Abstract
Several investigations in nuclear medicine departments have shown that the staff members are often not aware of the high risk of radiation exposure to the skin on the hands. This fact is mainly due to the beta radiation of the nuclides used for radiosynoviorthesis (RSO). Inappropriate or slack use of protective devices or bad practice may lead to high skin doses. In this chapter, basic radiation protection principles and methods are considered in order to reduce the occupational exposure, especially to beta radiation during RSO. Proper shielding of the active liquids and distance keeping are the most effective precautionary measures. Based on the physical and radiological characteristics of the RSO nuclides, which can cause high dose rates near vessels with radioactive solutions, the necessity of the use of appropriate shields for beta radiation and for the improvement of daily practice is demonstrated. Examples of well-proven appliances and tools are shown. Moreover, the challenges of skin dose monitoring with authorised partial-body dosimeters are discussed, and recommendations for the optimal wearing position of a ring dosimeter are given. In most cases, this is the first phalanx of the index finger of the nondominant hand with the detector-directed palmar. It is emphasised that, even in this optimal case, the real maximum skin dose is underestimated, on average by a factor of 6. Finally, the importance of accurate contamination monitoring as an essential radiation protection measure is emphasised.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- International Atomic Energy Agency
- Radiation Protection
- Optically Stimulate Luminescence
- Skin Dose
- Beta Radiation
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
Radiosynoviorthesis (RSO) requires the use of unsealed radioactive sources in the form of radionuclide solutions or colloidal suspensions.
The three common RSO nuclides, Yttrium-90, Erbium-169 and Rhenium-186 emit beta (β−) particles. Y-90 and Er-169 are pure beta emitters, whereas Re-186 also produces gamma radiation in 12 % of the decays. Relevant physical and radiological parameters of these nuclides are listed in Table 8.1. For comparison, the data of the most frequently used nuclides for diagnostics, Tc-99 m, are also given.
Obviously, as can be derived from the last three columns of the table, the dose rate factors (dose rate per unit of activity) and, thus, the hazard of skin exposure of staff members are much higher for beta particles than for gammas and also depends strongly on the maximum beta energy.
In situations of low radiation protection standards, the medical staff may receive high exposures (mainly to the skin on their hands) that might exceed the annual skin dose limit of 500 mSv [2]. Therefore, appropriate safety standards have to be strictly complied with.
2 General Radiation Protection Principles
Radiation protection is based on three rationales: justification, limitation and optimisation. These principles are defined and elucidated in numerous international recommendations (e.g. IAEA 1996 [3]) and national regulations. Particularly, the International Commission on Radiological Protection (ICRP) has addressed the nuclear medical community with several publications focusing on radiation protection of staff and patients in general and nuclear medicine [4–8]. In addition, the International Atomic Energy Agency (IAEA) has issued some comprehensive publications on this topic [9–11]. In the European Union, the basic safety standards for protection against the dangers arising from exposure to ionising radiation were implemented in the Council Directive 2013/59/Euratom (2013) [12].
2.1 Justification
A general definition of the justification principle is given in the European basic safety standards: “Medical exposure shall show a sufficient net benefit, weighing the total potential diagnostic or therapeutic benefits it produces, including the direct benefits to health of an individual and the benefits to society, against the individual detriment that the exposure might cause, taking into account the efficacy, benefits and risks of available alternative techniques having the same objective but involving no or less exposure to ionising radiation” [12]. In the EANM procedure guidelines for radiosynovectomy (2003) [13] and in Mödder (1995) [14], general justification criteria for RSO are given.
In the context of this article, the justification, i.e. the individual medical indication for a radionuclide therapy, is taken for granted and shall not be discussed here; however, it is a further precondition also for the justification of the occupational exposure of medical staff.
2.2 Limitation
The ICRP has defined dose limits for workers, which have been implemented in most countries [15].
The limit on the effective dose for occupational exposure shall be 20 mSv in any single year. However, in special circumstances or for certain exposure situations specified in national legislation, a higher effective dose of up to 50 mSv may be authorised by the competent authority in a single year, provided that the average annual dose over any five consecutive years – including the years for which the limit has been exceeded – does not exceed 20 mSv.
In most countries, the limit on the equivalent dose for the eye lens is still defined as 150 mSv in national legislation, but ICRP (2011) [16] and EURATOM (2013) [12] recommend 20 mSv in a single year or 100 mSv in any five consecutive years (subject to a maximum dose of 50 mSv in a single year).
In addition to the limits on effective dose, several limits on equivalent dose shall apply.
Especially in nuclear medicine, the limit on the equivalent skin dose (500 mSv per year) is of specific concern. In this case, the dose shall be averaged over an area of 1 cm2, regardless of the area exposed. For keeping the limit, the area considered is that where the highest dose is suggested.
For pregnant and breastfeeding workers, the equivalent dose to the unborn child shall be as low as reasonably achievable and unlikely to exceed 1 mSv during at least the remainder of the pregnancy after pregnancy has been notified to the employer. These members of staff shall not do work which involves a significant risk of intake of radionuclides or bodily contamination.
For apprentices aged between 16 and 18 years and for students aged between 16 and 18 years who, in the course of their studies, have to work with radiation sources, the limit on their effective dose shall be 6 mSv in a year. The equivalent dose limit for the eye lens shall be 15 mSv and for the skin, for extremities, 150 mSv in a year, respectively.
For emergency situations, the occupational exposure limit shall be set, in general, below an effective dose of 100 mSv. In exceptional situations, in order to save lives, prevent severe radiation-induced health effects or prevent the development of catastrophic conditions, a reference level for the effective dose from external radiation of emergency workers may be set above 100 mSv but no higher than 500 mSv. Before they start working, the workers must be informed clearly and comprehensively about the associated health risks and the available protection measures. They undertake these actions voluntarily.
2.3 Optimisation
To make sure that a worker does not receive or exceed the dose limits, all procedures that may cause exposures of staff members have to be optimised regarding radiation protection. The most common rule of optimisation in radiation protection is the “ALARA principle”. The acronym refers to the principle of keeping radiation doses “as low as reasonably achievable”. In this context, economic aspects, i.e. the costs of protection measures, should be taken into account.
3 Radiation Protection Measures
3.1 Shielding
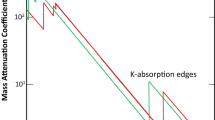
Shielding is a very effective protection measure, and it should be a matter of course that appropriate shielding for vials and syringes are used in everyday nuclear medicine and radiopharmacy operations. Materials with high density, i.e. with high atomic numbers Z, such as tungsten or lead are most suitable for the protection against gamma radiation. Generally, these shields are also appropriate for mixed beta/gamma emitters, for example, Re-186. However, its larger weight makes handling difficult. Therefore, shields from low-Z materials, e.g. transparent plastic such as acrylic glass or polycarbonate, are preferred for radionuclides that emit high-energy betas, such as Y-90 and Re-186. Besides, the use of low-Z shields minimises secondary bremsstrahlung. Though, it should be mentioned that the contribution of bremsstrahlung to the (total) exposure is often overestimated, and top priority is given to the efficient shielding of the betas. Monte Carlo simulations showed that Y-90 is shielded more effectively by 5 mm tungsten than by 10 mm acrylic glass because of the additional absorption of the bremsstrahlung [17]. This, however, is only important when high activities must be shielded and is not relevant for RSO.
The shielding thickness required depends on nuclide type and the activity. Moreover, a syringe shield should have a manageable size and weight. Beta particles are completely absorbed if the thickness of the shielding material exceeds the maximum particle range (see Table 8.1). For Y-90 (E β,max = 2.3 MeV), the nuclide with the highest beta energy used in nuclear medicine, the range in plastic is about 9 mm. Therefore, shields that are designed for Y-90 are also appropriate for Re-186 (E β,max = 1.08 MeV), which has a maximum range of 3.4 mm. Handling of Er-169 does not require vial or syringe shields. Their low-energy beta particles (E β,max = 0.35 MeV) have a short range (plastic: 0.8 mm, glass: 0.5 mm), and they are not able to penetrate the walls of common syringes or vials. The dose rate is additionally decreased due to the self-shielding within the radionuclide solution. Further attenuation of the exposure is provided by protective gloves.
There are several types of shields for vials, syringes and containers available that are used for therapeutic radiopharmaceuticals. Most of them are also appropriate for beta emitters and should also be employed for RSO procedures. Figure 8.1 shows a typical syringe shield designed especially for the 1 ml syringes common in RSO.
However, the use of suitable shielding does not guarantee tolerable radiation exposures. Even when applying a syringe shield, there is still an unshielded area with high dose rates at its base. In particular, during the injection of the nuclides into the joints, the needle has to be placed carefully in the joint. Usually, the needle hub is fixed with two fingers during the injection for some seconds. This common practice, during which the almost unshielded finger tips are in close contact with the Y-90 activity, may cause very high local skin exposures within a short period of time. To avoid this, a special protective ring has been developed. It provides both shielding and distance to the needle. This Macrolonring™ (Fig. 8.2) is available in sterile packages. It fits to Braun-type needles only and must be put over the needle before performing the puncture. The ring should also be used to reduce skin exposure during the preparation of active syringes (Fig. 8.3).
Of course, shields often hamper handling, especially when injecting the radiopharmaceutical into the joint. However, it is wrong to believe that shielding might as well be ignored if only you work faster. An acrylic shielding reduces the dose rate by one or two orders of magnitude. In contrast, it is impossible to increase your working speed by such a factor.
The whole body and eye exposure of staff during preparation can be reduced significantly when the withdrawal of syringes is performed behind conventional bench top shields such as lead walls, castles or lead glass windows. RSO staff can also protect themselves against beta radiation by means of special commercially available or “home-made” acrylic benchtop shields.
The syringes filled with radiopharmaceuticals should be stored and transported to the treatment room in an acrylic glass box (Fig. 8.4) or, alternatively, in a common glass tray with a lid.
Due to the fact that used and apparently empty needles, syringes, vials, etc. may contain considerable amounts of radionuclides, waste containers also have to be shielded adequately.
When manipulating nuclides that emit high-energy betas – such as Y-90 – exposure of the eye lens must also be taken into consideration.
3.2 Distance
Even experienced radiopharmaceutical or clinical staff often does not know that the high-energy betas from Y-90 have a maximum range of about 9 m in air. However, it should be well established that good enough, the dose rate decreases with the square of the distance to the source. Therefore, keeping the distance is the easiest and cheapest measure in terms of radiation protection, and all opportunities should be used to take advantage of the distance to radioactive substances. This is especially important in all situations where the processing of unshielded radiopharmaceuticals cannot be avoided. In such situations, the use of tools (such as clamps and pincers), which also diminish the risk of skin contamination, is strongly recommended. Figures 8.5 and 8.6 exemplify the use of such tools in RSO.
The principle to never make direct contact with unshielded vessels containing radionuclides with your fingers should be observed. This also holds true for any potentially contaminated vessels such as vials, syringes, tubes, etc. after discharging a radioactive liquid. The remaining activity within apparently empty vessels may be in the order of some 10 MBq, and careless direct contact to the skin may result in unnecessarily high exposures. Therefore, shielding and keeping your distance should also be considered when disposing of contaminated material and radioactive waste. Adequate waste management and disposal are a special task that cannot be discussed here in detail. IAEA (2006) [10], for example, gives additional advice.
Admittedly, there is a high degree of dexterity necessary in order to inject a solution into a joint using forceps, instead of gripping the needle with a hand. Moreover, the risk for injection outside of the joint increases. This practice requires special training. Alternatively, the above-mentioned Macrolonring™ should be used (Fig. 8.2).
Moreover, when manipulating beta-emitting nuclides with high-energy, e.g. Y-90, exposure of the eye lens must also be taken into consideration, especially against the background of the recent ICRP (2011) [16] recommendation to reduce the annual dose limit to the eye lens from 150 to 20 mSv. The use of shielding and increasing the distance also improve the protection of the eye lens. For answering the question of whether wearing protective glasses in the field of RSO is necessary, studies are still in progress.
4 Monitoring
4.1 Personal Dosimetry
Nuclear medicine staff must be routinely monitored for occupational radiation exposure, both to their whole body and parts of their bodies, if 3/10 of the dose limits might be exceeded, e.g. 150 mSv for the skin dose. Commonly, a personal dosimeter for monitoring the effective dose is worn on the chest, usually with film, thermoluminescence (TLD) or optically stimulated luminescence (OSL) dosimeters. It is also recommended to wear an additional extremity dosimeter for monitoring the skin dose to the hands for the majority of radiation workers in nuclear medicine, including radiopharmacy staff. Mostly TLD ring dosimeters are worn on the fingers for this purpose. Usually, these dosimeters are designed to measure photon radiation, e.g. in interventional radiology. In nuclear medicine, the more suitable solution is to wear ring dosimeters designed for mixed beta and photon fields. These dosimeters consist of a special TLD with a thin cover. Figure 8.7 shows three different types of these well-established dosimeters.
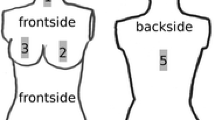
Even if appropriate individual dosimeters are available and actually worn by the exposed staff, monitoring does not necessarily provide results suitable to prove that the skin dose limit is observed. There is another essential issue to be considered: when handling radiopharmaceuticals in medical practices, staff in particular is exposed to rather non-uniform radiation fields. It is advisable to measure the skin dose at the part of the body which presumably receives the highest exposure.
The problem of valid skin dose monitoring was subject of the European research project ORAMED (“optimisation of radiation protection for medical staff”) [17]. Measurements of individual doses and their distribution across the hands of staff were performed in nuclear medicine diagnostics and therapy. This extensive study confirmed earlier results from RSO [2] as well as from other fields of nuclear medicine [18]: the thumb or index finger tips on the nondominant hand most frequently receives the highest dose [19].
Since the fingertip is not suited to wear a ring dosimeter, it should be worn preferably on the index finger base (first phalanx) of the nondominant hand, with the detector turned to the palmar direction [20]. The dosimeters should not be worn on the ring finger of the dominant hand, as it is common.
However, even if the routine ring dosimeter is attached to the base of the nondominant hand’s index finger, the maximum skin dose is underestimated by a factor of about 6 on average. This factor increases considerably when wearing the dosimeter, e.g. on the ring finger or on the wrong hand. The deviation between the dosimeter reading and the maximum dose also increases when the radiation field is more inhomogeneous, e.g. due to insufficient protection measures, such as working without shields. Routine skin dose monitoring often results in severe underestimation of actual skin exposure and, consequently, in a belittlement of the hazard. Therefore, more effort has to be put into improving radiation protection measures.
4.2 Contamination Monitoring
Since RSO requires the handling of unsealed liquid radionuclides, there is an increased risk of skin contamination and incorporation. It goes without saying that eating, drinking and smoking are prohibited in controlled areas.
Nitrile or vinyl instead of latex gloves should be worn to avoid hand contamination, since some radioactive solutions may easily penetrate latex. Before leaving the controlled area, hands have to be routinely checked for contamination with an appropriate contamination monitor that should be in stand-by mode in any nuclear medical facility. The responsible staff members must be trained both in performing measurements of contamination measurements and in decontamination measures.
More detailed instructions related to radiation protection in radionuclide therapy are given in IAEA (2006) [10]. Advice that is particularly useful for several radionuclides is also available on a number of websites, among them the American Health Physics Society’s (HPS) [21] homepage.
References
Delacroix D, Guerre JP, Leblanc P, et al. Radionuclide and radiation protection data handbook 2002. Radiat Prot Dosim. 2002;98:1.
Barth I, Mielcarek J. Occupational exposure during radiosynoviorthesis. In: Proceedings of the 6th European ALARA Network Workshop “Occupational Exposure Optimisation in the Medical Field and Radiopharmaceutical Industry.” Madrid, 23–25 Oct 2002. p. 43–6, ISBN 84-7834-437-3.
IAEA. International basis safety standards for protection against ionizing radiation and for the safety of radioactive sources, IAEA Safety Series, vol. 115. Vienna: International Atomic Energy Agency; 1996. PO Box 100, A-1400.
ICRP. Radiological protection and safety in medicine. International Commission on Radiological Protection, Publication 73, Ann. ICRP vol 26(2). Oxford: Elsevier; 1996.
ICRP. International Commission on Radiological Protection radiation dose to patients from radiopharmaceuticals, Publication 80, Ann. ICRP vol 28(3). Oxford: Elsevier; 1998.
ICRP. International Commission on Radiological Protection pregnancy and medical radiation, Publication 84, Ann. ICRP vol 30(1). Oxford: Elsevier; 2000.
ICRP. International Commission on Radiological Protection release of patients after therapy with unsealed radionuclides, Publication 94, Ann. ICRP vol 34(2). Oxford: Elsevier; 2004.
ICRP. International Commission on Radiological Protection, the 2007 recommendations of the International commission on radiological protection, ICRP Publication 103, Ann. ICRP 37(2–4). Oxford: Elsevier; 2007.
IAEA. International Atomic Energy Agency, applying radiation safety standards in nuclear medicine. IAEA Safety Report Series No. 40, Vienna. 2005.
IAEA. International Atomic Energy Agency, nuclear medicine resources manual. Vienna: International Atomic Energy Agency; 2006. ISBN 92-0-107504-9.
IAEA. International Atomic Energy Agency, release of patients after radionuclide therapy. Safety Report Series No. 63, Vienna. 2009.
EURATOM. 2013. COUNCIL DIRECTIVE 2013/59/EURATOM of 5 Dec 2013 laying down basic safety standards for protection against the dangers arising from exposure to ionising radiation, and repealing Directives 89/618/Euratom, 90/641/Euratom, 96/29/Euratom, 97/43/Euratom and 2003/122/Euratom, EN Off J Eur Union 14.01.2013, L13/1ff.
EANM Procedure Guidelines for Radiosynovectomy. EANM procedure guidelines for radiosynovectomy. Eur J Nucl Med. 2003;30(3):BP16. March 2003 – EANM 2003.
Mödder G. Radiosynoviorthesis: involvement of nuclear medicine in rheumatology and orthopaedics. Mecckenheim: Warlich; 1995.
ICRP. International Commission on Radiological Protection general principles for the radiation protection of workers, Publication 75, Ann. ICRP vol 27(1). Oxford: Elsevier; 1997.
ICRP. International Commission on Radiological Protection, statement on tissue reactions. 21 Apr 2011.
ORAMED. 2011. http://www.oramed-fp7.eu/.
Whitby M, Martin CJ. A multi-centre study of dispensing methods and hand doses in UK hospital radiopharmacies. Nucl Med Commun. 2005;26:49–60.
Rimpler A, Barth I, Ferrari P, et al. Extremity exposure in nuclear medicine therapy with 90Y-labelled substances – Results of the ORAMED project. to be published in Rad Meas. (2011). http://dx.doi.org/10.1016/j.radmeas.2011.05.068.
Sans Merce M, Ruiz N, Barth I, et al. Recommendations to reduce hand exposure for standard nuclear medicine procedures. Radiat Meas. 2011;46:1330–3.
HPS http://hpschapters.org/northcarolina/nuclide_information_library.php3.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Barth, I., Rimpler, A. (2015). Radiation Exposure of Medical Staff and Radiation Protection Measures. In: Kampen, W., Fischer, M. (eds) Local Treatment of Inflammatory Joint Diseases. Springer, Cham. https://doi.org/10.1007/978-3-319-16949-1_8
Download citation
DOI: https://doi.org/10.1007/978-3-319-16949-1_8
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-16948-4
Online ISBN: 978-3-319-16949-1
eBook Packages: MedicineMedicine (R0)