Abstract
Falls are a common and serious, but potentially preventable, problem after stroke. Avoiding falls requires balance, which is a fluid and dynamic physical skill. There are a number of perceptual, neurological, and mechanical mechanisms underlying our ability to balance, and they are complex and heterogeneous. Depending on where strokes occur in the brain, balance may be affected in different ways. It is important to identify stroke patients who are at risk of falls in order to optimize prevention, and a number of stroke-specific risk factors have been identified, but the available assessment scales have only limited sensitivity and specificity. If management of falls risk in stroke is to be effective, assessments have to identify the precise and individual mechanisms underlying balance problems, and then specific management has to be targeted at these deficits. The consequences of falls after stroke can be severe and include loss of confidence and loss of independence, as well as serious injury including fractures. Stroke patients are at greater risk of osteoporosis, particularly on the hemiplegic side, which occurs rapidly following paresis. Management of falls risk post-stroke should also include timely assessment of bone health and the associated fracture risk.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
FormalPara Key Messages-
Following a stroke, falls risk is increased over and above the falls risk associated with ageing.
-
The assessment of stroke patients who are at risk of falls should be multidisciplinary, so too should the delivery of interventions designed to prevent them.
-
Bone density is lost rapidly in the hemiparetic limb following a stroke, with resultant increased fracture risk.
-
Along with osteoporosis drug treatment, exercise, nutrition, and addressing falls risk are important strategies to reduce fracture risk.
Incidence of Falls After Stroke
Epidemiology
Falls are common at all stages after stroke. Studies have reported that between 22 and 39 % of people with stroke fall at least once during their inpatient stay in rehabilitation units, and that falls rates in stroke patients are between 3.4 and 17.8 falls per 1,000 patient days [1–5]. This compares with average fall estimates of between 2 and 7 falls per 1,000 patient days in the general inpatient population. At first glance, these numbers may seem surprisingly high. One possible explanation for this is that inpatient stays for stroke patients are of relatively long duration and the accumulated day-by-day risk over time leads to these high incidences. However, analyses of falls rates over time in inpatients lend support to the notion of added extra risk attributable to stroke. The risk of falls in stroke is not restricted to a hospital setting. At 6 months, the incidence of falls has been observed to be between 37 and 73 % [6–9] and studies that assessed falls rate in patients who had a stroke over a year previously have found higher incidences compared with non-stroke controls (36 % vs. 24 % in one study and 23 % vs. 11 % in another) [10, 11].
Circumstances of Falling
The existing literature on falls in stroke has, in many cases, taken care to analyse what people were doing and where and when they fell. Studies in inpatient acute and rehabilitation care settings [1, 4, 5, 12–14] have reported that falls commonly occur beside the bed or in the toilet/bathroom area. This may be because people spend much of their time in these areas while they are inpatients. However, these are also places where people often make transfers. Broadly similar patterns have been observed in community settings [6, 10, 11, 15, 16]. After discharge from hospital, falls occur most often during the day, and most often in the home. The lounge, bedroom, and garden are the places where falls occur most frequently and the most likely activities at the time of falling are walking or transferring.
Why Strokes Lead to Falls
Falls are common in the frail older person. Since 75 % of stroke patients are older than 65 years of age, many reasons for older people to fall impact on stroke survivors falling. Examples include generally decreased muscle strength and postural reflexes, impaired sensory systems such as vision, less dynamic blood pressure responses to changes in posture, joint disease, cognitive impairment, reduced reaction time, and incontinence. However, strokes can lead directly to falls because of the vital role almost every part of our brain plays in maintaining our balance. Balance itself is a highly complex and dynamic skill. Even when standing still, there is a constantly activated feedback loop that keeps us upright—a simple observation that underlines this fact is that everyone, when standing, exhibits a certain degree of natural postural sway. In some this is barely noticeable, and in others it is more marked (measurements of sway have been reported as a predictor of falls in older people) [17]. As we stand, our sway is continuously registered by our proprioceptive, vestibular, and visual systems. Next, the information is processed by our central nervous system. Finally, small and accurate compensatory movements occur, in particular in the muscles of the lower legs and feet, to correct the sway and restore the centre of balance to a central position.
The problem of balance as we locomote around and interact within the world is greater still. Walking and not falling is a skill that takes years to learn because it is so complex. In order to walk in a balanced way, multimodal sensory information about speed, direction, limb position, and body tilt must be combined in the brain with information about the environment, including the surface underfoot and obstacles in our way. This information is then used by the brain to produce a motor response—this has to be smooth, fluent, and precise so that as our centre of gravity pitches to and fro with every step, our legs provide just the right amount of force in exactly the right direction to keep us moving forward in an upright position. The same considerations apply to every movement we have learnt to make, from walking up a step and rising out of a chair, to getting into a car. To balance we must also be able to compensate for the unexpected—whether catching a toe on a floor-level obstacle or being pushed by an impulse at the shoulder, we can only stay on our feet by rapid and accurate corrective movements. To avoid falls we must also use our memory and executive abilities, for example: To navigate a familiar environment in poor lighting conditions such as a nocturnal visit to the bathroom, we must use spatial memory about the location of obstacles and room layout to plan the safest route.
Anterior Circulation Strokes
Hemiplegia is the most common result of a stroke in the motor cortex. If a limb is too weak, it is less likely to be able to compensate when called upon to provide a crucial extra impulse in response to an unexpected change in the centre of gravity. A weak leg is less likely to be able to maintain extension during the stance phase of walking, which can lead to buckling at the knee and a loss of stability. Decreased foot clearance during the swing phase, whether from weakness at the hip, knee, or ankle can result in tripping. A weak arm may not generally impede normal locomotion, but if someone uses a walking aid, they are recruiting their arm into helping to provide a larger base on the floor. The weaker the arm, the less stable the base and the less tolerance to unexpected forces. In a near-fall situation, it is often the arm that steadies balance, whether on a piece of furniture or a hand rail. A weak arm, in this situation, is less likely to save a person from falling.
Frontal lobe strokes may affect the prefrontal cortex and may affect executive function and lead to poor planning and initiation of movement, which would lead to unsafe mobilization and risky decisions. Also within the frontal lobe, the premotor and supplementary motor cortices have an important role in representing complex sequences of movements. If the premotor or supplementary motor cortices are affected by stroke, it could lead to an inability to execute the complex movements involved in gait and lead to instability. Gait apraxia is sometimes seen in these patients, which may also contribute to falls risk.
A stroke affecting the sensory cortex could cause problems with joint position sense on one side. If proprioception in a limb is affected, it is unlikely to be able to sense the subtle dynamic changes in joint position which must be called upon to inform our balance mechanisms. This might be especially problematic if there is an unexpected obstacle underfoot. Proprioception in the upper limbs is also important for balance because patients often need to use their arms to help with transfers, to use walking aids, or to reach out to steady themselves if they overbalance.
Strokes affecting the posterior parietal cortex can often lead to visual or sensory inattention or neglect. A patient neglecting one side is more likely to encounter unseen obstacles on that side and may trip and fall. In addition, neglect of one side can cause problems with recognition of a problem on that side, which makes rehabilitation, and the re-learning of balanced gait, difficult. Posterior parietal strokes can lead to topographical disorientation, or topographical agnosia, as the systems underlying the mental map of the environment break down. These patients may not be able to represent accurately the layout of environments, especially if they are unfamiliar. They will then be more vulnerable to falls as they encounter unfamiliar or unexpected obstacles.
Strokes affecting the deep brain structures, such as the basal ganglia, can also interrupt sensory or motor pathways, causing problems with proprioception and hemiplegia as described, or may result in extra-pyramidal symptoms of bradykinesia, stiffness, and tremor leading to a decreased ability to compensate during dynamic movements.
Posterior Circulation Strokes
If the occipital cortex is affected, or indeed any of the optic radiation, visual field deficits may result. This causes patients not to see obstacles in an aspect of their visual field; often one quadrant or one half. They may be able to compensate for this to varying degrees, partly dependent on the attention they are able to pay to the affected side. More profoundly affected may be patients with bilateral occipital cortical damage, which can result in an inability to see anything at all (although some movement perception may be preserved). This phenomenon is known as cortical blindness. These patients self-evidently will have problems seeing where they are going and be more at risk of falls. The visual pathway takes information from the optic nerves to the posterior occipital lobe, and then back into “higher order” visual processing areas in the so-called ventral and dorsal streams. The dorsal stream, which includes the superior occipital and posterior parietal lobes, is particularly involved in the perception of depth and movement. Strokes in this area can lead to impaired depth perception—these patients may have increased difficulty staying balanced in physical tasks that involve a representation of how far away something is. Examples would include stepping over an obstacle, climbing a step or over-/under-shooting a handle or bannister.
Brainstem lesions may cause hemiplegia or hemisensory loss from their interruption of ascending or descending pathways, or may cause gaze palsies resulting in difficulty tracking motion, increasing falls risk. A patient with diplopia will have problems forming the unified visual image and this may impair depth perception with an effect on falls risk as outlined above. However, the brainstem is also the centre for the integration of vital information from the vestibular system. Neurones in the vestibular portion of the eighth cranial nerve synapse at four vestibular nuclei in the superior medulla and inferior pons. From these nuclei, some motor neurons travel in the lateral vestibulospinal tract to modulate postural adjustments in a descending reflex arc. Meanwhile, many neurons travel directly to the inferior cerebellum to reach the flocculonodular node for the integration of vestibular information for eye and head control, as well as control of axial muscles for balance. Some neurones from the vestibular nuclei link directly to oculomotor nuclei to mediate the vestibulo-ocular reflex (causing our eyes to move in the opposite direction to our head to keep our visual percept stable). A stable visual percept is very important in balance as we rely heavily on “optic flow” (the expansion, contraction, or translation of an optical image on our retina) to obtain information about the movement of our head relative to the environment [18]. Patients with strokes affecting these pathways may have balance problems and exhibit saccadic abnormalities.
It may be seen, therefore, that strokes in the brainstem and cerebellum can be particularly ruinous to balance, with interruption of spinocerebellar, cerebrocerebellar, and/or vestibulocerebellar pathways leading to ataxia, incoordination, and falls.
Muscle Tone
Following a stroke, the tone in muscles may change. Too little tone, and a limb is less able to support the weight put upon it, which may lead to postural instability. Patients with low tone in a limb may not be able to provide the firm, quick impulse of a stumble, required to correct an unexpected shift of the centre of gravity. On the other hand, too much tone results in a stiff limb which cannot exercise the dynamic changes in power required to mediate balance. In addition, the postural reflexes may be affected, and there may be too strong an efferent impulse in response to stretch.
Environment
The falls risk after stroke goes beyond particular physical impairments. Very often, stroke patients are hospitalized and may spend some days in bed. During this time and despite best efforts, they may suffer deconditioning and so when they mobilize again they are less strong and less steady. Very often after a stroke, the usual environment of people changes, whether that is because they are in hospital and unused to the physical layout, or they have been moved to different rehabilitation centre, or their home has been adapted in response to their changed care needs, or in some cases because they have had to go into residential care. They may have to use equipment, such as commodes, which they have not used before. The unfamiliar environment presents new physical challenges, and these may lead to falls, particularly at a time when motor functions are being re-learnt.
Psychological Factors
Good balance and falls avoidance after stroke depend on patients maintaining a certain level of mobility and pushing themselves to learn or re-learn motor skills. Doing these things requires a certain level of psychological health, but depression is common after stroke, and depressed patients may be less inclined to take on these challenges. Another psychological consequence of stroke may be fear of falling, which can itself lead to falls in the manner described below.
Drugs
Many of the conditions associated with stroke are treated with medications that can increase patients’ falls risk. Examples include antihypertensives that can induce cerebral hypoperfusion, often worse with standing, which can lead to light-headedness and balance problems; antidepressants such as tricyclic antidepressants (TCAs) that have been associated with clinically significant orthostatic hypotension, cardiac rhythm disturbance and drowsiness; and antipsychotic drugs, used to treat agitation, that predispose to psychomotor slowing and extrapyramidal symptoms [19].
Incontinence
Urinary incontinence is common after stroke, as detailed in Chap. 8, and is a recognized risk factor for falls. This may be simply because underlying severe disability can lead to both incontinence and falls. However, if patients need to get up to go to the toilet frequently, or rush to avoid accidents, or have to change wet clothes too often, they may be at risk of falls. Further detail on this is discussed in the relevant chapter.
Assessment of Falls Risk
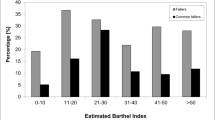
It is useful to be able to predict which patients are likely to fall and quantify individuals’ falls risk. By identifying such patients, targeted falls prevention interventions can be undertaken to help reduce risk. A number of studies have examined which patient factors are associated with falls (Tables 11.1a, b, c and d). The studies vary in methodology, findings, and conclusions and there is a dearth of randomized studies. Overall, it appears that in terms of impairments, visuospatial neglect and cognitive impairment seem to be most reliably associated with falls. Depression as a complication also seems to be an important factor. Fallers have consistently worse balance in the studies covered, and there is some data to suggest they walk slower. The data showing increased falling with lower functional performance indicates that patients’ disabilities may be more important that their impairments when it comes to falls prediction.
These observations have led some researchers to devise tools that can be used to predict falls risk based on observable patient characteristics (Table 11.2). In general, no test has been found to have excellent sensitivity and specificity for falling, but low Berg Balance scores have been found to be fairly good predictors of falling in the community (especially when combined with a history of falls) [8] and in hospital [29]. Rapport et al. [32] reported that when a falls questionnaire was combined with neuropsychological tests of impulsivity, falls could be predicted in 80 % of cases of male right middle cerebral artery territory stroke survivors in a rehabilitation setting. Nyberg et al. [34] give a scoring system that is based on the data observed in their study which correlated significantly with the fall risk, but this has not been independently validated. Part of the difficulty in devising a test to predict falls in stroke patients lies in the fact that so many different factors may contribute to falls risk. A simpler test is likely to ignore important variables, whereas a more complex one may be unwieldy.
Mitigating Falls Risk
The most compelling reason to understand and assess falls risk after stroke is to prevent people from falling. In the community-dwelling general elderly population, there is an established, evidence-based acceptance that certain interventions are effective in reducing falls. These include exercise programmes, prescribing modification programmes, interventions for visual impairment, and home safety interventions, as well as multifactorial assessments and interventions [35]. As described below, there is less evidence, however, supporting such interventions in the stroke patient population [36].
Physical Therapy and Exercises
Most stroke patients receive some form of physiotherapy and most stroke specialists would agree that physiotherapeutic interventions are key to restoring mobility and balance. After a stroke, ways of coping with deficits have to be learnt, and it is unquestionable that in many patients supervised practice of physical skills will provide benefits. Physiotherapy helps to identify impairments in dynamic function as well as the ways in which patients physically compensate for the deficits. Sometimes falls may result from the deficits themselves and sometimes from the compensatory mechanisms (e.g., over-reliance on unaffected limbs to the extent that balance is affected, known as “pusher syndrome”). Physiotherapists can help teach patients adaptive and balanced ways of mobilizing so that they can reduce their falls risk.
Physiotherapists and occupational therapists both have an important role to play in determining what patients can and cannot do safely. This is vital to prevent falls in both inpatient and community settings. By setting guidelines about what patients should be doing on their own, and what they should be doing with supervision, what aids they should be using, and what mobilisation techniques they should employ, therapists can help ensure that the falls risk is minimized as long as patients are operating on a day-to-day basis within their recommended safe levels of function. Of course, if falls do occur it is mandatory to determine whether patients were operating within these recommended safe levels, or whether they were doing something over and above what had been recommended. In the case of a patient who falls despite following recommendations, further assessments may be warranted to determine if there was another unrecognized cause of the fall. In some cases, discussion may need to take place about whether the previously agreed safe levels of function are actually still safe. Sometimes new, lower levels may need to be set, but of course this may compromise the independence of patient. The decision to do this would have to take place as part of a wider analysis of the patients’ goals and wishes as well as the overall direction of rehabilitation. Conversely, the management of a patient who falls after “giving it a go” with a risky and unrecommended manoeuvre is very different. The reasons that the patient has for taking the risk need to be sought in order to determine the approach to take. On the one hand, the patient may not be aware of the risk and require an explanation; alternatively, they might acknowledge the risk but go ahead anyway because of an urge for independence. In all these cases, an individualized approach needs to be taken, in order that the management plans can be tailor-made for each patient. In many cases, there is also a difficult balance to be struck between independence and safety.
A number of randomized controlled trials have addressed the question of whether falls can be reduced in stroke patients undergoing specific physiotherapeutic or exercise regimens. A small trial on early rehabilitation after stroke randomized 56 patients to normal care or an intervention group that were mobilized in the first 24 h post-stroke [37]. This intervention proved no less safe than normal care, but the rates of falls over the following year were no different. As previously discussed, falls are commonly seen while transferring. A study of 48 patients compared usual inpatient rehabilitation with a group who received extra sit-to-stand practice [38]. Although the intervention group’s sit-to-stand performance and quality of life improved, their falls rate remained unchanged. Another research group [39] gave patients a rehabilitation programme that included sit-to-stand training as well as training with a biofeedback device aimed at improving postural symmetry. Out of their 54 participants, they found that the intervention group suffered significantly fewer falls than the controls who underwent a conventional rehabilitation programme (42 % vs. 17 %, p < 0.05).
A larger study [40] randomized 146 patients with mobility problems over a year after a stroke to receive either community physiotherapy or no intervention. At 6 and 9 months, the intervention group had slightly better mobility and gait speed than the control group, but around 20 % of patients in both groups had fallen by these time points. Another community study [41] randomly assigned 61 patients to receiving either supervised agility training or Tai-Chi like stretching and weight-shifting practice. Even though the agility group fell less than the stretching/weight-shifting group (25 falls vs. 75 falls), this difference did not reach significance (p = 0.2). The agility group, whose training involved experimenter-induced standing perturbations, suffered significantly fewer falls on an unexpectedly moving platform. Yelnik et al. and Duncan et al. independently showed that falls were not reduced by a multi-sensorial approach to rehabilitation that included visual deprivation during exercise or by employing body-weight supported treadmill practice in place of home exercise including balance training [42, 43]. The latter study did, however, find significantly fewer falls in severely slow walkers who had balance training at home.
Medications
As previously discussed, commonly prescribed medications such as antihypertensives, antidepressants, sedatives, and other psychoactive drugs can predispose to falls. Some medications, however, may actually help decrease risk. Studies have demonstrated reduced falls rate and risk with vitamin D provision to patients with low vitamin D levels [44]. This may be mediated by the effect that vitamin D has on increasing muscle protein synthesis and thereby enhancing muscle strength. A further study showed an even greater reduction in falling from alendronate therapy compared with vitamin D therapy [45]. These findings have not however been replicated, and the putative mechanisms of a falls risk reduction with bisphosphonates are not clear [46, 47].
Interventions for Visual Impairment
Whilst randomized controlled trial data is lacking, there are a range of possible interventions for patients with visual field defects, diplopia, or other eye movement abnormalities after stroke [48]. Some are proposed to work by restoring the visual field (restitution); these aim to take advantage of the fact that patients with so-called cortical blindness can sometimes see moving objects in their affected field. Other strategies compensate for the deficit by changing behaviour, such as by training patients to scan across the visual field. Others still aim to substitute for the visual field defect by using a device or extraneous modification such as a prism. Finally, eye patches may be useful in patients who have diplopia.
Environmental Interventions and Equipment
A number of different environmental interventions are possible to try to help reduce falls risk with stroke patients. In the inpatient setting, chair alarms are sometimes used to alert nurses to patients getting up who may not be very safe to mobilize independently. Other strategies involve identifying patients at risk using alert badges at “board rounds” or alert wristbands. Inpatient environments should be well-lit with non-slippery floors and handrails that are easy to see.
Meanwhile at home, occupational therapy assessments are a key intervention in optimizing the environment to minimize falls risk. People’s homes may be messy with potential obstacles strewn on the floor. There may be slippery carpets or mats. The route to the toilet may be circuitous with bulky furniture in the way. These are things that are usually straightforward to fix. At the same time, balance may be improved with the provision of hand rails in opportune locations. Devices such as stair or bath lifts may help people who might otherwise fall at these locations. A convenient commode may also reduce long and risky trips to the bathroom. A range of other pieces of equipment usually recommended by physiotherapists may also help people’s balance after stroke. Some, such as sticks or orthoses, aid mobility and increase the physical area of people’s support base. The evidence-base for these therapy-directed interventions is extrapolated from interventions to prevent falls in older people in the absence of stroke-specific data [35, 49].
Social Environment
People who are at risk of falls may have the risk attenuated to some extent by the presence of other people to help them. For example, a common time for falls to occur is during transferring. If people have the right help and supervision at these times, whether from friends and family or formal carers, falls can be avoided.
Urinary Incontinence
Since urinary incontinence is associated with falls, and the relationship may be partly causal, it follows that managing the incontinence can help manage the falls risk. This will firstly involve assessments to uncover the precipitating factors leading to incontinence and, secondly, specific management strategies aimed at ameliorating or removing those factors. Of course, the management of incontinence, as much as the management of falls, is multidisciplinary, and very often physiotherapists and occupational therapists are invaluable in devising and practising toileting regimens to avoid incontinence after stroke.
Summary
A comprehensive evidence base from which to recommend particular interventions to reduce falls risk after stroke is lacking. It may be, however, that the evidence-based approach to falls reduction in the general older population can also be applied, to an extent, to stroke patients. This seems especially true of multifactorial interventions that are based on multifactorial risk assessments. However, not all strokes occur in older age and the stroke population has specific, separate problems and deficits that should be assessed and managed differently.
It is, however, fair to say that the first step in the management of falls risk after stroke is to identify the antecedent factors that contribute to the falls risk in that particular patient. There are many such factors and especially in stroke, different members of the multidisciplinary team have complementary roles in bringing these factors to light, according to their specialty. Just as the assessment of risk is multidisciplinary, so is its management. Patients at risk of falls after stroke will benefit from a coordinated approach to determine the most appropriate individualized interventions which can be applied by members of the different disciplines.
Consequences of Falls
Falls, when they do occur, can have severe consequences. Some are psychological, such as the development of a fear of falling, which can lead to its own complications. Others are due to injuries sustained at the time of fall, such as fractures or bleeding. People who fall and cannot get up for a long time may be at risk of hypothermia, dehydration, pressure sores, or rhabdomyolysis. There is a burden on carers of patients who fall and falls may lead to more stress for carers. Falls can lead to patients restricting the activities they do, and a resultant loss of independence. This can lead to reduced quality of life.
Fear of Falling
Fear of falling is increasingly recognized as an important determinant of morbidity after falling. It refers to anxiety about falling that may have been caused by a fall that actually occurred, or may just be a result of a general sense of imbalance. It affects people in a number of different ways. Firstly, there is the psychological burden of the anxiety. However, the mental state itself can also cause physical problems. If someone is afraid of falling they are less likely to attempt to mobilize; their mobility and balance then deteriorates, and, as a consequence, their fear of falling increases and becomes more justified.
Fear of falling often has functional consequences as well. People with fear of falling (or indeed with falls regardless of their emotional response) may try to do less around the house, with a resulting loss of independence. They may go out less and give up previously enjoyed activities or lose touch with their social network. These changes may have a profound impact on a patient’s quality of life. There is a possibility this could lead to poorer mental health and depression (although studies have only established a correlation and not a causal link between fear of falling and depression).
In stroke research, studies have shown correlations (again, not causal relationships) between fear of falling and indices of quality of life, depression, and anxiety [50]. Fear of falling can also hamper rehabilitation. Patients with anxieties about balance and falling may be less willing to try new compensatory mechanisms or practise recovering their mobility. This mandates an approach to stroke rehabilitation that includes consideration of patients’ psychological states, particularly with regard to their physical function. Cognitive behavioural therapy may be an invaluable tool to allow patients to learn to tackle their fear and has been shown to be effective in non-stroke patients who have fear of falling [51]. Meanwhile, exercise may have the dual benefit of increasing mobility and improving psychological health [52].
Bleeding Risk After Falling
A number of injuries can result from falling and, depending on the mechanism of the fall, bleeding may result. Such bleeding will be potentiated by the antithrombotic medications commonly prescribed to patients after ischaemic stroke. Many patients are prescribed anticoagulants for secondary stroke prevention but, despite the benefit, clinicians may be reluctant to prescribe them in patients at risk of falling because of worries about contributing to bleeding, including traumatic subdural or intracerebral haemorrhage. A number of key studies have addressed this clinical dilemma. Man-Song-Hing et al. [53] analysed data from 49 different studies examining falls, anticoagulation, and intracranial haemorrhage in non-stroke patients and calculated that a person with atrial fibrillation (AF) on warfarin would have to fall 295 or more times a year to make warfarin more risky than beneficial. This probably cannot be usefully extrapolated to stroke patients, however, as it relies on assumptions about the rates of falls which are based on non-stroke patients, and the authors only used traumatic subdural haemorrhage in their analysis of factors that would count against warfarin. Gage et al. [54] retrospectively analysed records of 1,245 Medicare beneficiaries with AF and found that patients treated with warfarin (around half) were no more likely to suffer intracranial haemorrhage, but if they did, it was more likely to be fatal. However, because of the reduction in stroke rates in the warfarin group, warfarin protected patients overall from a composite endpoint of stroke, intracranial haemorrhage, myocardial infarction, and death. It is difficult, however, to draw robust conclusions about the efficacy and safety of warfarin in fallers from this study as there is a selection bias in that patients in the study were only on warfarin because their physician thought that it would be safe and beneficial enough to prescribe and there was no standardized way of assessing falls risk; whether patients were at risk of falls or not was taken from remarks written in the notes. The BAFTA trial [55] randomized 973 over-75-year-olds with AF to either warfarin or aspirin. Patients were recruited from 200 English GP practices, but excluded if their GP found, there were clinical reasons to chose warfarin over aspirin, or vice versa. There were 24 primary events (21 strokes, two other intracranial haemorrhages, and one systemic embolus) in people assigned to warfarin and 48 primary events (44 strokes, one other intracranial haemorrhage, and three systemic emboli) in people assigned to aspirin. These data support the notion that warfarin is not associated with a high excess bleeding risk in the elderly. It should be noted that the sample in the BAFTA study is likely to have excluded some patients at high risk of falls, if their GPs used these patients’ falls risk as a reason to prefer aspirin. Donze et al. [56] studied 515 patients discharged home on warfarin for AF and found that while patients at high risk of falls (determined using a screening questionnaire) had a higher annual rate of major bleeding than those at lower risk (8 % vs. 6.8 %), this was not significant. These studies perhaps argue that extra major bleeding rates with warfarin are overestimated.
Osteoporosis and Fractures Post-Stroke
Epidemiology
Several studies have noted the higher incidence of fragility fracture (mainly hip fracture) in stroke survivors, as well as a higher prevalence of stroke history amongst series of hip fracture patients than matched controls [57–60]. Studies vary considerably in age ranges, ethnicity, methodology, and confounders, but almost all have demonstrated a risk ratio of hip fracture in stroke survivors of between 1.5 and 4 times that of the general population [57–61]. Hip fracture risk is most apparent in younger-aged stroke patients (though absolute fracture numbers are lower), with a large Swedish study from national hospital data finding an 8- to 12-fold higher risk of hip, as well as all fragility fractures, in stroke survivors under 60 years versus the age-matched general population [59]. A similar series from Scotland also found the highest odds ratio (fivefold) amongst younger female stroke survivors [60].
Apart from the devastating event of a hip fracture in any individual, younger stroke patients in particular seem to have a greater loss of independence from baseline and a greater mortality risk than similar-aged hip fractures without a prior stroke [62]. The morbidity ratio following hip fracture seems less influenced by a stroke history in older age, though remained higher than in those without [60, 63, 64]. Hip fracture is already a grave event for any older individual, with a consistent 25–30 % 1-year mortality seen in most large series [65]. The well-known female preponderance of osteoporosis and fracture risk in the general population is less striking post-stroke, with a narrowing of the gender gap in fracture prevalence [59, 60, 66]. Reasons for this are explained further below, given the specific fracture risk factors in stroke survivors, which are common to both genders. Fracture risk is highest in the early days post-stroke, waning over subsequent years [59, 60, 66]. Factors likely to contribute to this are firstly, there is a rapid decline in bone mineral density (BMD) in the immediate aftermath of a stroke, notably in the hemiparetic side, and secondly, falls risk is notably higher in the early days post-stroke.
Reasons for Increased Fracture Risk Post-Stroke
Falls
As discussed earlier in the chapter, stroke survivors are prone to frequent falls, and a fall is the leading contributor to fragility fracture post-stroke [60].
Bone Mineral Density (BMD) Reduction
Low BMD has been associated with a higher stroke risk in later life, meaning the stroke patient might already be predisposed to a higher fracture risk for reasons that are not entirely understood, but may involve shared risk factors for vascular calcification [67]. What is clear, however, is that there is a rapid and substantial decline in BMD following an acute stroke, as is the case following spinal cord injury and as seen in astronauts [57]. A key factor seems to be the sudden loss of weight-bearing stress on the skeleton, causing “disuse osteopenia.” Mechanical forces on bone are applied through both muscle forces and ground reaction forces, and loss of bone mass occurs very rapidly in their absence. From measures of BMD, bone turnover markers, and bone biopsy studies, bone loss begins almost immediately following stroke (probably due to the loss of muscle tone), progresses until 3–4 months later, and continues at a reduced pace until 1 year [57, 68–70]. There are no prospective studies looking at changes in BMD beyond 12 months, however. Any data beyond this time point comes from cross-sectional studies, but extrapolation from spinal cord-injury patients suggests that a stabilization of BMD is reached thereafter [71].
Available studies have used different modalities to measure BMD and have included patients with varying degrees of disability, making comparisons difficult [57]. Despite this, the consensus is that generally as much as 17 % of BMD is lost in the first year after a stroke vs. a usual bone loss (after peak growth) in adults of about 1–2 % per year [57, 69, 72]. Moreover, in hemiparesis, as much as 2 % of the BMD loss occurs in the first month. The degree of bone loss relates to motor disability, with those who are ambulant immediately following a stroke showing a much lesser fall in BMD [73–75]. Bone density reduction occurs predominantly on the paretic side, and upper limb is affected more than lower, due to its usually greater degree of paresis. It is the case though, that the dynamic changes in bone metabolism following hemiplegia have local as well as generalized effects on the skeleton, with an up to 4 % BMD loss seen on the non-paretic side [68, 74, 75]. Peripheral quantitative CT has gained an increasing role in looking at bone microarchitecture and has potential to overcome the deficits of dual energy X-ray absorptiometry (DXA) BMD scanning in fracture risk prediction [76]. A prospective study using this modality is currently underway in stroke survivors that may give further insight into the pathophysiology of post-stroke bone loss [77].
Loss of Mechanical Loading Effects on Bone Mass
The skeleton is constantly remodelled through life, through a balanced process of osteoblastic bone formation and osteoclastic bone resorption, which allows skeletal growth in childhood, healing following fractures, and adaptation of bone size and strength to mechanical force. This finely balanced process is influenced by numerous factors such as age, hormones, and mechanical loading. Uncoupling of the remodelling process of bone formation and resorption leads to increased resorption, development of osteoporosis, and increased fracture risk. Given that mechanical unloading is a key contributor to post-stroke osteoporosis, it is important to understand the pathophysiology in order to consider therapeutic strategies.
Though the precise mechanism of this uncoupling following removal of usual loading forces remains elusive, important scientific advances have been made in recent years. It is the osteocyte rather than the osteoblast or osteoclast that senses the mechanical load [78]. Osteocytes account for at least 90 % of bone structure throughout the skeleton and are formed from mature osteoblasts. There are numerous membrane-spanning channels within the osteocyte known as gap junctions, which allow osteocytes to connect directly with one another from deep within bone tissue, allowing rapid transmission of signals. These channels are formed by the linkage of membrane protein complexes; connexin43 (Cx43) being the most predominant one in bone. Cx43 is an important regulator of the ability of bone cells to respond to mechanical stimuli, through controlling calcium oscillations which occur in the osteocyte following mechanical loading [79, 80]. These loading forces also drive interstitial fluid through the unmineralized matrix surrounding osteocytes, enhancing flow and therefore transport of nutrients, waste, and signals between cells. The osteocyte is activated, in turn, through the actin cytoskeleton of its dendritic processes [80, 81].
The subsequent pathways that translate into altered bone mass are also not fully elucidated, but apart from calcium oscillations occurring, numerous substances are released by the osteocyte in response to mechanical loading such as nitric oxide and prostaglandins. These have an anabolic effect on osteoblast activity and may inhibit osteoclast activity [81]. The latter occurs by suppression of a cytokine produced by osteoblasts called receptor activator of nuclear factor kappa-B (RANK) ligand, which is a potent stimulator of osteoclast function. Mice lacking RANK ligand in osteocytes are protected from bone loss induced by hind-limb unloading [82], and the monoclonal antibody denosumab that is a RANK ligand inhibitor has shown significant clinical efficacy in post- menopausal osteoporosis.
Another important discovery in more recent years is of the Wnt gene signaling pathway, which has allowed much greater understanding of bone homeostasis in general, as well as in the context of mechanical loading effects [83, 84]. The term Wnt stems from a combination of “integration site 1” gene and a homology gene known as “wingless.” The Wnt gene signaling pathway has a central role in regulating development of many body organs and tissues. In bone, it is the major driver of osteoblast activity and of bone mass [85]. A Wnt protein is produced by the osteocyte and binds to a number of co-receptor complexes such as “Frizzled receptor” and low-density lipoprotein receptor-related protein (Lrp)5 located on the osteoblast. This complex, through a cytoplasmic protein called B-catenin, results in nuclear transcription of target genes for osteoblast proliferation and function. The role of inhibitors of Wnt signaling antagonists seems crucial to the development of disuse osteopenia. One such, named sclerostin, is produced by the osteocyte and prevents the formation of the Wnt complex, by competitively binding with Lrp5, thereby leading to greatly reduced osteoblast activity and bone formation. In animal studies, when osteocytes sense a mechanical load, they reduce the expression of sclerostin, whereas mechanical unloading causes decrease of Wnt signaling activity accompanied by upregulation of the Sost gene encoding for sclerostin production [84, 86]. Transgenic sclerostin-deficient mice were protected from bone loss stimulated by hindlimb suspension, implicating sclerostin as an important factor in the dramatic bone loss that occurs when weight-bearing ceases, such as in the hemiparesis setting [86]. Sclerostin levels have been measured in humans but show an inconsistent relationship with BMD. One study in women with post-stroke osteoporosis noted elevated levels, however, which were associated with low BMD [83]. The Wnt pathway is the target of several novel osteoporosis drugs in development, such as the sclerostin inhibitor rosozumab, which shows promising results in phase II trials [87].
Vitamin D/PTH/Calcium Imbalance
Vitamin D deficiency is widespread in the general population, particularly in older and housebound people. Stroke survivors with impaired mobility are more prone, as they may spend less time outdoors getting sunlight exposure [88]. The early, marked increase in osteoclastic activity following loss of mechanical load after a stroke leads to a significant increase in calcium release into the circulation, which may not be detected unless measured by serum ionized calcium or by urinary calcium excretion [57, 89]. Suppression of parathyroid hormone (PTH) then occurs in response to this, which leads to reduced renal production of 1,25 hydroxy Vitamin D (1,25 OHD3) which may further deplete Vitamin D levels in an already deficient patient. Although PTH and 1,25 OHD3 may have a role in modulating the bone response to unloading, the relationship is complex and remains unclear [90].
Nutritional Deficiencies
Apart from vitamin D and calcium, there are several other vitamins and trace elements which play a role in bone homeostasis but no clear evidence implicates them or their deficiency in osteoporosis and fracture risk in the general population other than mention of the following:
-
Vitamin K is essential for the carboxylation of two substances called matrix gla protein and osteocalcin, which are important components of healthy bone [91]. Vitamin K is stored in the liver, and stores are depleted by periods of fasting of as little as 3 days and in one small study in stroke survivors, levels were independently related to low BMD [92, 93]. In a large prospective study, women with baseline Vitamin K deficiency had higher risk of subsequent osteoporosis and hip fracture, which could be a potential contributor to post-stroke osteoporosis in a deficiency setting [94].
-
Vitamin B12 and folate deficiency lead to elevated homocysteine levels, which are associated with increased fracture risk, though low B12 and folate have not been causally associated with low bone mass or fracture risk [95]. Despite this, one small placebo-controlled study of B12 and folate supplementation in a group of very disabled stroke survivors seemed to reduce fracture risk after 2 years, but a larger trial in a less-dependent stroke population did not [96, 97]. Assessment for B12 and folate deficiency would be prudent in stroke patients, however, with bone health as well as general health in mind.
Iatrogenic Factors
Following a stroke, a patient is most likely to be prescribed a concoction of new medications, which have clear evidence of benefit for reducing future vascular risk. Not all these are without potentially harmful effects on bone health. Warfarin, being a vitamin K antagonist, may impair bone density and has a plausible biological mechanism to do so. Observational data in various cohorts, including stroke survivors, have linked warfarin with increased bone loss and fracture risk [98, 99]. More recently, however, a large prospective series of warfarin users refuted this finding [100]. The gains of warfarin therapy for stroke prevention in AF will certainly outweigh any potential fracture risk, particularly when the association is not entirely clear. The novel oral anticoagulant drugs (NOACs) do not have this inhibitory effect on the vitamin K cycle and therefore should not have this adverse effect. Unfractionated heparin, though now rarely used, leads to increased fracture risk; low molecular weight heparins seem largely free of this effect, though again are seldom used following stroke [101].
For the patient with epilepsy post-stroke, anticonvulsants are implicated in osteoporosis, mainly through impairment of vitamin D metabolism, and this largely applies to older agents such as phenytoin and carbamazepine. Newer anticonvulsants may be free from this effect but this is not entirely clear from the few studies to date [102, 103]. Proton pump inhibitors, often co-prescribed with aspirin prophylactically, are also associated with a higher fracture risk, possibly through impaired calcium absorption which is stomach acid-dependent [104, 105]. Numerous other medications relevant to the stroke patient have also been implicated as contributors to alerted bone mass and fracture risk. These include selective serotonin re-uptake inhibitor (SSRI) and serotonin/noradrenaline reuptake inhibitor (SNRI) antidepressants, antipsychotics, anxiolytics, statins, and glitazones [106]. Polypharmacy in the post-stroke setting is common and, though necessary, warrants evaluation of risk/benefit ratio in a population already at high risk of fracture.
Post-Stroke Osteoporosis Management
It is clear that in the aftermath of a stroke, the skeleton undergoes marked dynamic changes leading to accelerated loss of bone mass and increased fracture risk. Acknowledging this and addressing reversible risk factors should be part of routine, early post-stroke care, though a few international stroke guidelines make this specific recommendation [107].
Assessment
The traditional gold standard investigation for fracture risk assessment is a DXA bone density scan. In recent years, several fracture risk assessment tools have been developed to overcome the limitation of a DXA scan, given that the greatest proportion of fragility fractures occur in those who are osteopenic rather than osteoporotic. Low BMD, though a major fracture risk factor, is only one of many, including age and prior fracture, as we have discussed. FRAX® is the most commonly used risk assessment tool worldwide, but doesn’t account for stroke or immobility in its risk assessment. QFracture® is another tool that does, as a single category of prior stroke/TIA/myocardial infarction, acknowledging the association of vascular disease with increased fracture risk, but there is no specific inclusion of hemiparesis or immobilization [108]. Despite differences between the two tools, they have been shown to perform similarly at a population level [109]. Fracture risk assessment tools have limitations, in older age in particular, and none have been assessed in a stroke population specifically [110].
Interventions
Interventions can be divided into factors addressing falls risk and factors addressing bone health directly. The former is dealt with in detail in the previous section on falls post-stroke. Strategies to improve bone density include exercise, nutrition, and pharmacotherapy.
Exercise
Immobility is a leading contributor to post-stroke osteoporosis; therefore importance of weight-bearing exercise where possible is essential. In a detailed review on all post-stroke exercise regimens, three controlled trials were identified that investigated the effect on BMD [107]. There seems to be some benefit in early physiotherapy and weight-training exercise in maintaining bone density and structure on the paretic side, though more dedicated research on this area is needed. Whole-body vibration induces osteogenesis in animal studies and has shown some beneficial effects on bone in older adults, but one trial specifically in chronic stroke patients showed no beneficial effects on bone turnover markers [111].
Nutrition
Vitamin D status should be evaluated following stroke for those with paresis, given the rapid skeletal metabolic changes that occur with immobilization, as well as the likely sunlight deprivation that may follow. This practice may reduce falls as well as fracture rates [112]. Dosages and preparations of vitamin D supplied to deficient patients varied in studies, but in line with osteoporosis guidelines in general, replacement with 800–1,000 units of colecalciferol is advised, +/− calcium supplementation, bearing in mind the immobilization hypercalcaemia that may occur and existing dietary calcium intake. There have been recent concerns of increased cardiovascular risk from supplemented calcium where dietary intake is adequate, though this remains controversial [113, 114]. However, expert bone societies do advocate estimation of dietary calcium intake before supplementation [115, 116]. Single high-dose boluses of vitamin D should be avoided, as they have been linked to possible increased falls and fracture risk [117].
Vitamin deficiencies such as B12 and folate should be replaced only if low, as is usual practice. Vitamin K is rarely measured routinely and sufficient intake can be obtained from a balanced diet. Though one study from Japan found that vitamin K administration led to improved BMD in chronic stroke patients, there was no comparator group in this small cohort [118]. Soy proteins have mildly oestrogenic effects and can reduce osteoclastic and increase osteoblastic activity. Sato et al. studied the effect of the synthetic soy protein ipriflavone in hemiplegic stroke patients [119] and found it to prevent BMD decline to a greater degree than vitamin D3 or placebo. However, the study was small (n = 30 per arm), looked at metacarpal rather than axial BMD, and included both males and females. Since then, a larger placebo-controlled trial of ipriflavone in a postmenopausal population over 4 years found no beneficial effect on BMD [120] and it is not routinely recommended for fracture risk reduction, even in the post-stroke setting.
There are numerous other nutrients that may influence bone metabolism such as copper, zinc, vitamin C, and protein, but there is no firm evidence that supplementation of any will influence bone mass, even in the general population [121]. Particular attention to nutrition in the stroke survivor to achieve a healthy balanced intake is prudent for multiple reasons, including bone health.
Medication Review
In prescribing for the stroke patient who has a hemiparesis and/or immobility, it should be borne in mind the ability of certain drugs to impair bone density as mentioned above. For example, in post-stroke epilepsy, choosing a newer anticonvulsant may be wise. The need for proton pump inhibitors and SSRI antidepressants should be reviewed at regular intervals. In treating hypertension, thiazides may have a beneficial effect on the skeleton by reducing urinary calcium excretion and can enhance osteoblastic calcium uptake [122]. Frusemide, on the other hand, is associated with increased fracture risk, possibly through urinary calcium loss [122]. However, both agents may increase falls risk by reducing blood pressure, as mentioned earlier.
Bone-Sparing Pharmacotherapy
A number of bisphosphonates have been evaluated in stroke survivors. Etidronate, alendronate, and zoledronate have demonstrated attenuation of BMD reduction following hemiparetic stroke [57, 68, 123]. Risedronate has also shown to reduce hip fracture risk in Japanese male and female stroke patients [46, 47], but fracture numbers were in single figures only. No randomized trials have been conducted in Caucasian or Afro-Carribean cohorts. The anti-resorptive monoclonal antibody denosumab is a potent agent for fracture prevention in post-menopausal women, but has not so far been trialled in stroke or immobilized patients specifically. Given the marked failure of bone formation in the stroke setting, an anabolic agent such as the PTH analogue teriparatide, along with the even more potent sclerostin inhibitor rososuzamab, currently in phase III trials, has theoretical benefits in the hemiplegic stroke patient but this remains to be determined beyond animal data at present [124, 125]. Meanwhile, in stroke survivors, standard age-related osteoporosis treatment guidelines should apply, with bisphosphonates being first-line therapy until further data emerges on optimal therapeutic agents in the post-stroke setting.
Conclusion
Falls and fractures are an important cause of morbidity following a stroke. Patients are at risk of falls, both in the immediate aftermath of their illness and, subsequently, in the community. Because the control of balance and locomotion depend on the functioning of separate neuronal pathways, strokes in different locations can cause falls in a number of different ways. Falls are also caused by the complications of stroke, as well as the medications prescribed to stroke patients. The identification, assessment, and management of patients who may fall involves a multidisciplinary approach, taking into account known risk factors, performing assessments of function and disability, and providing a patient-centred approach to the mitigation of risk.
Fractures are common following a stroke because of the increased falls risk and decreased bone loading on the paretic side. The osteocyte appears to have an important role to play in mediating the changes of hemiparetic bone loss, and there are promising advances in the identification of the cellular mechanisms underlying their action. Following a stroke, patients should be assessed for their risk of osteoporosis, including identification of their co-morbidities, medications, and metabolic abnormalities that constitute risk factors for the condition. Treatment of osteoporosis is multifactorial and includes exercise, nutrition, review of medications, and bone-sparing pharmacotherapy.
Patient Questions
-
Q. Since being discharged home after my stroke, I feel very unsteady when I walk around. What can I do to reduce my risk of falling?
-
A. Reducing your falls risk involves assessments and interventions from several different members of the stroke multidisciplinary team. The physiotherapist can evaluate your gait and balance, and give you rehabilitation and exercises to improve your strength and balance. They may provide you with walking aids and, if necessary, help you with spasticity. The occupational therapist can assess you in your own home and may make recommendations to improve your safety there. Meanwhile, your doctor can help tailor your medications to reduce your risk of falling.
-
Q. I have been prescribed warfarin because of my atrial fibrillation, but I have had a fall and I am worried about the risk of bleeding. What should I do?
-
A. Decisions about taking warfarin are always difficult if someone has a fall. The multidisciplinary team can help assess your falls risk and may be able to intervene to reduce your chances of falling. For many people, even if they have had a fall, the benefits of warfarin in reducing the chance of another stroke are greater than the risks of bleeding, but it is important to come to an individual decision that is right for you, in conjunction with your doctor.
-
Q. What can be done to reduce my risk of a fracture if I fall, after a stroke?
-
A. Interventions to reduce risk of falls should also help reduce your risk of a fracture but it is also advisable that bone health is addressed separately, soon after a stroke. This will take the form of addressing your other risk factors for a fracture, such as reviewing your medications and nutritional status, and may include conducting a bone density scan. The latter may need to be repeated within a year, because bone density can decline quite quickly following a stroke, especially where there is residual limb weakness. If you are found to have osteoporosis or to have a particularly high fracture risk, there are a number of medications available which your clinician may prescribe for you to help reduce this risk.
References
Nyberg L, Gustafson Y. Patient falls in stroke rehabilitation. A challenge to rehabilitation strategies. Stroke. 1995;26:838–42.
Davenport RJ, Dennis MS, Wellwood I, Warlow CP. Complications after acute stroke. Stroke. 1996;27:415–20.
Teasell R, McRae M, Foley N, Bhardwaj A. The incidence and consequences of falls in stroke patients during inpatient rehabilitation: factors associated with high risk. Arch Phys Med Rehabil. 2002;83:329–33.
Suzuki T, Sonoda S, Misawa K, Saitoh E, Shimizu Y, Kotake T. Incidence and consequence of falls in inpatient rehabilitation of stroke patients. Exp Aging Res. 2005;31:457–69.
Chaiwanichsiri D, Jiamworakul A, Kitisomprayoonkl W. Falls among stroke patients in Thai Red Cross rehabilitation center. J Med Assoc Thai. 2006;89:S47–52.
Forster A, Young J. Incidence and consequences of falls due to stroke: a systematic inquiry. BMJ. 1995;311:83–6.
Kerse N, Parag V, Feigin VL, McNaughton H, Hackett ML, Bennett DA, et al. Auckland Regional Community Stroke (ARCOS) Study Group. Falls after stroke: results from the Auckland Regional Community Stroke (ARCOS) study, 2002–2003. Stroke. 2008;39:1890–3.
Mackintosh SF, Hill KD, Dodd KJ, Goldie PA, Culham EG. Balance score and a history of falls in hospital predict recurrent falls in the 6 months following stroke rehabilitation. Arch Phys Med Rehabil. 2006;87:1583–9.
Mackintosh SFH, Hill K, Dodd KJ, Goldie P, Culham E. Falls and injury prevention should be part of every stroke rehabilitation plan. Clin Rehabil. 2005;19:441–51.
Mackintosh SFH, Goldie P, Hill K. Falls incidence and factors associated with falling in older, community-dwelling, chronic stroke survivors (>1 year after stroke) and matched controls. Aging Clin Exp Res. 2005;17:74–81.
Jørgensen L, Engstad T, Jacobsen BK. Higher incidence of falls in long-term stroke survivors than in population controls: depressive symptoms predict falls after stroke. Stroke. 2002;33:542–7.
Tutuarima JA, van der Meulen JHP, de Haan RJ, van Straten A, Limburg M. Risk factors for falls of hospitalized stroke patients. Stroke. 1997;28:297–301.
Aizen E, Shugaev I, Lenger R. Risk factors and characteristics of falls during inpatient rehabilitation of elderly patients. Arch Gerontol Geriatr. 2007;44:1–12.
Sze KH, Wong E, Leung HY, Woo J. Falls among Chinese stroke patients during rehabilitation. Arch Phys Med Rehabil. 2001;82:1219–25.
Hyndman D, Ashburn A, Stack E. Fall events among people with stroke living in the community: circumstances of falls and characteristics of fallers. Arch Phys Med Rehabil. 2002;83:165–70.
Gücüyener D, Ugur C, Uzuner N, Özdemir G. The importance of falls in stroke patients. Ann Saudi Med. 2000;20:322–3.
Thapa PB, Gideon P, Brockman KG, Fought RL, Ray WA. Clinical and biomechanical measures of balance as fall predictors in ambulatory nursing home residents. J Gerontol A Biol Sci Med Sci. 1996;51:M239–46.
Lee DN, Lishman JR. Visual proprioceptive control of stance. J Hum Mov Stud. 1975;1:87–95.
Darowski A, Chambers SA, Chambers DJ. Antidepressants and falls in the elderly. Drugs Aging. 2009;26:381–94.
Ugur C, Gücüyener D, Uzuner N, Özkan S, Özdemir G. Characteristics of falling patients with stroke. J Neurol Neurosurg Psychiatry. 2000;69:649–51.
Hyndman D, Ashburn A. People with stroke living, in the community: attention deficits, balance, ADL ability and falls. Disabil Rehabil. 2003;25:817–22.
Belgen B, Beninato M, Sullivan PE, Narielwalla K. The association of balance capacity and falls self-efficacy with history of falling in community-dwelling people with chronic stroke. Arch Phys Med Rehabil. 2006;87:554–61.
Soyuer F, Ozturk A. The effect of spasticity, sense and walking aids in falls of people after chronic stroke. Disabil Rehabil. 2007;29:679–87.
Schmid AA, Wells CK, Concato J, Dallas MI, Lo AC, Nadeau SE, et al. Prevalence, predictors, and outcomes of poststroke falls in acute hospital setting. J Rehabil Res Dev. 2010;47:553–62.
Yates JS, Lai SM, Duncan PW, Studenski S. Falls in community-dwelling stroke survivors: an accumulated impairments model. J Rehabil Res Dev. 2002;39:385–94.
Andersson AG, Kamwendo K, Seiger A, Appleros P. How to identify potential fallers in a stroke unit: validity indexes of four test methods. J Rehabil Med. 2006;38:186–91.
Czernuszenko A. Risk factors for falls in post-stroke patients treated in a neurorehabilitation ward. Neurol Neurochir Pol. 2007;41:28–35.
Tilson JK, Wu SS, Cen SY, Feng Q, Rose DR, Behrman AL, et al. Characterizing and identifying risk for falls in the LEAPS study: a randomized clinical trial of interventions to improve walking poststroke. Stroke. 2012;43:446–52.
Maeda N, Kato J, Shimada T. Predicting the probability for fall incidence in stroke patients using the Berg Balance Scale. J Int Med Res. 2009;37:697–704.
Smith J, Forster A, Young J. Use of the ‘STRATIFY’ falls risk assessment in patients recovering from acute stroke. Age Ageing. 2006;35:138–43.
Nyberg L, Gustafson Y. Using the Downton index to predict those prone to falls in stroke rehabilitation. Stroke. 1996;27:1821–4.
Rapport LJ, Webster JS, Flemming KL, Lindberg JW, Godlewski MC, Brees JE, et al. Predictors of falls among right-hemisphere stroke patients in the rehabilitation setting. Arch Phys Med Rehabil. 1993;74:621–6.
Hyndman D, Ashburn A. Stops walking when talking as a predictor of falls in people with stroke living in the community. J Neurol Neurosurg Psychiatry. 2004;75:994–7.
Nyberg L, Gustafson Y. Fall prediction index for patients in stroke rehabilitation. Stroke. 1997;28:716–21.
Gillespie LD, Robertson MC, Gillespie WJ, Sherrington C, Gates S, Clemson LM. Interventions for preventing falls in older people living in the community. Cochrane Collab Cochrane Database Syst Rev. 2012;9:CD007146.
Batchelor FA, Mackintosh SF, Said CM, Hill KD. Falls after stroke. Int J Stroke. 2012;7:482–90.
Bernhardt J, Dewey H, Thrift A, Collier J, Donnan G. A Very Early Rehabilitation Trial for Stroke (AVERT): phase II safety and feasibility. Stroke. 2008;39:390–6.
Barreca S, Sigouin CS, Lambert C, Ansley B. Effects of extra training on the ability of stroke survivors to perform an independent sit-to-stand: a randomized controlled trial. J Geriatr Phys Ther. 2004;27:59–68.
Cheng PT, Wu SH, Liaw MY, Wong AMK, Tang FT. Symmetrical body-weight distribution training in stroke patients and its effect on fall prevention. Arch Phys Med Rehabil. 2001;82:1650–4.
Green J, Forster A, Bogle S, Young J. Physiotherapy for patients with mobility problems more than 1 year after stroke: a randomised controlled trial. Lancet. 2002;359:199–203.
Marigold DS, Eng JJ, Dawson AS, Inglis JT, Harris JE, Gylfadottir S. Exercise leads to faster postural reflexes, improved balance and mobility, and fewer falls in older persons with chronic stroke. J Am Geriatr Soc. 2005;53:416–23.
Yelnik AP, Le Breton F, Colle FM, Bonan IV, Hugeron C, Egal V, et al. Rehabilitation of balance after stroke with multisensorial training: a single-blind randomized controlled study. Neurorehabil Neural Repair. 2008;22:468–76.
Duncan PW, Sullivan KJ, Behrman AL, Azen SP, Wu SS, Nadeau SE, et al., LEAPS Investigative Team. Body-weight supported treadmill rehabilitation after stroke. N Engl J Med. 2011;364:2026–36.
Sato Y, Iwamoto J, Kanoko T, Satoh K. Low-dose vitamin D prevents muscular atrophy and reduces falls and hip fractures in women after stroke: a randomized controlled trial. Cerebrovasc Dis. 2005;20:187–92.
Sato Y, Iwamoto J, Honda Y. An open-label trial comparing alendronate and alphacalcidol in reducing falls and hip fractures in disabled stroke patients. J Stroke Cerebrovasc Dis. 2011;20:41–6.
Sato Y, Iwamoto J, Kanoko T, Satoh K. Risedronate sodium therapy for prevention of hip fracture in men 65 years or older after stroke. Arch Intern Med. 2005;165:1743–8.
Sato Y, Iwamoto J, Kanoko T, Satoh K. Risedronate therapy for prevention of hip fracture after stroke in elderly women. Neurology. 2005;64:811–6.
Pollock A, Hazelton C, Henderson CA, Angilley J, Dhillon B, Langhorne P, et al. Interventions for disorders of eye movement in patients with stroke. Cochrane Database Syst Rev. 2011;(10):CD008389.
Voigt-Radloff S, Ruf G, Vogel A, van Nes F, Hull M. Occupational therapy for elderly; evidence mapping of randomised controlled trials from 2004–2012. Z Gerontol Geriatr. 2015;48(1):52–72.
Schmid AA, Van Puymbroeck M, Knies K, Spangler-Morris C, Watts K, Damush T, et al. Fear of falling among people who have sustained a stroke: a 6-month longitudinal pilot study. J Occup Ther. 2011;65:125–32.
Zijlstra GA, van Haastregt JC, Ambergen T, van Rossum E, van Eijk JT, Tennstdet SL, et al. Effects of a multicomponent cognitive behavioral group intervention on fear of falling and activity avoidance in community-dwelling older adults: results of a randomized controlled trial. J Am Geriatr Soc. 2009;57:2020–8.
Jayakody K, Gundasa S, Hosker C. Exercise for anxiety disorders: systematic review. Br J Sports Med. 2014;48:187–96.
Man-Son-Hing M, Nichol G, Lau A, Laupacis A. Choosing antithrombotic therapy for elderly patients with atrial fibrillation who are at risk for falls. Arch Intern Med. 1999;159:677–85.
Gage BF, Birman-Deych E, Kerzner R, Radford MJ, Nilasena DS, Rich MW. Incidence of intracranial hemorrhage in patients with atrial fibrillation who are prone to fall. Am J Med. 2005;118:612–7.
Mant J, Hobbs FD, Fletcher K, Roalfe A, Fitzmauriceb D, Lip GY, et al. Midland Research Practices Network (MidReC). Warfarin versus aspirin for stroke prevention in an elderly community population with atrial fibrillation (the Birmingham Atrial Fibrillation Treatment of the Aged Study, BAFTA): a randomised controlled trial. Lancet. 2007;370:493–503.
Donze J, Clair C, Hug B, Rodoni N, Waeber G, Cornuz J, Aujesky D. Risk of falls and major bleeds in patients on oral anticoagulation therapy. Am J Med. 2012;125:773–8.
Carda S, Cisari C, Invernizzi M, Bevilacqua M. Osteoporosis after stroke: a review of the causes and potential treatments. Cerebrovasc Dis. 2009;28:191–200.
Wu CH, Liou TH, Hsiao PL, Lin YC, Chang KH. Contribution of ischemic stroke to hip fracture risk and the influence of gender difference. Arch Phys Med Rehabil. 2011;92:1987–91.
Kanis J, Oden A, Johnell O. Acute and long-term increase in fracture risk after hospitalization for stroke. Stroke. 2001;32:702–6.
Dennis MS, Lo KM, McDowall M, West T. Fractures after stroke: frequency, types, and associations. Stroke. 2002;33:728–34.
Brown DL, Morgenstern LB, Majersik JJ, Kleerekoper M, Lisabeth LD. Risk of fractures after stroke. Cerebrovasc Dis. 2008;25:95–9.
Ramnemark A, Nilsson M, Borssen B, Gustafson Y. Stroke, a major and increasing risk factor for femoral neck fracture. Stroke. 2000;31:1572–7.
Ramnemark A, Nyberg L, Borssen B, Olsson T, Gustafason Y. Fractures after stroke. Osteoporos Int. 1998;8:92–5.
Fisher A, Srikusalanukul W, Davis M, Smith P. Poststroke hip fracture: prevalence, clinical characteristics, mineral-bone metabolism, outcomes, and gaps in prevention. Stroke Res Treat. 2013;2013:641943.
Mundi S, Pindiprolu B, Simunovic N, Bhandari M. Similar mortality rates in hip fracture patients over the past 31 years. Acta Orthop. 2014;85:54–9.
Pouwels S, Lalmohamed A, Leufkens B, de Boer A, Cooper C, van Staa T, et al. Risk of hip/femur fracture after stroke: a population-based case-control study. Stroke. 2009;40:3281–5.
Myint PK, Clark AB, Kwok CS, Loke YK, Yeong JK, Luben RN, et al. Bone mineral density and incidence of stroke: European prospective investigation into cancer–Norfolk population-based study, systematic review, and meta-analysis. Stroke. 2014;45:373–82.
Poole KE, Loveridge N, Rose CM, Warburton EA, Reeve J. A single infusion of zoledronate prevents bone loss after stroke. Stroke. 2007;38:1519–25.
Hamdy RC, Moore SW, Cancellaro V, Harvill L. Long-term effect of strokes on bone mass. Am J Phys Rehabil. 1995;74:351–6.
Paker N, Bugdayci D, Tekdos D, Dere C, Kaya B. Relationship between bone turnover and bone density at the proximal femur in stroke patients. J Stroke Cerebrovasc Dis. 2009;18:139–43.
Frotzler A, Berger M, Knecht H, Eser P. Bone steady-state is established at reduced bone strength after spinal cord injury: a longitudinal study using peripheral quantitative computed tomography (pQCT). Bone. 2008;43:549–55.
Lazoura O, Groumas N, Antoniadou E, Papadaki PJ, Papadimitriou A, Thriskos P, et al. Bone mineral density alterations in upper and lower extremities 12 months after stroke measured by peripheral quantitative computed tomography and DXA. J Clin Densitom. 2008;11:511–7.
Schnitzer TJ, Harvey RL, Nack SH, Supanwanid P, Maskala-Streff L, Roth E. Bone mineral density in patients with stroke: relationship with motor impairment and functional mobility. Top Stroke Rehabil. 2012;19:436–43.
Jørgensen L, Jacobsen BK, Wilsgaard T, Magnus JH. Walking after stroke: does it matter? Changes in bone mineral density within the first 12 months after stroke. A longitudinal study. Osteoporos Int. 2000;11:381–7.
Chang KH, Liou TH, Sung JY, Wang CY, Genant HK, Chan WP. Femoral neck bone mineral density change is associated with shift in standing weight in hemiparetic stroke patients. Am J Phys Med Rehabil. 2014;93:477–85.
Kazakia GJ, Tjong W, Nirody JA, Burghardt AJ, Carballido-Gamio J, Patsch JM, Link T, Feeley BT, Ma CB. The influence of disuse on bone microstructure and mechanics assessed by HR-pQCT. Bone. 2014;63:132–40.
Borschmann K, Pang MY, Iuliano S, Churilov L, Brodtmann A, Ekinci EI, Berhardt J. Changes to volumetric bone mineral density and bone strength after stroke: a prospective study. Int J Stroke. 2015;10(3):396–9.
Tatsumi S, Ishii K, Amizuka N, Li M, Kobayashi T, Kohno K, Ito M, Takeshita S, Ikeda K. Targeted ablation of osteocytes induces osteoporosis with defective mechanotransduction. Cell Metab. 2007;5:464–75.
Buo AM, Stains JP. Gap junctional regulation of signal transduction in bone cells. FEBS Lett. 2014;588:1315–21.
Schaffler MB, Cheung WY, Majeska R, Kennedy O. Osteocytes: master orchestrators of bone. Calcif Tissue Int. 2014;94:5–24.
Klein-Nulend J, Bakker AD, Bacabac RG, Vatsa A, Weinbaum S. Mechanosensation and transduction in osteocytes. Bone. 2013;54:182–90.
Xiong J, Onal M, Jilka RL, Weinstein RS, Manolagas SC, O’Brien CA. Matrix-embedded cells control osteoclast formation. Nat Med. 2011;17:1235–41.
Gaudio A, Pennisi P, Bratengeier C, Torrisi V, Lindner B, Mangiafico RA, et al. Increased sclerostin serum levels associated with bone formation and resorption markers in patients with immobilization-induced bone loss. J Clin Endocrinol Metab. 2010;95:2248–53.
Robinson JA, Chatterjee-Kishore M, Yaworsky PJ, Cullen DM, Zhao W, Li C, et al. Wnt/beta-catenin signaling is a normal physiological response to mechanical loading in bone. J Biol Chem. 2006;281:31720–8.
Burgers TA, Williams BO. Regulation of Wnt/β-catenin signaling within and from osteocytes. Bone. 2013;54:244–9.
Spatz JM, Ellman R, Cloutier AM, Louis L, van Vliet M, Suva LJ, et al. Sclerostin antibody inhibits skeletal deterioration due to reduced mechanical loading. J Bone Miner Res. 2013;28:865–74.
McClung MR, Grauer A, Boonen S, Bolognese MA, Brown JP, Diez-Perez A, et al. Romosozumab in postmenopausal women with low bone mineral density. N Engl J Med. 2014;370:412–20.
Sato Y, Metoki N, Iwamoto J, Satoh K. Amelioration of osteoporosis and hypovitaminosis D by sunlight exposure in stroke patients. Neurology. 2003;61:338–42.
Sato Y, Kaji M, Honda Y, Hayashida N, Iwamoto J, Kanoko T, et al. Abnormal calcium homeostasis in disabled stroke patients with low 25-hydroxyvitamin D. Bone. 2004;34:710–5.
Bikle DD, Halloran BP. The response of bone to unloading. J Bone Miner Metab. 1999;17:233–44.
Seibel MJ, Robins SP, Bilezikian JP. Serum undercarboxylated osteocalcin and the risk of hip fracture. J Clin Endocrinol Metab. 1997;82:717–8.
Usui Y, Tanimura H, Nishimura N, Kobayashi N, Okanoue T, Ozawa K. Vitamin K concentrations in the plasma and liver of surgical patients. Am J Clin Nutr. 1990;51:846–52.
Sato Y, Tsuru T, Oizumi K, Kaji M. Vitamin K deficiency and osteopenia in disuse-affected limbs of vitamin D-deficient elderly stroke patients. Am J Phys Med Rehabil. 1999;78:317–22.
Feskanich D, Weber P, Willett WC, Rockett H, Booth SL, Colditz GA. Vitamin K intake and hip fractures in women: a prospective study. Am J Clin Nutr. 1999;69:74–9.
Cagnacci A, Bagni B, Zini A, Cannoletta M, Generali M, Volpe A. Relation of folates, vitamin B12 and homocysteine to vertebral bone mineral density change in postmenopausal women. A five-year longitudinal evaluation. Bone. 2008;42:314–20.
Sato Y, Honda Y, Iwamoto J, Kanoko T, Satoh K. Effect of folate and mecobalamin on hip fractures in patients with stroke: a randomized controlled trial. JAMA. 2005;293:1082–8.
Gommans J, Yi Q, Eikelboom JW, Hankey GJ, Chen C, Rodgers H, et al. The effect of homocysteine-lowering with B-vitamins on osteoporotic fractures in patients with cerebrovascular disease: substudy of VITATOPS, a randomised placebo-controlled trial. BMC Geriatr. 2013;13:88.
Sato Y, Honda Y, Kunoh H, Oizumi K. Long-term oral anticoagulation reduces bone mass in patients with previous hemispheric infarction and nonrheumatic atrial fibrillation. Stroke. 1997;28:2390–4.
Gage BF, Birman-Deych E, Radford MJ, Nilasena DS, Binder EF. Risk of osteoporotic fracture in elderly patients taking warfarin: results from the National Registry of Atrial Fibrillation 2. Arch Intern Med. 2006;166:241–6.
Misra D, Zhang Y, Peloquin C, Choi HK, Kiel DP, Neogi T. Incident long-term warfarin use and risk of osteoporotic fractures: propensity-score matched cohort of elders with new onset atrial fibrillation. Osteoporos Int. 2014;25:1677–84.
Pettilä V, Leinonen P, Markkola A, Hiilesmaa V, Kaaja R. Postpartum bone mineral density in women treated for thromboprophylaxis with unfractionated heparin or LMW heparin. Thromb Haemost. 2002;87:182–6.
Phabphal K, Geater A, Limapichat K, Sathirapanya P, Setthawatcharawanich S, Leelawattana R. Effect of switching hepatic enzyme-inducer antiepileptic drug to levetiracetam on bone mineral density, 25 hydroxyvitamin D, and parathyroid hormone in young adult patients with epilepsy. Epilepsia. 2013;54:e94–8.
Salimipour H, Kazerooni S, Seyedabadi M, Nabipour I, Nemati R, Iranpour D, et al. Antiepileptic treatment is associated with bone loss: difference in drug type and region of interest. J Nucl Med Technol. 2013;41:208–11.
Khalili H, Huang ES, Jacobson BC, Camargo Jr CA, Feskanich D, Chan AT. Use of proton pump inhibitors and risk of hip fracture in relation to dietary and lifestyle factors: a prospective cohort study. BMJ. 2012;344:e372.
Ding J, Heller DA, Ahern FM, Brown TV. The relationship between proton pump inhibitor adherence and fracture risk in the elderly. Calcif Tissue Int. 2014;94:597–607.
Colón-Emeric C, O’Connell MB, Haney E. Osteoporosis piece of multi-morbidity puzzle in geriatric care. Mt Sinai J Med. 2011;78:515–26.
Borschmann K. Exercise protects bone after stroke, or does it? A narrative review of the evidence. Stroke Res Treat. 2012;2012:103697.
Hippisley-Cox J, Coupland C. Derivation and validation of updated QFracture algorithm to predict risk of osteoporotic fracture in primary care in the United Kingdom: prospective open cohort study. BMJ. 2012;344:e3427.
Rabar S, Lau R, O’Flynn N, Li L, Barry P, Guideline Development Group. Risk assessment of fragility fractures: summary of NICE guidance. BMJ. 2012;345:e3698.
Coughlan T, Dockery F. Osteoporosis and fracture risk in older people. Clin Med. 2014;14:187–91.
Pang MY, Lau RW, Yip SP. The effects of whole-body vibration therapy on bone turnover, muscle strength, motor function, and spasticity in chronic stroke: a randomized controlled trial. Eur J Phys Rehab Med. 2013;49:439–50.
Bischoff-Ferrari HA, Shao A, Dawson-Hughes B, Hathcock J, Giovannucci E, Willett WC. Benefit-risk assessment of vitamin D supplementation. Osteoporos Int. 2010;21:1121–32.
Li K, Kaaks R, Linseisen J, Rohrmann S. Associations of dietary calcium intake and calcium supplementation with myocardial infarction and stroke risk and overall cardiovascular mortality in the Heidelberg cohort of the European Prospective Investigation into Cancer and Nutrition study (EPIC-Heidelberg). Heart. 2012;98:920–5.
Bolland MJ, Grey A, Avenell A, Gamble GD, Reid IR. Calcium supplements with or without vitamin D and risk of cardiovascular events: reanalysis of the Women’s Health Initiative limited access dataset and meta-analysis. BMJ. 2011;342:d2040.
National Osteoporosis Society. Vitamin D and bone health: a practical clinical guideline for patient management; 2013. www.nos.org.
National Osteoporosis Foundation Clinician’s Guide to Prevention and Treatment of Osteoporosis. http://nof.org/hcp/clinicians-guide.
Sanders KM, Stuart AL, Williamson EJ, Simpson JA, Kotowicz MA, Young D, et al. Annual high-dose oral vitamin D and falls and fractures in older women: a randomized controlled trial. JAMA. 2010;303:1815–22.
Sato Y, Honda Y, Kuno H, Oizumi K. Menatetrenone ameliorates osteopenia in disuse-affected limbs of vitamin D- and K-deficient stroke patients. Bone. 1998;23:291–6.
Sato Y, Kuno H, Kaji M, Saruwatari N, Oizumi K. Effect of ipriflavone on bone in elderly hemiplegic stroke patients with hypovitaminosis D. Am J Phys Med Rehabil. 1999;78:457–63.
Alexandersen P, Toussaint A, Christiansen C, Devogelaer JP, Roux C, Fechtenbaum J, et al. Ipriflavone multicenter European fracture study “ipriflavone in the treatment of postmenopausal osteoporosis: a randomized controlled trial”. JAMA. 2001;285:1482–8.
Levi S, Lagari VS. The old of diet in osteoporosis prevention and management. Curr Osteoporos Rep. 2012;10:296–302.
Ghosh M, Majumdar SR. Antihypertensive medications, bone mineral density, and fractures: a review of old cardiac drugs that provides new insights into osteoporosis. Endocrine. 2014;46:397–405.
Ikai T, Uematsu M, Eun SS, Kimura C, Hasegawa C, Miyano S. Prevention of secondary osteoporosis postmenopause in hemiplegia. Am J Phys Med Rehabil. 2001;80:169–74.
Turner RT, Evans GL, Lotinun S, Lapke PD, Iwaniec UT, Morey-Holton E. Dose-response effects of intermittent PTH on cancellous bone in hindlimb unloaded rats. J Bone Miner Res. 2007;22:64–71.
Agholme F, Isaksson H, Li X, Ke HZ, Aspenberg P. Anti-sclerostin antibody and mechanical loading appear to influence metaphyseal bone independently in rats. Acta Orthop. 2011;82:628–32.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Dockery, F., Sommerville, P.J. (2015). Falls and Osteoporosis Post-Stroke. In: Bhalla, A., Birns, J. (eds) Management of Post-Stroke Complications. Springer, Cham. https://doi.org/10.1007/978-3-319-17855-4_11
Download citation
DOI: https://doi.org/10.1007/978-3-319-17855-4_11
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-17854-7
Online ISBN: 978-3-319-17855-4
eBook Packages: MedicineMedicine (R0)