Abstract
The demographic development in developed western countries entails a dramatic shortage of the health care workforce. Based on census and professional association provided data and projections the amount of this shortage is calculated for the USA and Germany. In best case scenarios we still come to conclusions that, to preserve the medical service level, we need a 30 % to 80 % larger health care workforce. Otherwise the number of Old agers served by one physician resp. nurse skyrockets within 10 to 15 years.Assumptions that enter the model are double checked exclusively coming to the conclusion that apparent easing factors turn out as time bombs or double edged.Of methods presented to match future supply and demand quality assurance, growth and diversification are promising. Consumer Health Informatics is introduced as diversification which can make use of trends in ICT and ease access to otherwise under-served population s.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Health care workforce
- Demographic development
- Prognosis
- Old age dependency ratio
- Rationing
- Health care delivery
1 Introduction
Developed mostly western countries have enjoyed more than six decades without major wars, epidemics, or famines. Populations get older in most of these countries. The phenomenon is almost universal, but its pace and shape differs across countries. With the exception of fading effects of World War Two still visible in 1960, the comparison between the 1960, the 2000 and the extrapolated 2040 age cohort pyramides suggest themselves as displaying intrinsic natural trends of populations in the absence disasters.
The years between 1950 and 1960 have been characterized as the baby boom . Birth rates were higher than death rates, reflecting optimism in a positive future on the one hand and continued medical progress on the other. After the baby boom came the baby bust and is here to stay. At the same time life expectancy has increased at a constant rate of 2 years per decade, with women always ahead half a decade of longer life expectancy for no known biological reason.
As a consequence it has become broadly acknowledged that population pyramides in developed societies are changing their shape. With proportions of older age groups increasing we are permanently confronted with dire prognosis about the funding of retirement pensions and of health care. This chapter will substantiate some of these demographic arguments by providing historical and recent figures and projections. It will, however, put more emphasis on work force than on finance. Concretely, we will analyze how populations have grown and will presumably keep growing or will decline, do the same for the whole work force and the health care work force and will come to observations and projections as to how many individuals in a population used to share, share now and will share in the foreseeable future the services of one physician, one nurse etc. i.e. we will explore several variants of the old age dependency ratio , resp. the more illustrative 1/old age dependency. Since utilization of health care resources is much higher at older ages leaving away young age dependency should not affect the validity of predicting health care services shortage too much. This is also underlined through a leaflet by the American Geriatrics Society at http://www.americangeriatrics.org/files/documents/Adv_Resources/PP_Priorities.pdf which contrasts the requirements for medical and nursing care of young and old people and through [6] which adds to the workload imposed upon the health care system through excess need of the chronically ill.
Under the assumptions that the population development continues along the lines of the past decades and that the organization of health care generally remains the same we will extrapolate that either health professionals will have to serve many more individuals or that a much larger proportion of the working population will have to work in the health care industry. Here finance will be back in the game: in that case a much larger part of the GDP will have to flow into health care.
Take Home
If populations in developed countries keep developing like in the past decades without any major disaster, a scarcity of the work force and primarily the health care workforce is immanent. Methods to substantiate and quantify this prognosis extrapolate from present population and medical industry statistics and census data.
2 Methodological Considerations
Regarding the sizes of the analyzed national economies, the immense variety of data being collected and published, and the inherent imprecision of census and population statistics selections have to be made and achieved results cannot claim to be more than orders of magnitudes and trends. Achieved projections will, however, demonstrate such a clear supply vs. demand deficit that some imprecision in the base data does not invalidate the drawn conclusions. Subsequently we outline and provide argument for the criteria applied to use some and not to use other data and how and why to combine them, trying to point to types of errors that the made choices may entail.
2.1 Criteria to Select Variables
Among the tremendous numbers of potentially useful variables we concentrate on very few. We only cover a time range of 40 years, some more than 20 years into the past and some less than 20 years into the future. We use overall population only i.e. we do not distinguish male-female, ethnicity, religion, education, region and type of residence etc. Within the population we only distinguish three age groups (Young age, Working age, Old age). To characterize the supply of health care we leave all material assets such as hospitals, practices, radiation units etc. and all consumed supply (pharmaceuticals, walking aids…) away. We rather concentrate on those resources that are hardest to multiply or to replace: physicians and nurses. Within the profession of physicians we do not distinguish specialties and we do not address part-time work at all.
2.2 Criteria to Select Nations
Health, diseases, suffering, and health care are universal phenomena. Qualitative aspects of disease and cure such as evolving threats (e.g. multiresistant bacteriae, the obesity epidemic, an increase in stress induced incidence of mental health problems) or evolving opportunities (e.g. minimally invasive surgery, genomic profiling, patient initiated enrollment in clinical trials) are universal but will not be addressed explicitly. However, while many other industries (traffic and transportation, finance, communication etc.) behave globally organization of health care is markedly different across countries. Therefore, trying to average across countries does not make sense. The same applies to age: trying to average across dynamics of aging populations would blur characteristic developments. Therefore, we prefer not to discuss the relation between population dynamics and health care organization with reference to the population of the developed countries as a whole but rather take two representative countries and their dynamics as examples for the following arguments. We try to derive that their national economics each almost inevitably face severe shortage of human resource or – in the unlikely case of dramatic growth of the health care workforce – severe financial demand, if present population developments continue without major interventions.
Two countries have been selected to provide most of the data and arguments for a number of reasons: The United States of America and Germany both have a solid foundation of statistical data but differ somewhat in their population dynamics and differ markedly in their organization and financing of the health care system. Some detail about the difference is supplied in Sect. 17.4 Studying other health care systems goes beyond the scope of this volume.
Publicly available figures about the population development and the quantitative development of the health care industries are retrieved from various sources and finally summarized in Table 2.2.
2.3 Criteria to Select Information Resources
As different as the societies and their health care systems themselves are their reporting authorities. Therefore, absolute figures may not be comparable across countries. However, as long as reporting authorities are used consistently and consequently within each country, at least trends within such as percent increase or percent decrease per unit time should be reliable. As to Germany not even this is easy, because Germany underwent a major turnover in 1988 through 1990 when the two states of Federal Republic of Germany (“West Germany” ) and German Democratic Republic (“East Germany” ) merged (German unification ). German figures from before 1990 are, therefore, based on different polling and reporting structures and should not be used here. Hence, we compare trends from past (1990/1) to present (2008/10), the most recent consolidated data in both the USA and the unified Germany throughout the fields of population, work force, and health care.
Take Home
The USA and Germany are large representatives of very different health care systems. Reliable historical data for Germany are available since after the German re-unification in 1989. Using very coarse segmentation into age cohorts and neglecting all other health care assets and all demographic distinctions we start extrapolations from publicly available figures about the future demand and supply of health care workforce.
2.4 Base Figures and Derived Indicators of Health Care Demand and Supply
We compare the age segments below 20 (“Young age”), 20 through 64 (“Working age”) and beyond (“Old age”) in past and present and extrapolate to future (2025/30). The attributions of the age segments are somewhat arbitrary because some people start working before 20 and the retirement age is increasing in some societies. However, the segmentation and henceforth a certain amount of false attribution is done equally in the USA and Germany. Therefore, the type and amount of imprecision should be similar in both countries.
We use “workforce ” for the share of a population that has or actively seeks paid work. If the age limits of 20 to 65 as “Working age” were sharp the work force figures would have to be smaller than the Working age figures. The actual limits are not sharp and especially the retirement age is moving upward, possibly leading to a larger work force than Working age population. The work force in the USA and Germany has, however, been and presently is between 83 % and 90 % of the Working age, i.e. a certain share of the Working age population does not work or seek paid work.
From retrieved statistics we calculate
-
Persons in the Working age by persons in the Old age; to demonstrate the shift of the base population groups
-
Person in the Workforce by persons in the Old age; to modify for the actual participation rate of the Working age population in the Workforce
-
Physicians per thousand Working age persons; to demonstrate what share of the productivity of a society is devoted to delivering health related services
-
Physicians per thousand Workforce; equally modifying for the actual participation rate
and respectively for nurses.
While the above figures map a society in all its facets we now purposefully and suggestively focus on ratios that overemphasize the effects set through the aging of populations with their expected large share of high utilizers. As base figures (2008–2010) we take
-
the present number of Old agers served by one physician resp. one nurse
-
the present share of the Working age that serves as physicians or nurses.
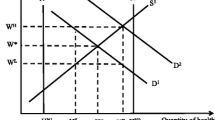
We then elaborate on the following two reciprocal scenarios which reflect two opposing possible courses of future action:
-
Positive formulation, the “Growth scenario”: A proportionally larger health care workforce will be employed to serve a growing share of Old age high utilizers. This will allow to maintain the present quality and coverage. To substantiate the growth formulation we calculate
$$\displaystyle{\left \vert present\;Old\;agers\;served\;by\;one\;physician\right \vert \times \left \vert \,future\;Old\;agers\right \vert }$$resp. for \(\left \vert present\;nurses\right \vert \) where \(\left \vert expression\right \vert \) denotes number of individuals identified by “expression”.
-
Negative formulation, the “Dilution scenario”: The proportion of health care within the overall Working age will remain constant. As a consequence each health care professional will have to care for more Old age high utilizers. To substantiate the dilution formulation we calculate
$$\displaystyle{ \frac{\left \vert \,future\;Old\;agers\right \vert \times \left \vert present\;Working\;agers\right \vert } {\left \vert \,future\;Working\;agers\right \vert \times \left \vert present\;physicians\right \vert }}$$
and respectively for nurses.
With a smaller share of the Working age and a larger share of the Old age it can be expected that either the proportion of health care professionals of the Working age has to be increased (Growth scenario) or the Old-age clients to be served by one health care professional increases (Dilution scenario).
Take Home
By calculating ratios between figures characterizing the demand (mainly Old agers) and the supply (mainly health care workforce) we extrapolate the future demand to supply prognosis under two opposite assumptions:
- Growth scenario :
assumes that the dependency ratios remains as today and predicts the required increase in physicians and nurses
- Dilution scenario :
assumes that the share of physicians and nurses of the Working age remains as today and predicts the future increase in Old agers depending on one physician resp. nurse
2.5 The “Best Case” Strategy of Selection
All figures carry some degree of imprecision and obviously all predictions are at best as reliable as their assumptions materialize. Therefore, we will over again be in the situation to choose between several figures within the likely range. In all such situation we will assume best case scenarios concerning expected shortages. For number of physicians and nurses we will adopt the largest figures projected. If population models vary in their assumption about number of yearly immigrants we will adopt the model with the largest immigration rate, because immigrants mostly are in the Working age and therefore increase the workforce pool. Proceeding like this will lead to projections that characterize the best possible future situation: in the Growth scenario the least required growth and in the Dilution scenario the least extent of dilution. In other words: it can only get worse than the projected figures suggest.
One could argue that worst case scenarios should rather be presented. Of course everybody is free to do so and the methods of data collection and modeling subsequently applied are equally suited for worst cases. However, the best case will already turn out so dire that its figures together with the knowledge that it can only get worse are absolutely alarming.
In an investigation for the Association of American Medical Colleges (AAMC) Atul Grover has collected a number of arguments relating to the physician workforce why we indeed have to anticipate that it will get worse [7]. They address both the supply and demand side. On the supply side they include the following arguments which leads to lower supply of physician work:
-
1.
The physician age pyramid itself is not a pyramid but rather has largest numbers in age groups that approach retirement
-
2.
The willingness to retire early is large
-
3.
The enrollment to medical school s has kept declining
-
4.
The percentage of female physicians is continually rising which makes the likelihood of periods of maternal leave and the choice for part-time work also rise
-
5.
Only a minority would wish to work more for more money while the majority would like to reduce working hours .
Without going into detail the above effects numbered 1, 4, and to a lesser extent 3 hold for Germany as well.
These arguments about internal mechanisms that reduce actual supply of physician work hours superimposing the raw numbers of trained physicians are complemented by arguments of likely increased demand that has other causes than aging of the population. For the United States the largest potential of increased demand depends on the development of health insurance for those who are presently not insured.
Take Home
The raw figures achieved in the model 2.2.4 most likely underestimate the immanent problems because the estimated physician head counts excludes the effects of
the aging physician population
an increasing share of female physicians with their likely consequences of maternal leave and part-time work
reduced working hours in general
declining enrollment to medical schools
3 Sources and Results
3.1 The USA
3.1.1 Sources
US population data mostly are from Censusscope , a university institute for demographics and population studies which also makes animated population pyramid s through several decades available at http://www.censusscope.org/us/chart_age.html. US work force data are taken from the report [11] available from the Bureau of Labor Statistics at http://www.bls.gov/emp/ep_pub_labor_force.htm. US physician historical data have been taken from the AMA site at http://www.ama-assn.org/resources/doc/clrpd/2008-trends.pdf [2], while for the future development reports and projections provided by the Association of American Medical Colleges (AAMC) appear like a well researched resource although it obviously is AAMC’s role to lobby for an increase in physician workforce (https://members.aamc.org/eweb/upload/The%20Complexities%20of%20Physician%20Supply.pdf, [3]). Nurse supply and projections have recently been reported in a scholarly article by Auerbach and coworkers [1]. A crisp assessment of the upcoming problems can also be found in [10].
3.1.2 Results and Projections
For the United States population growth is expected to persist until 2030, with an overall increase from 248.6 to 365.7 million people. This roughly 47 % increase is unequally distributed through the age groups: Young agers and Working agers increase by one third while Old agers more than double from 31.2 to 71.6 million. The predicted development of workforce nearly equals the predicted growth of the Working age segment of the population. Health care professions growth outperforms the workforce growth. For physicians the expected increase over 40 years is 41 % and for nurses 254 %.
From these base figures we can derive that the Workforce to Old age ratio declines by nearly 41 %. While in 1990/91 4.09 individuals were there for one Old ager, it will be as few as 2.42 in 2030. The physician share of the work force increases by approximately 5 % while the nurse share of the workforce nearly doubles (11.70 in 1990 vs. 21.88 in 2030 of 1000 workforce).
Coming to figures that point out demand and supply of the most needy – the population of Old agers – we find that in 1990/91 one physician worked for 50.7 Old agers while according to figures from the above sources and straight projections he will be working for 82.3 Old agers in 2025. Under the dilution scenario assumptions where we assume that the share of the physicians in the workforce remains constant while the workforce itself declines one physician will have to work for 97.5 Old agers, that is nearly twice as many as 40 years earlier. Official figures from nurses are less alarming: indeed does the number of Old agers served by one nurse decrease moderately from 20.9 to 18.9, while in our Dilution scenario it increases to 25.6. Our Growth scenario requests 1226.4 thousand physicians while AMA predicts 869.9 thousand. This discrepancy goes into the same direction as a shortage predicted by AMA at http://www.ama-assn.org/ama/pub/news/news/strengthen-physician-workforce.page of 124,000–159,000 physicians by 2025. For nurses our Growth scenario requests exactly the same figure required for 2030, namely 3785 thousand.
3.2 Germany
3.2.1 Sources
Germany has had a comprehensive and all encompassing population registration and intermittent censuses introduced through the Prussian emperors in 1876 which continued into both post World War II Germanies and the unified Germany and provides highly reliable data except for the often overlooked effect of individuals moving to an abroad where they need not register as “immigrants” and hence do not notify local authorities about their emigrations. This often applies to guest workers from European Union states when they retire and return to their home countries. The primary national resource to collect and present such data is the Statistische Bundesamt with its web resource destatis , comparable to the US Census Bureau UCB. At https://www.destatis.de/bevoelkerungspyramide/ (a resource in German where bevoelkerungspyramide stands for population pyramid) offers a configurable panel that displays the age distributions of the German population from 1960 to 2008 and extrapolates until 2060. Of course, for the extrapolations assumptions must be made. Destatis offers four variants that vary by birth rate (number of children per woman, from 1.2 to 1.6), life expectancy at birth in 2060 (male: 85.0 to 87.7, female 89.2 to 91.2) (im-)migration surplus (100,000 to 200,000). The best case is high birth rate, low life expectancy , high immigration , because birth and immigration mostly add prospective or actual Working age individuals, while low life expectancy removes Old agers from the equation.Footnote 1
German labor statistics come from Institut für Berufs- und Arbeitsmarktforschung, a research institution affiliated with the Bundesagentur für Arbeit (similar to the US Bureau of Labor Statistics). At http://doku.iab.de/kurzber/2011/kb1611.pdf [4] they provide historical data and projections into 2030 and beyond which can be varied by a few assumptions. These include reproduction rate and immigration figures.
Statistics on individuals with the academic qualification of a physician can build on data from Federal State Medical Association s. When a student has graduated from medical school he becomes a compulsory member and is inevitably registered at his Federal State Medical Association and remains registered for the rest of his life, whether he practices or not. When he moves membership automatically transfers to the new Federal State Medical Association. Compared to the US licensing where physicians can be and often are licensed in more than one state or may lose and later regain their license this means that German figures should be highly reliable.
Statistics on actively practicing physicians draw on two sources. Physicians in private practices are contracting with a social insurance reimbursement structure (Kassenärztliche Vereinigung ) that geographically mirrors the Federal State Medical Associations. With the exception of very few physician who only treat patients that pay from their own purse or have a private rather than the social health insurance, this fully maps practicing medicine outside hospitals and figures are available from the Kassenärztliche Vereinigung. Physicians working in hospitals are reported through employment data of hospitals and always have a certain delay and noise due to part time vs. full time, how physicians organize their work and hence whether they are contracting with exactly one such organization or attending to more than one hospital.Footnote 2
In Germany the Federal Ministry of Health maintains the “Gesundheitsberichterstattung des Bundes ” (“Federal Health Monitoring System”, ) [5] which acts as an authority steered by the Robert-Koch-Institut (comparable to the US Center for Disease Control, CDC ), and the German Federal Statistical Office (comparable to the US Census Bureau, UCB) and assembles figures from the above primary sources to provide comprehensive reports on health and health care delivery.
The physician statistics date back to 1990, with a sharp increase owed to German unification from 1990 to 1991. To avoid the risk of badly supported figures of the period of transition we start in 1991 and compare to 2009. For physician and nurse figures mid-range projections are not available. Therefore, we use linear extrapolations from the data available for 1990/1 and for 2008/9 as a very approximate replacement. Respective figures and others derived on their bases are in italic fonts in Table 2.2.
3.2.2 Results and Projections
German population peaks at 81.7 million in 2008/9 and is expected to decline to 80.2 million in 2030, almost precisely back to the figure of 1990/1. Young agers and Working agers decline by 17 % respectively 14 % from 1990 to 2030 while Old agers increase by 87 % from 11.9 to 22.3 million between 1990/1 and 2030.
Expectations about workforce differ a lot from population development figures. A decrease from 42.9 to 41.0 million over 40 years – which is only 4.5 % – contrasts to the above-mentioned 14 % decrease in the Working age. Arguments in support of this higher participation rate are that more females would seek and find paid work and that retirement ages are already increasing. The latter strictly speaking is not a participation effect but an expansion of the pool from which workforce is supplied. If the assumption that more females participate materializes it is likely to amplify another critical aspect of the population statistics. Unless sophisticated financial and organizational models of care for minors become available those females who work will mostly not be mothers and will bear no or fewer children. For a longer range perspective this first reduces the Young age cohort and 20 years later the Working age cohort.
Physician and nurse figures have developed very differently. While physician figures have increased to a similar extent as in the United States and are extrapolated to grow from 242.2 to 403.5 (32 %) in 2030, the nursing workforce will decline from 913.4 towards 844.0 (thousand FTE each). This unique strange sizing of the two major professions in the German medical industry is to some extent owed to the fact that medicine is an academic while nursing to the most part is a nonacademic profession here which lends nurses less workplace and lobbying power than physicians. On the other hand it leads to physicians being seen by patients for various purposes where nurses legally offer services in many other countries (such as medication refills, wound primary treatment, …). Germany has an amazingly high yearly frequency of patient visits to doctors of appr. 14.
The German workforce to Old age ratio declines by dramatic 49 %. In 1990/1 it was 3.61 and official agency projections predict 1.84 in 2030. During the same time interval the share of physicians of the workforce partially compensates for the decline as it increases from 5.69 to 9.84 (per thousand workforce), while the share of nurses remains nearly constant, reaching 20.58 in 2030.
The analysis focusing on demand and supply with respect to the growing Old age populations and straight projection from public resources finds that one physician will serve 55.3 Old agers, one nurse will serve 26.4 in 2030, from 48.7 respectively 13.0 in 1990/1. Assuming the Dilution scenario one physician will serve 78.0, one nurse will serve 29.0 Old agers. In the Growth scenario Germany will require 430.0 thousand physicians and 1158.3 thousand nurses in 2013, an apparently moderate 16.5 thousand more physicians and an apparently alarming 314.3 thousand more nurses than extrapolated. The projection of both physicians and nurses are, however, badly supported by evidence. The extrapolated number of physicians is likely to overestimate the true development. The 1990/1 and 2008/9 figures from which the linear extrapolations was made, represent a 2008/9 physician workforce age pyramid with overweight in the age groups beyond 50, hence a large number of practicing physicians retiring in the interval of prediction. At the same time enrollment to medical schools is lower now than a decade ago and the political pressure to finish the curriculum in time – and hence to save teaching resources – is higher than the pressure to create more study opportunities. Furthermore, from first enrollment to licensing as a General Practitioner or medical specialist takes at least 11 years in Germany. Opening (yet to be built) new medical school s in 2015 would not help until 2026. Education of licensed nurses is much shorter. That is why politics can achieve more short-term effects when the need for more nurses becomes acknowledged.
3.3 US: German Differences
The most notable difference between the two economies is that the USA all in all have a solid growth situation fueled through nearly sustainable birthrates and an active immigration policy directed at skilled young people. In contrast, Germany is on the verge of decline. Even in the most growth prone variant of the population pyramid by destatis Germany will keep losing 2 million per decade after 2030. No wonder, because Germany’s birthrate is far below sustainable and Germany only tolerates some random influx from poor countries and some asylum seekers.
Another difference which is not so remarkable in figures today is that German statistics still believe in an unrealistically high participation rate of their Working age in the workforce as a welcome measurable productivity indicator of the national economy. While the US prediction holds a hidden reserve of more than 25 % (173 million of 199.2 million working) and therefore maintain a social fabric of continuously available individuals for family work and volunteer assistance in local or national situations of immediate need Germans believe to see more than 95 % barred in work contracts with foreseeable frictions when children want to be brought up or emergencies hit.
The third notable difference between the two economies is the difference between the medical and nursing contributions to health care. While in the USA the medical contribution grows so slowly that future physicians become responsible for an unsurmountable number of elderly patients, the US nursing contribution grows much faster, but when comparing the 2009/10 figure of 15.4 versus the Dilution scenario predicted 25.6 elderly being taken care of by one nurse is still alarming. This reduction of care provision by 40 % is similar to the German one of 34 %, and precisely the same figures of reduction hold for physicians. The details are presented in Table 2.2.
Take Home
Even in best case scenarios, i.e. with all necessary assumptions made so as to overestimate future supply and to underestimate future demand, health care faces severe shortage or requires a dramatic increase in workforce, as summarized in Table 2.1.
3.4 Challenging the Assumptions
One can of course challenge the assumptions made as actually being best case. One challenge is to argue that a higher percentage of the Working age can actually be available as workforce because reproduction rate s are declining and hence fewer Working age individuals will take parental leave . This may be correct, however, it delays the problem by 20 years rather solving it, as already outlined in Sect. 2.3.2.2.
Another challenge to the modeling assumptions is that the increased need of care towards the older end of the population is compensated for by a lower need of the Young age and Working age segments of the population because these segments get smaller. This is true to some extent. However, the absolute figures in the Young age population are already now smaller than the Old age figures. Altogether, both, Young agers and Working agers utilize health care less than Old agers. Therefore, the potential reduction is likely to be overcompensated by the increase requested by the Old agers.
It can also be argued that the Working age segment becomes larger because retirement age s are becoming higher. This is actually already the case. However, we are talking about a couple of months, maybe 2 or 3 years of increased retirement age at most. Therefore, even if we assume that these higher ages fully materialize in the sense that workers indeed sustain their individual workforce for three more years while staying as healthy as the rest of the Working age population we add a segment of 3 years to the Working age which in the model is 45 years, which is 7 %. Compared to that the increase required according to Table 2.2, Growth scenario, is between 32 % (German physicians) and 80 % (German nurses), with US figures in between, i.e. by far too large to be outweighed by higher retirement age. Other observations for Germany further invalidate the argument.
The following argument is double edged: More Working agers may be involved in caring for elderly family because of the shortage of qualified professionals and increasing fees. The undeniable moral responsibility to care for family may withdraw additional qualified workforce hence thus adding to the problem in a self reinforcing loop. The reverse may also be the case: With professional care for the elderly readily available qualified individuals may seek or maintain professional employment hence further reducing the size of the problem. It is up to us to make a choice.
Take Home
Developments that come to mind as being able to ease the dire prognosis either delay the problems or have side effects that aggravate them.
4 Options to Match Supply and Demand
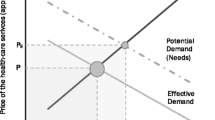
From the analysis above it should be clear that health care delivery faces severe shortages in less than one generation in the future when no action is taken. Believing today that an unchanged health care system will provide equal or better treatment than we have it today for equal or longer duration than today is wishful thinking. The opposite is the likely case. We therefore introduce several paths of action that the health care systems can take and briefly evaluate their prognosis. When it comes to finance more detail can be found in Chap. 16 For all the following consideration the caveat should be in the readers mind that health care is not an open market . Increasing demand will not entail increased supply naturally for at least two reasons. First, the purchasing power of those in need is often insufficient to pay the prices that would cover the providers’ cost. Therefore, not until insurance coverage is (nearly) all encompassing is there a business model for growth of the health care industry. Second, the lag time between increasing demand and increased supply is at least three plus seven years: three for building and staffing new medical schools and seven for short university and specialty training curricula. And like the financial markets – where we should have taken action before major actors collapsed – we should initiate fundamental changes early enough. We should have them in place before scores of health care professionals retire early or are burnt out, overwhelmed by continuously growing demand.
4.1 Rationing
Principally available services can be offered to some and denied to others. Criteria about whom to serve and whom not to serve can be diverse. The most clear-cut criterion is age: upper age limits are defined for services in general or varying by service. Harder to pinpoint criteria are merit and need. Persons can be eligible in their order of merit for the society which now pays back. Persons can be eligible in their order of need, that is a society acknowledges the severity of a problem without premises. Services can also be attributed to those who can pay as long as they can pay. This criterion can be modified as to servicing those who have sufficient insurance coverage. Whether such criteria satisfy the moral principle of distributive justice (cf. Sect. 17.11.7) may also be doubted and even if they would, determining a strict order of merits, needs etc. requires additional time and effort that we do not really want to invest.
None of these criteria are fully satisfactory and hence rationing is not something desirable but rather a backdoor when resources are just not there. In the above ways criteria are made explicit and transparent and can be subject of democratic decision-making. They become law and when the situation is there a health care professional can deliver or deny services by referring to that law rather than being seen personally responsible for a denial. Rationing can also be called reduced allocation of resources. It happens on all levels of the health care system by decisions of building or closing hospitals, by hiring or not hiring staff, and by offering or denying services. It already silently happens whenever a patient seeks hospital service and is turned away because the hospital is fully occupied. This is a rationing that just happens, accidentally, unregulated, and which only reaches the attention of jurisdiction when life-threatening situations are not handled properly. With numbers of clients continuously rising and numbers of professionals not rising it will just happen more and more often as time passes.
Criteria can be experimented with in a democratic process. However, pressure group interests can force whole societies into criteria that hurt other pressure groups’ interests. Regarding the ever-increasing number of elderly age rationing may be opted out although it is the easiest to apply criterion, requiring and allowing the least deliberation.
Take Home
Rationing is a euphemistic expression for denying services to some in need. It is neither desirable nor easy, because criteria and processes for rationing are anything but easy to formulate and to implement.
4.2 Volume Increase at Equal Cost, with Quality at Risk
Volume increase without increasing resources is also called rationalizing. Its underlying assumption is that the same effect can be achieved with less effort. Since most medical interventions include care provider – patient encounters and care provider time cannot be split or multiplied rationalizing likely means shorter care provider – patient sessions. There is certainly potential through more structured processes, better preparation and presentation of patient data, and leaving away all communication that is not related to the medical case. It is a less humane service but when having to choose one would probably prefer some service to no service at all. The more severe risk of the rationalizing approaches is that it can be done once or twice or maybe three times and with every step the service runs thinner. But unless we take the human fully out of the equation there is a lower limit of a meaningful care provider – patient encounter. Operating in the vicinity of this lower limit increases the risks of overlooking critical signs or identifying favorable therapy options. In other words: quality of the service is at stake.
Take Home
Rationalization is an euphemistic expression for reducing effort while hoping to maintain quality. The largest proportion of health care effort is provider – patient contact times. If this is continually reduced errors are a likely consequence.
4.3 Reduced Effort per Case Through Quality Improvement
David Bates and his coworkers at Brigham and Women’s Hospital in Boston have provided conclusive evidence of astounding reduction of efforts by consequently applying CPOE Footnote 3 in a system that backed up by comprehensive decision support and alerting functionality [9]. Over 10 years they showed that for an investment of $ 11.8 million they could collect a return of $ 26.2 million. Among the largest savings were decreased length of stay through renal function adapted dosing, nurse time in providing medication administration records, fewer ADE ’s etc. These three of the top four dollar savers are directly related to reduced human resource utilization. Although not explicitly stated a decrease in ADE’s also means a reduction in work effort. In other words: the savings they can make due to quality improvements to a large extent are reduced workloads. The amount of savings reported here is in the order of magnitude of the shortage predicted above. So is this the solution to all our problems?
It certainly is an important step into the right direction. At Brigham and Women’s they avoid many medical errors and save many lives. Most likely they still have some ADE’s, and they keep trying to reduce them. But when there are no more ADE’s, there are still patients to treat. Quality improvement approaches reduce efforts but this effect reaches a saturation. When saturation is reached the problem of increasing demand is still there, meeting a better prepared supply, though.
Take Home
Structures and processes to warn of errors before they happen are a worthwhile endeavor to achieve better outcomes for patients and at the same time to reduce effort. This should be a permanent undercurrent but it does not solve the problem of shortage to its full extent.
4.4 Growth
Growth is certainly an option. In Sect. 2.3 the required amount of growth has been outlined. It has been pointed to the fact that investment cycles to increase the medical workforce are extremely long. But after all investing into the medical industry to a major part means investing into local jobs rather than jobs abroad as they often materialize when investing into technology or less demanding or less personal services. Growth necessitates a larger amount of the GDP flowing into the medical industry. This is a likely roadblock regarding all the public uproar about the necessity to curb health care cost. Some scholars, however, go against the tides: Hall and Jones [8] use arguments of perceived marginal value of spending for health care and of spending for non-health goods and services in the USA to predict an increase of 33 % by 2050; not too far from what we find in Sect. 2.3.3 especially when regarding a widely expected slower growth of the population.
Take Home
Although politically unthinkable to some, allowing the health care system to grow is not primarily a cost factor for an economy: It rather boosts a high end mostly domestic labour market rather than exporting jobs.
4.5 Diversification of Delivery
Three directions of delivery diversification will be presented:
-
Employing less qualified or differently qualified personnel or machines
-
Intensely using data in preparation and execution of patient – professional encounters
-
Automated diagnosis and treatment
We already see for instance in Great Britain that nurses take far ranging responsibility in medication refills. In Germany psychologist s with additional elements of clinical education can fully responsibly treat psychiatric patients. So why not give dietitian s, physiotherapist s, optometrist s and other paramedical profession s full responsibility for their diagnosis and treatment? We also already face and maybe enjoy that hotel services in hospitals are provided through hotel personnel rather than nurses. We see robots transporting all kinds of material in hospitals and other places. Why not let them transport patients within the hospital.
The more complicated a case the more important are comprehensive data and their presentation in well intelligible form. It starts with making them available for asynchronous assessment allowing the physician to take a look at not so busy hours. E-mail as means of communication has already found a place in many physician-patient relations. Furthermore, information management and processing like summarizing of patient data before a patient visit could help the physician to concentrate on the essentials. Of course signs may be overlooked because they do not fit the criteria of the summarizing software. We also see telemedicine in operation allowing the best specialized individual to offer his service through the distance rather than relying on local capacities that are not able to find the right diagnosis or therapy or need too much time and effort. We see various ways to let the health care professional – mostly the physician – act more efficiently but he is still personally actively involved case by case.
When searching the Internet we can enter symptoms, diseases, drug and treatment names, names of hospitals or physicians and will most likely find some, maybe an overwhelming amount of information. If we correctly describe our problem, select an appropriate information source and understand the information we may know how to proceed: wait, treat ourselves, maybe purchase pharmaceuticals online, see the right specialist. We also already see depression, obesity, and other questionnaires on the internet allowing us to get an idea how severe our problem is. Without immediate involvement of the medical professional we can undergo triage and screening to help us decide whether we should seek professional advice. For various conditions we already find full-fledged treatment programs on the internet or other communications media. We receive treatment without a human being being a step-by-step provider. We may receive alerts to seek professional help when our problem escalates. This takes the health care professional almost entirely out of the operational loop and assigns him a role of developer or back-end service provider “behind” an online service. This diversification requires an investment in health care professional and other resources up front. When gone life it takes off workload because many encounters between professional and client are replaced by advice available online. From the perspective of managing their personal workload physicians should therefore be enthusiastic about investing into Consumer Health Informatics services. Of course, various other aspects play a role here, many of which will be addressed in the rest of this volume. But in the sense of taking preventive action before being overwhelmed by a continuously rising number of patients Consumer Health Informatics should be regarded as an option.
This also diversifies among the prospective clients: it can be the better educated who benefit most because they better understand provided guidance. It can as well be under-served populations in remote places, uninsured persons, who would not have access to medical services at all unless they are openly available through communications media. And we should not leave Old agers out of consideration. The Old agers we are preparing for are the mid-fifties of today, many of them computer savvy. Empirical evidence mainly in Chap. 11 demonstrate that many affected Old agers of today not only manage but appreciate being supported and safeguarded through technical means. Other evidence in sections such as Sect. 3.2 exists as well, though, which indicates that respective patient behaviors are not always rational.
Take Home
Diversification comes through
giving paramedical professions more responsibility
involving non-medical professions for mundane services
employing ICT to enable the patient to become active
The latter is the call for Consumer Health Informatics. Health care professionals can see it as a preventive measure to build good Consumer Health Informatics services before the whole industry is overwhelmed with ever more patients per provider.
5 Benefits from Growth in Other Industries and Segments
Needless to say that all such concepts and developments benefit massively from information and communication technology that develops fast all around us. Be it the masses of data available on servers and in cloud s which are ubiquitously available through fast Internet or mobile communication services. Be it the methods to make communication in open nets safe against intruders. We may think of ever more broadly available smaller and smaller high-quality devices such as smartphones or tablets. Many of us already use sensors attached to the body to track sports activities and GPS to localize ourselves. We are surrounded by surveillance cameras, motion detectors, acceleration detector s etc. This is all happening and sustained through business models of micro-payment, lifestyle and entertainment triggered purchasing power , support of business processes etc. Most of the devices we carry and the services we use are idle most of the time. Unless we need very specialized sensors, extraordinarily high resolution of images, extremely high availability, we can transport medical “payload” through an infrastructure that is already in place.
These considerations gain further attraction through the fact that – although presently they are still behind – developing countries and under-served population s catch up fast in terms of availability and command of up to date information and communication technology. Messages circulate which bemoan that there are now more working cell phones than working toilets on planet Earth and proclaim better sanitation as a major development goal (http://newsfeed.time.com/2013/03/25/more-people-have-cell-phones-than-toilets-u-n-study-shows/). It goes without saying that hygienic sanitation is an urgent need. But these same messages also support that technological and infrastructure barriers for the underprivileged to benefit from available services are dwindling.
Take Home
Many technical enablers for Consumer Health Informatics are developing fast. ICT infrastructures and ubiquitous devices are being used for lifestyle and entertainment purpose, mostly not exploiting bandwidth and processing power. They are right there as a bandwagon waiting for medical services to be added. Patients can make choices, including otherwise under-served populations who are getting access at considerable pace.
Notes
- 1.
This should by no means be taken sarcastically; it is just to illustrate the effects of assumptions made as clearly as possible.
- 2.
In Germany there is no one-on-one matching structure for the US licensing and license renewal process. Physicians in own private practices are obliged to provide proof of a certain amount of CME taken per 3 year interval to preserve their contract with the social insurance system. Hospitals have QA programs part of which target at qualification of employed physicians.
- 3.
Computerized Physician Order Entry, also Computerized Provider Order Entry: ordering medications or diagnostic or therapeutic procedures online; in advanced implementations combined with an electronic record system where contraindications or interactions of new orders with the present patient medication or condition can be checked and alerts can be issued.
References
Auerbach DI, Buerhaus PI, Staiger DO. Registered nurse supply grows faster than projected amid surge in new entrants ages 23–6. Health Aff. 2011;30(12):2286–92. doi: 10.1377/hlthaff.2011.0588
AMA. Health care trends 2008. http://www.ama-assn.org/resources/doc/clrpd/2008-trends.pdf, 2008. 121p.
Dill MJ, Salsberg ES. The complexities of physician supply and demand. https://members.aamc.org/eweb/upload/TheComplexitiesofPhysicianSupply.pdf, Nov 2008. 90p.
Fuchs J, Söhnlein D, Weber B. Projektion des Arbeitskräfteangebots bis 2050, (in German). http://doku.iab.de/kurzber/2011/kb1611.pdf, Aug 2011.
Federal Health Monitoring System GBE. http://www.gbe-bund.de/. Accessed 20 May 2011: search string: “employment 2006”.
Gulley SP, Rasch EK, Chan L. It we build it, who will come? Working-age adults with chronic health care needs and the medical home. Med Care. 2011;49(2).
Grover A. Physician workforce issues. http://michigan.gov/documents/healthcareworkforcecenter/WayneStatePresentationGROVER_192782_7.pdf, Mar 2007.
Hall RE, Jones CI. The value of life and the rise in health spending. Q J Econ. 2007;122(1):39–72. doi: 10.1162/qjec.122.1.39.
Kaushal R, Jha AK, Franz C, Glaser J, Shetty KD, Jaggi T, Middleton B, Kuperman GJ, Khorasani R, Tanasijevic M, Bates DW. Return on investment for a computerized physician order entry system. JAMIA. 2006;13(3):261–6. doi: 10.1197/jamia.M1984.
Sade RM. The graying of America: challenges and controversies. J Law Med Ethics. 2012;2012(Spring):6–9.
Toossi M. Projections of the labor force to 2050: a visual essay. http://www.bls.gov/emp/ep_pub_labor_force.htm, 2012. 14p.
Author information
Authors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Wetter, T. (2016). Economy 1: Immanent Mismatch Between Demand and Supply of Health Care Workforce. In: Consumer Health Informatics. Health Informatics. Springer, Cham. https://doi.org/10.1007/978-3-319-19590-2_2
Download citation
DOI: https://doi.org/10.1007/978-3-319-19590-2_2
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-19589-6
Online ISBN: 978-3-319-19590-2
eBook Packages: MedicineMedicine (R0)