Abstract
This chapter discusses methods of single-lung ventilation using a double lumen tube, bronchial blocker, or endobronchial intubation. The postoperative management of thoracic patients is also reviewed with a focus on strategies to prevent complications. Lastly, the most common cardiac, pulmonary, and esophageal complications are summarized.
Access provided by Autonomous University of Puebla. Download chapter PDF
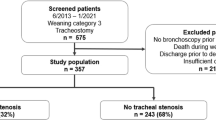
Similar content being viewed by others
Keywords
Intraoperative Considerations
-
Three main options for lung isolation during single-lung ventilation exist:
-
1.
Endobronchial intubation
-
2.
Bronchial blocker
-
3.
Double lumen tube (DLT)
-
1.
-
After sedation, diagnostic bronchoscopy is performed to identify any anatomical or pathological findings that might affect lung isolation strategies and confirm anatomy of planned bronchial resection. Final positioning of lung isolation tubes or blockers should be confirmed with fiber-optic bronchoscopy and subsequently repeated after patient re-positioning and when necessary during a thoracic operative procedure.
Double Lumen Tube (DLT)
-
DLTs are the preferred method for lung isolation.
-
Benefits include selective deflation and re-inflation of either lung, the ability to suction an independent lung prior to re-inflation, and a lower risk of dislodgment compared to other modalities.
-
Specific DLTs are available for the left and right main stem bronchi, and are available in different sizes (adults: 35—41 Fr; children: 28—32 Fr). Correct size selection of DLT requires careful review of CT scan or chest X-ray. The most accurate way to choose DLT size is based on the direct measurement of the left bronchial width using CT or chest X-ray if the left bronchus is seen [1]. If the left bronchus is not seen, size can be calculated using tracheal width [2]:
-
Tracheal width ≥18 mm: 41 Fr
-
Tracheal width ≥16 mm: 39 Fr
-
Tracheal width ≥15 mm: 37 Fr
-
Tracheal width ≥14 mm: 35 Fr
-
-
For emergency cases where imaging is not readily available, the following general guidelines can also be used [3]:
-
Male >170 cm: 41 Fr
-
Male <170 cm: 39 Fr
-
Female >160 cm: 37 Fr
-
Female <160 cm: 35 Fr
-
Endobronchial Intubation
-
Traditional endotracheal tube or a specially designed endobronchial tube is advanced into the main stem bronchi.
-
This method might be favorable in pediatric patients, or patients undergoing carinal resection.
-
Endobronchial intubation with traditional endotracheal tube should only be reserved for emergency situations due to risk of inadequate single-lung ventilation and/or failure of lung isolation.
Bronchial Blocker (BB)
-
Specially designed BBs or Fogarty vascular embolectomy catheters can be used.
-
In patients with impaired pulmonary function who cannot tolerate full independent lung collapse, a selective lobe blocking can be achieved with the combination of bronchial blockers and direct visualization using a pediatric bronchoscope.
-
BBs are also useful in patients with tracheostomy tubes or patients with difficult airway, where a double lumen tube insertion may not be feasible.
-
Dislodgment of a BB may obstruct ventilation, especially when placed on the short right main stem bronchus. This requires immediate deflation and repositioning.
Postoperative Care
Clinical Pathways (Tables 2.1 and 2.2)
-
Fast-track and enhanced recovery pathways in thoracic surgery utilizing a written, multimodal, evidence-based, step-by-step approach to perioperative care are increasingly utilized.
-
Basic principles include written daily patient education goals, smoking cessation, preoperative physiotherapy, nutrition supplementation, epidural pain control, early mobilization, early feeding, and early drain removal.
Fluid Management
-
Thoracic surgery does not induce large fluid shifts and intravascular fluid losses compared to other surgical procedures.
-
Collapse and re-expansion of lung parenchyma, heterogeneous pulmonary compliance in lateral decubitus position, elevated positive pressure ventilatory pressures, or increased pulmonary arterial pressures during single-lung ventilation may induce pulmonary edema that should be monitored and managed postoperatively.
-
Avoiding fluid overload through judicious, if not restricted, crystalloid and colloid administration intraoperatively and postoperatively is therefore critical in all thoracic patients, especially in patients with limited pulmonary reserve, or with cases requiring increasing pulmonary resection, where the remaining lung is subjected to the entire cardiac output. Fluid restriction while maintaining adequate end-organ perfusion is essential.
-
Transient hypotension and decreased urine output may be seen due to relative rather than absolute hypovolemia in patients with high thoracic epidural analgesia and should be managed with judicious fluid administration, decreasing epidural dosing as well as its concentration of local anesthetic, and occasionally using low dose vasopressor administration.
Analgesia
-
Principles of analgesia include [7]:
-
1.
Multimodal analgesia (e.g., acetaminophen, NSAID and opiate)
-
2.
Meticulous and continuous attention to each patient’s pain, while dynamically adjusting analgesia, particularly in the first 48 h
-
3.
Identifying patients at increased risk for postoperative pain
-
4.
Targeted use of epidural and intercostal blockade
-
1.
-
Thoracotomy incisions may be very painful (Fig. 2.1), impairing adequate mobilization, inspiration and expectoration, leading to atelectasis, retention of secretions, infection or worse. Inadequate analgesia contributes to a significant number of postoperative complications in these patients. Inadequate control of pain on postoperative days 1 and 2 is an independent predictor of chronic post-thoracotomy pain. It is thus imperative to control pain effectively and immediately.
-
The use of high thoracic epidural anesthesia is associated with improved pain control and decreased risk of pulmonary complications (such as pneumonia, atelectasis, prolonged mechanical ventilation, and re-intubation from respiratory failure), compared to patient-controlled analgesia and narcotic administration [8]. There is also a reduction in opioid consumption.
-
Thoracoscopic incisions are generally far less painful; however, chronic pain may occur due to levering a trocar on the rib and neurovascular bundle above. Preemptive analgesia with intercostal nerve blocks and local infiltration is an essential adjunct to multimodal oral and intravenous analgesia.
-
Over-sedation should be avoided when switching patients to oral or subcutaneous narcotics, as this may lead to subsequent hypoventilation and hypercarbia.
-
Risk factors for poor postoperative pain control include: preoperative patient preparedness, high opioid tolerance, young age, psychological factors (e.g., preoperative anxiety, depression, neuroticism), chronic pain, incision type (thoracotomy > VATS), and rib resection [9–13].
Chest Tube Management
-
Chest tubes are routinely placed in virtually all operations whereby the parietal pleura has been entered to allow for evacuation of air, detection and management of air leaks, and drainage of hemothorax, chylothorax, enteric content, or other types of pleural effusions.
-
Principles of chest tube placement include being positioned for optimal drainage (fluid: posterior and basal; air: apical and anterior), with tube caliber directed at expected output (large-bore chest tube for sanguinous fluid; pigtail for air and serous fluid).
-
Postoperatively, the patient is asked to voluntarily cough or perform a Valsalva’s maneuver and the water sealed chamber is observed for bubbles (Fig. 2.2). The fluid level in the water chamber should move up and down with deep respiration and coughing.
-
Stationary fluid level in the water seal indicates either intra-thoracic or extra-thoracic tube blockage.
-
Large swings in the fluid level indicate the presence of a large residual pleural space.
-
-
Persistent air leak can be detected by suddenly placing (or increasing) the chamber on suction and observing a sudden rush of air through the system. For patients with small air leaks, the chest tube can be clamped for a couple of hours and then unclamped while on vacuum suction to observe the sudden rush of air; however, clamping overnight is neither necessary nor advisable.
Suction:
-
Placement of chest tubes on suction rather than water seal after lung resection has not been shown to affect the duration of chest tube, duration of hospital stay, or duration of air leak. However, placing chest tube on suction is associated with a lower incidence of pneumothorax after pulmonary resection [14, 15].
-
As a principle of management, the minimal suction to achieve intended pleural drainage objectives is optimal.
-
Chest tube placed in post-pneumonectomy patients should not be on suction due to the risk of mediastinal shift and cardiac herniation.
Removal:
-
The ideal volume drainage to predict safe removal of chest tubes is unknown. 200 mL/24 h with no air leak is commonly quoted as the threshold for removal; however, there is no evidence to support this.
-
Chest tubes can be safely removed with drainage volumes of up to 500 mL/24 h without increasing the risk of fluid re-accumulation [16, 17].
-
Commonly, the target removal date of the second tube after a lobectomy is on day 3 if there is <300 mL of non-chylous fluid in 24 h with no air leak.
-
Chest tubes should be removed sequentially and each tube should be removed while off suction, with simultaneous application of an occlusive dressing to prevent air entry during its removal.
-
Respiratory Care
-
It is imperative for patients to maintain the ability to deliver an effective cough (pulmonary toilet) and to maintain good bronchial hygiene.
-
Incisional pain can lead to significant chest wall splinting, preventing proper airway clearance of secretions and mucus plugs. This is further exacerbated by a strong smoking history and chronic bronchitis.
-
Placing a pillow over the incision while coughing reduces pain.
-
-
Early ambulation, fluid restriction, aggressive pain control, chest physiotherapy, and prevention of over-sedation with narcotic medications all contribute to a better pulmonary recovery in the postoperative period.
-
Nasotracheal suctioning, flexible bronchoscopy, mechanical ventilation may be required, especially in patients with poor preoperative pulmonary function.
-
Other supportive therapies include (as necessary):
-
Humidified oxygen
-
Bronchodilators
-
N-acetylcysteine
-
Diuretics
-
High flow, high humidity oxygen
-
Postoperative Complications
-
The Thoracic Morbidity and Mortality (TM&M) classification is a system to standardize and grade the presence and severity of surgical complications after non-cardiac thoracic surgery (available at: http://www.ottawatmm.org[18])
Cardiac Complications
-
Thoracic surgery patients are at high-risk of cardiac complications due to similar risk factors (e.g., smoking).
-
The most common are myocardial ischemia, arrhythmias and heart failure.
-
All patients should undergo thorough preoperative screening for cardiac comorbidities.
Atrial Fibrillation:
-
15–40 % of all patients undergoing major thoracic surgery will develop atrial fibrillation depending on preoperative left-atrial function [19].
-
Management should address rate-control, with anticoagulation indicated after several days of refractory fibrillation, along with treatment of any precipitating factors (e.g., electrolyte imbalance—potassium and magnesium, pain, sepsis, hypoxemia, hemothorax).
Respiratory Complications
-
Most common complication after thoracic surgery.
-
Workup of patients in respiratory distress includes: chest X-ray, ECG, lab-work (CBC, serum chemistries, renal function tests, arterial blood gas, cardiac enzymes) and additional studies as necessary.
Respiratory Failure
-
Can occur secondary to multiple causes, including pneumonia, pulmonary edema, acute respiratory distress syndrome (ARDS), aspiration, mucus plug, atelectasis, heart failure, hypoventilation, sepsis, and pulmonary embolus.
-
Management should address the suspected cause(s), while providing adequate oxygenation and/or ventilatory support as required. Flexible bronchoscopy can also be done for pulmonary toilet and mucus plugs.
-
Aspiration (Fig. 2.3)
-
Most common in patients after esophagectomy secondary to vagotomy and subsequent dysmotility.
-
Early mobilization and ambulation promotes better pulmonary function and decreases incidence of aspiration.
Pulmonary Edema (Fig. 2.4)
-
Can be caused by pulmonary hypertension (increased resistance after lung resection) and impaired lymphatic drainage after lymph node dissection, favoring fluid accumulation and edema.
-
Post-pneumonectomy Syndrome:
-
Severe pulmonary edema occurring early after pneumonectomy, characterized by diffuse infiltrates, significant right-to-left shunting, and hypoxemia.
-
Presentation and management is similar to acute lung injury or ARDS—namely, minimizing lung injury (including lung-protective ventilation and avoiding over resuscitation).
-
Prolonged Air Leaks
-
Persistent air leak >5 days, frequently occur after lung resection (15 %)
-
Increases length of stay and readmissions, with substantial economic burden
-
Strategies to decrease incidence of air leaks:
-
Sealants: shown to reduce postoperative air leaks and time to chest tube removal, however not always associated with reduced hospital length-of-stay [20].
-
Routine use unlikely to be cost-effective
-
Should be considered in high-risk patients (e.g., bullectomy, severe emphysema)
-
-
Flap coverage
-
Tenting of the lung
-
Use of Bovine patch to buttress staple in high-risk patients
-
Bronchopleural Fistula (BPF)
-
Breakdown of the stump can occur secondary to ischemia, tumor recurrence, poor wound healing or empyema resulting in BPF.
-
BPFs can be hard to distinguish from persistent air leaks, but should be suspected in moderate to severe air leaks, especially in immunocompromised patients.
-
Diagnosis is confirmed by flexible bronchoscopy.
-
Hemodynamically stable patients can be initially managed conservatively by tube thoracostomy, antibiotics, and respiratory support (+/− mechanical ventilation).
-
If ventilatory support is required, airflow through the leaking stump should be minimized. This can be done using lung-isolation techniques.
-
-
Failure of conservative management mandates surgical reinforcement of the stump with a muscle flap.
Deep Vein Thrombosis (DVT) and Pulmonary Embolism
-
Thoracic patients with malignancies are at high risk for developing DVTs and pulmonary embolisms, and should be maintained on prophylactic anticoagulation throughout admission.
-
With sequential compression devices used intraoperatively, along with postoperative prophylactic anticoagulation, rates of clinically significant venous thrombosis are expected to be low (<2 %).
Thoracic Duct Injury
-
Patients undergoing extensive mediastinal dissection such as during esophagectomy are prone to duct injuries.
-
Incidence: 1–3 % post-esophagectomy [21].
-
-
Diagnosis is usually made after initiation of enteral feeding which causes an accumulation of a triglyceride-rich milky fluid in the chest cavity. See Chapter 4 : Pleural Disorders (Chylothorax)
-
Treatment of low output leaks (<1 L/day) can be done conservatively, by keeping the chest tube drainage under water seal and off vacuum suction.
-
High output thoracic duct injuries (>1 L/day) usually require surgical ligation.
-
Recent randomized controlled trial suggests that mass ligation decreases the risk of chylothorax [21].
Vocal Cord Paralysis
-
Recurrent laryngeal nerve injury can occur during esophagectomy, cervical mediastinoscopy, and mediastinal lymph node dissection.
-
Injury may lead anywhere from weak voice, hoarseness, and ineffective cough, to permanent voice loss, stridor, and acute airway obstruction.
-
Vocal cords are best assessed by visualization using a fiber-optic laryngoscope.
-
Higher rates of recurrent nerve trauma after cervical anastomosis for esophagectomy compared to thoracic anastomosis (OR 7.14, 95 % CI 1.09–10.78) [22]
Esophageal Complications
Esophageal Anastomotic Leak
-
Most leaks occur either early <48 h or after 1 week, secondary to conduit ischemia and necrosis or staple line dehiscence.
-
Early anastomotic leak (<48 h) reflects a technical complication or conduit necrosis.
-
Delayed anastomotic leak (7–10 days) reflects ischemia of the conduit.
-
-
Cervical anastomosis
-
Intrathoracic anastomosis
-
Risk factors include: cardiovascular disease (heart failure, coronary artery disease, peripheral vascular disease), smoking, use of vasopressors, location (higher risk in cervical), poor nutritional status and tension on the anastomosis [24].
-
Technical factors affecting anastomotic integrity—no difference in [25]:
-
Hand-sewn vs. stapled
-
Minimally invasive vs. open
-
Anterior vs. posterior route of reconstruction
-
Ischemic conditioning of gastric conduit
-
-
Leaks associated with reduced long-term survival after esophagectomy [26]
Diagnosis
-
Early leaks should be suspected with increase in chest tube drainage volume, drainage of enteric/bilious content, drainage of coffee ground fluid from the nasogastric tube, in addition to fever, leukocytosis, subcutaneous emphysema and signs of sepsis from mediastinitis and empyema.
-
Late anastomotic leaks present more subtly and might require esophagogastroscopy to evaluate the extent of the leak and graft ischemia.
-
Diagnosis can be confirmed by CT (with oral contrast), contrast esophagogram or esophagogastroscopy (to look for extent of leak and viability of the conduit)
-
Many centers advocate for routine contrast esophagogram prior to feeding; however, this is not a universal practice and highly controversial.
-
Many institutions perform contrast esophagogram only based on clinical suspicion, due to its low sensitivity, high false-negative rate and limited impact on patient management [27, 28].
-
Management
-
All patients: antibiotics, controlled drainage (chest tube), nutritional support (enteric), and aggressive resuscitation.
-
Early fulminant leak (<48 h): re-exploration, debridement, and revision of anastomosis.
-
Either primarily repaired, reinforced (with serratus, omentum, pericardium, or stent), or diverted with delayed reconstruction (esophagostomy spit fistula, gastrostomy, feeding jejunostomy, and colon interposition at 3–6 months) depending on time to management and degree of contamination.
-
-
Cervical anastomosis (2–10 days): leaks can be managed by opening the skin incision (to allow for drainage and assessment of gastric viability) and packing the wound.
-
Intrathoracic anastomosis (2–10 days):
-
Higher mortality rate compared to cervical anastomosis
-
Small leaks in stable patients can be managed conservatively with or without stenting for partial tissue loss
-
Large and uncontrolled leaks and conduit necrosis require re-exploration and debridement.
-
Either primarily repaired, reinforced (with serratus, omentum, pericardium or stent), or diverted with delayed reconstruction (esophagostomy spit fistula, gastrostomy, feeding jejunostomy, and colon interposition at 3–6 months) depending on time to management and degree of contamination.
-
-
-
Smaller leaks that are managed conservatively can develop strictures requiring future dilation.
Delayed Gastric Emptying
-
Occurs after significant manipulation, resection of the stomach and transaction of the vagus nerve.
-
Clinical presentation: regurgitation/vomiting, aspiration, acid reflux, early satiety
-
Barium swallow to confirm diagnosis
-
Prevention:
-
Narrow conduit
-
Avoidance of conduit redundancy or twisting
-
Adequate closure of hiatus
-
References
Brodsky JB, Lemmens HJ. Tracheal width and left double-lumen tube size: a formula to estimate left-bronchial width. J Clin Anesth. 2005;17(4):267–70.
Brodsky JB, Macario A, Mark JB. Tracheal diameter predicts double-lumen tube size: a method for selecting left double-lumen tubes. Anesth Analg. 1996;82(4):861–4.
Orlewicz MS, Coleman AE, Choromanski D, Meyers AD. Double-Lumen endotracheal tube placement. Medscape. http://emedicine.medscape.com/article/1999993-overview. Accessed 26 Jan 26 2015.
Li C et al. An enhanced recovery pathway decreases duration of stay after esophagectomy. Surgery. 2012;152(4):606–14. discussion 614-6.
Numan RC et al. A clinical audit in a multidisciplinary care path for thoracic surgery: an instrument for continuous quality improvement. Lung Cancer. 2012;78(3):270–5.
Muhling B, Orend KH, Sunder-Plassmann L. Fast track in thoracic surgery. Chirurg. 2009;80(8):706–10.
Bottiger BA, Esper SA, Stafford-Smith M. Pain management strategies for thoracotomy and thoracic pain syndromes. Semin Cardiothorac Vasc Anesth. 2014;18(1):45–56.
Popping DM et al. Protective effects of epidural analgesia on pulmonary complications after abdominal and thoracic surgery: a meta-analysis. Arch Surg. 2008;143(10):990–9. discussion 1000.
Ip HY et al. Predictors of postoperative pain and analgesic consumption: a qualitative systematic review. Anesthesiology. 2009;111(3):657–77.
Bachiocco V et al. Intensity, latency and duration of post-thoracotomy pain: relationship to personality traits. Funct Neurol. 1990;5(4):321–32.
Caumo W et al. Preoperative predictors of moderate to intense acute postoperative pain in patients undergoing abdominal surgery. Acta Anaesthesiol Scand. 2002;46(10):1265–71.
Landreneau RJ et al. Postoperative pain-related morbidity: video-assisted thoracic surgery versus thoracotomy. Ann Thorac Surg. 1993;56(6):1285–9.
Egbert LD et al. Reduction of postoperative pain by encouragement and instruction of patients. A study of doctor–patient rapport. N Engl J Med. 1964;270:825–7.
Coughlin SM, Emmerton-Coughlin HM, Malthaner R. Management of chest tubes after pulmonary resection: a systematic review and meta-analysis. Can J Surg. 2012;55(4):264–70.
Cerfolio RJ, Bass C, Katholi CR. Prospective randomized trial compares suction versus water seal for air leaks. Ann Thorac Surg. 2001;71(5):1613–7.
Cerfolio RJ, Bryant AS. Results of a prospective algorithm to remove chest tubes after pulmonary resection with high output. J Thorac Cardiovasc Surg. 2008;135(2):269–73.
Bjerregaard LS et al. Early chest tube removal after video-assisted thoracic surgery lobectomy with serous fluid production up to 500 ml/day. Eur J Cardiothorac Surg. 2014;45(2):241–6.
Seely AJ et al. Systematic classification of morbidity and mortality after thoracic surgery. Ann Thorac Surg. 2010;90(3):936–42. discussion 942.
Raman T et al. Preoperative left atrial dysfunction and risk of postoperative atrial fibrillation complicating thoracic surgery. J Thorac Cardiovasc Surg. 2012;143(2):482–7.
Belda-Sanchis J et al. Surgical sealant for preventing air leaks after pulmonary resections in patients with lung cancer. Cochrane Database Syst Rev. 2010;1, CD003051.
Lai FC et al. Prevention of chylothorax complicating extensive esophageal resection by mass ligation of thoracic duct: a random control study. Ann Thorac Surg. 2011;91(6):1770–4.
Biere SS et al. Cervical or thoracic anastomosis after esophagectomy for cancer: a systematic review and meta-analysis. Dig Surg. 2011;28(1):29–35.
Martin LW et al. Management of intrathoracic leaks following esophagectomy. Adv Surg. 2006;40:173–90.
Kassis ES et al. Predictors of anastomotic leak after esophagectomy: an analysis of the society of thoracic surgeons general thoracic database. Ann Thorac Surg. 2013;96(6):1919–26.
Markar SR et al. Technical factors that affect anastomotic integrity following esophagectomy: systematic review and meta-analysis. Ann Surg Oncol. 2013;20(13):4274–81.
Kofoed SC et al. Intrathoracic anastomotic leakage after gastroesophageal cancer resection is associated with reduced long-term survival. World J Surg. 2014;38(1):114–9.
Solomon DG, Sasaki CT, Salem RR. An evaluation of the routine use of contrast radiography as a screening test for cervical anastomotic integrity after esophagectomy. Am J Surg. 2012;203(4):467–71.
Tirnaksiz MB et al. Effectiveness of screening aqueous contrast swallow in detecting clinically significant anastomotic leaks after esophagectomy. Eur Surg Res. 2005;37(2):123–8.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Alamri, H. (2015). Operative and Postoperative Considerations. In: Madani, A., Ferri, L., Seely, A. (eds) Pocket Manual of General Thoracic Surgery. Springer, Cham. https://doi.org/10.1007/978-3-319-17497-6_2
Download citation
DOI: https://doi.org/10.1007/978-3-319-17497-6_2
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-17496-9
Online ISBN: 978-3-319-17497-6
eBook Packages: MedicineMedicine (R0)