.1007/978-3-319-19926-9_1
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-19925-2
Online ISBN: 978-3-319-19926-9
eBook Packages: MedicineMedicine (R0)