Abstract
The infection of biomaterials, particularly medical implants, represents a significant challenge during surgical implantation processes and the subsequent recovery period for the recipient of the implant.
Infections arising from such surgical procedures not only adversely affect the well-being of the patient; they also place a significant burden on the healthcare systems of many countries around the world. A great deal of effort has been made in attempts to minimise or prevent pathogenic bacteria from contaminating these biomaterials. These efforts have included the development of techniques for rendering the surfaces anti-fouling through chemical modification or functionalization of the surface. Recent focus, however, has been placed on the production of antibacterial surfaces. Developments in the area of nanofabrication have allowed the chemical and physical characteristics of the surface of implant materials to be modified such that the molecular to micro-scale topological features can now be accurately controlled.
This chapter will provide an overview of the current approaches and techniques being used or are being developed in the design of antibacterial metallic implant surfaces. Such surfaces can be subjected to a number of chemical and physical modification techniques to achieve this aim, with the resulting surfaces being found to not only exhibit antibacterial behaviour, but also biocompatibility.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Implant surfaces
- Antibacterial
- Bactericidal
- Titanium
- Biocide-releasing surfaces
- Nanoparticles
- Surface topography
6.1 Introduction
Bacterial infection of biomaterials has long been a significant problem, both during implant surgery and after the implantation process (Lavernia et al. 2006; Bozic and Ries 2005; Montanaro et al. 2011; Arciola et al. 2012; Campoccia et al. 2013a, b; Busscher et al. 2012; Whitehouse et al. 2002). Infection that results from receiving a contaminated biomedical implant substantially affects the quality of life for the patient and represents a large burden to society by increasing the number of clinical procedures having to be undertaken in the healthcare system, thus increasing the costs of health care. For example, it has been estimated that antibiotic treatment and revisionary surgery for replacement of an infected total hip causes the primary procedure costs to triple to an average of $75,000 in the US (Lavernia et al. 2006; Bozic and Ries 2005). It has been found that infections that have arisen from orthopaedic surgery prolonged the hospital stay for patients by a median of 2 weeks each, approximately doubled the re-hospitalisation rates, and increased healthcare costs by more than 300 % (Whitehouse et al. 2002). Complications arise as a result of the the pathogenic bacteria developing resistance to the natural host defense mechanisms and antibiotics. This means that treatment of the infection whilst the implant is still resident in the patient is usually unsuccesful, leading to the necessity for surgical intervention (Olson et al. 2002; Davies 2003; Vasilev et al. 2009; Høiby et al. 2010). It appears that only a low dose of inoculum is required to result in the infection of an implant; in an animal model study, it was found that 100 colony-forming units (cfu) of S. aureus were sufficient to infect 95 % of the subcutaneous implants used in the study (Arciola et al. 2012; Campoccia et al. 2013b; Song et al. 2013). Most of the microorganisms that cause implant infections are present in the host flora, of which the most frequent are Staphylococci, Streptococci, Pseudomonas species and coliform bacteria (Campoccia et al. 2013a, b; Olson et al. 2002; Davies 2003).
In an effort to combat implant-associated bacterial infection, recent focus has been placed on the development of antibacterial surfaces (Campoccia et al. 2013a, b; McLean et al. 1993; Yoshinari et al. 2001; Wan et al. 2007a, b; Zhao et al. 2009; Vasilev et al. 2009; Rautray et al. 2010; Glinel et al. 2012; Hajipour et al. 2012; Hasan et al. 2013). With the current growth in the development of novel nanofabrication tools, modifying the chemical and physical characteristics of implant surfaces has been shown to co ntrol the molecular to micro-scale topological features of many substrate surfaces. This chapter will provide an insight into the current methods being used for the design of antibacterial surfaces on implant materials and a rationale for the applicability of the unique surfaces being produced.
6.2 Strategies Being Used for the Design of Antibacterial Implant Surfaces
6.2.1 Overview
Implantable biomaterials have long been used for restoring joint function, reduce pain or stabilise fractured bones (Pourbaix 1984; Cui and Luo 1999; Wan et al. 2007a, b; Zhao et al. 2009; Rautray et al. 2010; Minagar et al. 2012; Andani et al. 2014). Antibacterial implant materials need to be both antibacterial and biocompatible (Anselme et al. 2010; Zhao et al. 2009, 2014; Vasilev et al. 2009; Busscher et al. 2012; Campoccia et al. 2013a, b). In 1987, Anthony Gristina first introduced the concept of a “race for the surfaces” to describe the competition that exists between the integration of tissue cells onto the surface of an implant material and the adhesion of pathogenic bacteria (Gristina 1987; Gristina et al. 1988). Clearly, it is desirable for the host tissue to have the opportunity to establish itself over the surface of a biomedical implant in order that the implant surface is connected to the body, allowing further tissue generation to take place without the invasion of pathogenic bacteria. It is therefore not surprising that a variet y of alternative approaches have been developed for the construction of biomaterials that exhibit antibacterial properties that can simultaneously support the host tissue integration and effectively deal with any bacteria coming into contact with the surface.
Here, the different approaches currently being used to reduce the vulnerability of medical devices to bacterial attachment will be discussed. The current designs for antibacterial biomaterials can be classified into two major groups, classified according to their mode of action. The first is antifouling surfaces, which have the ability to repel or prevent bacteria from adhering to their surface. The second is bactericidal surfaces, which have the ability to damage or kill a ny pathogenic bacteria coming into contact with the surface (Fig. 6.1).
Schematic representation of the different strategies currently being used in the design of antibacterial surfaces (Adapted from Campoccia et al. 2013a)
6.2.2 Antifouling Surfaces
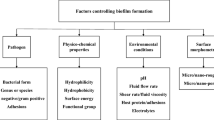
Bacterial adhesion to a n implant surface occurs when bacteria are able to make contact with a surface that provides them with a favourable environment for changing from their planktonic state to that of being sessile; this is most often accompanied by the production of a bacterial biofilm (Olson et al. 2002; Anselme et al. 2010; Arciola et al. 2012; Foster et al. 2014). It is clear that an infection arising from the presence of pathogenic bacteria would not occur if the bacteria involved were unable to initially colonise the medical device. The complex mechanisms associated with bacterial attachment have long been studied in order to gain an understanding into the methods by which metallic antibacterial surfaces can be designed such that this event can be prevented. A wide range of chemico-physical properties and functional groups on both the substrate and pathogen have been modified in order to modulate the attachment of these bacteria (Fusetani 2004, 2011; Hasan et al. 2013; Bazaka et al. 2011a, 2012; Webb et al. 2011; Crawford et al. 2012). More recently, surface architectures that contain specific surface porosity, roughness and geometry have been used to produce metallic biomaterial surfaces that are resistant to microbial colonisation (Meng et al. 2014; Anselme et al. 2010; Webb et al. 2011; Crawford et al. 2012; Bazaka et al. 2012).
Metallic biomaterial devices are often exposed to body fluids and a rich protein environment at the site of surgical implantation (Arciola et al. 2003; Campoccia et al. 2013a, b). It is known that a variety of host proteins promote bacterial attachment and the formation of biofilm s. These are called microbial surface components recognizing adhesive matrix molecules, or MSCRAMMs, and these include collagen, fibrinogen, fibronectin, laminin, vitronectin, clumping factor A and B, bone-sialoprotein, elastin, IgG and other possible components (Lv et al. 2013; Montanaro et al. 2011; Patti et al. 1994; Arciola et al. 2012; Foster et al. 2014; Foster and Höök 1998; Hauck et al. 2006; Lambris et al. 2008). The biomaterial surfaces are therefore required to support the adsorption of host adhesins onto their surface to ensure the successful subsequent integ ration of tissue, whilst at the same time being able to repel the bacteria or be anti-adhesive towards them.
Chemical me thods can be used to construct microbe-repellent surfaces by attaching antifouling molecules to the surfaces of implant materials (Neoh et al. 2012; Campoccia et al. 2013a, b). Common chemical modification approaches include rendering the surfaces superhydrophobic/superhydrophilic or highly hydrated or non-charged, each of these being unfavourable for bacterial adhesion under certain circumstances (Fig. 6.1) (Campoccia et al. 2013a, b). One of the most common coatings to render the surface hydrophilic is poly(ethylene glycol) (PEG) . The inhibition mechanism of such surfaces is based on the dynamic motion and steric repulsion of hydrated polymer chains, which prevents bacterial attachment (Harris et al. 2004; Maddikeri et al. 2008). In addition, polycationic polymers exhibit antifouling effects have been used by directly coating or grafting them onto biomedical devices (Chua et al. 2008; Subbiahdoss et al. 2010; Shi et al. 2008; Hu et al. 2010; Siedenbiedel and Tiller 2012). Heparin coatings have also been shown to exhibit a high anti-adhesive effect for bacteria by increasing the hydrophilicity of the surfaces. The heparin forms a highly hydrated layer between the pathogens and the substrate (Ruggieri et al. 1987; Arciola et al. 1993). It was reported that heparin can inhibit the extent of S. epidermidis binding to fibronectin, thus preventing the subsequent colonisation of the surface (Arciola et al. 2003; Bustanji et al. 2003). Another approach, where quorum-sensing inhibitors (e.g. furanones and their derivatives) are incorporated onto biomedical device surfaces, was used to disrupt the processes responsible for the formation of a biofilm (Fig. 6.1) (Fusetani 2004, 2011). This approach, however, has significant drawbacks in terms of the long-term stability of the coating and the possible cytotoxicity of these additives in biomedical applications. Current approaches use surface topography as the factor by which the degr ee of bacterial adhesion and subsequent biofilm formation can be controlled or prevented. Techniques such as this represent a more robust method for creating surfaces that repel or control the extent of microbe attachment (Webb et al. 2011, 2014; Hasan et al. 2013; Grinthal and Aizenberg 2014; Bazaka et al. 2012; Crawford et al. 2012). For example, superhydrophobic surfaces have been shown to exhibit antifouling characteristics and can be obtained by physically modifying the micro- and nano-structures of biomaterial surfaces by mimicking natural surface structures such as that of the lotus leaf (Truong et al. 2012; Fadeeva et al. 2011; Crick et al. 2011). By tailoring the precise and specific surface topographical parameters, these surfaces have shown promising results in their ability to limit the initial adhesion of pathogenic bact eria (Webb et al. 2011, 2014; Hasan et al. 2013).
6.2.3 Bactericidal Surfaces
Another com mon approach in the prevention of biofilms on biomedical devices is the utilization of bioactive antibacterial agents that act by contact killing the bacteria. These techniques involve coating the substrate with various immobilized antimicrobial substances such as antibacterial peptides (Brouwer et al. 2011; McCloskey et al. 2014; Salwiczek et al. 2014), quaternary amines (Mei et al. 2012; Schaer et al. 2012), nitric oxide (Fox et al. 2010; Nablo et al. 2005) or antibacterial metals (silver, zinc, cobalt, aluminium and copper) (Kawashita et al. 2000; McLean et al. 1993; Heidenau et al. 2005; Lemire et al. 2013; Stafford et al. 2013; Prantl et al. 2010; Wan et al. 2007a). These substances are not released from the substrate, and as such they directly interact with any pathogenic bacteria coming in contact with the surface (Williams and Worley 2000). Bioactive antibacterial coatings have been used extensively in applications that require the surface to be self-sterilizing over extended periods (Williams and Worley 2000; Campoccia et al. 2013a).
Silver and it s derivatives are some of the earliest bactericidal agents that have been largely applied in a wide range of applications (Zhao et al. 2009; Kawashita et al. 2000; McLean et al. 1993; Nomiya et al. 1997; Dueland et al. 1982; Richards 1981; Bayston et al. 2010). Other metals that have also been reported to exhibit bactericidal effects, mostly in their composite form, include zinc, cobalt, aluminium and copper (Heidenau et al. 2005; Lemire et al. 2013; Samanovic et al. 2012; Stafford et al. 2013; Hoene et al. 2013; Prantl et al. 2010; Shirai et al. 2009; Wan et al. 2007a, b). The use of antimicrobial metals is, however, often associated with certain degree of cytotoxicity . This can have an impact on the host cell response, leading to the loss of cell viability and the failure of tissue integration (Heidenau et al. 2005; Hoene et al. 2013; Paasche et al. 2011; Vasilev et al. 2009). This occurs mainly as a result of corrosion of the metal in the physiological environment, which causes the release of metal ions at relatively high concentrations, leading to local toxicity and occasionally metal accumulation in the target organs (Campoccia et al. 2013b; Lemire et al. 2013; Vasilev et al. 2009). The mechanisms responsible for the antibacterial activity of metals and metal ions is not fully understood. Gordon et al. suggested that silver interacts with thiol groups, causing the inactivation of critical enzymes in the respiratory chain an d t he induction of hydroxyl radicals (Gordon et al. 2010).
Another emerging strategy for the manufacture of antimicrobial surfaces is the incorporation of biocide-releasing surfaces such as those containing nanoparticles . The extent of the bactericidal effect of these surfaces depends on the size, shape, concentration and chemical composition of the nanoparticles (Cui et al. 2012b; Zhang et al. 2013; Hajipour et al. 2012). While the exact mechanisms of the antimicrobial activity are also not fully understood, most nanoparticles are seen to generate reactive oxygen species and damage the cell membranes (Cui et al. 2012b; Zhang et al. 2013; Hajipour et al. 2012). For example, gold nanoparticles exhibit bactericidal effects against E. coli by inhibiting ATP synthase activity, followed by the inhibition of the ribosome sub-unit in tRNA binding (Cui et al. 2012b). There is still a lack of knowledge on the toxicology of nanoparticles, with most of the available data being inconsistent and largely non-reproducible (Campoccia et al. 2013a; Yildirimer et al. 2011). The negative impact of nanoparticles in biomedical applications includes the induction of apoptosis, introduction of toxic effects to the genome and the possible translocation of nanoparticles to distant tissues and organs, with an associated risk of systemic effects (Yildirimer et al. 2011; Campoccia et al. 2013a).
The major problem, however, is that biofilms display an increased tolerance towards antimicrobial agents, which substantially restricts our ability to treat biofilm-related infections in clinical settings. While the increased resilience of biofilms to wards antibiotic s is multifactorial, this resistance can be attributed to the presence of persistent bacteria, those that can enter into a specific phenotype state that allows them to survive in the presence of 1000 times the minimum inhibitory concentration of bactericidal antibiotics (Olson et al. 2002; Davies 2003). Persistent cells have recently been the subject of increased investigation with a view to limiting their biofilm-associated antibiotic tolerance. The current strategy for preventing the formation of biofilm s has been to develop ways by which the initial bacterial adhesion step can be inhibited, which will subsequently limit the grow th of the biofilm (Hasan et al. 2013; Fusetani 2004).
Recently, the effects of surface topography on the attachment responses of bacterial and mammalian cells has been under investigation in an effort to obtain an insight into the competition that takes place when bacteria and host tissue compete for attach ment on a substrate surface (Hasan et al. 2013). When trying to prevent biofilm s from forming on medical implant surfaces, a common approach is to develop a surface structure that can both physically inhibit the growth of bacteria, but at the same time promote tissue integration. Nano-structured surfaces have shown numerous promising results. Interesting reports have demonstrated that surfaces containing nanopillar arrays that mimic the structure of dragonfly wings can exhibit a bactericidal effect to not only Gram positive and Gram negative bacteria, but also their spores (Hasan et al. 2013; Ivanova et al. 2013; Bazaka et al. 2012). Recent research has also shown that mammalian cells are biocompatible with these high aspect ratio structured surfaces that contain complex geometries, in which the cells appeared to be able to maintain their viability, adhesion to the surface and their subsequent cellular activities (Kim et al. 2007; Robinson et al. 2012; Elnathan et al. 2014; Jahed et al. 2014). For the reasons previously described, the ability to design surfaces that possess antimicrobial properties without the need for the surface to contain antibiotics or chemical additives represents a significant step forward in developing implant materials that are less likely t o be the cause of post-operative infections.
6.3 Fabrication Techniques
Since the advent of micro- and nano-technology, a number of fabrication techniques have been developed that can be used to modify the surface properties of metallic implants on a molecular-, nano- and micro-scale. Antibacterial metallic surfaces can be fabricated via two principal methods: chemical and physical modification (Jeon et al. 2014; Lv and Feng 2006; Yoshinari et al. 2001; Vasilev et al. 2009; Hasan et al. 2013; Salwiczek et al. 2014). Techniques such as surface chemical functionalization, chemical vapour deposition, anodic oxidation, hydrothermal treatment and ion implantation involve chemical reactions occurring at the surface to modify the surface properties. Techniques such as physical vapour deposition, layer-by-layer coating, and sol-gel coating utilise physical adsorption on implan t surfaces without altering the surface chemistry.
6.3.1 Chemical Modification
This section highlights the techniques that employ processes such as wet chemistry and high energy sources to alter the surface characteristics of metal surfaces. Here, we present a general overview of the chemical modification techniques that can be used to produce antibacterial metallic surfaces in Figs. 6.2 and 6.3.
Representative antibacterial m etallic surfaces fabricated via various chemical fabrication techniques. (A) (a) SEM images of the top-view of TiO2 nanotube surfaces; the nanotubes are approximately 40–97 nm in diameter and 300 nm in length. (b) (inset) the changed morphologies of the surface after the adhesion patterns of Streptococcus mutans, cultured for 48 h (Adapted with permission from Cui et al. 2012a, b). (B) FE-SEM images of (a) pure ZnO, (b) TiO2/ZnO, (c) Ag/TiO2/ZnO particles, and (d) high magnification of (c). (e) and (f) represent the zones of inhibition tests for (top) TiO2/ZnO and (bottom) Ag/TiO2/ZnO composite surfaces towards E. coli (Adapted with permission from Pant et al. 2013). (C) Colony-forming units relative to control against P. gingivalis on 1 cm2 plates for 48 h against different ion-implanted Ti surfaces (Adapted with permission from Yoshinari et al. 2001)
(A) Confocal microscopic im ages of (a) a control Ti rod and (b) Ti rods covalently linked with vancomycin (vanc); (c) The antibacterial efficiency of the control and Ti-vanc rods towards S. aureus incubated at a time period from 0 to 30 h. The Ti-Vanc rods showed fewer adherent colonies at all times than control rods. (d) Represents the fluorescent stains for the viable cells on the control Ti surface (Adapted with permission from Antoci et al. 2007). (B) SEM images of (a) Ag-TiO2 and (b, c) Cu-TiO2 films. (d) TEM cross section micrograph of Ag-TiO2 and (e) planar view of Cu-TiO2 coatings show the metal nanoparticle distribution in the TiO2 matrix through chemical vapour deposition (CVD). (f) The influence of Ag (left) and Cu (right) content of M-TiO2 nanocomposite coatings on the antibacterial behaviour against S. aureus. The coloured zone corresponds to inactive surfaces according to the JIZ test (Adapted with permission from Maury et al. 2014)
6.3.1.1 Chemical Functionalisation
Chemical functio n alization of various metallic surfaces has been one of the most commonly used techniques for preparing anti bacterial surfaces (Zobrist et al. 2011; Ogaki et al. 2010; Gerberich and Bhatia 2013). This fabrication technique is suitable for designing antifouling and bactericidal surfaces that can kill bacteria on contact. The functionalisation of inert metallic surfaces is, however, a challenge. To overcome this problem, there are two strategies used for functionalising surfaces such that they contain antifouling or bactericidal agents (Yuan et al. 2011; Gadenne et al. 2013; Antoci et al. 2007; Godoy-Gallardo et al. 2014; Holmberg et al. 2013; Chen et al. 2013): These are: (1) developing adhesion coatings, such as self-assembled monolayers (SAM); or (2) functionalising metallic surfaces with active groups, such as thiol (-SH), hydroxyl (-OH), amine (-NH2) or carboxylic groups (-COOH).
The first strategy is to coat the surface with self-assembled monolayers (SAM) to act as an adhesion layer for the immobilisation of antibacterial agents (Yuan et al. 2011; Gadenne et al. 2013). For example, self-assembled monolayers of aminoundecyltrimethoxysilane were used as an adhesion layer on Ti substrates to covalently bond polysaccharides extracted from Ulva rotundata and Ulva compressa seaweed (Gadenne et al. 2013). Adhesion of Pseudomonas aeruginosa cells was shown to be reduced by 90 % on these surfaces compared to the control surface. Conjugation of poly(ethylene glycol) (PEG) brushes on stainless steel was used to couple with hydrolytic enzymes such as lysozyme (Yuan et al. 2011), creating a surface that exhibited a high degree of antifouling and bactericidal behaviour towards E. coli and S. aureus cells. The dual coupling of the PEG derivative along with lysozyme served a dual function; displaying antifouling properties towards bovine serum albumin protein and antibacterial behaviour towards the specific bacterial strains (Yuan et al. 2011).
A second approa ch is to func tionalise surface with reactive groups, then covalently bind antibiotics or antimicrobial peptides (AMP) to the surface (Antoci et al. 2007; Godoy-Gallardo et al. 2014; Holmberg et al. 2013; Chen et al. 2013). A number of studies have been reported for the successful tethering of antibiotics to metallic implant surfaces. For example, non-reactive Ti surfaces were chemically modified to carry amine groups that reacted with vancomycin (Antoci et al. 2007). This method was shown to be able to preserve the antibacterial properties of the modified Ti surfaces, while preventing the release of antibiotics into the surrounding body fluid. In other studies, AMP were conjugated onto metall ic surfaces. For example, Ti surfaces were chemically modified to contain hydroxyl groups, onto which hydrophilic poly (ethylene glycol) was conjugated as a spacer between the AMP and the Ti surface (Gabriel et al. 2006).
6.3.1.2 Chemical Vapour Deposition
Chemical vapour deposition (CVD) is yet another chemical process that has been used to fabricate an antibacterial layer over substrate surfaces on a large scale (Wilkinson et al. 2013; Bazaka et al. 2010, 2011a, b, 2012; Dastjerdi and Montazer 2010; Maury et al. 2014; Varghese et al. 2013). In a deposition process, the substrate is exposed to antibacterial monomer precursors, which react with the substratum under plasma condition to synthesise antibacterial surfaces. These processes have been used to fabricate both inorganic and organic antibacterial coatings.
Inorganic coatings on metallic implant surfaces such as silver, TiO2 and other photocatalytic metal oxides was performed using CVD (Dastjerdi and Montazer 2010; Maury et al. 2014; Varghese et al. 2013). Composite TiO2 films, coupled with other metallic ions such as Ag+ or Cu2+, have also been synthesized using CVD (Maury et al. 2014). TiO2 nano-composite films coupled with Ag have been shown to exhibit strong bactericidal efficiency against S. aureus, where a minimum film thickness of 100 nm has been found to be essential for rendering the film antibacterial in nature (Maury et al. 2014). Flame-assisted chemical vapour deposition has also been recently employed to fabricate silver-silica coatings on glass surfaces, the antibacterial efficiencies of which have been tested using E. coli, S. aureus and P. aeruginosa (Varghese et al. 2013). A plasma deposition method has also been used to deposit Cu ions on titanium alloy surfaces. This combination of Cu ions embedded onto Ti6Al4V surfaces has proven to be an effective method for preparing an antibacterial surface, since the amount of copper ions released from the surface resulted in killing ~99 % of the bacterial cells (Hempel et al. 2014).
For organic coatings to be prepared using CVD, monomers of antibacterial agents need to be used as precursors for the formation of antibacterial polymer films on a substrate (Bazaka et al. 2010, 2011a, b; Pegalajar-Jurado et al. 2014). For example, substrata have been encapsulated with polyterpenol thin films prepared from antibacterial terpinen-4-ol monomers using radio frequency plasma enhanced chemical vapour deposition (Bazaka et al. 2010, 2011b). These polyterpenol films were found to be effective against P. aeruginosa and S. aureus cells due to the preservation of original terpinen-4-ol molecules in the resulting film str ucture (Bazaka et al. 2010, 2011b). In another study, plasma polymerised thin films produced from antibacterial 1,8-cineole monomers were shown to inhibit the proliferation of E. coli and S. aureus (Pegalajar-Jurado et al. 2014).
6.3.1.3 Anodic Oxidation
Electrochemical anodic oxidation techniques have been used to fabricate highly ordered nanoporous nanotubes on metal surfaces (Cui et al. 2012a; Li et al. 2013; Yue et al. 2014; Minagar et al. 2012; Visai et al. 2011). In particular, TiO2 nanotubes have been recognized as promising biomaterials, with proven biocompatibility, thermal stability and corrosion resistance. Enhancement of the antibacterial properties of TiO2 nanotubes can be achieved through the use of UV illumination or the i ncorporation of antibiotic loadings (Cipriano et al. 2014; Cui et al. 2012a; Çalışkan et al. 2014; Chennell et al. 2013). For example, TiO2 nanotub e layers have been designed to become photocatalytic, which can disrupt the viability of Streptococcus mutans (Cui et al. 2012a), whereas the incorporation of gentamycin inside the nanotube patterns was found to improve their antibacterial properties (Çalışkan et al. 2014).
6.3.1.4 Hydrothermal Treatment
Hydrothermal synt hesis is an environmental friendly process for synthesising antibacterial surfaces because the synthesis reaction is completely contained in aqueous solutions inside a closed system, making use of acidic or basic solutions as the reaction medium (Huo et al. 2013; Pant et al. 2013; Hebeish et al. 2013; Li et al. 2014; Wong et al. 2011). In such processes, the operating temperature is held above the boiling point of water to autogenously produce a saturated vapour pressure. As with the anodic oxidation technique, this technique is only suitable for the preparation of antibacterial inorganic coatings, such as silver, TiO2, and other photocalytic materials (Huo et al. 2013; Pant et al. 2013; Hebeish et al. 2013; Li et al. 2014). For example, a one-step hydrot hermal synthesis has been used to fabricate ZnO and silver nanoparticles coupled with a passive TiO2 layer to improve the antibacterial efficiency of photocatalytic TiO2 layers (Pant et al. 2013). In addition, it has been reported that Ti nanowires doped with silver exhibited commendable antimicrobial efficiency to w ards various Pseudomonas species (Hebeish et al. 2013; Li et al. 2014).
6.3.1.5 Ion Implantation
Ion implantation has been used as a method for doping antibacterial inorganic ions onto the surface of biomedical implants under the immersion of plasma (Cui and Luo 1999; Rautray et al. 2010; Lu et al. 2012; Yoshinari et al. 2001; Zhao et al. 2009). Ti and Ti alloys modified with ion imp lantation (F+) were shown to inhibit the growth of both Porphyromonas gingivalis and Actinobacillus actinomycetemcomitan (Yoshinari et al. 2001; Rautray et al. 2010). In addition, it was shown that F+ implanted surfaces did not inhibit the proliferation of fibroblast L929-cells (Yoshinari et al. 2001). Silver and copper ion-doped Ti surfaces prepared using ion implantation processes were shown to reduce th e viability of S. aureus cells coming into contact with the surface (Wan et al. 2007a).
6.3.2 Physical Modification
Physical modification techniques coat metallic substrates through physical adsorption without altering the surface chemistry. Here, we present a general overview of the physical modification techniques that can be used for t he preparation of antibacterial metallic surfaces (Fig. 6.4).
Representative antibacteria l metallic surface fabricated via various physical fabrication techniques. (A) FE-SEM images of the (a) TiAgN and (b) ZrAgN coatings fabricated through physical vapour deposition (PVD). Scale bars indicate 5 μm. Inset image (c) represents the clear zone of inhibitions of the coated samples against S. mutans after 18 h incubation (Adapted with kind permission from Kang and Lim 2014). (B) A schematic illustration of the antimicrobial property of the layer-by-layer assembly of single wall carbon nanotubes along with the polyelectrolytes poly(L-lysine) and poly(L-glutamic acid) (Adapted from Aslan et al. 2012). (C) Reaction scheme for producing quaternary ammonium silanes (QAMS) using tetra-alkoxysilane as attaching unit. Macromonomers with monofunctional (QAMS-1), bifunctional (QAMS-2) or trifunctional methacryloxy functionalities (QAMS-3) have been fabricated based on the molar ratio of the two trialkoxysilanes through the process of sol-gel coating. Inset image represents the antimicrobial activity of the polymerized resin through the confocal laser scattering microscopy images of 48 h microbial biofilms of S. mutans (top), A. naeslundii (middle) and C. albicans (bottom) respectively (Adapted with permission from Gong et al. 2012)
6.3.2.1 Physical Vapour Deposition (PVD)
Physical vapour deposition (PVD), due to its environmentally friendly characteristics, convenience and precision in deposition, has become one of the commonly used techniques in preparing uniform surface coatings (Zaborowska et al. 2014; Percival et al. 2005; Ip et al. 2006; Ivanova et al. 2011; Chang et al. 2013; Trivedi et al. 2014). A number of reports have shown that physical vapour deposition has also been used to deposit uniform coatings on titanium and its alloys. This technique fabricates an antibacterial surface by employing a twin-gun magnetron sputtering system to synthesize uniform coatings o f silver and zirconium oxide (Zaborowska et al. 2014; Percival et al. 2005; Ip et al. 2006; Ivanova et al. 2011; Chang et al. 2013). This process is also commonly used to deposit silver coatings on titanium surfaces, since the silver coating provides a biocompatible surface and also helps to reduce the attachment and viability of bacteria (Zaborowska et al. 2014; Percival et al. 2005; Ip et al. 2006; Ivanova et al. 2011; Chang et al. 2013). Additionally, this system offers almost no cytotoxicity issues towards mammalian cells.
Another slight variation of this tec hnique, arc-ion plating (AIP), has also been used to fabricate TiAgN and ZrAgN alloys coatings (Kang and Lim 2014). These coatings serve as efficient antibacterial coatings by reducing the adhesion and viability of S. mutans (Kang and Lim 2014). AIP is a widely used technique in the biomedical industry due to its advantages, including its ability to produce a dense metal vapour, high ionization efficiency and high deposition rate (Joo et al. 2009). Plasma nitriding of stainless steel surfaces with Ag+ ions has also resulted in the synthesis of highly efficient antimicrobial surfaces, which have been re ported to eliminate almost all (~97 %) of the inoculating bacterial cells of E. coli and S. epidermidis in a 6 h time span by the method of contact killing (Dong et al. 2011).
6.3.2.2 Layer-by-Layer Coatings
Layer-by-layer self-assembly (LbL) is the technique that has been used to encapsulate antibiotics, antimicrobial peptides and nanomaterials onto metallic surfaces (De Villiers et al. 2011; Hammond 1999, 2004; Decher 1997; Linford et al. 1998). The technique has some essential steps, as follows: (1) A charged substrate is submerged in a solution of an oppositely-charged colloid, designed to assist the adsorbtion of the first monolayer, (2) this is followed by a washing cycle to remove unbound material and impede the contamination of the surface with the oppositely-charged colloid, (3) the coated substrate is re-submerged to finally adsorb the second layer and thus a series of multi-layered deposits is formed in this manner (De Villiers et al. 2011). There also have been instances where no washing step is required in the sample preparation, as in the case of strong electrolytes, where the polymer is strongly bound to the surface by electrostatic interactions (Linford et al. 1998).
Feature size s lesser than 1 μm can be easily obtained, since the limitations of this technique are only restricted by the fairly large dimensions of the bound macromolecules in the solution (De Villiers et al. 2011). A recent use of this technique has been in the fabrication of antibacterial surfaces. Here, the antimicrobial efficiency of single-walled carbon nanotubes (SWNT) that were layer-by-layer assembled with poly (L-lysine) and poly (L-glutamic acid) were well studied for their resistance to the attachment of the bacterial strains of E. coli and S. epidermidis (Aslan et al. 2012, 2013). This assembly of multilayer films has the ability of reducing the proliferation rates of the bacterial cells by up to 90 % (Aslan et al. 2012, 2013). With LbL technology, multi-faceted surfaces with altered shapes can be conveniently coated with conformal ultra-thin films (Hammond 2004; Decher 1997). Layer by layer assembly has also been used to fabricate a cross-linked polymeric thin film using a polycation, N, N-dodecyl, methyl-polyethylenimine and a polyanion, poly (acrylic acid). Surfaces containing this combination have been reported to be highly effective against the commonly found infecting strains of E. coli and S. aureus (Wong et al. 2010). This film exhibited considerable antibacterial effectiveness by causing cell lysis when the cells came in contact wi th the surface of the polymeric film.
6.3.2.3 Sol-Gel Coating
Sol-gel coating processe s involve the conversion of monomers into antibacterial colloidal solutions (sols) that acts as precursors for an integrated network (gel) of the coatings (Chun et al. 2007; Rivero et al. 2011; Talebian et al. 2014; Visai et al. 2011). Sol-gel TiO2 coatings on stainless steel orthodontic wires have been shown to reduce the viability of Streptococcus mutans and Porphyromonas gingivalis (Chun et al. 2007). A novel antibacterial coating composed of an organic-inorganic hybrid matrix of tetraorthosilicate and a polyelectrolyte was successfully doped with Ag nanoparticles through sol-gel processes (Rivero et al. 2011). This specific coating has ability to eliminate the growth of Lactobacillus plantarum. Nickel oxide nanoparticles that were immobilised in a sol-gel coating were also found to exhibit a high degree of antibacterial activity against S. aureus and E. coli cells (Talebian et al. 2014).
6.4 Future Perspectives
In general, this chapter provided an overview of the current approaches and techniques that have been developed in the design of antibacterial metallic implant surfaces. Metallic implant surfaces can be modified to become either antifouling or bacter icidal in nature. To achieve this, there are a number of chemical or physical modification techniques that have been developed for the fabrication of antibacterial metallic implant surfaces. In the last few decades, the surface chemical characteristics of a surface have been modified such that the resulting surface is not only antibacterial, but also biocompatible. Investigation of the cytotoxicit y and biocompatibility of such modified materials requires significant resources. One of the currently emerging approaches for determining the cytotoxicity and biocompatibility of a surface is to develop surface micro- and nano-architectures that generate repulsive forces towards bacteria (Ivanova et al. 2012, 2013; Hasan et al. 2013). These techniques have proven to be a good starting point for the innovative design of metallic biomaterials, and represent an alternative approach to the methods that have traditionally been adopted. To date, only a limited number of studies have been performed to address these issues (Ivanova et al. 2012, 2013; Fadeeva et al. 2011). These recently developed methods for modifying the nanotopography of surfaces may prove to be very useful techniques for the fabrication of a new generation of antifouling or bactericidal b io materials.
References
Andani MT, Shayesteh Moghaddam N, Haberland C, Dean D, Miller MJ, Elahinia M (2014) Metals for bone implants. Part 1. Powder metallurgy and implant rendering. Acta Biomater 10(10):4058–4070. doi:10.1016/j.actbio.2014.06.025
Anselme K, Davidson P, Popa AM, Giazzon M, Liley M, Ploux L (2010) The interaction of cells and bacteria with surfaces structured at the nanometre scale. Acta Biomater 6(10):3824–3846. doi:10.1016/j.actbio.2010.04.001
Antoci V, King SB, Jose B, Parvizi J, Zeiger AR, Wickstrom E, Freeman TA, Composto RJ, Ducheyne P, Shapiro IM (2007) Vancomycin covalently bonded to titanium alloy prevents bacterial colonization. J Orthop Res 25(7):858–866. doi:10.1002/jor.20348
Arciola CR, Radin L, Alvergna P, Cenni E, Pizzoferrato A (1993) Heparin surface treatment of poly(methylmethacrylate) alters adhesion of a Staphylococcus aureus strain: utility of bacterial fatty acid analysis. Biomaterials 14(15):1161–1164. doi:10.1016/0142-9612(93)90161-T
Arciola CR, Bustanji Y, Conti M, Campoccia D, Baldassarri L, Samorì B, Montanaro L (2003) Staphylococcus epidermidis-fibronectin binding and its inhibition by heparin. Biomaterials 24(18):3013–3019. doi:10.1016/S0142-9612(03)00133-9
Arciola CR, Campoccia D, Speziale P, Montanaro L, Costerton JW (2012) Biofilm formation in Staphylococcus implant infections. A review of molecular mechanisms and implications for biofilm-resistant materials. Biomaterials 33(26):5967–5982. doi:10.1016/j.biomaterials.2012.05.031
Aslan S, Deneufchatel M, Hashmi S, Li N, Pfefferle LD, Elimelech M, Pauthe E, Van Tassel PR (2012) Carbon nanotube-based antimicrobial biomaterials formed via layer-by-layer assembly with polypeptides. J Colloid Interface Sci 388(1):268–273. doi:10.1016/j.jcis.2012.08.025
Aslan S, Määttä J, Haznedaroglu BZ, Goodman JP, Pfefferle LD, Elimelech M, Pauthe E, Sammalkorpi M, Van Tassel PR (2013) Carbon nanotube bundling: influence on layer-by-layer assembly and antimicrobial activity. Soft Matter 9(7):2136–2144. doi:10.1002/adma.201001215
Bayston R, Vera L, Mills A, Ashraf W, Stevenson O, Howdle SM (2010) In vitro antimicrobial activity of silver-processed catheters for neurosurgery. J Antimicrob Chemother 65(2):258–265. doi:10.1093/jac/dkp420
Bazaka K, Jacob MV, Truong VK, Wang F, Pushpamali WAA, Wang JY, Ellis AV, Berndt CC, Crawford RJ, Ivanova EP (2010) Plasma-enhanced synthesis of bioactive polymeric coatings from monoterpene alcohols: a combined experimental and theoretical study. Biomacromolecules 11(8):2016–2026. doi:10.1021/bm100369n
Bazaka K, Jacob MV, Crawford RJ, Ivanova EP (2011a) Plasma-assisted surface modification of organic biopolymers to prevent bacterial attachment. Acta Biomater 7(5):2015–2028. doi:10.1016/j.actbio.2010.12.024
Bazaka K, Jacob MV, Truong VK, Crawford RJ, Ivanova EP (2011b) The effect of polyterpenol thin film surfaces on bacterial viability and adhesion. Polymer 3(1):388–404. doi:10.3390/polym3010388
Bazaka K, Jacob MV, Crawford RJ, Ivanova EP (2012) Efficient surface modification of biomaterial to prevent biofilm formation and the attachment of microorganisms. Appl Microbiol Biotechnol 95(2):299–311. doi:10.1007/s00253-012-4144-7
Bozic KJ, Ries MD (2005) The impact of infection after total hip arthroplasty on hospital and surgeon resource utilization. J Bone Joint Surg Ser A 87(8):1746–1751. doi:10.2106/JBJS.D.02937
Brouwer CPJM, Rahman M, Welling MM (2011) Discovery and development of a synthetic peptide derived from lactoferrin for clinical use. Peptides 32(9):1953–1963. doi:10.1016/j.peptides.2011.07.017
Busscher HJ, Van Der Mei HC, Subbiahdoss G, Jutte PC, Van Den Dungen JJAM, Zaat SAJ, Schultz MJ, Grainger DW (2012) Biomaterial-associated infection: locating the finish line in the race for the surface. Sci Transl Med 4(153):153rv110. doi:10.1126/scitranslmed.3004528
Bustanji Y, Arciola CR, Conti M, Mandello E, Montanaro L, Samorí B (2003) Dynamics of the interaction between a fibronectin molecule and a living bacterium under mechanical force. Proc Natl Acad Sci U S A 100(23):13292–13297. doi:10.1073/pnas.1735343100
Çalışkan N, Bayram C, Erdal E, Karahaliloğlu Z, Denkbaş EB (2014) Titania nanotubes with adjustable dimensions for drug reservoir sites and enhanced cell adhesion. Mater Sci Eng C 35:100–105. doi:10.1016/j.msec.2013.10.033
Campoccia D, Montanaro L, Arciola CR (2013a) A review of the biomaterials technologies for infection-resistant surfaces. Biomaterials 34(34):8533–8554. doi:10.1016/j.biomaterials.2013.07.089
Campoccia D, Montanaro L, Arciola CR (2013b) A review of the clinical implications of anti-infective biomaterials and infection-resistant surfaces. Biomaterials 34(33):8018–8029. doi:10.1016/j.biomaterials.2013.07.048
Chang Y-Y, Huang H-L, Chen Y-C, Weng J-C, Lai C-H (2013) Characterization and antibacterial performance of ZrNO–Ag coatings. Surf Coat Technol 231:224–228. doi:10.1016/j.surfcoat.2012.05.084
Chen X, Sevilla P, Aparicio C (2013) Surface biofunctionalization by covalent co-immobilization of oligopeptides. Colloids Surf B: Biointerfaces 107:189–197. doi:10.1016/j.colsurfb.2013.02.005
Chennell P, Feschet-Chassot E, Devers T, Awitor KO, Descamps S, Sautou V (2013) In vitro evaluation of TiO2 nanotubes as cefuroxime carriers on orthopaedic implants for the prevention of periprosthetic joint infections. Int J Pharm 455(1–2):298–305. doi:10.1016/j.ijpharm.2013.07.014
Chua PH, Neoh KG, Kang ET, Wang W (2008) Surface functionalization of titanium with hyaluronic acid/chitosan polyelectrolyte multilayers and RGD for promoting osteoblast functions and inhibiting bacterial adhesion. Biomaterials 29(10):1412–1421. doi:10.1016/j.biomaterials.2007.12.019
Chun MJ, Shim E, Kho EH, Park KJ, Jung J, Kim JM, Kim B, Lee KH, Cho DL, Bai DH, Lee SI, Hwang HS, Ohk SH (2007) Surface modification of orthodontic wires with photocatalytic titanium oxide for its antiadherent and antibacterial properties. Angle Orthod 77(3):483–488. doi:10.2319/0003-3219(2007)077[0483:SMOOWW]2.0.CO;2
Cipriano AF, Miller C, Liu H (2014) Anodic growth and biomedical applications of TiO2 nanotubes. J Biomed Nanotechnol 10(10):2977–3003. doi:10.1166/jbn.2014.1927
Crawford RJ, Webb HK, Truong VK, Hasan J, Ivanova EP (2012) Surface topographical factors influencing bacterial attachment. Adv Colloid Interf Sci 179–182:142–149. doi:10.1016/j.cis.2012.06.015
Crick CR, Ismail S, Pratten J, Parkin IP (2011) An investigation into bacterial attachment to an elastomeric superhydrophobic surface prepared via aerosol assisted deposition. Thin Solid Films 519(11):3722–3727. doi:10.1016/j.tsf.2011.01.282
Cui FZ, Luo ZS (1999) Biomaterials modification by ion-beam processing. Surf Coat Technol 112(1–3):278–285. doi:10.1016/S0257-8972(98)00763-4
Cui C, Gao X, Qi Y, Liu S, Sun J (2012a) Microstructure and antibacterial property of in situ TiO2 nanotube layers/titanium biocomposites. J Mech Behav Biomed Mater 8:178–183. doi:10.1016/j.jmbbm.2012.01.004
Cui Y, Zhao Y, Tian Y, Zhang W, Lü X, Jiang X (2012b) The molecular mechanism of action of bactericidal gold nanoparticles on Escherichia coli. Biomaterials 33(7):2327–2333. doi:10.1016/j.biomaterials.2011.11.057
Dastjerdi R, Montazer M (2010) A review on the application of inorganic nano-structured materials in the modification of textiles: focus on anti-microbial properties. Colloids Surf B: Biointerfaces 79(1):5–18. doi:10.1016/j.colsurfb.2010.03.029
Davies D (2003) Understanding biofilm resistance to antibacterial agents. Nat Rev Drug Discov 2(2):114–122. doi:10.1038/nrd1008
De Villiers MM, Otto DP, Strydom SJ, Lvov YM (2011) Introduction to nanocoatings produced by layer-by-layer (LbL) self-assembly. Adv Drug Deliv Rev 63(9):701–715. doi:10.1016/j.addr.2011.05.011
Decher G (1997) Fuzzy nanoassemblies: toward layered polymeric multicomposites. Science 277(5330):1232–1237. doi:10.1126/science.277.5330.1232
Dong Y, Li X, Tian L, Bell T, Sammons R, Dong H (2011) Towards long-lasting antibacterial stainless steel surfaces by combining double glow plasma silvering with active screen plasma nitriding. Acta Biomater 7(1):447–457. doi:10.1016/j.actbio.2010.08.009
Dueland R, Spadaro JA, Rahn BA (1982) Silver antibacterial bone cement. Comparison with gentamicin in experimental osteomyelitis. Clin Orthop Relat Res 169:264–268
Elnathan R, Kwiat M, Patolsky F, Voelcker NH (2014) Engineering vertically aligned semiconductor nanowire arrays for applications in the life sciences. Nano Today 9(2):172–196. doi:10.1016/j.nantod.2014.04.001
Fadeeva E, Truong VK, Stiesch M, Chichkov BN, Crawford RJ, Wang J, Ivanova EP (2011) Bacterial retention on superhydrophobic titanium surfaces fabricated by femtosecond laser ablation. Langmuir 27(6):3012–3019. doi:10.1021/la104607g
Foster TJ, Höök M (1998) Surface protein adhesins of Staphylococcus aureus. Trends Microbiol 6(12):484–488. doi:10.1016/S0966-842X(98)01400-0
Foster TJ, Geoghegan JA, Ganesh VK, Höök M (2014) Adhesion, invasion and evasion: the many functions of the surface proteins of Staphylococcus aureus. Nat Rev Microbiol 12(1):49–62. doi:10.1038/nrmicro3161
Fox S, Wilkinson TS, Wheatley PS, Xiao B, Morris RE, Sutherland A, Simpson AJ, Barlow PG, Butler AR, Megson IL, Rossi AG (2010) NO-loaded Zn2+-exchanged zeolite materials: a potential bifunctional anti-bacterial strategy. Acta Biomater 6(4):1515–1521. doi:10.1016/j.actbio.2009.10.038
Fusetani N (2004) Biofouling and antifouling. Nat Prod Rep 21(1):94–104. doi:10.1039/b302231p
Fusetani N (2011) Antifouling marine natural products. Nat Prod Rep 28(2):400–410. doi:10.1039/c0np00034e
Gabriel M, Nazmi K, Veerman EC, Amerongen AVN, Zentner A (2006) Preparation of LL-37-grafted titanium surfaces with bactericidal activity. Bioconjug Chem 17(2):548–550. doi:10.1021/bc050091v
Gadenne V, Lebrun L, Jouenne T, Thebault P (2013) Antiadhesive activity of ulvan polysaccharides covalently immobilized onto titanium surface. Colloids Surf B: Biointerfaces 112(0):229–236. doi:10.1016/j.colsurfb.2013.07.061
Gerberich BG, Bhatia SK (2013) Tissue scaffold surface patterning for clinical applications. Biotechnol J 8(1):73–84. doi:10.1002/biot.201200131
Glinel K, Thebault P, Humblot V, Pradier C-M, Jouenne T (2012) Antibacterial surfaces developed from bio-inspired approaches. Acta Biomater 8(5):1670–1684. doi:10.1016/j.actbio.2012.01.011
Godoy-Gallardo M, Mas-Moruno C, Fernández-Calderón MC, Pérez-Giraldo C, Manero JM, Albericio F, Gil FJ, Rodríguez D (2014) Covalent immobilization of hLf1-11 peptide on a titanium surface reduces bacterial adhesion and biofilm formation. Acta Biomater 10(8):3522–3534. doi:10.1016/j.actbio.2014.03.026
Gong SQ, Niu LN, Kemp LK, Yiu CKY, Ryou H, Qi YP, Blizzard JD, Nikonov S, Brackett MG, Messer RLW, Wu CD, Mao J, Bryan Brister L, Rueggeberg FA, Arola DD, Pashley DH, Tay FR (2012) Quaternary ammonium silane-functionalized, methacrylate resin composition with antimicrobial activities and self-repair potential. Acta Biomater 8(9):3270–3282. doi:10.1016/j.actbio.2012.05.031
Gordon O, Slenters TV, Brunetto PS, Villaruz AE, Sturdevant DE, Otto M, Landmann R, Fromm KM (2010) Silver coordination polymers for prevention of implant infection: thiol interaction, impact on respiratory chain enzymes, and hydroxyl radical induction. Antimicrob Agents Chemother 54(10):4208–4218. doi:10.1128/AAC.01830-09
Grinthal A, Aizenberg J (2014) Mobile interfaces: liquids as a perfect structural material for multifunctional, antifouling surfaces. Chem Mater 26(1):698–708. doi:10.1021/cm402364d
Gristina AG (1987) Biomaterial-centered infection: microbial adhesion versus tissue integration. Science 237(4822):1588–1595. doi:10.1126/science.3629258
Gristina AG, Naylor P, Myrvik Q (1988) Infections from biomaterials and implants: a race for the surface. Med Prog Technol 14(3–4):205–224
Hajipour MJ, Fromm KM, Akbar Ashkarran A, Jimenez de Aberasturi D, Larramendi IRD, Rojo T, Serpooshan V, Parak WJ, Mahmoudi M (2012) Antibacterial properties of nanoparticles. Trends Biotechnol 30(10):499–511. doi:10.1016/j.tibtech.2012.06.004
Hammond PT (1999) Recent explorations in electrostatic multilayer thin film assembly. Curr Opin Colloid Interface Sci 4(6):430–442. doi:10.1016/S1359-0294(00)00022-4
Hammond PT (2004) Form and function in multilayer assembly: new applications at the nanoscale. Adv Mater 16(15):1271–1293. doi:10.1002/adma.200400760
Harris LG, Tosatti S, Wieland M, Textor M, Richards RG (2004) Staphylococcus aureus adhesion to titanium oxide surfaces coated with non-functionalized and peptide-functionalized poly(L-lysine)-grafted- poly(ethylene glycol) copolymers. Biomaterials 25(18):4135–4148. doi:10.1016/j.biomaterials.2003.11.033
Hasan J, Crawford RJ, Ivanova EP (2013) Antibacterial surfaces: the quest for a new generation of biomaterials. Trends Biotechnol 31(5):295–304. doi:10.1016/j.tibtech.2013.01.017
Hauck CR, Agerer F, Muenzner P, Schmitter T (2006) Cellular adhesion molecules as targets for bacterial infection. Eur J Cell Biol 85(3–4):235–242. doi:10.1016/j.ejcb.2005.08.002
Hebeish A, Abdelhady M, Youssef A (2013) TiO2 nanowire and TiO2 nanowire doped Ag-PVP nanocomposite for antimicrobial and self-cleaning cotton textile. Carbohydr Polym 91(2):549–559. doi:10.1016/j.carbpol.2012.08.068
Heidenau F, Mittelmeier W, Detsch R, Haenle M, Stenzel F, Ziegler G, Gollwitzer H (2005) A novel antibacterial titania coating: metal ion toxicity and in vitro surface colonization. J Mater Sci Mater Med 16(10):883–888. doi:10.1007/s10856-005-4422-3
Hempel F, Finke B, Zietz C, Bader R, Weltmann K-D, Polak M (2014) Antimicrobial surface modification of titanium substrates by means of plasma immersion ion implantation and deposition of copper. Surf Coat Technol. doi:10.1016/j.surfcoat.2014.01.027
Hoene A, Prinz C, Walschus U, Lucke S, Patrzyk M, Wilhelm L, Neumann HG, Schlosser M (2013) In vivo evaluation of copper release and acute local tissue reactions after implantation of copper-coated titanium implants in rats. Biomed Mater 8(3):035009. doi:10.1088/1748-6041/8/3/035009
Høiby N, Bjarnsholt T, Givskov M, Molin S, Ciofu O (2010) Antibiotic resistance of bacterial biofilms. Int J Antimicrob Agents 35(4):322–332. doi:10.1016/j.ijantimicag.2009.12.011
Holmberg KV, Abdolhosseini M, Li Y, Chen X, Gorr SU, Aparicio C (2013) Bio-inspired stable antimicrobial peptide coatings for dental applications. Acta Biomater 9(9):8224–8231. doi:10.1016/j.actbio.2013.06.017
Hu X, Neoh KG, Shi Z, Kang ET, Poh C, Wang W (2010) An in vitro assessment of titanium functionalized with polysaccharides conjugated with vascular endothelial growth factor for enhanced osseointegration and inhibition of bacterial adhesion. Biomaterials 31(34):8854–8863. doi:10.1016/j.biomaterials.2010.08.006
Huo K, Zhang X, Wang H, Zhao L, Liu X, Chu PK (2013) Osteogenic activity and antibacterial effects on titanium surfaces modified with Zn-incorporated nanotube arrays. Biomaterials 34(13):3467–3478. doi:10.1016/j.biomaterials.2013.01.071
Ip M, Lui SL, Poon VK, Lung I, Burd A (2006) Antimicrobial activities of silver dressings: an in vitro comparison. J Med Microbiol 55(1):59–63. doi:10.1099/jmm.0.46124-0
Ivanova EP, Hasan J, Truong VK, Wang JY, Raveggi M, Fluke C, Crawford RJ (2011) The influence of nanoscopically thin silver films on bacterial viability and attachment. Appl Microbiol Biotechnol 91(4):1149–1157. doi:10.1007/s00253-011-3195-5
Ivanova EP, Hasan J, Webb HK, Truong VK, Watson GS, Watson JA, Baulin VA, Pogodin S, Wang JY, Tobin MJ, Löbbe C, Crawford RJ (2012) Natural bactericidal surfaces: mechanical rupture of Pseudomonas aeruginosa cells by cicada wings. Small 8(16):2489–2494. doi:10.1002/smll.201200528
Ivanova EP, Hasan J, Webb HK, Gervinskas G, Juodkazis S, Truong VK, Wu AHF, Lamb RN, Baulin VA, Watson GS, Watson JA, Mainwaring DE, Crawford RJ (2013) Bactericidal activity of black silicon. Nat Commun 4:2838. doi:10.1038/ncomms3838
Jahed Z, Molladavoodi S, Seo BB, Gorbet M, Tsui TY, Mofrad MRK (2014) Cell responses to metallic nanostructure arrays with complex geometries. Biomaterials 35(34):9363–9371. doi:10.1016/j.biomaterials.2014.07.022
Jeon H, Simon CG, Kim G (2014) A mini‐review: cell response to microscale, nanoscale, and hierarchical patterning of surface structure. J Biomed Mater Res B Appl Biomater 102(7):1580–1594
Joo Y-K, Zhang S-H, Yoon J-H, Cho T-Y (2009) Optimization of the adhesion strength of arc ion plating TiAlN films by the Taguchi method. Materials 2(2):699–709. doi:10.3390/ma2020699
Kang B-M, Lim Y-S (2014) Antibacterial properties of TiAgN and ZrAgN thin film coated by physical vapor deposition for medical applications. Trans Electr Electron Mater 15(5):275–278. doi:10.4313/TEEM.2014.15.5.275
Kawashita M, Tsuneyama S, Miyaji F, Kokubo T, Kozuka H, Yamamoto K (2000) Antibacterial silver-containing silica glass prepared by sol-gel method. Biomaterials 21(4):393–398. doi:10.1016/S0142-9612(99)00201-X
Kim W, Ng JK, Kunitake ME, Conklin BR, Yang P (2007) Interfacing silicon nanowires with mammalian cells. J Am Chem Soc 129(23):7228–7229. doi:10.1021/ja071456k
Lambris JD, Ricklin D, Geisbrecht BV (2008) Complement evasion by human pathogens. Nat Rev Microbiol 6(2):132–142. doi:10.1038/nrmicro1824
Lavernia C, Lee DJ, Hernandez VH (2006) The increasing financial burden of knee revision surgery in the United States. Clin Orthop Relat Res 446:221–226. doi:10.1097/01.blo.0000214424.67453.9a
Lemire JA, Harrison JJ, Turner RJ (2013) Antimicrobial activity of metals: mechanisms, molecular targets and applications. Nat Rev Microbiol 11(6):371–384. doi:10.1038/nrmicro3028
Li H, Cui Q, Feng B, Wang J, Lu X, Weng J (2013) Antibacterial activity of TiO 2 nanotubes: influence of crystal phase, morphology and Ag deposition. Appl Surf Sci 284:179–183
Li J, Liu X, Qiao Y, Zhu H, Ding C (2014) Antimicrobial activity and cytocompatibility of Ag plasma-modified hierarchical TiO2 film on titanium surface. Colloids Surf B: Biointerfaces 113:134–145. doi:10.1016/j.colsurfb.2013.08.030
Linford MR, Auch M, Möhwald H (1998) Nonmonotonic effect of ionic strength on surface dye extraction during dye-polyelectrolyte multilayer formation. J Am Chem Soc 120(1):178–182. doi:10.1021/ja972133z
Lu T, Qiao Y, Liu X (2012) Surface modification of biomaterials using plasma immersion ion implantation and deposition. Interface Focus 2(3):325–336. doi:10.1098/rsfs.2012.0003
Lv Q, Feng Q (2006) Preparation of 3-D regenerated fibroin scaffolds with freeze drying method and freeze drying/foaming technique. J Mater Sci Mater Med 17(12):1349–1356
Lv W, Luo J, Deng Y, Sun Y (2013) Biomaterials immobilized with chitosan for rechargeable antimicrobial drug delivery. J Biomed Mater Res A 101 A(2):447–455
Maddikeri RR, Tosatti S, Schuler M, Chessari S, Textor M, Richards RG, Harris LG (2008) Reduced medical infection related bacterial strains adhesion on bioactive RGD modified titanium surfaces: a first step toward cell selective surfaces. J Biomed Mater Res A 84(2):425–435. doi:10.1002/jbm.a.31323
Maury F, Mungkalasiri J, Bedel L, Emieux F, Dore J, Renaud FN (2014) Comparative study of antibacterial efficiency of M-TiO2 (M Ag, Cu) thin films grown by CVD. Key Eng Mater 617:127–130. doi:10.4028/www.scientific.net/KEM.617.127
McCloskey AP, Gilmore BF, Laverty G (2014) Evolution of antimicrobial peptides to self-assembled peptides for biomaterial applications. Pathogens 3(4):792–821. doi:10.3390/pathogens3040791
McLean RJC, Hussain AA, Sayer M, Vincent PJ, Hughes DJ, Smith TJN (1993) Antibacterial activity of multilayer silver-copper surface films on catheter material. Can J Microbiol 39(9):895–899
Mei L, Ren Y, Loontjens TJA, van der Mei HC, Busscher HJ (2012) Contact-killing of adhering streptococci by a quaternary ammonium compound incorporated in an acrylic resin. Int J Artif Organs 35(10):854–863. doi:10.5301/ijao.5000149
Meng J, Zhang P, Wang S (2014) Recent progress in biointerfaces with controlled bacterial adhesion by using chemical and physical methods. Chem Asian J 9(8):2004–2016. doi:10.1002/asia.201402200
Minagar S, Berndt CC, Wang J, Ivanova E, Wen C (2012) A review of the application of anodization for the fabrication of nanotubes on metal implant surfaces. Acta Biomater 8(8):2875–2888. doi:10.1016/j.actbio.2012.04.005
Montanaro L, Speziale P, Campoccia D, Ravaioli S, Cangini I, Pietrocola G, Giannini S, Arciola CR (2011) Scenery of Staphylococcus implant infections in orthopedics. Future Microbiol 6(11):1329–1349. doi:10.2217/fmb.11.117
Nablo BJ, Prichard HL, Butler RD, Klitzman B, Schoenfisch MH (2005) Inhibition of implant-associated infections via nitric oxide release. Biomaterials 26(34):6984–6990. doi:10.1016/j.biomaterials.2005.05.017
Neoh KG, Hu X, Zheng D, Kang ET (2012) Balancing osteoblast functions and bacterial adhesion on functionalized titanium surfaces. Biomaterials 33(10):2813–2822. doi:10.1016/j.biomaterials.2012.01.018
Nomiya K, Tsuda K, Sudoh T, Oda M (1997) Ag(I)-N bond-containing compound showing wide spectra in effective antimicrobial activities: polymeric silver(I) imidazolate. J Inorg Biochem 68(1):39–44. doi:10.1016/S0162-0134(97)00006-8
Ogaki R, Alexander M, Kingshott P (2010) Chemical patterning in biointerface science. Mater Today 13(4):22–35. doi:10.1016/S1369-7021(10)70057-2
Olson ME, Ceri H, Morck DW, Buret AG, Read RR (2002) Biofilm bacteria: formation and comparative susceptibility to antibiotics. Can J Vet Res 66(2):86–92
Paasche G, Ceschi P, Löbler M, Rösl C, Gomes P, Hahn A, Rohm HW, Sternberg K, Lenarz T, Schmitz KP, Barcikowski S, Stöver T (2011) Effects of metal ions on fibroblasts and spiral ganglion cells. J Neurosci Res 89(4):611–617. doi:10.1002/jnr.22569
Pant HR, Pant B, Sharma RK, Amarjargal A, Kim HJ, Park CH, Tijing LD, Kim CS (2013) Antibacterial and photocatalytic properties of Ag/TiO2/ZnO nano-flowers prepared by facile one-pot hydrothermal process. Ceram Int 39(2):1503–1510. doi:10.1016/j.ceramint.2012.07.097
Patti JM, Allen BL, McGavin MJ, Höök M (1994) MSCRAMM-mediated adherence of microorganisms to host tissues. Annu Rev Microbiol 48:585–617
Percival S, Bowler P, Russell D (2005) Bacterial resistance to silver in wound care. J Hosp Infect 60(1):1–7. doi:10.1016/j.jhin.2004.11.014
Pegalajar-Jurado A, Easton CD, Styan KE, McArthur SL (2014) Antibacterial activity studies of plasma polymerised cineole films. J Mater Chem B 2(31):4993–5002
Pourbaix M (1984) Electrochemical corrosion of metallic biomaterials. Biomaterials 5(3):122–134. doi:10.1016/0142-9612(84)90046-2
Prantl L, Bürgers R, Schreml S, Zellner J, Gosau M (2010) A novel antibacterial silicone implant material with short- and long-term release of copper ions. Plast Reconstr Surg 125(2):78e–80e. doi:10.1097/PRS.0b013e3181c2a708
Rautray TR, Narayanan R, Kwon TY, Kim KH (2010) Surface modification of titanium and titanium alloys by ion implantation. J Biomed Mater Res B Appl Biomater 93(2):581–591. doi:10.1002/jbm.b.31596
Richards RME (1981) Antimicrobial action of silver nitrate. Microbios 31(124):83–91
Rivero PJ, Urrutia A, Goicoechea J, Zamarreño CR, Arregui FJ, Matías IR (2011) An antibacterial coating based on a polymer/sol-gel hybrid matrix loaded with silver nanoparticles. Nanoscale Res Lett 6(1):1–7. doi:10.1186/1556-276X-6-305
Robinson JT, Jorgolli M, Shalek AK, Yoon MH, Gertner RS, Park H (2012) Vertical nanowire electrode arrays as a scalable platform for intracellular interfacing to neuronal circuits. Nat Nanotechnol 7(3):180–184. doi:10.1038/nnano.2011.249
Ruggieri MR, Hanno PM, Levin RM (1987) Reduction of bacterial adherence to catheter surface with heparin. J Urol 138(2):423–426
Salwiczek M, Qu Y, Gardiner J, Strugnell RA, Lithgow T, McLean KM, Thissen H (2014) Emerging rules for effective antimicrobial coatings. Trends Biotechnol 32(2):82–90. doi:10.1016/j.tibtech.2013.09.008
Samanovic MI, Ding C, Thiele DJ, Darwin KH (2012) Copper in microbial pathogenesis: meddling with the metal. Cell Host Microbe 11(2):106–115. doi:10.1016/j.chom.2012.01.009
Schaer TP, Stewart S, Hsu BB, Klibanov AM (2012) Hydrophobic polycationic coatings that inhibit biofilms and support bone healing during infection. Biomaterials 33(5):1245–1254. doi:10.1016/j.biomaterials.2011.10.038
Shi Z, Neoh KG, Kang ET, Poh C, Wang W (2008) Bacterial adhesion and osteoblast function on titanium with surface-grafted chitosan and immobilized RGD peptide. J Biomed Mater Res A 86(4):865–872. doi:10.1002/jbm.a.31648
Shirai T, Tsuchiya H, Shimizu T, Ohtani K, Zen Y, Tomita K (2009) Prevention of pin tract infection with titanium-copper alloys. J Biomed Mater Res B Appl Biomater 91(1):373–380. doi:10.1002/jbm.b.31412
Siedenbiedel F, Tiller JC (2012) Antimicrobial polymers in solution and on surfaces: overview and functional principles. Polymer 4(1):46–71. doi:10.3390/polym4010046
Song Z, Borgwardt L, Høiby N, Wu H, Sørensen TS, Borgwardt A (2013) Prosthesis infections after orthopedic joint replacement: the possible role of bacterial biofilms. Orthop Rev 5:e14. doi:10.4081/or.2013.e14
Stafford SL, Bokil NJ, Achard ME, Kapetanovic R, Schembri MA, McEwan AG, Sweet MJ (2013) Metal ions in macrophage antimicrobial pathways: emerging roles for zinc and copper. Biosci Rep 33(4):e00049
Subbiahdoss G, Pidhatika B, Coullerez G, Charnley M, Kuijer R, van der Mei HC, Textor M, Busscher HJ (2010) Bacterial biofilm formation versus mammalian cell growth on titanium-based mono-and bi-functional coatings. Eur Cell Mater 19:205–213
Talebian N, Doudi M, Kheiri M (2014) The anti-adherence and bactericidal activity of sol–gel derived nickel oxide nanostructure films: solvent effect. J Sol-Gel Sci Technol 69(1):172–182. doi:10.1007/s10971-013-3201-8
Trivedi P, Gupta P, Srivastava S, Jayaganthan R, Chandra R, Roy P (2014) Characterization and in vitro biocompatibility study of Ti–Si–N nanocomposite coatings developed by using physical vapor deposition. Appl Surf Sci 293(0):143–150. doi:10.1016/j.apsusc.2013.12.119
Truong VK, Webb HK, Fadeeva E, Chichkov BN, Wu AHF, Lamb R, Wang JY, Crawford RJ, Ivanova EP (2012) Air-directed attachment of coccoid bacteria to the surface of superhydrophobic lotus-like titanium. Biofouling 28(6):539–550. doi:10.1080/08927014.2012.694426
Varghese S, Elfakhri S, Sheel D, Sheel P, Bolton F, Foster H (2013) Novel antibacterial silver‐silica surface coatings prepared by chemical vapour deposition for infection control. J Appl Microbiol 115(5):1107–1116. doi:10.1111/jam.12308
Vasilev K, Cook J, Griesser HJ (2009) Antibacterial surfaces for biomedical devices. Expert Rev Med Devices 6(5):553–567. doi:10.1586/erd.09.36
Visai L, De Nardo L, Punta C, Melone L, Cigada A, Imbriani M, Arciola CR (2011) Titanium oxide antibacterial surfaces in biomedical devices. Int J Artif Organs 34(9):929–946. doi:10.5301/ijao.5000050
Wan YZ, Raman S, He F, Huang Y (2007a) Surface modification of medical metals by ion implantation of silver and copper. Vacuum 81(9):1114–1118. doi:10.1016/j.vacuum.2006.12.011
Wan YZ, Xiong GY, Liang H, Raman S, He F, Huang Y (2007b) Modification of medical metals by ion implantation of copper. Appl Surf Sci 253(24):9426–9429. doi:10.1016/j.apsusc.2007.06.031
Webb HK, Hasan J, Truong VK, Crawford RJ, Ivanova EP (2011) Nature inspired structured surfaces for biomedical applications. Curr Med Chem 18(22):3367–3375. doi:10.2174/092986711796504673
Webb HK, Crawford RJ, Ivanova EP (2014) Wettability of natural superhydrophobic surfaces. Adv Colloid Interf Sci 210:58–64. doi:10.1016/j.cis.2014.01.020
Whitehouse JD, Deborah Friedman N, Kirkland KB, Richardson WJ, Sexton DJ (2002) The impact of surgical-site infections following orthopedic surgery at a community hospital and a university hospital: adverse quality of life, excess length of stay, and extra cost. Infect Control Hosp Epidemiol 23(4):183–189. doi:10.1086/502033
Wilkinson M, Kafizas A, Bawaked SM, Obaid AY, Al-Thabaiti SA, Basahel SN, Carmalt CJ, Parkin IP (2013) Combinatorial atmospheric pressure chemical vapor deposition of graded TiO2–VO2 mixed-phase composites and their dual functional property as self-cleaning and photochromic window coatings. ACS Comb Sci 15(6):309–319
Williams JF, Worley SD (2000) Infection-resistant nonleachable materials for urologic devices. J Endourol 14(5):395–400. doi:10.1089/end.2000.14.395
Wong SY, Li Q, Veselinovic J, Kim B-S, Klibanov AM, Hammond PT (2010) Bactericidal and virucidal ultrathin films assembled layer by layer from polycationic N-alkylated polyethylenimines and polyanions. Biomaterials 31(14):4079–4087. doi:10.1016/j.biomaterials.2010.01.119
Wong CL, Tan YN, Mohamed AR (2011) A review on the formation of titania nanotube photocatalysts by hydrothermal treatment. J Environ Manag 92(7):1669–1680
Yildirimer L, Thanh NTK, Loizidou M, Seifalian AM (2011) Toxicological considerations of clinically applicable nanoparticles. Nano Today 6(6):585–607. doi:10.1016/j.nantod.2011.10.001
Yoshinari M, Oda Y, Kato T, Okuda K (2001) Influence of surface modifications to titanium on antibacterial activity in vitro. Biomaterials 22(14):2043–2048. doi:10.1016/S0142-9612(00)00392-6
Yuan S, Wan D, Liang B, Pehkonen S, Ting Y, Neoh K, Kang E (2011) Lysozyme-coupled poly (poly (ethylene glycol) methacrylate)− stainless steel hybrids and their antifouling and antibacterial surfaces. Langmuir 27(6):2761–2774. doi:10.1021/la104442f
Yue C, Kuijer R, Kaper HJ, van der Mei HC, Busscher HJ (2014) Simultaneous interaction of bacteria and tissue cells with photocatalytically activated, anodized titanium surfaces. Biomaterials 35(9):2580–2587
Zaborowska M, Welch K, Brånemark R, Khalilpour P, Engqvist H, Thomsen P, Trobos M (2014) Bacteria-material surface interactions: methodological development for the assessment of implant surface induced antibacterial effects. J Biomed Mater Res B Appl Biomater. doi:10.1002/jbm.b.33179
Zhang W, Li Y, Niu J, Chen Y (2013) Photogeneration of reactive oxygen species on uncoated silver, gold, nickel, and silicon nanoparticles and their antibacterial effects. Langmuir 29(15):4647–4651. doi:10.1021/la400500t
Zhao L, Chu PK, Zhang Y, Wu Z (2009) Antibacterial coatings on titanium implants. J Biomed Mater Res Part B Appl Biomater 91(1):470–480. doi:10.1002/jbm.b.31463
Zhao B, Van Der Mei HC, Subbiahdoss G, De Vries J, Rustema-Abbing M, Kuijer R, Busscher HJ, Ren Y (2014) Soft tissue integration versus early biofilm formation on different dental implant materials. Dent Mater 30(7):716–727. doi:10.1016/j.dental.2014.04.001
Zobrist C, Sobocinski J, Lyskawa J, Fournier D, Miri V, Traisnel M, Jimenez M, Woisel P (2011) Functionalization of titanium surfaces with polymer brushes prepared from a biomimetic RAFT agent. Macromolecules 44(15):5883–5892
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Pham, V.T.H., Bhadra, C.M., Truong, V.K., Crawford, R.J., Ivanova, E.P. (2015). Designing Antibacterial Surfaces for Biomedical Implants. In: Ivanova, E., Crawford, R. (eds) Antibacterial Surfaces. Springer, Cham. https://doi.org/10.1007/978-3-319-18594-1_6
Download citation
DOI: https://doi.org/10.1007/978-3-319-18594-1_6
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-18593-4
Online ISBN: 978-3-319-18594-1
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)