Abstract
A thyroid enlargement, i.e., a goiter, may be due to many causes both congenital and acquired and could be detected at any age during childhood and adolescence. Goiters can be diffuse or nodular and associated with normal or altered thyroid function. The most common pediatric thyroid diseases in which the goiter can represent a clinical feature were discussed. The goiters were also defined according to the age of presentation (neonatal goiters and goiters in children and adolescents). Lastly, an algorithm for the diagnostic approach to the most common causes of diffuse goiters in the pediatric age was presented.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
14.1 Introduction
A thyroid enlargement, i.e., a goiter, may be due to many causes both congenital and acquired and could be detected at any age during childhood and adolescence. Goiters can be diffuse or nodular and associated with normal or altered thyroid function. The thyroid enlargement may be caused by increased TSH secretion acting as growth factor, by TSH receptor stimulating antibodies or by a TSH-independent process, such as inflammation or neoplastic or infiltrative disease. The relative frequency of the various forms varies according to the age [1]. Table 14.1 shows goiter’s classification according to congenital or acquired causes.
14.2 Thyroid Volume (TV) in Childhood and Adolescence: Normative Data
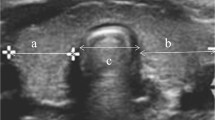
The availability of normative data is essential for goiter diagnosis, in particular in epidemiological studies to establish the goiter prevalence in school-age children as an indicator of iodine intake in a country [2]. Today, the measurement of TV by ultrasound is a validated technique used for grading goiter. Nevertheless also with this method, it is hard to establish globally valid reference intervals for TV due to differences in genetic and environmental factors. In 2004, the WHO and ICCIDD proposed new international reference values for TV by ultrasound in 6–12-year-old children living in six areas of long-term iodine sufficiency on five continents [2]. The median TV increased with age from 1.6 to 3.3 ml, but the differences found between regions suggested that population-specific references in different countries may be more accurate. TV increases significantly with other anthropometric variables, in particular body surface area (BSA). In an extensive study on 859 prepubertal Danish children from an iodine-sufficient area, the GH/IGF1 axis was found positively correlated with thyroid size, suggesting a role in the regulation of thyroid growth [3]. In a cross-sectional survey of 937 Dutch schoolchildren aged 6–18 years, TV increased with age, but a steep increase has been observed at different ages in girls and boys coinciding with pubertal peak of height velocity [4]. In newborns, it is even more difficult to establish normative data, due to both greater technical difficulties and possible influence of maternal factors (iodine intake, smoking in pregnancy). The few studies in the literature are conflicting, with mean TV value varying from the Belgian value of 0.84 to the Scottish value of 1.6 ml [5].
14.3 Congenital Goiters
The causes of congenital goiters are sometimes hereditary, and usually only the most severe forms may be evident at birth. Different disorders lead to congenital goiters (Table 14.1).
14.3.1 Dyshormonogenesis
These genetic defects in each step of synthesis of thyroid hormones (TH) are inherited as autosomal recessive traits. Clinical manifestations comprise a variable degree of congenital hypothyroidism (CH), with increased secretion of TSH and goiter. Occasionally, these disorders can be identified prenatally, when a fetus with goitrous nonimmune hypothyroidism is diagnosed in a euthyroid mother. Intra-amniotic injections of L-thyroxine have been reported to decrease the size of the fetal thyroid gland. However, experience with this procedure is limited, and the risk of provoking premature labor or infections should be evaluated with care by multidisciplinary specialist teams [1, 6–8]
Actually, these defects may be detected by newborn screening and include
-
Iodide transport defects (ITD), caused by impaired Na(+)/I(−) symporter (NIS)-mediated active iodide accumulation into thyroid follicular cells. Low to absent radioiodide uptake at scintigraphy represents the diagnostic tool. Hereditary molecular defects in NIS have been shown to cause ITD [9].
-
Iodide organification defects (IOD) due to thyroid peroxidase (TPO), dual oxidase 2 (DUOX2), and the DUOX maturation factor 2 (DUOXA2) gene inactivating mutations. TPO is a heme-binding protein localized on the apical membrane of the thyrocyte, and TPO enzymatic activity is essential for thyroid hormonogenesis. Currently, 61 properly annotated mutations in the TPO gene have been reported, of which the majority are missense mutations [10]. Hydrogen peroxide (H2O2) is the substrate used by TPO for oxidation and incorporation of iodine into thyroglobulin (Tg), a process known as organification. The main enzymes composing the H2O2-generating system are DUOX2 and DUOXA2. Affected patients show a positive perchlorate discharge test and high phenotypic variability, ranging from transient to permanent forms of CH. Up to now, only two cases of CH due to DUOXA2 defects have been published. The phenotypic expression is probably influenced by genetic background and environmental factors. DUOX and DUOXA constitute a redundant system in which DUOX1/DUOXA1 can at least partially replace the function of DUOX2/DUOXA2. Furthermore, increased nutritional iodide could ensure a better use of H2O2 provided by DUOX1 [11]. To identify IOD, a 123I scintiscan with KClO4 discharge test should be performed. A 123I discharge >90 % of the basal uptake measured 2 h after 123I administration is typical of total IOD, while discharge ranging 10–90 % indicates partial IOD [12].
-
Pendred Syndrome characterized by sensorineural deafness, goiter, and a partial defect in iodide organification. The degree of goiter and hypothyroidism varies and appears to depend on nutritional iodide intake. Pendred syndrome is caused by biallelic mutations in the SLC26A4 gene, which encodes pendrin, a multifunctional anion exchanger. Pendrin is mainly expressed in the thyroid, the inner ear, and the kidney. In the thyroid, pendrin localizes to the apical membrane of thyrocytes, where it may be involved in mediating iodide efflux. Loss-of-function mutations in the SLC26A4 gene are associated with a partial iodide organification defect, presumably because of a reduced iodide efflux into the follicular lumen. In the kidney, pendrin functions as a chloride/bicarbonate exchanger. In the inner ear, pendrin is important in the maintenance of a normal anion transport and the endocochlear potential [13].
-
Thyroglobulin (Tg) biosynthesis defects. Impaired Tg synthesis is one of the putative causes for dyshormonogenesis of the thyroid gland. This type of hypothyroidism is characterized by intact iodide trapping, normal organification of iodide, and usually low or undetectable Tg levels in relation to high TSH [14]. When untreated, the patients develop goiter.
-
Iodotyrosine deiodinase defects (ITDD) result from mutations in the DEHAL1 gene that encodes for the thyroidal enzyme that deiodinates mono- and diiodotyrosines (MIT, DIT). In fact, MIT and DIT are by-products formed in excess during TH synthesis, and this enzymatic activity represents an efficient system for iodide recycling within the thyroid gland [15]. ITDDs are characterized by hypothyroidism, compressive goiter, and variable mental retardation, whose diagnostic hallmark is the elevation of iodotyrosines in serum and urine. However, the specific diagnosis of this type of hypothyroidism is not routinely performed, due to technical and practical difficulties in iodotyrosine determinations [16].
14.3.2 Activating Mutations of the TSH Receptor
Germline mutations of the TSH receptor gene that result in constitutive activation of the receptor are a rare cause of diffuse goiter and not autoimmune hyperthyroidism, which may be present at birth or become evident years or even decades later. These mutations are inherited as autosomal dominant traits; as a result, there may be a family history of hyperthyroidism and goiter [17].
14.3.3 Activating Mutations of the G-Protein α Subunit
These somatic mutations are present in the thyroid gland in infants and children with the McCune-Albright syndrome and result in thyroid hyperplasia or formation of nodules and, ultimately, in toxic nodular goiters [18]. Other features of the syndrome, such as cafè au lait skin pigmentation, precocious puberty, and polyostotic fibrous dysplasia, are usually present and provide clues to the underlying diagnosis. The hyperthyroidism is permanent, and in some cases thyroid ablation could be needed.
14.3.4 Thyroid Hemiagenesis
Thyroid hemiagenesis may cause unilateral goiter in neonates or, more often, in children because of compensatory hypertrophy of the contralateral lobe. Pathology that can be associated in the remnant thyroid lobe includes adenocarcinoma, adenoma, multinodular goiter, and chronic thyroiditis [19].
14.3.5 Thyroglossal Duct Cyst
The thyroglossal duct cysts form along the pathway of the gland in fetal life from the base of the tongue to the neck. Normally, the duct is obliterated at birth, but cysts can form within it. Most are located in the midline between the hyoid bone and the isthmus of the thyroid. Generally, they are diagnosed later in childhood and should undergo surgical resection [20].
14.4 Acquired Goiters
14.4.1 Neonatal Goiters (Maternal/Environmental Factors)
-
Transplacental passage of maternal antibodies/goitrogens. Women with autoimmune thyroid diseases may produce antibodies that cross the placenta, resulting in fetal and neonatal goiter and thyroid dysfunction. Antithyroid drugs (ATDs) (propylthiouracil, methimazole, or carbimazole) for the treatment of maternal Graves’ disease or other iodine-containing drugs (expectorans, amiodarone, nutritional supplements, skin disinfectants) all cross the placenta and can cause fetal hypothroidism and goiter. Transplacental passage of TSH receptor blocking antibodies is rarely accompanied by goiter (though typically the gland is normal size or small). In maternal Graves’ disease, transplacental passage of TSH receptor stimulating antibodies (TRAb) that mimic the action of TSH can cause fetal and neonatal thyrotoxicosis and goiter [1]. Although transplacental passage of maternal TRAb does occur early in gestation, the fetal concentration is low until the end of the second trimester when placental permeability increases. Therefore, measurement of maternal TRAb concentration during 24–28 weeks of pregnancy is recommended. If the value is over three times normal, close follow-up for fetal and neonatal thyrotoxicosis is needed [21, 22]. Even women who are euthyroid due to ATD or hypothyroid due to thyroidectomy or radioiodine ablation can have persistent high levels of TRAb which can cause fetal or neonatal thyrotoxicosis. The clinical features of fetal hyperthyroidism are tachycardia (>160 beats/min), intrauterine growth retardation, advanced bone maturation, and goiter. Fetal goiter can also be present in fetal hypothyroidism due to transplacental passage of ATD given to the mother, and this iatrogenic fetal goiter usually regresses on reduction of doses of ATD [21]. Today, serial fetal ultrasonographic monitoring carried out by a highly experienced operator can be an important tool [6, 23]. Symptoms of neonatal thyrotoxicosis can be apparent at birth or may be delayed due to the effect of transplacental passage of maternal ATD or effect of coexisting blocking antibodies, but they are apparent by 10–15 days of life [24]. The clinical manifestations of neonatal hyperthyroidism are related to the involvement of central nervous system (irritability, restlessness), cardiovascular system (tachycardia, cardiac failure, systemic and pulmonary hypertension), and eye (periorbital edema, lid retraction, exophthalmos). Signs of hypermetabolism include hyperphagia with poor weight gain, diarrhea, and sweating. Other signs are hepatosplenomegaly, acrocyanosis, and thrombocytopenia. Diffuse goiter, usually small but occasionally large enough to cause tracheal compression, is present in most infants. Neonatal thyrotoxicosis patients require emergency treatment. The goal of the treatment is to normalize thyroid functions as quickly as possible by ATD administration, to avoid iatrogenic hypothyroidism while providing management and supportive therapy for the infant’s specific signs. The mortality is 12–20 % due to heart failure [6]. Neonatal thyrotoxicosis usually resolves spontaneously between 3 and 12 weeks of life, until the maternal antibodies have disappeared, although it can persist for 6 months or even longer.
-
Severe iodine deficiency (ID). Various studies have shown that during pregnancy not only severe but also moderate ID may cause significant maternal-fetal complications. Normal levels of TH are essential for neuronal migration and myelination of the fetal brain. For the first 12 weeks of gestation, the fetus is completely dependent upon maternal thyroxine. Subsequently, the fetal thyroid becomes able to concentrate iodine and synthesize iodothyronines. However, little hormone synthesis occurs until the 18th–20th week. As ID affects both maternal and fetal thyroid, the risk of goiter development and hypothyroidism is increased in both the mother and fetus. Cretinism represents the most severe form of the broad spectrum of developmental changes caused by maternal ID, with various grades of intellectual impairment depending on ID severity [22, 25].
14.4.2 Goiters in Children and Adolescents
-
Chronic autoimmune (Hashimoto’s) thyroiditis (HT). A firm, bumpy, nontender goiter discovered incidentally during a routine examination is the most common clinical presentation of HT in children [26]. This condition is uncommon in children younger than 4 years of age. The peak age of onset is in early to mid puberty (1–2 % of schoolchildren aged 11–18 years, female-to-male ratio 2:1). It is well known that the risk of HT is higher in individuals with chromosomal abnormalities (Klinefelter, Turner, Down syndromes) and other autoimmune diseases. HT may be generally associated with euthyroid state but also with hypothyroidism (3–13 % of cases) that may be subclinical (up to 35 % of cases) and rarely with hyperthyroidism (Hashitoxicosis). This last condition is caused by autoimmune damage to follicular cells, resulting in the release of preformed TH into circulation. It can present in a fashion similar to Graves’ disease, but it is generally a self-limiting condition and lacks opthalmopathy [27]. In almost all children (85–90 % of cases), high serum concentrations of antithyroid peroxidase (TPO) antibodies and antithyroglobulin (TG) antibodies are detected at first evaluation, while TSH receptor blocking antibodies have been reported in 9.2 % of the cases [28].
In a recent systematic review, Monzani et al. [29] concluded that HT in children may show a more benign evolution than in adults. Subclinical hypothyroidism is a remitting process with a low risk of evolution toward overt hypothyroidism (0–28.8 % of cases). The initial presence of goiter and elevated TG antibodies and a progressive increase in TPO antibodies and TSH value seem to predict this evolution [29, 30].
A complete evaluation of goiter includes ultrasonography of the thyroid that would reveal during follow-up scattered hypoechogenicity and eventually nodules. In HT, prevalence of thyroid nodularity has been reported by Corrias et al. [31]. As high as 35 % of cases in a cohort of 365 patients affected by juvenile HT and papillary carcinoma was found in 3 % of patients with thyroid nodes by fine-needle aspiration biopsy. Treatment with L-thyroxine could reduce thyroid size both in children with or without hypothyroidism, as shown by Svensson et al. [32] in a series of 90 children with goiter and HT.
Taking into account the low rate of progression to an overt hypothyroidism, Monzani et al. [29] suggest that treatment of SH should be indicated in the presence of clinical signs or symptoms of impaired thyroid function or goiter or TSH >10 mU/L.
-
Colloid (simple) goiter. Colloid goiter is a thyroid diffuse enlargement due to unknown causes, usually occurring in adolescent girls. It is not correlated to thyroidal hormonal dysfunction and may show recurrence in some family pedigrees (autosomal dominant inheritance). In a study on female twins, the cumulative concordance rates for goiter in monozygotic and dizygotic twins were 53 % and 20 %, respectively [33].
Histological examination reveals flattened epithelium, variable follicular size, and dense colloid. The natural history of this rare condition is generally benign with extremely slow (many years) spontaneous regression that is not influenced by L-thyroxine treatment.
-
Iodine deficiency goiter. The incidence of endemic goiter due to iodine deficiency has been dramatically reduced in the last 50 years due to iodine supplementation (mainly through the routine utilization of iodized salt) in the western world; however, it has been estimated that about 2 billion people worldwide are at risk for endemic goiter [25]. Urinary iodine excretion less than 50 mcg/L is associated to higher risk of goiter. In children, endemic goiter can be associated with subclinical or mild hypothyroidism, since T3 concentrations may be normal or even high. Association with vitamin A deficiency may increase the risk of thyroid goiter in children with severe iodine deficiency through an increased TSH stimulation, which in turn reduces the risk of hypothyroidism [2].
-
Goitrogens. The principal goitrogenic substance is iodine. Excessive ingestion of iodine, (i.e., from iodine-containing expectorants) may cause thyroid goiter, especially in children with chronic autoimmune thyroiditis. Kelp consumption is another source of possible iodine intoxication. Among other goitrogenic drugs or foods are reported lithium, interferon, cassava, and millet. In association with goiter, children may develop also hypo- or hyperthyroidism. However, when the goitrogenic drug or food is removed, thyroid normal function and size should be restored [34].
-
Graves’ disease. This condition is the most common cause of hyperthyroidism in children and adolescents (overall incidence 1:5,000 children). Adolescent females with a family history of autoimmune thyroid disease are predominantly affected.
The thyromegaly is present in almost all cases with smooth rubbery texture, but also behavioral manifestations are common findings. The frequency of presenting symptoms is shown in Table 14.2. The clinical onset of Graves’ disease can be insidious in most children and the diagnosis delayed up to 6–12 months [27]. The classical hormonal picture at onset is typical, with elevated thyroid hormones and suppressed TSH level. In milder cases, TSH suppression is present without high free T4 levels. Autoantibodies (aTPO and TG) could be detected but are not pathogenetic, as they are TSH receptor antibodies (TRAb). As recently reported by Gastaldi et al. [35], although no clinical variable investigated is constantly associated with a definite outcome, the absence of goiter at the diagnosis may be associated with a better outcome. The most relevant predictor of Graves’ disease outcome was serum level of TRAb; TRAb at time of diagnosis less than 2.5 times the upper reference limit, TRAb normalization during ATD, and TRAb normalization timing may each predict positive outcomes.
Table 14.2 Frequency of presenting symptoms of Graves disease in pediatric patients followed in our clinic (2000–2012) -
Subacute thyroiditis. When the thyroid goiter is tender and painful, subacute thyroiditis should be suspected also in children, even if uncommon in these young patients. They usually develop thyroid goiter after a viral upper respiratory tract infection. Evaluation of thyroid function reveals a classical hyperthyroid phase (that lasts 2–6 weeks) with subsequent (subclinical) hypothyroidism (2–7 months) and finally restoration of normal thyroid function.
-
Acute suppurative thyroiditis. Another rare goiter in childhood is represented by acute suppurative thyroiditis. In this condition, goiter onset is abrupt and accompanied by general symptoms of infection as fever, chills, sore throat, and even dysphagia. The goiter is painful, tender, and could be asymmetric for the swelling of a thyroid lobe only (commonly the left one), with generally a pyriform sinus fistula [36].
14.4.3 Nodular Goiters (Thyroid Cysts, Adenomas, Carcinomas)
Thyroid cysts are uncommon in children and are classified as simple cysts or mixed solid and cystic nodules. Among the rare causes of hyperthyroidism, toxic adenomas are reported also in children. Mutations of TSH receptor gene or alpha subunit of G protein have been detected in some children who could show solitary or toxic multinodular goiter [18, 37]. Malignant nodules are solitary or could be found in the context of multinodular goiter. Conditions that are at risk of malignancy are previous irradiation of head and neck, exposure to nuclear fallout, and thyroiditis [31]. The diagnosis of pediatric thyroid nodules should be based on a stepwise evaluation that includes clinical, laboratory, and radiographic modalities. While laboratory assessments establish thyroid function, ultrasonographic imaging identifies clinically unapparent nodules and provides detailed nodule characterization for suspected malignant lesions. Scintiscan in patients with hyperthyroidism and fine-needle aspiration biopsy in patients with euthyroidism represent the next logical step [38].
The fine-needle aspiration biopsy is a safe technique even in childhood and adolescence, offering the best sensitivity, specificity, and accuracy in detecting malignancy compared with conventional approaches.
14.5 Differential Diagnosis of Goiters
References
LaFranchi S (2014) Congenital and acquired goiter in children. UpToDate. http://www.uptodate.com/contents/search. Accessed 24 Mar 2014
Zimmermann MB, Hess SY, Molinari L et al (2004) New references values for thyroid volume by ultrasound in iodine-sufficient schoolchildren: a World Health Organization/Nutrition for Health and Development Iodine Deficiency Study Group Report. Am J Clin Nutr 79:231–237
Boas M, Hegedus L, Feldt-Rasmussen U et al (2009) Association of thyroid gland volume, serum insuline-like growth factor-1, and anthropometric variables in euthyroid prepubertal children. J Clin Endocrinol Metab 94:4031–4035
Wiersinga WM, Podoba J, Srbecky M et al (2001) A survey of iodine intake and thyroid volume in Dutch schoolchildren: reference values in an iodine-sufficient area and the effect of puberty. Eur J Endocrinol 144:595–603
Perry RJ, Hollman AS, Wood AM et al (2002) Ultrasound of the thyroid gland in the newborn: normative data. Arch Dis Child Fetal Neonatal Ed 87:F209–F211
Polak M, Luton D (2014) Fetal thyroidology. Best Pract Res Clin Endocrinol Metab 28:161–173
Ribault V, Castanet M, Bertrand AM et al (2009) Experience with intraamniotic thyroxine treatment in nonimmune fetal goitrous hypothyroidism in 12 cases. J Clin Endocrinol Metab 94:3731–3739
Leger J, Olivieri A, Donaldson M et al (2014) European Society for Pediatric Endocrinology consensus guidelines on screening, diagnosis and management of congenital hypothyroidism. J Clin Endocrinol Metab 81:80–103
Nicola JP, Nazar M, Serrano-Nascimento C et al (2011) Iodide transport defect: functional characterization of a novel mutation in the Na+/I− symporter 5’-untranslated region in a patient with congenital hypothyroidism. J Clin Endocrinol Metab 96:E1100–E1107
Ris-Stalpers C, Bikker H (2010) Genetics and phenomics of hypothyroidism and goiter due to TPO mutations. Mol Cell Endocrinol 322:38–43
Weber G, Rabbiosi S, Zamproni I et al (2013) Genetic defects of hydrogen peroxide generation in the thyroid gland. J Endocrinol Invest 36:261–266
Cassio A, Corbetta C, Antonozzi I et al (2013) The Italian screening program for primary congenital hypothyroidism: actions to improve screening, diagnosis, follow-up, and surveillance. J Endocrinol Invest 36:195–203
Bizhanova A, Kopp P (2010) Genetics and phenomics of Pendred syndrome. Mol Cell Endocrinol 30(322):83–90
van de Graaf SA, Ris-Stalpers C, Veenboer GJ et al (1999) A premature stopcodon in thyroglobulin messenger RNA results in familial goiter and moderate hypothyroidism. J Clin Endocrinol Metab 84:2537–2542
Moreno JC, Klootwijk W, van Toor H et al (2008) Mutations in the iodotyrosine deiodinase gene and hypothyroidism. N Engl J Med 358:1811–1818
Iglesias A, García-Nimo L, Cocho de Juan JA et al (2014) Towards the pre-clinical diagnosis of hypothyroidism caused by iodotyrosine deiodinase (DEHAL1) defects. Best Pract Res Clin Endocrinol Metab 28:151–159
Biebermann H, Winkler F, Kleinau G (2010) Genetics defects, thyroid growth and malfunctions of the TSHR in pediatric patients. Front Biosci (Landmark Ed) 15:913–933
Ringel MD, Schwindinger WF, Levine MA (1996) Clinical implications of genetic defects in G proteins. The molecular basis of McCune-Albright syndrome and Albright hereditary osteodystrophy. Medicine (Baltimore) 75:171–184
Peña S, Loehn B, Robertson H et al (2010) Thyroid hemiagenesis: report of a case and review of the literature. Laryngoscope 120(Suppl 4):S174
Josephson GD, Spencer WR, Josephson JS (1998) Thyroglossal duct cyst: the New York Eye and Ear Infirmary experience and a literature review. Ear Nose Throat J 77:642–644
Batra CM (2013) Fetal and neonatal thyrotoxicosis. Indian J Endocrinol Metab 17(Suppl 1):S50–S54
Stagnaro-Green A, Abalovich M, Alexander E et al (2011) Guidelines of the American Thyroid Association for the diagnosis and management of thyroid disease during pregnancy and postpartum. Thyroid 21:1081–1114
Huel C, Guibourdenche J, Vuillard E et al (2009) Use of ultrasound to distinguish between fetal hyperthyroidism and hypothyroidism on discovery of a goiter. Ultrasound Obstet Gynecol 33:412–420
Levy-Shraga Y, Tamir-Hostovsky L, Boyko V et al (2014) Follow-up of newborns of mothers with Graves’ disease. Thyroid 24:1032–1039
Zimmermann MB (2009) Iodine deficiency in pregnancy and the effects of maternal iodine supplementation on the offspring: a review. Am J Clin Nutr 89:68S–72S
de Vries L, Bulvik S, Phillip M (2009) Chronic autoimmune thyroiditis in children and adolescents: at presentation and during long-term follow-up. Arch Dis Child 94:33
Muirhead S (2001) Diagnostic approach to goiter in children. Paediatr Child Health 6:195–199
Feingold SB, Smith J, Houtz J et al (2009) Prevalence and functional significance of thyrotropin receptor blocking antibodies in children and adolescents with chronic lymphocytic thyroiditis. J Clin Endocrinol Metab 94:4742–4748
Monzani A, Prodam F, Rapa A et al (2013) Natural history of subclinical hypothyroidism in children and adolescents and potential effects of replacement therapy: a review. Eur J Endocrinol 168:R1–R11
Radetti G, Gottardi E, Bona G et al (2006) The natural history of euthyroid Hashimoto’s thyroiditis in children. J Pediatr 149:827–832
Corrias A, Cassio A, Weber G et al (2008) Thyroid nodules and cancer in children and adolescents affected by autoimmune thyroiditis. Arch Pediatr Adolesc Med 162:526–531
Svensson J, Ericsson UB, Nilsson P et al (2006) Levothyroxine treatment reduces thyroid size in children and adolescents with chronic autoimmune thyroiditis. J Clin Endocrinol Metab 91:1729–1734
Brix TH, Kyvik KO, Hegedus L (1999) Major role of genes in the etiology of simple goiter in females: a population-based twin study. J Clin Endocrinol Metab 84:3071
Friedrich-Rust M, Theobald J, Zeuzem S et al (2009) Thyroid function and changes in ultrasound morphology during antiviral therapy with pegylated interferon and ribavirin in patients with chronic hepatitis C. J Viral Hepat 16:168–177
Gastaldi R, Poggi E, Mussa A et al (2014) Graves disease in children: thyroid-stimulating hormone receptor antibodies as remission markers. J Pediatr 164:1189–1194
Wasniewska M, Vigone MC, Cappa M et al (2007) Acute suppurative thyroiditis in childhood: spontaneous closure of sinus pyriform fistula may occur even very early. J Pediatr Endocrinol Metab 20:75–77
Schwab KO, Pfarr N, van der Werf-Grohmann N et al (2009) Autonomous thyroid adenoma: only an adulthood disease? J Pediatr 154:931–933
Corrias A, Einaudi S, Chiorboli E et al (2001) Accurancy of fine needle aspiration biopsy of thyroid nodules in detecting malignancy in childhood: comparison with conventional clinical, laboratori, and imaging approaches. J Clin Endocrinol Metab 86:4644–4648
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Cassio, A., Bal, M.O., Bettocchi, I., Baronio, F. (2015). Thyroid Enlargement from Newborn to Adolescent. In: Bona, G., De Luca, F., Monzani, A. (eds) Thyroid Diseases in Childhood. Springer, Cham. https://doi.org/10.1007/978-3-319-19213-0_14
Download citation
DOI: https://doi.org/10.1007/978-3-319-19213-0_14
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-19212-3
Online ISBN: 978-3-319-19213-0
eBook Packages: MedicineMedicine (R0)