Abstract
The normal course of adolescence presents many developmental challenges at the biological, psychological, and interpersonal level (Steinberg 2004; Levpuscek 2006). The onset of puberty, increasing complexity of peer relationships and increased expectations at home, school, and often work, can make successful transition through adolescence complex even for the most well-adjusted teen. Social anxiety disorder (SAD) in adolescence exacerbates these challenges exponentially. As such, study of SAD during this developmental stage is of particular importance, given that SAD frequently onsets during adolescence and disrupts functioning and quality of life throughout the life span (Brown et al. J Abnorm Psychol 110:49–58, 2001; Burstein et al. J Am Acad Child Adoles Psychiatry 50:870–880, 2011; Rosellini et al. J Psychopathol Behav Assess 35:356–365, 2013). This chapter provides an overview of the ways in which adolescence provides fertile ground for the development and exacerbation of SAD, focusing on the particular challenges unique to this developmental stage at the biological, cognitive, behavioral, and interpersonal level. Next, we review the ways in which empirically supported treatments and interventions have been tailored to meet those challenges in this age group. The chapter also addresses how recent sociocultural changes and contemporary research have increased awareness of how these challenges can extend and develop during emerging adulthood. Finally, we discuss new frontiers in empirically supported treatments to engage the challenges accompanying this newly recognized developmental stage transition.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Social anxiety disorder
- Social anxiety
- Adolescence
- Emerging adulthood
- Young adults
- Empirically supported treatment
- Cognitive behavioral therapy
- Group therapy
- Development
- Launching emerging adults program
Introduction
Whether a child presenting for treatment for the first time, or an adult recalling when they first began to struggle with excessive fear in social performance situations, the teenage years have been identified repeatedly as a key time for social anxiety disorder (SAD) to take root and flourish in ways that can be determinant for the entire course of the person’s life. For this reason, study of SAD during the adolescent years provides both fruitful insight into the origins and course of the disorder and may also offer a crucial context for intervention.
Among anxiety disorders, SAD has one of the earliest onset and, without intervention, tends to follow a chronic course (Brown et al. 2001; Burstein et al. 2011; Juster and Heimberg 1995; Reich et al. 1994; Rosellini et al. 2013; Stein and Stein 2008). In fact, the median age of onset of SAD appears to be more accurately described as bimodal; in one large sample of individuals presenting for treatment, 21 % reported an age of onset before the age of 10, and 47.6 % reported an age of onset during adolescence/early adulthood (14–22) (Rosellini et al. 2013). Age of onset in the middle childhood years (10–14) or adult years (over 23)Footnote 1 is relatively rare (Rosellini et al. 2013; Wittchen and Fehm 2003 Footnote 2). For more details, please see Chap. 3. A 3-year longitudinal study found that whereas depression typically followed an episodic course, anxiety and symptoms of social anxiety, in particular, tended to operate with trait stability akin to personality attributes (Prenoveau et al. 2011). The early developmental stages of psychopathology (EDSP) study, a prospective, longitudinal study of 3,021 community participants reported that generally by the age of 19, the individual’s SAD stabilized or began a progressive worsening that persisted into adulthood (Wittchen and Fehm 2003).
When one looks at the particular challenges of the developmental stage, it is perhaps no surprise that adolescence is such a fertile ground in which SAD can take root. Traditionally, the period between 13 and 18 years old is viewed as one of tumultuous change. Almost immediately after adolescence emerged as a distinct developmental phase, it was famously characterized as a period of “storm and stress” (Hall 1904), during which questions of identity become paramount (Erikson 1959). Of course, the major change that comes to mind for many is the development of sexual maturity through puberty; however, of late the organizational changes within the brain are now thought to be equally epochal. Through the process of synaptic pruning, massive numbers of neuronal connections die off as the brain shifts from a sponge seeking maximal input to a powerfully efficient processing machine (Compas 2004). Adolescents’ abilities to represent information symbolically and to reason abstractly significantly mature. Of course, this ultimately positive reorganization has a few short-term costs; the attrition of neuronal connections between the frontal lobes and limbic structures has been implicated in the higher propensity to risky behavior often observed in teens (Steinberg 2004).
In tandem with these improvements in functioning, everyday tasks of living become more difficult during adolescence. Expectations at school and home tend to increase dramatically, as adolescents are expected to function more independently (although often without commensurate increases in freedom). Adolescents at school take on not just more work, but more complicated and academically challenging work. “Multitasking” is expected with greater frequency and flawlessness. Expectations at home can shift to include more responsibility (e.g., more chores or more work) and increased self-direction (e.g., waking oneself up, initiating homework with less monitoring).
Relationships with parents can become more complicated as well, although not necessarily in the expected way. Relationship patterns change dramatically within the stage of adolescence. For example, in a sample of 495 Slovenian teens between the ages of 13 and 19, Puklek Levpušček (2006) reported that support seeking from and idealization of parents decreased significantly during early and late adolescence; mid-adolescence (during eighth grade) appeared to be a particularly critical point, during which children were most likely to report high self-sufficiency and defensiveness around need for parental support, before developing a more balanced view of self in relation to family during late adolescence. Parents often view their relationships with teens as suddenly more fraught and difficult, as they find their child questioning their authority and values more and more frequently. Infuriatingly, they see their teens walk away from pitched battles over house standards and rules relatively unscathed, viewing the conflict less as a death match over the future and more as an exchange of opinion (Smetana 1997; Steinberg 2001).
Peer relationships become substantially more salient and charged. With the rise of the “invisible audience” and increasing questions about identity and one’s future (presumably offshoots of the improved ability to reason symbolically), adolescents become more aware that their own views of self may differ substantially from their peers’ opinions, and even the uncertainty over what others’ opinions might be can be threatening and worrisome (Elkind 1967). At the same time, the importance of peers becomes paramount as adolescents step into taking charge of their friendships, and the first tentative first steps toward establishing their sexual identity (Buote et al. 2007; LaGreca and Prinstein 1999), just at a moment where their brains and bodies may be least equipped to manage all the input. For more details, please see Chap. 3, 5 and 8.
All this change and much more happen just in the course of normal development. Successful transition through adolescence depends on meeting these new challenges with a strong foundation of early experience. Compounding their significance, the manner and degree to which adolescents are able to meet these challenges may variably confer risk and resilience as they navigate through subsequent developmental transitions during later adulthood. The ways in which SAD further complicates these developmental transitions are myriad and pervasive. For example, symptoms of social anxiety can interfere with the process of differentiating from parents and adopting a more independent role, contribute to avoidance of peers at exactly the moment when peers are meant to become major influences in the development of one’s proto-adult identity, and as a result often inhibit or even bring the transition into adulthood to an effective halt. In addressing SAD clinically, therefore, clinicians must take into account all of the vulnerabilities and developmental challenges present in this period and respond in a comprehensive and inclusive way.
This recognition and the recognition that adolescents face specific challenges that are qualitatively distinct from other age groups led Albano and colleagues (1991) to develop cognitive-behavioral group treatment for adolescents (CBGT-A). CBGT-A, a developmental adaptation of Heimberg’s successful protocol for treating adults with SAD (Heimberg et al. 1985, 1990; Hope and Heimberg 1993), is designed to be delivered by co-therapists for groups of adolescents between the ages of 13 and 17 years. CBGT-A consists of 16 to 20 90-min group therapy sessions with adolescents scheduled over a 3- to 4-month time period and adds meetings with parents at four strategically placed sessions during the program. The multicomponent protocol is divided into two phases, with the first phase of treatment (i.e., sessions 1 through 8) focusing on psychoeducation and skill building in such areas as social problem-solving, assertiveness, and cognitive restructuring; and the second phase (i.e., sessions 9 through 14) emphasizing within-session behavioral exposure and homework exposure assignments. Session 15 involves exposure tasks performed in front of an audience of parents, and session 16 focuses on final exposures and termination (Albano and Barlow 1996). Empirical research, though limited somewhat in scope, has supported the efficacy of this approach (Albano et al. 1995; Garcia-Lopez et al. 2002, 2006; Hayward et al 2000; Olivares et al. 2002).
This multifaceted approach was an early recognition of the fact that adapting group (or, for that matter, individual) treatment for adolescents requires careful attention not just to the course and challenges in normal development, but also to the early risk factors that render the child vulnerable to anxiety and the conditioning factors and challenges that occur during adolescence which exploit this vulnerability. We will now consider the specific developmental challenges that predict SAD and the types of interventions that can target those challenges. As we will see, effective evidence-based interventions for SAD in adolescents have consistently emphasized a multifaceted approach, consistent with the complex interplay of factors that leads to the onset of SAD.
Anxiety disorders do not typically appear sui generis; they are frequently the product of distal developmental influences, so that an anxiety problem that arises at 14 or 23 can still be influenced by factors that were present at (or even before) birth. Developmental psychologists (and increasingly clinical psychologists) place a premium on developmental pathways, highlighting the various vulnerabilities, conditioning events, and maintaining factors underlying a disorder (Higa-McMillan and Ebesutani 2011; Vasey and Dadds 2001). Although age of onset during adolescence appears to be more strongly related to the presence of some acute stressor or stressors around the time the SAD developed, most researchers believe the individual’s response to these stressors is strongly influenced by a variety of vulnerabilities produced by exposure to any number of risk factors (Rosellini et al. 2013). It is also worth considering early factors in the onset of SAD because earlier age of onset predicts increases in symptom severity, autonomic arousal, depression, higher levels of neurotic temperament, and functional impairment (Rosellini et al. 2013: see Knappe et al. Chap. 3, this volume). Failing to consider the early factors that predict SAD in adolescence would therefore mean that not only would we miss the key predictors of why SAD develops in adolescence, but that we would also neglect the most severely afflicted, those who may experience exponentially exacerbated difficulties during their teenage years.
Biological Risk Factors
As with so many mental and emotional disorders, the road toward adolescent SAD can begin before the child is even born. A broad scientific consensus has gathered in support of the heritability of SAD (e.g., Fyer et al. 1993, 1995; Hughes et al. 2009; Kendler et al. 1992; Mannuzza et al. 1995; Reich and Yates 1988). First-degree relatives of adults with SAD are three times more likely to be afflicted with SAD (compared with first-degree relatives of control participants) (Fyer et al. 1993, 1995; Mannuzza et al. 1995; Reich and Yates 1988). Twin studies have yielded heritability estimates of 30–65 % (Kendler et al. 1992; Beatty et al. 2002). These estimates are more pronounced as a function of subtype of SAD. For example, Stein and colleagues (1998) found that first-degree relatives of adults with generalized SAD were ten times more at risk for generalized SAD; no enhanced risk was found for the nongeneralized subtype.
It should be noted that the heritability estimates reported here are not necessarily specific risk for SAD. Whereas both of the Fyer et al. (1993, 1995) and the Reich and Yates (1988) studies found evidence for specific risk, other studies have found more complicated pathways, finding evidence that a variety of parental mental illnesses, including panic disorder and especially major depression, can predict SAD in offspring (Horwath and Weissman 1995; Biederman et al. 2001; Lieb et al. 2000). Inheritance of SAD demonstrates concordance or nonsignificant differences in heritability between monozygotic and dizygotic twins (Kendler et al. 1992; Skre et al. 1993). Stein and Stein 2008 has suggested that genetic inheritance of internalizing disorders may be best characterized as the passing on of broad, nonspecific traits that are predictive of anxiety disorders in general rather than of SAD in particular.
A key inherited nonspecific set of traits appears to be behavioral inhibition to the familiar (BI), first identified by Kagan and colleagues (1988; Kagan 1989). BI was used to describe observation of generalized emotional and behavioral tendencies among 10–15 % of Caucasian infants to withdraw or become upset when presented with new or otherwise unfamiliar stimuli. In the youngest children, BI might look like withdrawal, looking to parents or becoming upset when presented with a new toy. In preschool-aged and elementary school-aged children, this temperamental tendency might manifest as constricted emotional expression, hesitancy when speaking or approaching a new situation, and/or reluctance to engage in conversation with peers or adults. In a meta-analytic review of the link between BI and SAD, researchers indicated that BI predicted a three- to sevenfold increase in risk, translating to 40 % of children with BI developing SAD (Clauss and Blackford 2012). However, it is worth noting that the same study concluded that BI was best construed as a generalized risk factor for SAD, not an early precursor; in support of this contention, Clauss and Blackford (2012) cite that the majority of children with BI do not develop SAD, and children with BI do not automatically suffer from the same deficits in emotional regulation and pervasive fear of negative evaluation seen in children with SAD. On the other hand, as noted by Perez-Edgar and Guyer (2014), the precise relationship between BI and SAD has not been definitively established by any direct research.
Multiple studies have supported the stability of BI from infancy through toddlerhood and into middle and late childhood (Caspi and Silva 1995; Asendorph 1994; Fordham and Stevenson‐Hinde 1999; Goldsmith and Lemery 2000). Kagan and colleagues (1988) posited that the observed emotional and behavioral correlates of BI were a function of a lower response threshold of the basolateral and central nuclei of the amygdala and projections to the striatum, hypothalamus, and the sympathetic chain and cardiovascular system. This hypothesis has been supported in some studies, although not consistently (Hirshfeld et al. 1992; also, for a review, see Ollendick and Hirshfeld-Becker 2002). Similarly, BI and SAD have been frequently linked in the literature. Among the children from the original Kagan et al. studies, the rates of generalized SAD were found to be substantially higher among those who demonstrated highest BI as toddlers, as compared with the adolescents who were most extroverted as toddlers (34 % vs. 9 %, respectively) (Schwartz et al. 1999). The differences were even starker among girls (44 % vs. 6 %). A separate study found that adolescents with childhood BI were four to five times more likely to develop social anxiety disorder than adolescents without childhood BI (Biederman et al. 2001). At least one study suggested that BI was uniquely predictive of lifetime SAD (as opposed to being more generally predictive of the presence of any anxiety disorder) (Chronis-Tuscano et al. 2009).
Consistent with the BI hypothesis, researchers have also noted significant links between hyperreactivity of the amygdala in response to emotional expression in others and SAD (Battaglia et al. 2012; Blair et al. 2011; Guyer et al. 2008). The first critical fMRI study of adolescents found evidence for significantly higher amygdala and fusiform gyrus activation in response to fearful faces; in addition to the amygdala’s role coordinating fear activities, the fusiform gyrus is implicated in facial recognition (Guyer et al 2008). Battaglia and colleagues (2012) were able to successfully predict onset of SAD in a group of 14- to 15-year-olds by measuring brain reactivity (particularly in the amygdala) to angry and fearful faces at the age of 8–9 years old. Blair and colleagues (2011) reported significantly increased reactivity in the amygdala and rostral anterior cingulate cortex in both adolescents and adults with SAD in response to others’ emotional expression. The authors went on to note that the failure to find any significant interactions except in the context of SAD and reactivity to target emotion suggested a developmentally stable disruption (as opposed to a developmental deterioration) (Blair et al. 2011). That is, the disruption associated with SAD appears to be an independent interference on the normal development of facial recognition and recognition of emotion in others’ faces. Although these studies offer important support for long-held conventional wisdom around the role of the amygdala in anxiety disorders, it is worth noting that each of these studies suffers from relatively small samples and accompanying power difficulties.
Addressing Biological Risk Factors in Clinical Treatment
In effective evidence-based treatment, consideration of biological vulnerabilities can influence both assessment and psychoeducation about the nature of the disorder. Clinicians may want to attend in particular to adolescents endorsing early onset of SAD or families endorsing high prevalence of anxiety among first-degree relatives. These adolescents may be at particularly high risk for high levels of social anxiety and avoidance, and referral for psychiatric consultation or more intensive treatment options may be appropriate to consider at an earlier point in treatment. In our clinic, for example, adolescents with earlier onset and higher family loading for anxiety and youth with greater functional impairment may be offered individual and group therapy to occur concurrently as a means of giving a higher “dose” of intervention.
Of equal, or perhaps even more importance, appropriately educating families about genetic and temperamental risk for anxiety disorders is crucial. As noted previously, SAD can manifest as more of a trait personality factor rather than an illness with a more chronic or intermittent course (Wittchen and Fehm 2003). Accordingly, many individuals can interpret the notion that SAD is partially heritable as more or less a “life sentence” or that their symptoms are not amenable to psychosocial change. Given the importance placed on developing a strong sense of identity during this stage, defining oneself as an “anxious person,” as our patients all too frequently do, can be an especially sticky and pernicious form of self-fulfilling prophecy. It can be important to engage and challenge these ideas. It can be worth noting that it was only among the extreme 10–15 % of individuals with BI that Kagan and his team saw stability of symptoms into adulthood, and even among that 10–15 %, quite a few demonstrated apparently spontaneous shifts toward increased comfort with the unfamiliar or even extroversion. As noted above, even the largest estimate of individuals identified with BI who later develop SAD peaks at 48 % (Clauss and Blackford 2012). During the psychoeducation process, therefore, it is crucial for clinicians to discuss the overall plasticity of the brain, especially in these early years, and that early trends toward distress and dysfunction are amenable to amelioration or even radical change. It is also crucial to help those adolescents who have a nascent, or even well-developed notion of themselves as “anxious people” to use cognitive restructuring to challenge this inaccurate (and often self-fulfilling) label and help them become more aware of other constructive aspects of identity.
There is a diametric peril for the psychoeducating clinician, of course. While communicating optimism or the potential for change, the clinician should be careful not to share an overly rosy perspective; increasing numbers of clinicians are considering the possibility that while anxiety can be regulated effectively, it may also require a lifelong commitment to challenging one’s anxiety and using skills gained in treatment to sustain gains from therapy.
SAD and Family Organization
In early childhood, parents assume a crucial role, from facilitating to disrupting the arc of development. For example, parents can influence positive growth during early life by directly and indirectly promoting social skills, encouraging peer interactions through supervision and direct facilitation (such as scheduling play dates), and offering feedback on appropriate and inappropriate types of play (Masia and Morris 1998). In contrast to nonaffected individuals, adults and teens with social anxiety disorder are more likely to report memoires of less affectionate parents who were more socially isolated and hyperconcerned about the opinions of others, who behaved in both overprotective and in rejecting or neglectful ways, who were ashamed of their own shyness and poor social performance, who tended to discipline by shaming, and who tended to isolate their children as well (Arrindell et al. 1989; Bogels et al. 2001; Bruch and Heimberg 1994; Burgess et al. 2001; Caster et al. 1999; Lieb et al. 2000; Parker 1979). In complement to these retrospective reports, other studies have found that parents of anxious children have demonstrated both impaired ability to help their children engage with peers and are more likely to encourage avoidance of potentially threatening situations (Barrett et al. 1996b; Finnie and Russell 1988). Notably, these problematic parental behaviors appear to be uniquely predictive of difficulties in their offspring. One study found that while parental lack of emotional warmth and family dysfunction were both uniquely predictive of adolescent SAD, parental psychopathology only predicted SAD in the context of other vulnerability factors (although the authors added that psychopathology may be crucial to disorder onset, they qualified that this variable likely plays a more secondary role in contributing to the maintenance of symptoms over time) (Knappe et al. 2009).
Given that so many of these studies have a limited frame of reference or rely on self-report or memories of past interactions, the possibility cannot be ruled out that the nascent vulnerability to anxiety may have influenced (or even coerced) parental responses. Still, these conclusions are bolstered by the results of some work focusing on parental and sibling impressions of their own behaviors and observational studies, which find that parents of anxious youth also view themselves as overprotective and relatively more rejecting than the average parent (Garcia-Lopez et al. 2009, 2014; Gulley et al. 2014; Hudson and Rapee 2001, 2005; Lieb et al. 2000; Rubin and Mills 1990; Siqueland et al. 1996; also, see Wong and Rapee, Chap. 2; Knappe et al., Chap. 4, this volume, for a comprehensive review). It is also worth noting that in this literature, “parenting” is often code for the relationship with the mother; fathers remain underrepresented in these research studies. Among the few studies that have focused in particular on father nurturing behaviors, there is little consistency. One study supported a connection between overcontrolling parenting behaviors and social anxiety (Greco and Morris 2002), while another study failed to find any clear link between a father’s parenting style and social anxiety (Hudson and Rapee 2002).
More recently, researchers have begun to address this deficit—Bogels and colleagues (2011) suggested that the behavior of fathers might be more impactful on the anxiety of their children than maternal behaviors. In contrast, Knappe et al. (2012) reported distinct and contrasting patterns of parental dysfunction, such that maternal overprotection and paternal rejection and lower emotional warmth predicted SAD in their children. Interestingly, the crossover relationships were not found to be true—paternal overprotection and maternal rejection or lack of warmth failed to significantly predict SAD in their children (Knappe et al. 2012).
Intervening at the Familial Level
Research indicates that the nature of parenting of children with SAD can be ambivalent and inconsistent, reflecting patterns of overprotectiveness, overcontrolling behaviors and neglect, and tendency to encourage avoidance or social isolation. Clinically, we often see other complicated parental emotions underlying these patterns. A representative sample can include emotions such as concern and anxiety over their child’s future; anger or upset around the teen’s failure to take responsibility or initiative; confusion over the “can’t vs. won’t” issue (i.e., whether their child is avoiding or truly incapable of engaging with a particular task or challenge), and therefore when to push and when to be understanding; and sadness in recognizing similar patterns or struggles from their own past or present lives. We have seen these emotional responses, and many others, in the course of treating adolescents (and, in turn, their parents) in our clinic.
These clinical observations have been borne out in research. Garcia-Lopez and colleagues (2009) reported that in a clinical sample of 16 adolescents with SAD, adolescents with parents who were high in parental overinvolvement, criticism, and hostility (a construct known as expressed emotion) failed to benefit from a school-based CBT intervention. Garcia-Lopez and colleagues (2009) also emphasized that this pattern differentiated socially anxious adolescents from their adult counterparts, for whom outside criticism was less of a variable.
These parental emotions can lead to a variety of other mutually detrimental patterns. Frequently, parents can become overly intrusive, offering instrumental support or even solutions as opposed to encouraging independence or efficacy on the part of the child and offering support only when needed. All too often we have seen parents complete therapy and school homework assignments or otherwise advocate for their anxious adolescent because they were afraid to let the adolescent negotiate the situation on his or her own. Another common pattern is inconsistency in parenting behaviors, as parents often attempt to compensate for their ambivalence and confusion by vacillating between disciplinary and supportive approaches in unpredictable ways. The inconsistency can come at the between-parent level, where father and mother have different points of view and apply those perspectives simultaneously, resulting in confusion for the child and bringing the parents into conflict. Inconsistency can also come at the within-parent level, where a mother or father can apply supportive approaches until suddenly losing temper at the lack of progress, or meet the child’s avoidance with strong discipline only to immediately retreat into support or apologies. Parents frequently struggle with the paradox of knowing they need to encourage independence but being afraid to let the child struggle, and on occasion fail, or being unsure how to encourage or discipline because they cannot discern willful violations of expectations or rules from impairing symptoms of anxiety.
Given that, developmentally, the hope is that parents are becoming somewhat less involved during adolescence, bringing them into treatment can seem somewhat counterintuitive. The truth is, parents can still play crucial roles as allies; the important part is helping them to become more involved in constructive ways as a support system (as opposed to a strict authority) and help the entire family unite around a shared goal and purpose, with clearer understanding of the best skills to help the child move forward.
Albano and colleagues (1991) understood the importance of involving parents in CBGT-A in transitional sessions. By directly involving parents in treatment at key times, parents could get crucial instruction in the skills their children were using in order to help support their adolescent’s practice and use of those skills. Involving parents in goal setting helps them better direct their efforts. For example, as opposed to “shotgunning” feedback—that is, giving reactive and inconsistent feedback in a variety of areas, often in the form of criticism—feedback could be more focused around specific goal areas. In other words, feedback could be strategically directed at supporting improvement within two or three specific domains where the child could consistently challenge him or herself, and the parent could give both praise and constructive feedback in a consistent manner, building better reinforcement of gains. In concert, by observing exposures, parents could gain valuable insight into their child’s independent capabilities and challenges as well as see how facilitating exposure with effective application of cognitive restructuring and processing of the situation critically differs from simply compelling a child to engage in an anxiety-provoking situation. Each of these is a key technique to help parents become more constructively involved, while also allowing the teen significant independence and authority over their own treatment and life choices.
Other treatment models involve parents in different ways. In a small, randomized, controlled trial examining the efficacy of social skills training (SST; Spence 1995) in treating children and adolescents, a clinical sample of socially anxious children and adolescents (ages 7–14) were assigned either to SST plus parental involvement (PI; n = 17), SST with no parent involvement (NPI; n = 19) or a wait list control group (WLC; n = 14) (Spence et al. 2000). In the PI condition, parents viewed all child-focused SST sessions through a one-way mirror and simultaneously received 12 weekly group parent training sessions. Children and adolescents who received SST with either PI or NPI both improved compared to WLC. Although no significant differences were found in outcomes between PI or NPI SST groups at either posttreatment or 12-month follow-up time points, investigators noted a trend toward superior results when parents were involved in treatment.
A third use of parents can be simply involving them at the outset of treatment, during the orientation and psychoeducation phases. Beidel and colleagues employed such a model in their social effectiveness training for children (SET-C; Beidel et al. 1998). In this case, although the treatment was found to be effective overall in both immediate and long-term follow-ups, the contributions of the parental component were not directly assessed. This treatment also targeted children slightly before the teen years (age 8–12), further complicating the direct comparison with other models.
Another school-based intervention also incorporated targeting parents high in expressed emotion in the form of high overinvolvement, criticism, and hostility. This treatment program, called Intervencion en Familias & Adolescentes con Fobia Social (IFAFS; Garcia-Lopez et al. 2014), was an adaptation of a program targeting social anxiety in adolescents without directly targeting families. The original program consisted of 12 weekly group sessions of 90 min each and incorporated psychoeducation, social skills training, cognitive restructuring, and exposure through use of peer assistants and video feedback, all during school hours and with additional, optional individual sessions. IFAFS built on this previous clinical program by incorporating five additional 120-min group sessions specifically for parents, offering psychoeducation about social anxiety and expressed emotion, and giving parents feedback on communication skills and use of contingency management to help them better manage their child’s anxiety. In direct comparison of the derivative and parent component-enhanced IFAFS programs, adolescents in the IFAFS program reported somewhat higher diagnosis remission rates (although not statistically significant).
Still, one may reasonably conclude as a result of the research that parents play a crucial role in the development of SAD and may also be a crucial component of treatment. However, as we can see here, there are several models for how one might approach this issue (not to mention the numerous trials that fail to include parents at all), and more research is critical to determine whether one model offers greater benefits and change relative to the others.
Conditioning Events
During adolescence, the research focus has narrowed on the role of conditioning events, proximal events that lead directly to the manifestation of social anxiety, or cause a nascent vulnerability to flower (Higa-McMillan and Ebesutani 2011). Consistent with behavioral learning models of anxiety, anxiety arises in response to direct classical or operant conditioning (e.g., a child is ridiculed or bullied by peers, leading to social withdrawal or avoidance) or through modeling or observational learning (e.g., a child observes parental social withdrawal and apes that avoidance among peers). Previously unthreatening events, such as raising a hand in class, speaking to unfamiliar people, or talking to peers can become a fraught and complicated situation as the awareness of others increases in tandem with the ability to abstractly reason. Indeed, a single instance of physiological hyperarousal and real or perceived social humiliation can be enough to poison performance in a narrow or wide array of social performance situations (Higa-McMillan and Ebesutani 2011). Estimates of adults with social anxiety disorder who can recall their anxiety rising in response to a single social performance failure range between 23 and 58 %, although evidence is generally in favor of the majority of adults recalling a conditioning incident (Kendler et al. 2002; Öst and Hugdahl 1981; Öst 1985; Stemberger et al. 1995).
Active peer rejection appears to be a significant proximal risk factor or conditioning event for SAD (Inderbitzen et al. 1997; La Greca and Lopez 1998). Adolescents with social anxiety tend to have fewer close friends and often view the quality of the friendships they do have to be low (La Greca and Lopez 1998). Prospective studies have linked peer victimization to increasing rates of both the experience of social anxiety and the onset of SAD in adolescence (Siegel et al. 2009; Storch et al. 2005). Although peer victimization has been linked with onset of a number of disorders, including depression, its relationship with SAD appears to be unique and pernicious. Ranta and colleagues (2009) reported that adolescents meeting criteria for SAD were more likely to report past episodes of peer victimization than adolescents who did not have SAD; although higher levels of peer victimization were more prevalent among adolescents with both depression and SAD, peer victimization and depression were not directly related. Follow-up work in this area drew patterns in longitudinal development (Ranta et al. 2013). Direct peer victimization at the age of 15 predicted SAD in boys at the age of 17, and SAD also predicted later peer victimization. Ranta and colleagues (2013) proposed a reciprocal and mutually reinforcing relationship between these variables, such that social avoidance led to risk in victimization, which in turn predicted avoidance and again victimization. In girls, only relational victimization was predictive of SAD. Persistence of victimization was also reported to be four to five times more frequent in boys than it was in girls in the sample.
Addressing Conditioning Events in Treatment
Whereas learning theory predicts the development of a disorder, it can also play a crucial role in helping overcome those learning events through effective use of exposure. Given the key role of conditioning events in kindling SAD and social avoidance during adolescence, it is no surprise that every empirically effective treatment for SAD in adolescence employs some form of exposure (Albano et al 1995; Beidel et al. 2000; Gallagher et al. 2004; Garcia-Lopez 2000, 2007; Hayward et al. 2000; Spence et al. 2000).
Additionally, the focus on group treatments and social skill development reinforces the importance that treatment research has placed on engaging potential deficits in functioning and the need to overcome social neglect and improve overall social functioning. As previously mentioned, CBGT-A places social skill development as a core priority of treatment (Albano et al. 1991). Spence’s SST places even greater emphasis on social skills training through modeling, role-playing, prompts, and reinforcement, first taught didactically as “micro-skills” and later in the context of in-session practice. The 12-week program consists of weekly, hour-long group sessions followed by 30 min of social practice “games.” Beidel and colleagues’ (1998) SET-C goes even further still; during the 24 twice-weekly treatment sessions spanning 12 weeks, participants attend both a 60-min individual exposure session and a 60-min social skills training group. In addition, immediately following each social skills training group, children participate in a 90-min peer generalization session with a group of outgoing, unfamiliar peers. These sessions are designed to provide participants with opportunities to practice social skills with nonanxious peers through collaborative group activities (e.g., bowling, pizza parties, etc.).
Masia and colleagues (1999) developed Skills for Academic and Social Success (SASS) program, which was primarily derived from SET-C with adaptations for practical delivery in a high school environment (e.g., briefer sessions, incorporation of teachers) and developmental modifications for an adolescent population (e.g., age-appropriate social skills training, addition of training in “realistic thinking”). The SASS program consists of 14 group sessions: one session of psychoeducation and orientation, one session of instruction in realistic thinking, five sessions each of social skills training and exposure, and the remaining sessions focusing on relapse prevention and the opportunity to practice skills in the context of two unstructured social activities (e.g., pizza parties). Another unique aspect of the protocol pertains to direct involvement of teachers who were asked to conduct practice exposure exercises with group members (e.g., spontaneously calling them in class).
Although bullying and peer victimization have received significant study as their own phenomena, they have never been directly studied in the context of treatment for SAD. However, there is recent work by La Greca et al. (2014) on the development of the PEERS/UTalk program for the prevention of depression and SAD among adolescents with elevated social anxiety and depressive symptoms. This interpersonal treatment program also includes components that are aimed at enhancing adolescents’ strategies for dealing with interpersonal peer victimization (see Chap. 11). Even among the social skills groups mentioned here, it is unclear how much focus has been given to negotiating peer victimization. Again, we see that there is a sound empirical basis for attention to intervention in challenging the impact of conditioning events through the use of exposure, social skills training, and other forms of adaptive skills. What remains unclear are what components might be most vital or what approaches might be most effective in accomplishing this goal.
Future Directions: Developmental Functioning as a Target of Treatment Intervention
Although one can reasonably find evidence for a building consensus around the development, phenomenology, and effective treatment of SAD in adolescence, a close examination of these issues will reveal substantial issues. Definitions of basic constructs and populations of interest have shown considerable variability. SAD first appeared in the third edition of the Diagnostic and Statistical Manual for Mental Disorders (DSM; APA 1980). Since then, the diagnostic construct has undergone substantial revisions in every edition, and DSM-5 (APA 2013) is no exception. Children and adolescents did not receive diagnoses of social phobia (the former SAD) in DSM-III and DSM-III-R, instead receiving a diagnosis of avoidant disorder of childhood or adolescence. DSM-5 officially changed the name from social phobia to social anxiety disorder in an attempt to better communicate the scope and consequence of the disorder. The DSM-5 also expanded the definition of SAD to include fear of any form of negative evaluation (as opposed to fear of only humiliation or embarrassment), as well as the role of clinician judgment in evaluating how disproportionate the individual’s fears might be in sociocultural context (Heimberg et al. 2014). In a similar vein, definitions of periods of childhood and adolescence have also varied in research samples, contributing to complexity in making direct comparisons of results across research studies.
What this means is that the definitions of SAD and adolescence have been somewhat moving targets, and although many of these results have been presented here as equivalent, they can include somewhat different groups and fail to include others who perhaps had flawed understanding of their condition. For example, rather than the generalized/nongeneralized subtype frequently alluded to in this paper, DSM-5 has opted for a new specifier, “performance only,” emphasizing a narrower range of the condition in a subgroup of individuals. The implications of these definitions and redefinitions have unclear and understudied implications for the operationalization of SAD both in the past and in the future.
One may also note that despite DSM-III’s early suggestion that SAD in childhood might be somewhat different from adult SAD, most techniques represent downward extensions of adult models. Adult models have hypothesized that social anxiety is maintained through mental imagery or schema defining what is expected as a performance standard in a given social situation and then evaluating all the ways in which the mental image of self deviates from that ideal standard (Rapee and Heimberg 1997). What is less clear is how well these adult models describe SAD in adolescence; given that SAD primarily onsets in adolescence, the reader may be forgiven for thinking this process has a bit of a backwards quality.
A number of studies have found evidence that, relative to their nonsocially anxious counterparts, socially anxious teens generate more negative interpretations of ambiguous and neutral social performance situations, worry about negative outcomes, and have flawed representations of both social threat and their own ability to perform effectively in social situations (Cartwright-Hatton et al. 2005; Miers et al. 2008; Muris et al. 2000; Rheingold et al. 2003; Spence et al. 1999). Higa and Daleiden (2008) reported that heightened SAD was associated with heightened self-focus in teens, but experimental manipulation of self-imagery to heighten negative self-awareness did not influence ratings of social anxiety in nonanxious teens, whether self- or observer reported (Alfano et al. 2008). Such events can be further complicated by cognitive factors; socially anxious children and teens have been found to be hypervigilant for threatening social-evaluative cues relative to their less anxious peers (Foa et al. 1996; Lucock and Salkovskis 1988; Muris et al. 2000). Socially anxious teens also demonstrate deficits in executive control, such as finding it more difficult to eliminate no longer relevant material from memory in a directed forgetting task (Gomez-Ariza et al. 2013). And, although interest in selective attention for threatening stimuli has become an area of hot research interest over the last decade, thus far no studies have examined adolescents for these biases (Higa-McMillan and Ebesutani 2011).
Besides concerns over the gaps in research that might help us further understand SAD, we must also consider that even the extensive extant research on SAD in adolescence, particularly of the biological and especially neurological underpinnings of SAD, is plagued by small and overwhelmingly white samples. In addition to the concerns over sufficient power, especially as the ambitions and analyses of these samples grow ever more complex, we must be concerned over the homogeneity of the samples as well. In their seminal review regarding the study of anxiety disorders in African-American populations, Neal and Turner (1991) noted that the mode of nonwhite participants in research studies on anxiety was zero. Lamentably, a cursory review of the literature will indicate that in the ensuing two decades, this situation has not improved much.
With these major caveats in mind, we can note that the last two decades have also generated exciting progress in understanding SAD in adolescence, and we can best regard these as challenges and directions for growth. The chronic and often deteriorating lifetime course of SAD makes a strong case for early recognition and early intervention in this disorder. As we have come to use more developmentally informed approaches in the conceptualization and targeting of the illness, our own understanding has grown exponentially. Treatment models have shown great foresight in emphasizing a multidimensional approach to this multifaceted problem. Further armed with research about the early risk factors and stressors that cause social anxiety to take hold over the individual, we are now able to think of the period in a way that is even more embedded in the specific developmental tasks and challenges of adolescence. To that end, treatment of the adolescent (ages 13–17) and the emerging adult (ages 18–28) in our clinic now involves a multifaceted, exposure and family-based approach that is patient-centered with intervention components prescribed according to functional and developmental impairments.
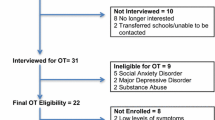
The launching emerging adults program (LEAP; Albano A.M. (unpublished)) incorporates our earlier model of CBGT-A and expands upon the role and tasks of development in the healthy transition from adolescence to independent adult functioning. It is well established that an interaction of adolescent avoidance of social-anxiety provoking situations and parental overprotection (e.g., inadvertent or deliberate reinforcement of avoidance, assisting with task completion) serves to maintain anxiety. This parental involvement also prevents or delays the adolescent’s development of the ability to take on situations and tasks that are normative for their emerging independent functioning (see Table 9.1). These tasks involve everyday activities from shopping for one’s self to arranging for healthcare visits, to seeking out opportunities for education or employment, to effectively managing social and romantic relationships and their ups and downs, without parental intervention. If parents continue to be centrally engaged in the completion of behaviors, on adolescent’s behalf, that promote the adolescent’s development, then the teen is compromised not just with greater anxiety but also with having less skill and ability to function independently over time. Indeed, through a pattern of parental leveling and even removal of essential opportunities for developmentally appropriate challenge and growth, it is proposed that this cycle takes the adolescent off of the track of normal or typical development, fostering a greater and longer dependency on the parents and inhibiting their transition to adult functioning. Therefore, effective treatment needs to address not only the adolescent’s anxiety but also the context of parent-adolescent interactions that maintain anxiety and stalls development. Figure 9.1 presents a schematic representation of the LEAP treatment model, whereby adolescents engage in individual and/or group CBT, with specific “transition sessions” designed to address parent-adolescent interactions.
A model for developmentally informed CBT for adolescents and emerging adults with social anxiety disorder: The launching emerging adults program (From Detweiler et al. (2014), with permission of Elsevier)
LEAP is in development in response to the absence of a focus in CBT programs on developmental tasks of transition from one stage to the next and, specifically, to increase independent functioning as the adolescent prepares for adulthood. Few CBT programs explicitly address autonomy issues and the implications for the transfer of responsibility for everyday tasks but also for managing the youth’s social anxiety (and related disorders) from parent to the adolescent. Adolescents (or young adults) are offered individual CBT, with the traditional anxiety exposures being largely conducted in group format, as in CBGT-A (Albano et al. 1991). This allows for individualized attention to the adolescent’s needs and for establishing a therapeutic alliance along with goal setting and cognitive work, while simultaneously capitalizing on the rich ecological validity of the group format with similar-aged peers for conducting exposures. These exposure groups are initially conducted within the clinic, using mainly the role-play format found in CBGT-A and in the Heimberg model. However, exposures then move to an in vivo format, to situations and activities found in the local environment, such as in stores, on subways, restaurants, and other public settings. The idea is to capitalize on the contextual elements of real situations to enhance the validity of the exposure and the unpredictability of the real world.
In addition, LEAP involves a series of parent-adolescent “transition sessions.” In these sessions conducted by an individual therapist, a developmental hierarchy is created in collaboration with the adolescent and parent, and then subsequent contextual exposures make explicit the parents’ stepping back to allow for focus on remediating the adolescent’s functional impairment while addressing anxiety and arrested development. Further, in these supportive contexts, adolescents and parents discuss their beliefs, frustration, wishes, and other aspects of emotion that they experience with each other, and through communication training and family problem-solving, they co-negotiate action plans for allowing more autonomy and acceptance of responsibility on the part of the adolescent for managing age-appropriate tasks. We often address the parents’ fear of their child “failing” in a given situation and work through the value of allowing “mess ups” to occur for the learning experience. In this way, parents are taught how to reduce the tendency to respond impulsively and emotionally and instead assume the role of effective, planful coaches and how to assist the adolescent without taking over the situation.
Related work by Garcia-Lopez and colleagues (2014) found promising results for adding a parent training component to a school-based treatment for social anxiety in adolescents (ages 13–18). For parents who evidenced high expressed emotion (EE), training to reduce EE via communication skills and appropriate contingency management led to greater decreases in social distress, avoidance, and social anxiety in their adolescents, as compared to the group treatment without parent training. Similarly, LEAP is designed to address family communication in the context of development. The ultimate goals of LEAP are to improve the adolescent’s management of anxiety, decrease avoidance, change family interaction patterns to be supportive rather than enabling, and to improve developmental outcomes that support independent functioning over the long term. Evaluation of the LEAP approach is underway.
In conclusion, viewing SAD and its treatment through a developmentally informed lens can help us tighten our operationalization of what SAD is and provide for the most rigorous scientific examination of the phenomenology and etiology associated with this disorder. Armed with this greater understanding and as we increase the size and diversity of our samples to reflect the true complexity of this condition, we can insure that our findings remain both flexibly cognizant of the intense variability inherent in this condition and robust to the challenges of measuring shifts in our understanding of what is happening for these at-risk teens and what is the best thing to do about it. The context of the family, within which the adolescent lives and is dependent upon for meeting his or her needs, needs to be a focus of evaluation and treatment for youth with social anxiety, despite the prevailing and commonplace ideas that a wide boundary between therapist and parents is necessary for engaging adolescents during treatment. And finally, exposure remains the cornerstone of effective treatment for SAD. We advocate for using enhanced, ecologically valid, and contextually rich exposures to maximize the potential for improvement in symptoms but also in overall adaptive functioning.
Notes
- 1.
One will note that the age-group labels differ somewhat from conventional labels (including, indeed, other chapters in this volume). For the purposes of accurate reporting, we have chosen to conform to the labels used in the research reviewed in this study. We will address this labeling concern in more detail in the conclusion of this chapter.
- 2.
In fact, the earlier Wittchen and Fehm article reported that epidemiological samples find a unimodal peak onset during childhood and adolescence, between the ages of 10 and 16, while clinical samples report evidence for somewhat lower age of onset of the generalized subtype as compared with the nongeneralized subtype. The nature of these subtypes, as well as their continued redefinition, has been debated as recently as the latest edition of the Diagnostic and Statistical Manual (DSM-5; APA 2013).
References
Albano AM, Barlow DH (1996) Breaking the vicious cycle: cognitive-behavioral group treatment for socially anxious youth. In: Hibbs ED, Jensen PS (eds) Psychosocial treatments for child and adolescent disorders: empirically-based strategies for clinical practice. APA, Washington, DC, pp 43–62
Albano AM, Marten PA, Holt CS (1991) Cognitive-behavioral group treatment of adolescent social phobia: therapist manual. Unpublished manuscript, State University of New York at Albany
Albano AM, Marten PA, Holt CS, Heimberg RG, Barlow DH (1995) Cognitive-behavioral treatment for social phobia in adolescents: a preliminary study. J Nerv Ment Dis 183:649–656
Alfano CA, Beidel DC, Turner SM (2008) Negative self-imagery among adolescents with social phobia: a test of the adult model of the disorder. J Clin Child Adolesc Psychol 37:327–336
American Psychiatric Association (1980) Diagnostic and statistical manual of mental disorders, 3rd edn. American Psychiatric Association, Washington, DC
American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders, 5th edn. American Psychiatric Association, Washington, DC
Arrindell WA, Kwee MG, Methorst GJ, Van der Ende J, Pol E, Moritz BJ (1989) Perceived parental rearing styles of agoraphobic and socially phobic in-patients. Br J Psychiatry 155:526–535
Asendorph JB (1994) The malleability of behavioral inhibition: a study of individual developmental function. Dev Psychol 30:912–919
Barrett PM, Rapee RM, Dadds MM, Ryan SM (1996b) Family enhancement of cognitive style in anxious and aggressive children. J Abnorm Child Psychol 24:187–203
Battaglia M, Zanoni A, Taddei M, Giorda R, Bertoletti E, Lampis V, Scanini S, Cappa S, Tettamanti M (2012) Cerebral responses to emotional expressions and the development of social anxiety disorder: a preliminary longitudinal study. Depress Anxiety 29:54–61
Beatty MJ, Heisel AD, Hall AE, Levine TR, La France BH (2002) What can we learn from the study of twins about genetic and environmental influences on interpersonal affiliation, aggressiveness, and social anxiety? A meta-analytic study. Commun Monogr 69:1–18
Beidel DC, Turner SM, Morris TL (1998) Social effectiveness therapy for children: a treatment manual. Medical University of South Carolina, Charleston
Beidel DC, Turner SM, Morris TL (2000) Behavioral treatment of childhood social phobia. J Consult Clin Psychol 68:1072–1080
Biederman J, Hirshfeld-Becker DR, Rosenbaum JF, Herot C, Friedman D, Snidman N, Kagan J, Faraone SV (2001) Further evidence of association between behavioral inhibition and social anxiety in children. Am J Psychiatry 158:1673–1679
Blair KS, Geraci M, Korelitz K, Otero M, Towbin K, Ernst M, Leibenluft E, Blair RJR, Pine DS (2011) The pathology of social phobia is independent of developmental changes in face processing. Am J Psychiatry 168:1202–1209
Bogels SM, van Oosten A, Muris P, Smulders D (2001) Familial correlates of social anxiety in children and adolescents. Behav Res Ther 39:273–287
Bogels S, Stevens J, Madiandzic M (2011) Parenting and social anxiety: fathers’ versus mothers’ influence on their children’s anxiety in ambiguous situations. J Child Psychol Psychiatry 52:599–606
Brown TA, Campbell LA, Lehman CL, Grisham JR, Mancill RB (2001) Current and lifetime comorbidity of the DSM-IV anxiety and mood disorders. J Abnorm Psychol 110:49–58
Bruch MA, Heimberg RG (1994) Differences in perceptions of parental and personal characteristics between generalized and nongeneralized social phobics. J Anxiety Disord 8:155–168
Buote VM, Pancer SM, Pratt MW, Adams G, Birnie-Lefcovitch S, Polivy J, Wintre MG (2007) The importance of friends: friendship and adjustment among 1st-year university students. J Adolesc Res 22:665–689
Burgess K, Rubin KH, Cheah C, Nelson L (2001) Socially withdrawn children: parenting and parent-child relationships. In: The self, shyness and social anxiety: a handbook of concepts, research, and interventions. Wiley, New York
Burstein M, He J-P, Kattan G, Albano AM, Avenevoli S, Merikangas KR (2011) Social phobia and subtypes in the national comorbidity survey-adolescent supplement: prevalence, correlates, and comorbidity. J Am Acad Child Adolesc Psychiatry 50:870–880
Cartwright-Hatton S, Tschernitz N, Gomersall H (2005) Social anxiety in children: social skills deficit, or cognitive distortion? Behav Res Ther 43:131–141
Caspi A, Silva PA (1995) Temperamental qualities at age three predict personality traits in young adulthood: longitudinal evidence from a birth cohort. Child Dev 66:486–498
Caster JB, Inderbitzen HM, Hope D (1999) Relationship between youth and parent perceptions of family environment and social anxiety. J Anxiety Disord 13:237–251
Chronis-Tuscano A, Degnan KA, Pine DS, Perez-Edgar K, Henderson HA, Diaz Y, Raggi VL, Fox NA (2009) Stable early maternal report of behavioral inhibition predicts lifetime social anxiety disorder in adolescence. J Am Acad Child Adolesc Psychiatry 48:928–935
Clauss JA, Blackford JU (2012) Behavioral inhibition and risk for developing social anxiety disorder: a meta-analytic study. J Am Acad Child Adolesc Psychiatry 51:1066–1075
Compas BE (2004) Processes of risk and resilience during adolescence: Linking contexts and individuals. In Lerner RM, Steinberg L (Eds.) Handbook of Adolescent Psychology, 2nd ed. John Wiley & Sons
Compton SN, Nelson AH, March JS (2000) Social phobia and separation anxiety symptoms in community and clinical samples of children and adolescents. J Am Acad Child Adolesc Psychiatry 39:1040–1046
Detweiler MF, Comer JS, Crum KI, Albano AM (2014) Social anxiety in children and adolescents: biological, developmental and social considerations. In: Hofmann SG, DiBartolo PM (eds) Social anxiety: clinical, developmental and social perspectives, 3rd edn. Academic Press, Amsterdam, pp 254–309
Elkind D (1967) Egocentrism in adolescence. Child Dev 38:1025–1034
Erikson EH (1959) Identity and the life cycle (Vol. 1). Psychological Issues. Monograph, 1. International Universities Press, New York
Finnie V, Russell A (1988) Preschool children’s social status and their mothers’ behavior and knowledge in the supervisory role. Dev Psychol 24:789
Foa EB, Franklin ME, Perry KJ, Herbert JD (1996) Cognitive biases in generalized social phobia. J Abnorm Psychol 105:433
Fordham K, Stevenson‐Hinde J (1999) Shyness, friendship quality, and adjustment during middle childhood. J Child Psychol Psychiatry 40:757–768
Fyer AJ, Mannuzza S, Chapman TF, Liebowitz MR, Klein DF (1993) A direct interview family study of social phobia. Arch Gen Psychiatry 50:286–293
Fyer AJ, Manuzza S, Chapman TF, Martin LY, Klein DF (1995) Specificity in familial aggregation of phobic disorders. Arch Gen Psychiatry 52:564–573
Gallagher HM, Rabian BA, McCloskey MS (2004) A brief group cognitive behavioral intervention for social phobia in childhood. J Anxiety Disord 18:459–479
Garcia-Lopez LJ (2000, 2007) Examining the efficacy of three cognitive-behavioural treatments aimed at overcoming social anxiety in adolescents. University of Murcia: Publication Service
Garcia-Lopez LJ, Olivares J, Turner SM, Albano AM, Beidel DC, Sanchez-Meca J (2002) Results at long-term among three psychological treatments for adolescents with generalized social phobia (II): clinical significance and effect size. Psicol Conductual Behav Psychol 10:371–385
Garcia-Lopez LJ, Olivares J, Beidel DC, Albano AM, Turner SM, Rosa AI (2006) Efficacy of three treatment protocols for adolescents with social anxiety disorder: a five-year follow up assessment. J Anxiety Disord 20:175–191
Garcia-Lopez LJ, Muela JM, Espinosa-Fernandez L, Diaz-Castela M (2009) Exploring the relevance of expressed emotion to the treatment of social anxiety disorder in adolescence. Journal of Adolescence 32:1371–1376
Garcia-Lopez LJ, Diaz-Castela MM, Muela-Martinez JA, Espinosa-Fernandez L (2014) Can parent training for parents with high levels of expressed emotion have a positive effect on their child’s social anxiety improvement? J Anxiety Disord 28:812–822
Goldsmith HH, Lemery KS (2000) Linking temperamental fearfulness and anxiety symptoms: a behavior–genetic perspective. Biol Psychiatry 48:1199–1209
Gomez-Ariza CJ, Iglesias-Parro S, Garcia-Lopez LJ, Diaz-Castela M, Espinosa-Fernandez L, Muela JA (2013) Selective intentional forgetting in adolescents to social anxiety disorder. Psychiatry Res 208:151–155
Greco L, Morris T (2002) Paternal child-rearing style and child social anxiety: investigation of child perceptions and actual father behavior. J Psychopathol Behav Assess 24:259–267
Gulley LD, Oppenheimer CW, Hankin BL (2014) Associations among negative parenting, attention bias to anger, and social anxiety among youth. Developmental Psychology 50:577–585
Guyer AE, Lau JY, McClure-Tone EB, Parrish J, Shiffrin ND, Reynolds RC, Chen G, Blair RJR, Leibenluft E, Fox NA, Ernst M, Pine DS, Nelson EE (2008) Amygdala and ventrolateral prefrontal cortex function during anticipated peer evaluation in pediatric social anxiety. Arch Gen Psychiatry 65:1303–1312
Hall GS (1904) Adolescence, vol 2. Appleton, New York
Hayward C, Varady S, Albano AM, Thienemann M, Henderson L, Schatzberg AF (2000) Cognitive-behavioral group therapy for social phobia in female adolescents: results of a pilot study. J Am Acad Child Adolesc Psychiatry 39:721–726
Heimberg RG, Becker RE, Goldfinger K, Vermilyea JA (1985) Treatment of social phobia by exposure, cognitive restructuring, and homework assignments. J Nerv Ment Dis 173:236–245
Heimberg RG, Dodge CS, Hope DA, Kennedy CR, Zollo L, Becker RE (1990) Cognitive behavioral group treatment for social phobia: comparison to a credible placebo control. Cognit Ther Res 14:1–23
Heimberg RG, Hofmann SG, Liebowitz MR, Schneier FR, Smits JAJ, Stein MB, Hinton DE, Craske MG (2014) Social anxiety disorder in DSM-5. Depress Anxiety 31:472–479
Higa CK, Daleiden EL (2008) Social anxiety and cognitive biases in non-referred children: the interaction of self-focused attention and threat interpretation biases. J Anxiety Disord 22:441–452
Higa-McMillan CK, Ebesutani C (2011) The etiology of social anxiety disorder in adolescents and young adults. In: Alfano CA, Beidel DC (eds) Social anxiety in adolescents and young adults: translating developmental science into practice. American Psychological Association, Washington, DC, pp 29–51
Hirshfeld DR, Rosenbaum JF, Beiderman J, Bolduc EA, Faraone SV, Snidman N, Reznick JS, Kagan J (1992) Stable behavioral inhibition and its association with social anxiety disorder. J Am Acad Child Adolesc Psychiatry 31:103–111
Hope DA, Heimberg RG (1993) Social phobia and social anxiety. In: Barlow DH (ed) Clinical handbook of psychological disorders: a step-by-step treatment manual. Guilford Press, New York, pp 99–136
Horwath E, Weissman MM (1995) Epidemiology of depression and anxiety disorders. In: Textbook in psychiatric epidemiology. Wiley-Liss, New York, pp 317–344
Hudson JL, Rapee RM (2001) Parent–child interactions and anxiety disorders: an observational study. Behav Res Ther 39:1411–1427
Hudson JL, Rapee RM (2002) Parent-child interactions in clinically anxious children and their siblings. J Clin Child Adolesc Psychol 31:548–555
Hudson JL, Rapee RM (2005) Parental perceptions of overprotection: specific to anxious children or shared between siblings? Behav Change 22:185–194
Hughes AA, Furr JM, Sood ED, Barmish AJ, Kendall PC (2009) Anxiety, mood, and substance use disorders in parents of children with anxiety disorders. Child Psychiatry Hum Dev 40:405–419
Inderbitzen HM, Walters KS, Bukowski AL (1997) The role of social anxiety in adolescent peer relations: differences among sociometric status groups and rejected subgroups. J Clin Child Psychol 26:338–348
Juster HR, Heimberg RG (1995) Social phobia: longitudinal course and long-term outcome of cognitive-behavioral treatment. Psychiatr Clin North Am 18:821–842
Kagan J (1989) Temperamental contributions to social behavior. Am Psychol 44:668–674
Kagan J, Reznick JS, Snidman N (1988) Biological bases of childhood shyness. Science 240:167–171
Kendler KS, Neale MC, Kessler RC, Heath AC, Eaves LJ (1992) The genetic epidemiology of phobias in women: the interrelationship of agoraphobia, social phobia, situational phobia, and simple phobia. Arch Gen Psychiatry 49:273–281
Kendler KS, Myers J, Prescott CA (2002) The etiology of phobias: an evaluation of the stress-diathesis model. Arch Gen Psychiatry 59:242–248
Knappe S, Beesdo K, Fehm L, Hofler M, Lieb R (2009) Do parental psychopathology and unfavorable family environments predict the persistence of social phobia? J Anxiety Disord 23:986–994
Knappe S, Beesdo-Baum K, Fehm L, Lieb R, Wittchen H-U (2012) Characterizing the association between parenting and adolescent social phobia. J Anxiety Disord 26:608–616
La Greca AM, Lopez N (1998) Social anxiety among adolescents: linkages with peer relations and friendships. J Abnorm Child Psychol 26:83–94
La Greca AM, Prinstein MJ (1999) Peer group. In: Silverman WK, Ollendick TH (eds) Developmental issues in the clinical treatment of children. Allyn & Bacon, Needham Heights, pp 171–198
La Greca AM, Mufson L, Ehrenreich-May J, Girio-Herrera E, Chan S (2014) Developing an evidence-based preventive intervention for peer victimized adolescents at risk for social anxiety disorder and/or depression. Presented at the biennial meeting of the International Society for Affective Disorders, Berlin, Apr 2014
Lieb R, Wittchen HU, Höfler M, Fuetsch M, Stein MB, Merikangas KR (2000) Parental psychopathology, parenting styles, and the risk of social phobia in offspring: a prospective-longitudinal community study. Arch Gen Psychiatry 57:859–866
Lucock MP, Salkovskis PM (1988) Cognitive factors in social anxiety and its treatment. Behav Res Ther 26:297–302
Manuzza S, Schneier FR, Chapman TF, Liebowitz MR, Klein DF, Fyer AJ (1995) Generalized social phobia: reliability and validity. Arch Gen Psychiatry 52:230–237
Masia CL, Beidel DC, Albano AM, Rapee RM, Turner SM, Morris TL, et al. (1999) Skills for academic and social success. Available from Carrie Masia-Warner, New York
Masia CL, Morris TL (1998) Parental factors associated with social anxiety: methodological limitations and suggestions for integrated behavioral research. Clin Psychol Sci Pract 5:211–228
Miers AC, Blöte AW, Bögels SM, Westenberg PM (2008) Interpretation bias and social anxiety in adolescents. J Anxiety Disord 22:1462–1471
Muris P, Merckelbach H, Damsma E (2000) Threat perception bias in nonreferred, socially anxious children. J Clin Child Psychol 29:348–359
Neal AM, Turner SM (1991) Anxiety disorders research with African Americans: current status. Psychol Bull 109(3):400
Olivares J, Garcia-Lopez LJ, Beidel DC, Turner SM, Albano AM, Hidalgo M (2002) Results at long-term among three psychological treatments for adolescents with generalized social phobia (I): statistical significance. Psicol Conductual 10:147–164
Ollendick TH, Hirshfeld-Becker DR (2002) The developmental psychopathology of social anxiety disorder. Biol Psychiatry 51:44–58
Öst LG (1985) Ways of acquiring phobias and outcome of behavioral treatments. Behav Res Ther 23:683–689
Öst LG, Hugdahl K (1981) Acquisition of phobias and anxiety response patterns in clinical patients. Behav Res Ther 19:439–447
Parker G (1979) Reported parental characteristics in relation to trait depression and anxiety levels in a non-clinical group. Australas Psychiatry 13:260–264
Perez-Edgar KE, Guyer AE (2014) Behavioral inhibition: temperament or prodrome? Curr Behav Neurosci Rep 1:182–190
Prenoveau JM, Craske MG, Zinbarg RE, Mineka S, Rose RD, Griffith JW (2011) Are anxiety and depression just as stable as personality during late adolescence? Results from a three-year longitudinal latent variable study. J Abnorm Psychol 120:832–843
Puklek Levpušček M (2006) Adolescent individuation in relation to parents and friends: age and gender differences. Eur J Dev Psychol 3:238–264
Ranta K, Kaltiala-Heino R, Pelkonen M, Marttunen M (2009) Associations between peer victimization, self-reported depression and social phobia among adolescents: the role of comorbidity. J Adolesc 32:77–93
Ranta K, Kaltiala-Heino R, Frojd S, Marttunen M (2013) Peer victimization and social phobia: a follow-up study among adolescents. Soc Psychiatry Psychiatr Epidemiol 48:533–544
Rapee RM, Heimberg RG (1997) A cognitive-behavioral model of anxiety in social phobia. Behav Res Ther 35:741–756
Reich J, Yates W (1988) Family history of psychiatric disorders in social phobia. Compr Psychiatry 29:72–75
Reich J, Goldenberg I, Vasile R, Goisman R (1994) A prospective follow-along study of the course of social phobia. Psychiatry Res 54:249–258
Rheingold AA, Herbert JD, Franklin ME (2003) Cognitive bias in adolescents with social anxiety disorder. Cognit Ther Res 27:639–655
Rosellini AJ, Rutter LA, Bourgeois ML, Emmert-Aronson BO, Brown TA (2013) The relevance of age of onset to the psychopathology of social phobia. J Psychopathol Behav Assess 35:356–365
Rubin KH, Mills RS (1990) Maternal beliefs about adaptive and maladaptive social behaviors in normal, aggressive, and withdrawn preschoolers. J Abnorm Child Psychol 18:419–435
Schwartz CE, Snidman N, Kagan J (1999) Adolescent social anxiety as an outcome of inhibited temperament in childhood. J Am Acad Child Adolesc Psychiatry 38:1008–1015
Siegel RS, La Greca AM, Harrison HM (2009) Peer victimization and social anxiety in adolescents: prospective and reciprocal relationships. J Youth Adolesc 38:1096–1109
Siqueland L, Kendall PC, Steinberg L (1996) Anxiety in children: perceived family environments and observed family interaction. J Clin Child Psychol 25:225–237
Skre I, Onstad S, Torgersen S, Lygren S, Kringlen E (1993) A twin study of DSM‐III‐R anxiety disorders. Acta Psychiatr Scand 88:85–92
Smetana JG (1997) Parenting and the development of social knowledge reconceptualized: a social domain analysis. In: Grusec JE, Kuczynski L (eds) Parenting and the internalization of values. New York, Wiley, pp 162–192
Spence SH (1995) Social skills training: enhancing social competence with children and adolescents. NFER-Nelson, Windsor
Spence SH, Donovan C, Brechman-Toussaint M (1999) Social skills, social outcomes, and cognitive features of childhood social phobia. J Abnorm Psychol 108:211
Spence SH, Donovan C, Brechman-Toussaint M (2000) The treatment of childhood social phobia: the effectiveness of a social skills training-based, cognitive-behavioral intervention, with and without parental involvement. J Child Psychol Psychiatry 41:713–726
Stein MB, Stein DJ (2008) Social anxiety disorder. Lancet 371:1115–1125
Stein M, Chartier M, Hazen A, Kozak M, Tancer M, Lander S (1998) A direct-interview family study of generalized social phobia. Am J Psychiatry 155:90–97
Steinberg L (2001) We know some things: parent–adolescent relationships in retrospect and prospect. J Res Adolesc 11(1):1–19
Steinberg L (2004) Risk taking in adolescence: what changes, and why? Ann N Y Acad Sci 1021(1):51–58
Stemberger RT, Turner SM, Beidel DC, Calhoun KS (1995) Social phobia: an analysis of possible developmental factors. J Abnorm Psychol 104(3):526–531
Storch EA, Masia‐Warner C, Crisp H, Klein RG (2005) Peer victimization and social anxiety in adolescence: a prospective study. Aggress Behav 31:437–452
Vasey MW, Dadds MR (2001) The developmental psychopathology of anxiety. Oxford University Press, New York
Wittchen H-U, Fehm L (2003) Epidemiology and natural course of social fears and social phobia. Acta Psychiatr Scand Suppl 108:4–18
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Guerry, J.D., Hambrick, J., Albano, A.M. (2015). Adolescent Social Phobia in Clinical Services. In: Ranta, K., La Greca, A., Garcia-Lopez, LJ., Marttunen, M. (eds) Social Anxiety and Phobia in Adolescents. Springer, Cham. https://doi.org/10.1007/978-3-319-16703-9_9
Download citation
DOI: https://doi.org/10.1007/978-3-319-16703-9_9
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-16702-2
Online ISBN: 978-3-319-16703-9
eBook Packages: MedicineMedicine (R0)